Abstract
We studied the predictors and patterns of high-sensitivity cardiac troponin T (hs-cTnT) elevation in patients with paroxysmal supraventricular tachycardia (PSVT) in the presence and absence of ischemic heart disease.
During calendar year 2013, we enrolled 70 of 72 consecutive adult patients with PSVT who presented at our center within 4 hours after the onset of tachycardia. On the basis of increased hs-cTnT at either of 2 initial measurements, we divided patients into groups (hs-cTnT–positive and hs-cTnT–negative), to study the predictors of enzyme elevation. We then divided the hs-cTnT–positive patients into 2 groups—those with and those without ischemic heart disease—and compared hs-cTnT changes.
We observed hs-cTnT elevation in 52 of the 70 patients (74.3%). The hs-cTnT–positive patients were significantly older (P=0.008) and had a significantly higher duration of tachycardia (P=0.01). Older age, the presence of chest pain, lower diastolic blood pressure, and longer duration of tachycardia increased the odds of enzyme elevation. Among patients with elevated hs-cTnT levels, the baseline and maximal hs-cTnT levels were significantly higher in ischemic patients (P=0.01 and P=0.003, respectively). The increase in hs-cTnT seemed to be higher and longer in ischemic patients, although this was not statistically significant (P=0.908). Finally, hs-cTnT did not decrease to baseline levels within 48 hours in either group.
We found that hs-cTnT levels increased in all our patients with PSVT, more so in those with ischemic heart disease.
Keywords: Biomarkers/analysis/blood; coronary disease/diagnosis; myocardial ischemia/pathology; predictive value of tests; prospective studies; tachycardia, paroxysmal/blood/diagnosis; tachycardia, supraventricular/blood/diagnosis; time factors; troponin T/analysis/blood
Cardiac troponin T (cTnT) is a highly sensitive and specific biomarker for the diagnosis of acute myocardial infarction (AMI).1 However, elevated cTnT is also seen in other cardiac and noncardiac conditions.2–5 It has therefore been proposed that the diagnosis of AMI should be made depending on changes in cTnT level in an appropriate clinical situation, to distinguish ischemic from nonischemic causes of cTnT elevation.6 In addition, recently available high-sensitivity troponin assays can reliably detect much lower concentrations of troponin than older assays could. However, minor changes or elevations in cTnT levels without other evidence for AMI can be confusing.
Paroxysmal supraventricular tachycardia (PSVT) has been identified as a probable cause of troponin elevation in the absence of severe ischemic heart disease (IHD).7,8 This can mislead clinicians in the management of PSVT. Therefore, defining the kinetic effects of troponin elevation, especially high-sensitivity troponin, as well as the predictors of elevation, is important for straightforward clinical diagnosis of a possible underlying ischemic condition.
In this study, we had 2 goals: to identify predictors of high-sensitivity cardiac troponin T (hs-cTnT) elevation; and to determine the pattern of changes in hs-cTnT levels in PSVT patients who had elevated hs-cTnT levels (with or without IHD) upon presentation at the emergency department of our tertiary-care cardiovascular center.
Patients and Methods
During calendar year 2013, we prospectively enrolled consecutive patients (age, >30 yr) who were admitted to the emergency department of Tehran Heart Center within 4 hours after the onset of a regular narrow-complex tachycardia, with symptoms of chest pain or dyspnea.
We recorded demographic characteristics, medical histories, blood pressures, and electrocardiographic variables for all participants. We excluded patients with a clear history or current evidence of congestive heart failure, chronic kidney disease, sepsis, pulmonary embolism, myocardial contusion, atrial fibrillation, severe valvular heart disease, electrophysiologic procedures within the previous 7 days, wide-complex tachycardia, and emergency presentation after 4 hours from the onset of tachycardia. Patients who had elevated levels of hs-cTnT in either the first or second sample (at presentation or 8 hr later) were compared with patients who did not have elevated levels of hs-cTnT, to evaluate predictors of hs-cTnT elevation. The patients were stabilized and cardioversion was performed, with sequential use of carotid sinus massage, intravenous adenosine, and verapamil. We then screened for the presence of IHD in the patients who had hs-cTnT elevation, and we compared changes in hs-cTnT levels between the patients with and without IHD.
Transthoracic echocardiography was performed after PSVT cardioversion. Patients with a left ventricular ejection fraction <0.35 or with severe valvular disease were excluded from the study.
All participants gave written informed consent. The study protocol conformed to the ethical guidelines of the Declaration of Helsinki, and it was approved by the Research Board of Tehran Heart Center and the Committee of Medical Ethics at Tehran University of Medical Sciences.
Cardiac Biomarker Testing
A sample of venous blood for hs-cTnT testing was taken from the antecubital vein at the time of presentation. The blood was immediately processed and kept frozen at −80 °C until it was assayed with use of a pre-commercial hs-cTnT assay on an Elecsys® 2010 platform (Roche Diagnostics; Penzberg, Germany). The high-sensitivity assay is reported in units of ng/L and reportedly has a coefficient of variation of 8% at 10 ng/L.9 Our patients were then categorized into 2 groups: hs-cTnT–positive (serum hs-cTnT level, ≥14 ng/L) and hs-cTnT–negative (serum hs-cTnT level, <14 ng/L).
Biomarkers were rechecked at 8-hour intervals during the first 24 hours, at 12-hour intervals during the second 24 hours, and, finally, 72 hours after admission, unless the hs-cTnT level decreased to 50% of the maximal level. If the first 2 measurements were within normal ranges for hs-cTnT, the patients were excluded from further sampling. The laboratory staff who performed the measurements were unaware of the study protocol. To reveal the pattern of enzyme elevation, we selected patients who had at least 3 consecutive measurements.
Evaluation of Ischemic Heart Disease
The presence of IHD was evaluated by means of diagnostic coronary angiography (CA), 256-slice cardiac computed tomographic angiography (CTA), or myocardial perfusion single-photon-emission computed tomography (SPECT) after biomarker sampling, at the physician's discretion on the basis of the clinical findings and each patient's consent. The indication for CA was clinical suspicion arising from the signs, symptoms, and electrocardiographic findings. Patients were considered to have IHD if they had reversible or fixed defects on myocardial perfusion scans or had coronary artery stenosis >70% on CA or CTA. The changes in enzyme levels were compared in the IHD-positive and the IHD-negative patients.
Statistical Analysis
Continuous variables are described as mean ± SD or median and interquartile range, and categorical variables are described as number and percentage. Continuous variables were compared between patients with and without hs-cTnT elevation, and also between the subgroups with and without IHD, with use of the Student t or Mann-Whitney U test. Categorical variables were compared between the mentioned groups by using the χ2 or Fisher exact test. Variables with P values <0.2 in the univariate analyses of enzyme elevation were entered into the multivariate model. The backward logistic regression model with entry and removal probability of 0.1 was used to determine the predictors of hs-cTnT elevation. The associations of independent predictors of hs-cTnT elevation in the model were expressed as odds ratios with 95% confidence intervals. Model discrimination was measured by using the area under the receiver operating characteristic curve, and model calibration was estimated by using the Hosmer-Lemeshow goodness-of-fit statistic (P=0.84). P values <0.05 were considered statistically significant. All statistical analyses were performed with use of PASW Statistics 18.0 (SPSS Inc., an IBM company; Chicago, Ill).
Results
Of the 72 PSVT patients referred to our center within the study period, 70 met the inclusion criteria (Table I). In the initial 2 measurements, 52 patients (74.3%) were hs-cTnT–positive. Levels of hs-cTnT were elevated at the first measurement in 42 of those 52 patients (80.8%), and at the second measurement in 10 patients (19.2%). The hs-cTnT–positive patients were significantly older (P=0.008), had chest pain as a statistically significant presenting symptom (P <0.001), and had higher rates of dyspnea and dyslipidemia (both P=0.05). The duration of tachycardia was significantly longer in the hs-cTnT–positive patients (P=0.01).
TABLE I.
Presenting Characteristics of 70 Patients According to hs-cTnT Level
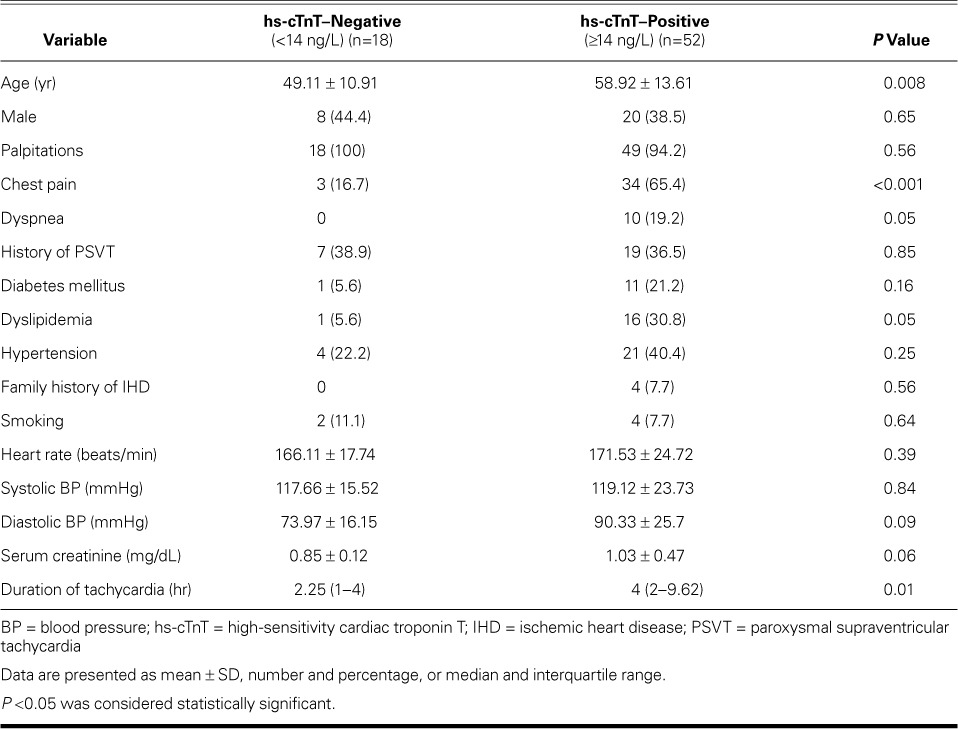
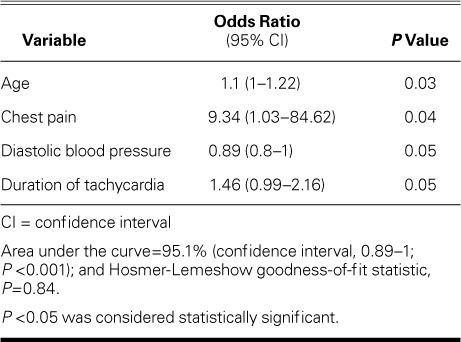
Older age, the presence of chest pain, lower diastolic blood pressure, and longer duration of tachycardia were the multivariate predictors of hs-cTnT elevation, and chest pain was the dominant predictor (Table II).
TABLE II.
Multivariate Predictors of Elevated High-Sensitivity Cardiac Troponin T Levels
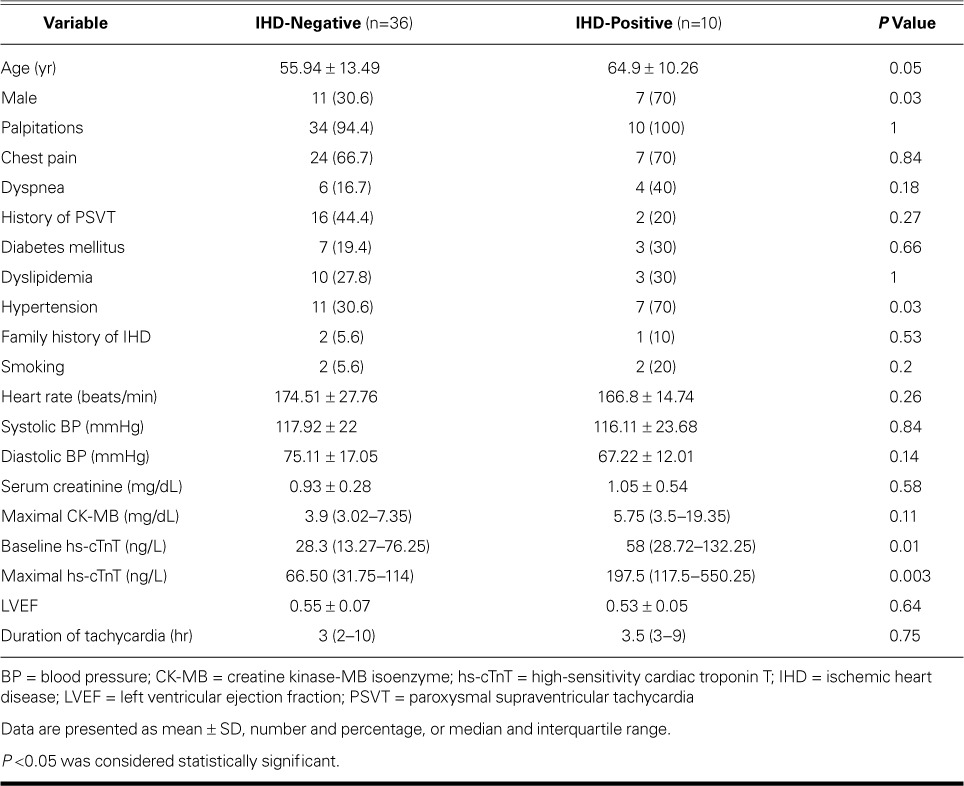
Six of the 52 patients with hs-cTnT elevation left the study and underwent no serial sampling. The remaining 46 patients were screened for IHD (Table III). Underlying IHD was ruled out in 23 patients by means of SPECT, in 8 by CA, and in 5 by CTA. Ten patients (21.7%) had underlying IHD as confirmed by CA results. The IHD-positive patients were older than the IHD-negative patients (P=0.05). In addition, more IHD patients were male (P=0.03) and hypertensive (P=0.03). The baseline and maximal levels of hs-cTnT were significantly higher in IHD-positive patients (P=0.01 and P=0.003, respectively) (Table III).
TABLE III.
Comparison of Patients with and without Underlying Ischemic Heart Disease
In the next step, we compared changes in hs-cTnT between patients with and without underlying IHD. In both the positive and negative groups, hs-cTnT levels began to rise within 16 hours after the onset of PSVT. This rise seemed to be more prominent in patients with IHD, although the difference was not statistically significant (P=0.908). The mean level of hs-cTnT began decreasing approximately 20 hours after the onset of tachycardia in the IHD-negative group but continued to increase in the IHD-positive group and peaked within 36 hours from the onset of tachycardia; however, hs-cTnT did not decrease to the levels at presentation within 48 hours in either group (Fig. 1). There was also no difference between the groups in changes in hs-cTnT over time (P=0.742).
Fig. 1.
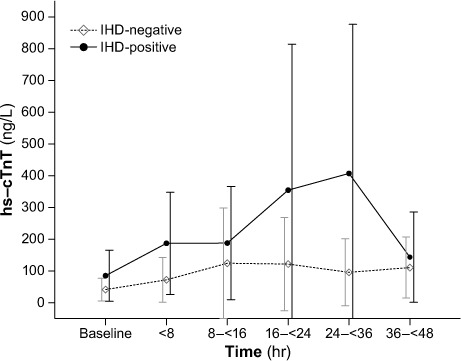
Graph compares hs-cTnT (high-sensitivity cardiac troponin T) levels (mean) and 95% confidence intervals in patients with and without ischemic heart disease (IHD). The mean level of hs-cTnT began decreasing approximately 20 hours after the onset of tachycardia in the IHD-negative group, but it continued to increase in the IHD-positive group, peaking within 36 hours of the onset of tachycardia.
Discussion
In this study, the prevalence of hs-cTnT elevation in PSVT patients was 74.3%, and 21.7% of these patients had underlying IHD. Levels of hs-cTnT rose within 16 hours of tachycardia, reaching maximal levels within 20 hours in IHD-negative patients compared with 36 hours in IHD-positive patients. In addition, hs-cTnT levels were significantly higher in IHD-positive patients, and those levels remained higher after 48 hours.
The newer, more sensitive cardiac biomarker assays have made it possible to recognize small degrees of myocardial injury. It has, however, been emphasized that cTnT elevation does not necessarily indicate myocardial necrosis and can be related only to myocardial damage, which can be caused by ischemic or nonischemic conditions.10 During emergency evaluations, elevated levels of cTnT should be interpreted as a sign of AMI with great caution; serial measurements of the biomarkers can effectively help in reaching proper decisions.11 Nevertheless, understanding the pattern of changes in hs-cTnT is crucial for differentiating between enzyme elevation in AMI and that related to ischemic myocardial injury from PSVT.
Although multiple authors of case reports and series have shown that cardiac enzyme levels rise during PSVT,7,12,13 we found only one study14 in which the pattern of enzyme elevation was described. Of note, elevated concentrations of serum cTnT are observed in many but not all patients with PSVT,8 rendering it difficult to explain the mechanism of cTnT elevation. It is argued that transient elevations of cTnT can occur without cardiomyocyte death, and several mechanisms have been proposed to explain this phenomenon.15 The initial release of cTnT might stem from the early-appearing myocyte pool and later from the structural pool.16 Regarding PSVT, the mechanism for elevation is probably the shortening of diastole with subsequent subendocardial ischemia.3 The multivariate predictors of hs-cTnT elevation in the current study were age, chest pain at presentation, low diastolic blood pressure, and longer duration of tachycardia. Accordingly, it seems that PSVT can increase hs-cTnT levels regardless of the presence of IHD, whereas IHD contributes to a higher elevation of the hs-cTnT level, for a longer duration. Because we excluded other comorbidities, cTnT increase could be related only to PSVT in our study.
We observed that high levels of hs-cTnT decreased with the response to treatment. This may show how PSVT is related to cardiac enzyme elevation. In the one study of the kinetic patterns of troponin elevation after PSVT,14 the investigators observed that patients who had no underlying cardiac pathologic conditions had cTnT elevation and that there was a trend toward a decrease in cTnT levels ≥6 hours from presentation, regardless of the presence or absence of underlying heart disease.
Previous comparisons of the pattern of troponin elevation in PSVT and ST-segment-elevation myocardial infarction (STEMI) showed that the level of troponin increased during the first day of STEMI and reached maximal levels after the first day from onset of STEMI,17 whereas in patients with PSVT alone, the maximal rise of the enzyme occurred within 8 to 16 hours of the onset of PSVT.
Heart rate during PSVT and the presence of impaired left ventricular systolic function have been reported as predictors of troponin elevation.8,18 In our study, heart rate did not correlate with elevation of hs-cTnT, although the duration of tachycardia had an association. This finding may be explained by these proposed mechanisms for troponin elevation during cardiac stress and tachycardia: troponin is released via integrin-mediated transient membrane leakage19 or through intact membranes via the formation of blebs that contain non-structurally bound troponin.20
Chief among the strengths of this study are prospective collection of data and procurement of several sequential samples. Moreover, we included patients who did not have elevated hs-cTnT at presentation but had increased levels in the next sampling.
Study Limitations
The main limitation of this study is its small patient cohort. In addition, we could not monitor all patients on an inpatient basis for changes in enzyme levels. Some patients refused to stay in the hospital after successful cardioversion, so fewer measurements were performed for them. Finally, the results of this single-center study might not easily extend to general populations because of demographic factors.
Conclusion
We found that older age, lower diastolic blood pressure, longer tachycardia duration, and chest pain were the main predictors of cTnT elevation in PSVT patients. Among patients with elevated enzyme levels, the maximal level of elevation was more likely to be higher in patients with IHD. Further studies with a larger population and a shorter time interval for troponin measurements are necessary to elucidate the exact changes in cardiac enzyme elevation in PSVT patients.
Acknowledgments
This study served as the doctoral dissertation of Dr. Mehdi Sayadnik for the degree of cardiology specialist. The authors thank the laboratory staff of Tehran Heart Center for their invaluable assistance.
References
- 1. Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, . et al. 2011 ACCF/AHA Focused Update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines [published erratum appears in Circulation 2011;123(22):e627]. Circulation 2011; 123 18: e426– 579. [DOI] [PubMed] [Google Scholar]
- 2. Bakshi TK, Choo MK, Edwards CC, Scott AG, Hart HH, Armstrong GP.. Causes of elevated troponin I with a normal coronary angiogram. Intern Med J 2002; 32 11: 520– 5. [DOI] [PubMed] [Google Scholar]
- 3. Jeremias A, Gibson CM.. Narrative review: alternative causes for elevated cardiac troponin levels when acute coronary syndromes are excluded. Ann Intern Med 2005; 142 9: 786– 91. [DOI] [PubMed] [Google Scholar]
- 4. Ammann P, Fehr T, Minder EI, Gunter C, Bertel O.. Elevation of troponin I in sepsis and septic shock. Intensive Care Med 2001; 27 6: 965– 9. [DOI] [PubMed] [Google Scholar]
- 5. Davoodi G, Mohammadi V, Shafiee A, Kazemisaeid A, Sadeghian S, Vasheghani-Farahani A, Yaminisharif A.. Detection of myocardial injury due to defibrillation threshold checking after insertion of implantable cardioverter/defibrillators. Acta Cardiol 2013; 68 2: 167– 72. [DOI] [PubMed] [Google Scholar]
- 6. Thygesen K, Alpert JS, White HD.. Universal definition of myocardial infarction. J Am Coll Cardiol 2007; 50 22: 2173– 95. [DOI] [PubMed] [Google Scholar]
- 7. Zellweger MJ, Schaer BA, Cron TA, Pfisterer ME, Osswald S.. Elevated troponin levels in absence of coronary artery disease after supraventricular tachycardia. Swiss Med Wkly 2003; 133 31–32: 439– 41. [DOI] [PubMed] [Google Scholar]
- 8. Ben Yedder N, Roux JF, Paredes FA.. Troponin elevation in supraventricular tachycardia: primary dependence on heart rate. Can J Cardiol 2011; 27 1: 105– 9. [DOI] [PubMed] [Google Scholar]
- 9. Giannitsis E, Kurz K, Hallermayer K, Jarausch J, Jaffe AS, Katus HA.. Analytical validation of a high-sensitivity cardiac troponin T assay. Clin Chem 2010; 56 2: 254– 61. [DOI] [PubMed] [Google Scholar]
- 10. Alpert JS, Thygesen K, Antman E, Bassand JP.. Myocardial infarction redefined--a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction [published erratum appears in J Am Coll Cardiol 2001;37(3): 973]. J Am Coll Cardiol 2000; 36 3: 959– 69. [DOI] [PubMed] [Google Scholar]
- 11. Wu AH, Bolger AF, Hollander JE.. Growing pains with the use of high-sensitivity cardiac troponin assays. J Am Coll Cardiol 2013; 62 14: 1250– 1. [DOI] [PubMed] [Google Scholar]
- 12. Jenab Y, Ghaffari-Marandi N.. Changes of high-sensitive troponin level in a patient with paroxysmal supraventricular tachycardia. Anadolu Kardiyol Derg 2012; 12 1: 77– 8. [DOI] [PubMed] [Google Scholar]
- 13. Kanjwal K, Imran N, Grubb B, Kanjwal Y.. Troponin elevation in patients with various tachycardias and normal epicardial coronaries. Indian Pacing Electrophysiol J 2008; 8 3: 172– 4. [PMC free article] [PubMed] [Google Scholar]
- 14. Schueler M, Vafaie M, Becker R, Biener M, Thomas D, Mueller M, . et al. Prevalence, kinetic changes and possible reasons of elevated cardiac troponin T in patients with AV nodal reentrant tachycardia. Acute Card Care 2012; 14 4: 131– 7. [DOI] [PubMed] [Google Scholar]
- 15. Thygesen K, Mair J, Katus H, Plebani M, Venge P, Collinson P, . et al. Recommendations for the use of cardiac troponin measurement in acute cardiac care. Eur Heart J 2010; 31 18: 2197– 204. [DOI] [PubMed] [Google Scholar]
- 16. Remppis A, Scheffold T, Greten J, Haass M, Greten T, Kubler W, Katus HA.. Intracellular compartmentation of troponin T: release kinetics after global ischemia and calcium paradox in the isolated perfused rat heart. J Mol Cell Cardiol 1995; 27 2: 793– 803. [DOI] [PubMed] [Google Scholar]
- 17. Antman EM. Decision making with cardiac troponin tests. N Engl J Med 2002; 346 26: 2079– 82. [DOI] [PubMed] [Google Scholar]
- 18. Chow GV, Hirsch GA, Spragg DD, Cai JX, Cheng A, Ziegelstein RC, Marine JE.. Prognostic significance of cardiac troponin I levels in hospitalized patients presenting with supraventricular tachycardia. Medicine (Baltimore) 2010; 89 3: 141– 8. [DOI] [PubMed] [Google Scholar]
- 19. Hessel MH, Atsma DE, van der Valk EJ, Bax WH, Schalij MJ, van der Laarse A.. Release of cardiac troponin I from viable cardiomyocytes is mediated by integrin stimulation. Pflugers Arch 2008; 455 6: 979– 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hickman PE, Potter JM, Aroney C, Koerbin G, Southcott E, Wu AH, Roberts MS.. Cardiac troponin may be released by ischemia alone, without necrosis. Clin Chim Acta 2010; 411 5–6: 318– 23. [DOI] [PubMed] [Google Scholar]


