When transcatheter aortic valve replacement (TAVR) emerged as an alternative to surgical aortic valve replacement (SAVR) in high-risk patients with aortic stenosis, differential outcomes in various patient subgroups became a topic of interest. The Partner Trial investigators first shed light on this issue with their publication of one-year outcomes, including subgroup analysis that showed improved survival rates in women after TAVR.1 Subsequently, multiple investigators have sought to define gender disparities in patients undergoing TAVR (Table I).2–7
TABLE I.
Studies of Transcatheter Aortic Valve Replacement in Women
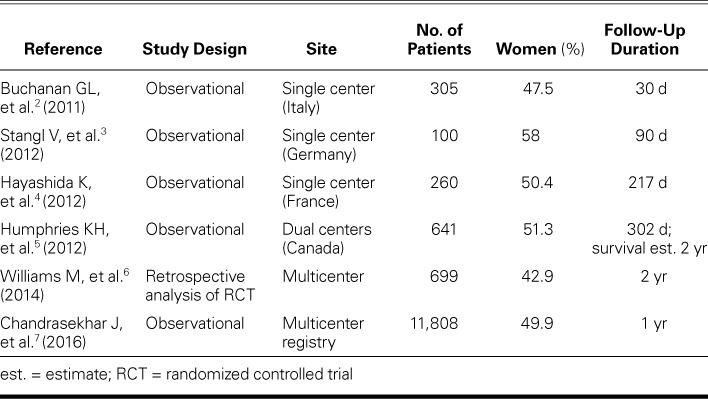
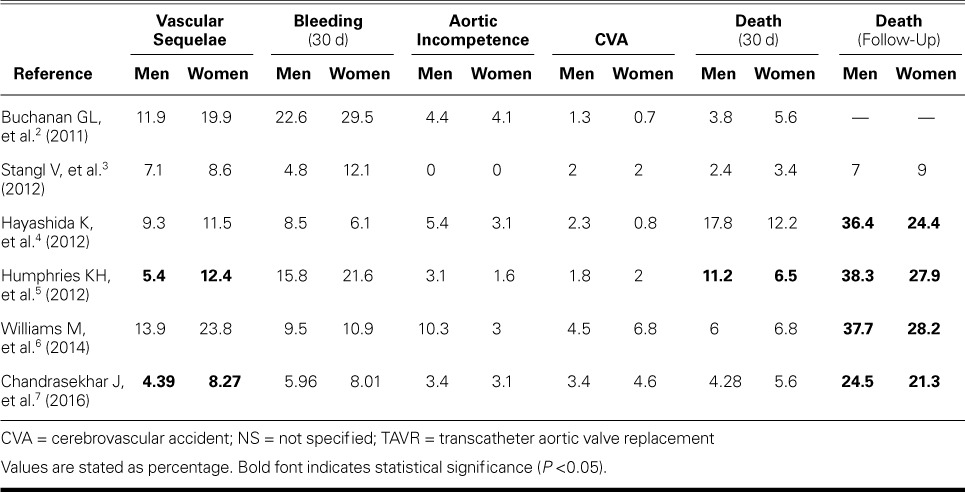
Early studies were predominantly single-center, real-world observational studies with relatively small sample sizes; nonetheless, some similar findings emerged. In terms of preoperative characteristics, female patients tended to have smaller body surface areas, smaller aortic annular diameters, and higher left ventricular ejection fractions (LVEF) (Table II).2–5 On the other hand, the prevalence of diabetes mellitus, coronary artery disease and prior revascularization, smoking, and peripheral vascular disease was higher in men. Procedural differences were most notable for smaller valve sizes in women (Table III).2–6 In regard to outcomes, the investigators consistently identified a trend toward higher rates of vascular sequelae and bleeding among women who underwent TAVR (Table IV).2–6 In the largest of these institutional experiences, Humphries and colleagues5 reported significantly lower mortality rates in women than in men (median follow-up duration, 302 d; estimated 2-yr survival rate, 38.3% vs 27.9%; P=0.007).
TABLE II.
Demographic Characteristics in the TAVR Studies
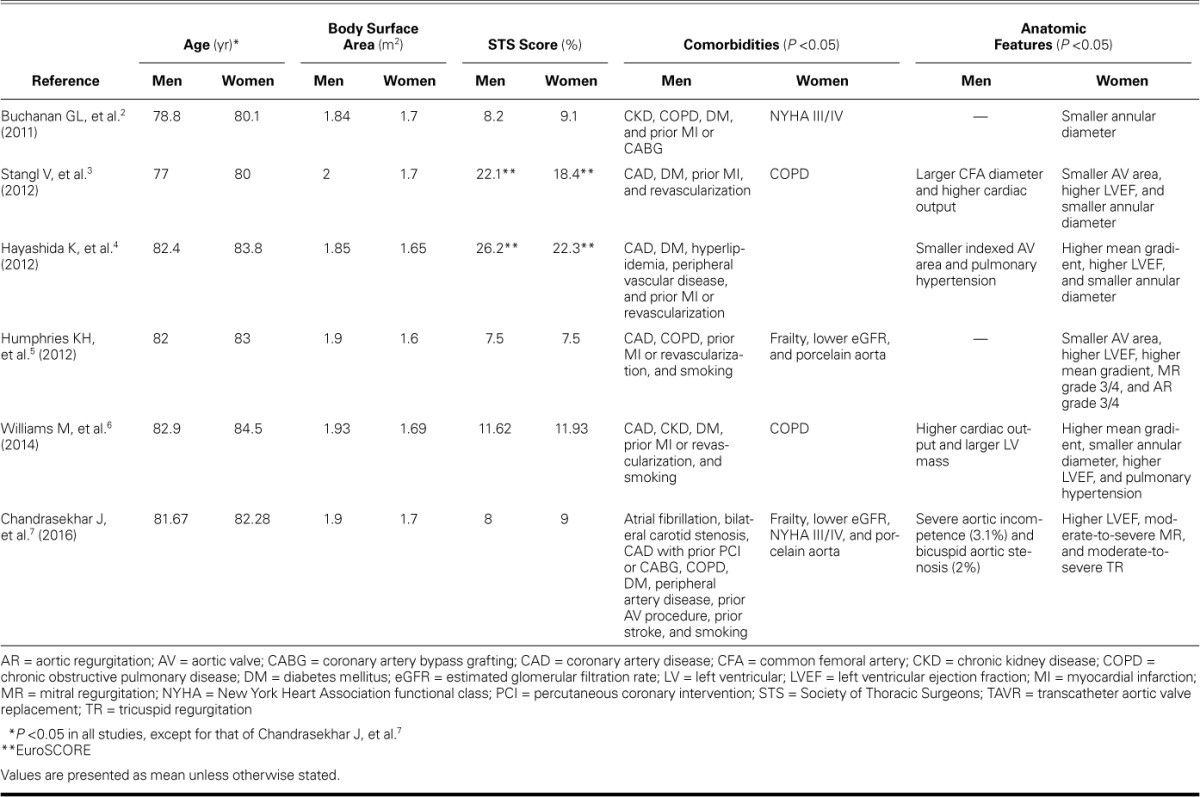
TABLE III.
Procedural Details in the TAVR Studies
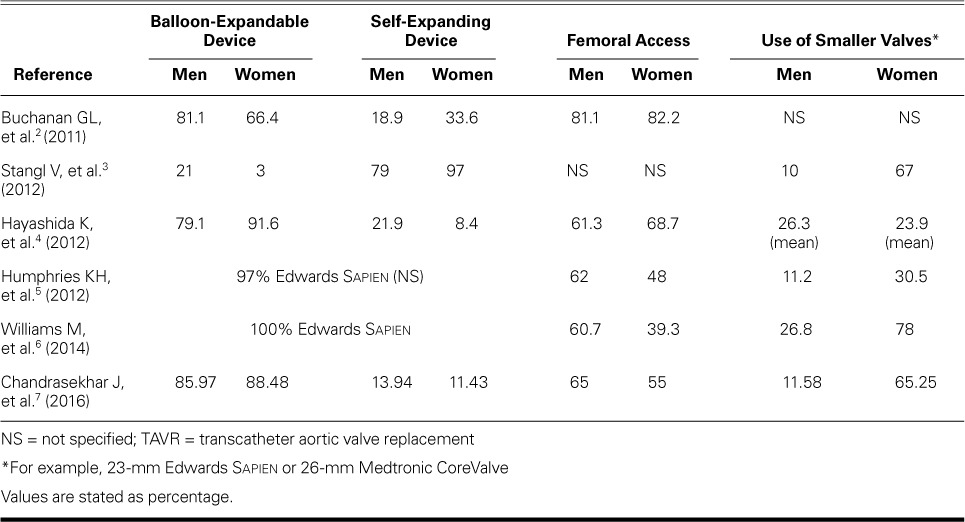
TABLE IV.
Outcomes in the TAVR Studies
Subsequently, the Partner Trial investigators6 published more robust insights related to the impact of female sex in patients undergoing TAVR versus SAVR. The Partner 1A investigators randomized 699 patients to TAVR or SAVR and included female sex as one of several predefined subgroups. Among enrolled patients, men were more likely to have coronary artery disease, peripheral vascular disease, a current or prior smoking history, diabetes mellitus, and chronic kidney disease. Women, however, were older and more likely to have a lower Society of Thoracic Surgeons score, a smaller body surface area, and chronic obstructive pulmonary disease. Men had higher cardiac output and greater left ventricular mass, whereas women had higher LVEF, higher mean gradients, and smaller aortic annular diameters. Women more frequently underwent nontransfemoral access and were given smaller prosthetic valves.
In terms of outcomes, women had a higher incidence of vascular sequelae and cerebrovascular accidents (CVA). The 30-day mortality rate was not significantly different between men and women. At 2 years, however, mortality rates improved among women. Of note, men assigned to SAVR had survival rates similar to those of men who underwent TAVR, and better survival rates than women who underwent SAVR. Meanwhile, women who underwent TAVR (in particular, via the transfemoral approach) had a survival benefit in comparison with those who had surgery. Although the superior long-term survival rate in women might be related to fewer baseline comorbidities, other findings are less clear. For instance, the higher incidence of CVA in women despite the lower incidence of baseline cerebrovascular disease in this group is not intuitively explainable.
Despite their important findings, the aforementioned studies are limited by confounding baseline demographic and anatomic differences. Chandrasekhar and colleagues7 analyzed the Transcatheter Valve Therapy registry, which includes all patients who have undergone commercial TAVR in the United States. The authors reviewed data on 11,808 patients, with outcomes adjusted for various potential confounders. Table II shows the baseline demographic, clinical, and anatomic differences among men and women.7 Women were more likely to undergo nontransfemoral access during TAVR and to need smaller valves. In-hospital vascular sequelae were significantly higher in women, who also showed a trend toward more bleeding events. Although the 30-day mortality rate was no different among men and women, women had higher survival rates at one year.
The body of evidence illustrates that men and women undergoing TAVR have unique demographic, comorbid, and anatomic characteristics that influence their procedural and long-term outcomes. The finding by the Partner Trial investigators that survival rates after TAVR were superior in women, despite an increased incidence of vascular sequelae and CVA, is now supported by large-registry data with statistical correction for potentially confounding factors. It is important to note that the cited studies included patients who were treated with predominantly early-generation TAVR devices. More recent advances with smaller-profile devices are likely to lower the incidence of vascular sequelae and the need for nontransfemoral access. These advances can be expected to expand the already evident advantage of TAVR over SAVR in women.
Further studies are needed to evaluate whether sex differences remain relevant in the current state of TAVR, which includes smaller-profile devices, patients typically at lower risk, broader valve indications, and an emphasis on minimally invasive approaches. In addition, the development of a preoperative risk calculator unique to female patients might lead to more accurate outcome predictions in this group.
References
- 1. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, . et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011; 364 23: 2187– 98. [DOI] [PubMed] [Google Scholar]
- 2. Buchanan GL, Chieffo A, Montorfano M, Maisano F, Latib A, Godino C, . et al. The role of sex on VARC outcomes following transcatheter aortic valve implantation with both Edwards SAPIEN™ and Medtronic CoreValve ReValving System® devices: the Milan registry. EuroIntervention 2011; 7 5: 556– 63. [DOI] [PubMed] [Google Scholar]
- 3. Stangl V, Baldenhofer G, Knebel F, Zhang K, Sanad W, Spethmann S, . et al. Impact of gender on three-month outcome and left ventricular remodeling after transfemoral transcatheter aortic valve implantation. Am J Cardiol 2012; 110 6: 884– 90. [DOI] [PubMed] [Google Scholar]
- 4. Hayashida K, Morice MC, Chevalier B, Hovasse T, Romano M, Garot P, . et al. Sex-related differences in clinical presentation and outcome of transcatheter aortic valve implantation for severe aortic stenosis. J Am Coll Cardiol 2012; 59 6: 566– 71. [DOI] [PubMed] [Google Scholar]
- 5. Humphries KH, Toggweiler S, Rodes-Cabau J, Nombela-Franco L, Dumont E, Wood DA, . et al. Sex differences in mortality after transcatheter aortic valve replacement for severe aortic stenosis. J Am Coll Cardiol 2012; 60 10: 882– 6. [DOI] [PubMed] [Google Scholar]
- 6. Williams M, Kodali SK, Hahn RT, Humphries KH, Nkomo VT, Cohen DJ, . et al. Sex-related differences in outcomes after transcatheter or surgical aortic valve replacement in patients with severe aortic stenosis: insights from the PARTNER trial (Placement of Aortic Transcatheter Valve). J Am Coll Cardiol 2014; 63 15: 1522– 8. [DOI] [PubMed] [Google Scholar]
- 7. Chandrasekhar J, Dangas G, Yu J, Vemulapalli S, Suchindran S, Vora AN, . et al. Sex-based differences in outcomes with transcatheter aortic valve therapy: TVT registry from 2011 to 2014. J Am Coll Cardiol 2016; 68 25: 2733– 44. [DOI] [PubMed] [Google Scholar]


