Abstract
Negative pressure wound therapy (NPWT) is a method for treating wound. However, there are no case reports using NPWT for treating congestion after arterialized venous flap. Therefore, this study reported favorable outcomes after using a single-use NPWT system for managing congestion. A 39-year-old man had his index finger caught by a press machine. The finger had a soft tissue defect at the ventral part. An arterialized venous flap taken from the right forearm was transplanted. Perfusion of the flap was favorable, but on postoperative day 5, congestion and the edema of the flap were found. Then, NPWT was initiated. The congestion and edema in the flap were improved without complications such as flap necrosis and wound infection. At 4 months postoperatively, the morphology of the finger was favorable. In this study, NPWT was speculated to force the deeper blood vessels within the flap to dilate with inducing drainage and the simultaneous reduction in excess blood flow to the cortical layer, resulting in the improvement of congestion. Negative pressure wound therapy was used for treating congestion after the transplantation of arterialized venous flap, and the wound was favorably managed.
Keywords: Soft tissue defect, the open fracture of the index finger, single-use, arterialized venous flap, NPWT, PICO
Introduction
Negative pressure wound therapy (NPWT) is a therapeutic method for treating wound reported by Argenta and Morykwas.1 Although its usefulness is already reported in several clinical studies and in basic research,2,3 most of the applications are limited only in extensive skin ulcers, and the applications for several joints and small areas, such as the fingers, are currently known to be difficult.4,5
Meanwhile, the effectiveness of arterialized venous flaps for treating finger trauma is known.6 However, these flaps sometimes give severe congestion such as bullae formation, severe postoperative swelling, and partial necrosis.7 There is no case report using NPWT for treating the congestion of an arterialized venous flap continuously from the early stages of surgery over an extended period of time.
This study used an arterialized venous flap for treating a soft tissue defect of the index finger of which middle phalanx was fractured externally. This report described the favorable outcomes after the treatment with a single-use NPWT system (PICO; Smith & Nephew, London, UK) for managing congestion. This study was performed with respect to high ethical standards and approved, when required, by the appropriate ethics committee. This study, therefore, was conducted in accordance with the World Medical Association Declaration of Helsinki (June 1964) and subsequent amendments. The patients voluntarily gave written informed consent to participate in this study.
Case Presentations
A 39-year-old man had his index finger caught by a press machine. He had the following injuries: an open fracture of the middle phalanx of the index finger, extensor tendon rupture, and a high-grade crush injury (Figure 1). During emergency surgery on the day of injury, Kirschner wires were used for fixing the fractured bones, and the extensor tendons were sutured. The finger had a soft tissue defect at the ventral to lateral part on the distal interphalangeal (DIP) joint due to the crush injury with exposing the middle phalanx. Because the unfavorable engraftment of the skin graft was expected, an arterialized venous flap from the right forearm was transplanted (Figure 2). A flap of 3 cm × 3 cm in size with 1 efferent vein and 2 afferent veins was taken, transferred to the defect of the index finger, and sutured loosely. The afferent vein of the flap was anastomosed to the radial digital artery of the index finger. One of the 2 efferent veins was anastomosed to the radial digital artery, and the other was anastomosed proximally to the cutaneous vein in the ventral part of the finger.
Figure 1.

The ventral part of the finger and X-ray image of the index finger at the time of injury. (A) Soft tissue defect was observed on the ventral part of the index finger that was pinned for fixing the open fracture of the middle phalanx. (B) X-ray image showed the fracture of the middle phalanx of the index finger.
Figure 2.
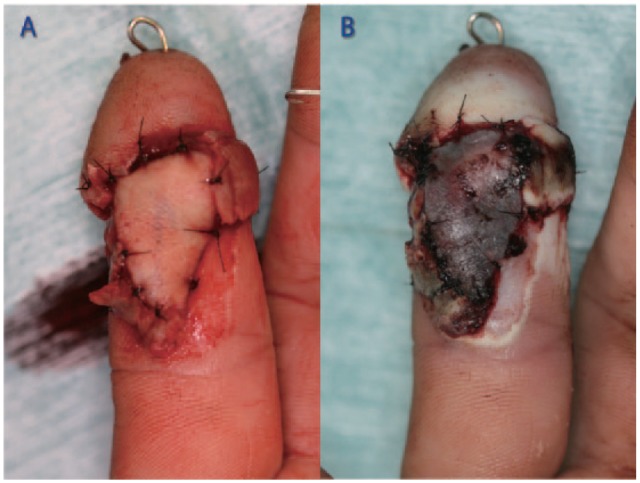
Intraoperative and postoperative views of the wound site of the index finger. (A) Photograph showed the intraoperative views of the wound after arterialized venous flaps transplant. (B) On postoperative day 5, the congestion of the flap on the wound was observed.
Although the perfusion of the flap was favorable, congestion and edema in the flap were observed on postoperative day 5 (Figure 2B). Therefore, a single-use NPWT system was initiated for improving the problems. First, the sufficient amount of no-sting barrier film (SECURA; Smith & Nephew) was applied for increasing the adhesion between the skin and the dressing (Figure 3A). Then, the barrier-film–covered finger was covered with the dressing in a spiral shape for allowing the aspiration port to appear at the dorsum of the hand. As a result, the dressing covered the whole index finger including the arterialized venous flap on DIP joint except fingertip. A gel seal (Renasys Adhesive Gel Patch; Smith & Nephew) was applied around the dressing (Figure 3B). Finally, a drape was applied (Figure 3C and D). This device delivered NPWT at a single preset pressure of −80 mm Hg. Negative pressure wound therapy dressing was exchanged twice a week by the same procedure for 3 weeks at the outpatient department, and the bullae formation, swelling, and the deep purple color of the flap due to congestion in the flap were found to be improved. Although only epidermal necrosis was found at the peripheral part of the flap, nearly all flaps were confirmed to be salvaged on the exchange of NPWT. After the application of NPWT dressing was completed, the wound was treated conservatively with vaseline ointment and a nonadherent pad (Derma Aid; ALCARE, Tokyo, Japan). As a result, the wound epithelialized in 2 months, and no complications, such as wound infection, were observed in the flap.
Figure 3.

Application procedure of PICO dressing. (A) Before the application of PICO dressing, the sufficient amount of no-sting barrier film (SECURA) was applied to the around the wound. (B) Gel sealer was applied to the middle part of the finger. (C) Photograph showed the dorsum of the hand after PICO dressing application. The aspiration port with drain tube was placed on the dorsum of the hand. (D) Photograph showed the palmar side of the hand after PICO dressing application.
At 4 months postoperatively, although mild atrophy that was one of common complications with arterialized venous flap was noted,8 the morphology of the finger was favorable (Figure 4A). Satisfactory synostosis was also observed radiographically. Although a little weakness in DIP joint movement with a percent total active motion of 61% was found, no limitations in the extension of each joint was noted, resulting in no inconvenience in daily life (Figure 4B).
Figure 4.
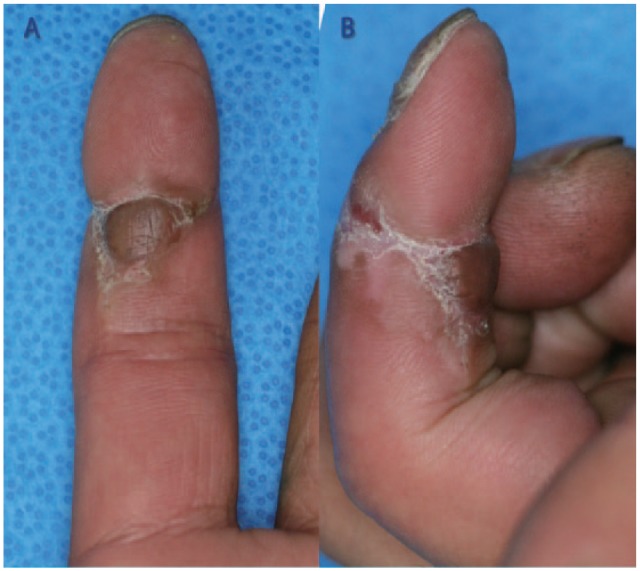
The wound at 4 months after surgery. (A) The ventral part of the finger. At 4 months postoperatively, although mild atrophy was found in the arterialized venous flap, the morphology was favorable. (B) The maximum flexion position of the finger. At 4 months postoperatively, although a little weakness was observed in distal interphalangeal joint movement with a percent total active motion of 61%, there was no inconvenience in daily life.
Discussion
Uygur et al9 and Qui et al10 used NPWT for treating congestion after free flap transplants and reported the improvement of congestion. Nelson et al11 also used NPWT after free flap transplants and reported a good contour morphology in addition to the improvement of flap edema, and the flap morphology is also satisfactory in that case after an extended course. In this study, NPWT was effective not only for treating the physiological congestion after arterialized venous flap transplants but also for providing an aesthetic satisfaction to the patients. Malmsjo et al investigated wound perfusion with NPWT and reported (1) the expansion of the deep tissues after the application of negative pressure to wound defects and (2) the dilation of the deeper vessels with increasing perfusion. They also reported the reduced perfusion of the cortical layer during wound suturing by the compressive force of the coating material.12 Malsiner et al13 reported that immunohistochemical analysis found an increase in the number of vessels treated by NPWT increase in chronic wound. In this study, the number of vessels in wound bed also increased by NPWT, and in addition, NPWT was speculated to allow the deeper blood vessels within the flap to dilate with inducing drainage and the simultaneous reduction in excess blood flow to the cortical layer, resulting in the improvement of congestion. Although only one case could be a weak point in this study, time to improve congestion and the severity of necrosis without NPWT were speculated be longer and higher than those fingers treated with NPWT, respectively. Kairinos performed NPWT in poorly perfused tissues and reported that (1) the tissue pressure in the surrounding tissues increased, (2) the capillaries are compressed, and (3) the perfusion could decrease.14 In this study, blood flow from afferent vein was speculated to decrease because of the reasons described in (2) and (3), and blood flow from efferent vein increased because of the reason described in (1). This study performed the revascularization of wound with the flap and improved the perfusion of surrounding tissues, and no decrease in perfusion to the extent was speculated to be observed, resulting in no severe necrosis at the flap or surrounding tissues with the use of NPWT. However, the effects of NPWT on the site of blood vessel anastomosis were unclear, and the application and timing of the use of NPWT after skin flap transplant are to be carefully investigated. Malmsjo et al12 previously compared conventional NPWT with foam to that with PICO dressings and reported no significant difference in their effectiveness for treating full-thickness skin defects and suture wounds. PICO was thought to be effective for treating a site, such as the fingers, which was difficult to perform conventional NPWT, and this device could allow patients to receive their treatments at the outpatients department.
On the use of PICO on the fingers, the following leak factors were expected: (1) the application site has several joints and a complex spatial construction, (2) there are many lines at the palms and ventral part of the fingers, and (3) the size of dressing is larger than the surface area of the wound. Fujitani et al5 used a surgical glove to prevent air leaks. For solving these issues, this study could make the following remarks on the use of NPWT device: (1) the dressing should be minimized for fitting the wound area, (2) the sufficient amount of no-sting barrier film (SECURA) should be applied for increasing the adhesiveness between the skin and the dressing, (3) the dressing should be applied to the finger in a spiral shape for allowing the aspiration port to appear at the dorsum of the hand and to avoid reaching the palmar area, (4) gel seal (Renasys Adhesive Gel Patch) should be applied to possible leaking sites followed by the application of dressing, and (5) the surroundings of the dressing should be covered with an all-cotton elastic bandage (Elascot; ALCARE) with applying light compression. Although the patient underwent rehabilitation immediately after surgery, the procedures described above allowed PICO dressing to be used without leak problems that was well tolerated during wound healing induced by NPWT. This procedure also can be applied to the fixation of the skin graft for hand injury requiring rehabilitation. In the future, the authors would accumulate cases and investigate the effects NPWT with PICO on perfusion within arterialized venous flaps. Also, the authors would compare the degrees of congestion, cosmetic, and treatment period without NPWT.
Conclusions
Negative pressure wound therapy was used to treat congestion after the transplantation of an arterialized venous flap, and the wound could be favorably managed. In addition, this NPWT device was easily used for the finger, which is known to be difficult to perform conventional NPWT with dressing.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: YN and MT conceived and designed the experiments. YN, SM, and MT analyzed and collected the data. SM and MT agree with manuscript results and conclusions. MT made critical revisions and approved final version. All authors reviewed and approved the final manuscript.
References
- 1. Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38:563–576. [PubMed] [Google Scholar]
- 2. Armstrong DG, Lavery LA, Consortium DFS. Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomised controlled trial. Lancet. 2005;366:1704–1710. [DOI] [PubMed] [Google Scholar]
- 3. Isago T, Nozaki M, Kikuchi Y, Honda T, Nakazawa H. Effects of different negative pressures on reduction of wounds in negative pressure dressings. J Dermatol. 2003;30:596–601. [DOI] [PubMed] [Google Scholar]
- 4. Herscovici D, Sanders RW, Scaduto JM, Infante A, DiPasquale T. Vacuum-assisted wound closure (VAC therapy) for the management of patients with high-energy soft tissue injuries. J Orthop Trauma. 2003;17:683–688. [DOI] [PubMed] [Google Scholar]
- 5. Fujitani T, Zenke Y, Shinone M, Menuki K, Fukumoto K, Sakai A. Negative pressure wound therapy with surgical gloves to repair soft tissue defects in hands. J UOEH. 2015;37:185–190. [DOI] [PubMed] [Google Scholar]
- 6. Takeuchi M, Sakurai H, Sasaki K, Nozaki M. Treatment of finger avulsion injuries with innervated arterialized venous flaps. Plast Reconstr Surg. 2000;106:881–885. [DOI] [PubMed] [Google Scholar]
- 7. Woo SH, Kim SE, Lee TH, Jeong JH, Seul JH. Effects of blood flow and venous network on the survival of the arterialized venous flap. Plast Reconstr Surg. 1998;101:1280–1289. [DOI] [PubMed] [Google Scholar]
- 8. Iglesias M, Fonseca-Lazcano JA, Moran MA, Butron P, Diaz-Morales M. Revascularization of arterialized venous flaps through a total retrograde reverse blood flow: randomized experimental trial of viability. Plast Reconstr Surg Glob Open. 2013;1:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Uygur F, Duman H, Ulkür E, Ceiköz B. The role of the vacuum-assisted closure therapy in the salvage of venous congestion of the free flap: case report. Int Wound J. 2008;5:50–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Qiu SS, Hsu CC, Hanna SA, et al. Negative pressure wound therapy for the management of flaps with venous congestion. Microsurgery. 2016;36:467–473. [DOI] [PubMed] [Google Scholar]
- 11. Nelson JA, Kim EM, Serletti JM, Wu LC. A novel technique for lower extremity limb salvage: the vastus lateralis muscle flap with concurrent use of the vacuum-assisted closure device. J Reconstr Microsurg. 2010;26:427–431. [DOI] [PubMed] [Google Scholar]
- 12. Malmsjö M, Ingemansson R. Effects of green foam, black foam and gauze on contraction, blood flow and pressure delivery to the wound bed in negative pressure wound therapy. J Plast Reconstr Aesthet Surg. 2011;64:e289–e296. [DOI] [PubMed] [Google Scholar]
- 13. Malsiner CC, Schmitz M, Horch RE, Keller AK, Leffler M. Vessel transformation in chronic wounds under topical negative pressure therapy: an immunohistochemical analysis. Int Wound J. 2015;12:501–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kairinos N, Voogd AM, Botha PH, et al. Negative-pressure wound therapy II: negative-pressure wound therapy and increased perfusion. Just an illusion? Plast Reconstr Surg. 2009;123:601–612. [DOI] [PubMed] [Google Scholar]


