Abstract
Takotsubo cardiomyopathy is a transient apical ballooning of the left ventricle typically with electrocardiographic changes and enzyme release without evidence of obstructive coronary artery disease. It typically occurs in postmenopausal women and may have a predilection for patients with anxiety disorders. The following is a case in which we believe takotsubo cardiomyopathy was induced by the tapering of antianxiety medications. We feel that health care professionals should be aware of this possibility in such a patient population especially when they have demonstrated cardiovascular symptomatology.
Keywords: Takotsubo cardiomyopathy, anxiolytic, tapering
Case
The patient was a 67-year-old white woman with a past medical history of hypertension, undefined anxiety disorder, major depression, cerebral aneurysm surgery, tonsillectomy, cholecystectomy, and a right bundle branch block (RBBB). She had a history of chest pain followed up with a myocardial perfusion studying that was determined as normal.
She has allergies to bupropion and tape. Her current medications included valsartan 80 mg/d, metoprolol 25 mg/d, simvastatin 20 mg/d, fluoxetine 20 mg/d, imipramine 50 mg/d, solifenacin 5 mg/d, aripiprazole 2 mg/d, clonazepam 0.5 mg/d, and nabumetone 500 mg as needed.
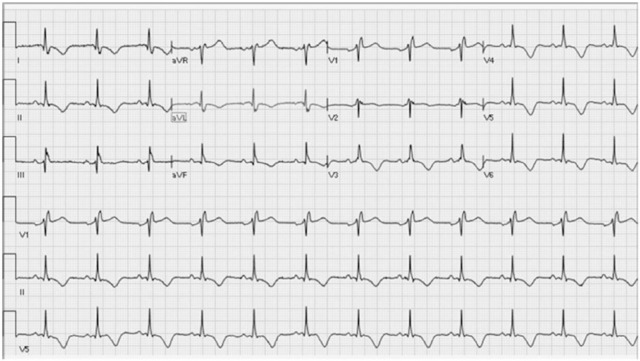
She initially presented with an electrocardiogram demonstrating junctional rhythms for which we discontinued her metoprolol. Subsequent Holter monitoring was performed which revealed sinus rhythm with episodes of junctional rhythm and several sinus pauses of 3.6 seconds. Some reports suggest that rhythm disturbances may be attributable to medications such as clonazepam and fluoxetine.1,2 After consulting with her psychiatrist, it was felt that we could attempt to taper some of her medications because her mood had been stable for an extended period of time. Within 3 days of decreasing dosages of clonazepam and fluoxetine, she presented to the hospital with substernal chest pressure, a RBBB with T-wave inversions (Figure 1), as well as a peak troponin release (1.24 ng/mL, normal 0-0.5; peak creatine kinase MB of 15.2 ng/mL, normal 0-5; and B-type natriuretic peptide of 3028 pg/mL, normal 0-99) consistent with myocardial infarction and left ventricular dysfunction. An echo was performed which revealed anterior apical hypokinesia with an ejection fraction of 40% (Figure 2). A coronary catheterization was also performed which demonstrated normal coronaries (Figure 3). A repeat echo was ordered several weeks later and yielded normal wall motion and ejection fraction. Several weeks later, there was also resolution of the T-wave changes. Although cardiac magnetic resonance imaging was not performed to further support the diagnosis of takotsubo cardiomyopathy, we feel that this case meets the proposed Mayo criteria for takotsubo cardiomyopathy which includes the absence of a myocarditis or pheochromocytoma, transient apical hypokinesia, normal coronaries, new T-wave changes, and elevated biomarkers.3 The patient’s medications were reinitiated and a dual chamber pacemaker was implanted.
Figure 1.
Initial electrocardiogram with a right bundle branch block and diffuse T-wave inversions.
Figure 2.
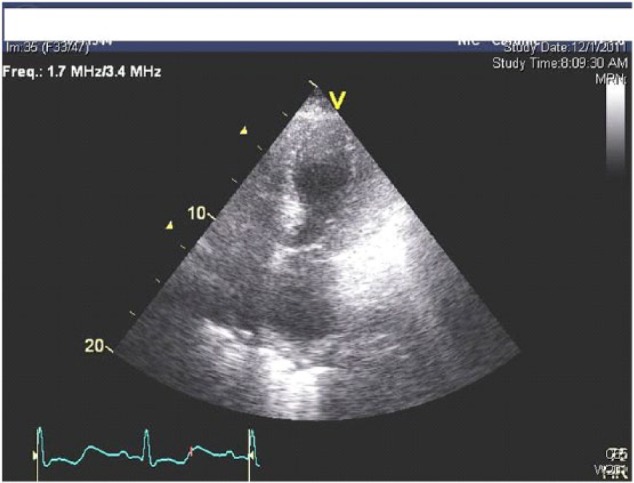
Echocardiogram, in systole, demonstrating apical hypokinesia in an apical 4-chamber view.
Figure 3.
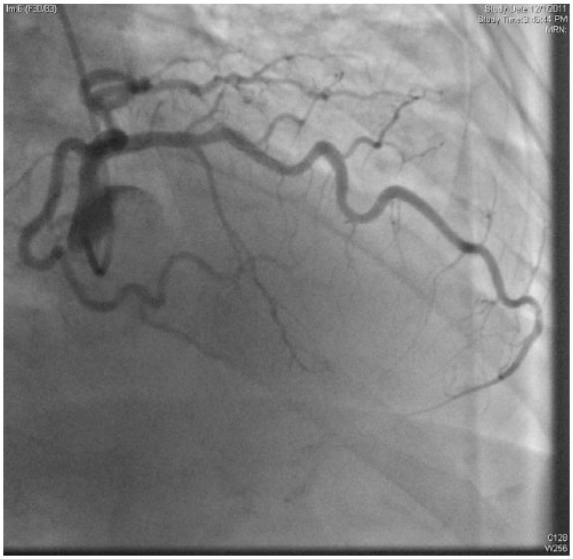
Coronary angiogram, in an RAO (right anterior oblique) projection, demonstrating a normal left anterior descending artery.
Discussion
Takotsubo cardiomyopathy is rare disorder believed to be stress induced for which the cause is not completely clear. Several theories include coronary spasm, catecholamine toxicity, apical myocardial sensitivity, microvascular dysfunction, and metabolic abnormalities.4 Literature shows that anxiodepressive disorders and chronic psychological stress are common in patients with takotsubo cardiomyopathy.5 Other case reports also relate takotsubo cardiomyopathy to the exacerbation of psychiatric illnesses.6 Studies have also documented the phenomenon of takotsubo cardiomyopathy after electroconvulsive therapy.7,8 Given a reported recurrence rate of takotsubo cardiomyopathy of 10%, literature suggests that symptoms may resolve when stress-related symptoms subside and reappear when they are present.9 Recent literature also shows that preexisting psychiatric illness is associated with recurrence of takotsubo cardiomyopathy.10
This patient had history of anxiodepressive disorder with prior chest pains and developed signs and symptoms when she began tapering her medication which meets the criteria for stress-induced takotsubo cardiomyopathy. The tapering of her anxiodepressive medication may have triggered an episode of takotsubo cardiomyopathy. We feel that it is important to be more cognizant of medication discontinuation and changes in patients with anxiodepressive disorders and a history of prior cardiac symptomatology. This case may also suggest that anxiolytic medication could play a therapeutic role in treatment and prevention of takotsubo cardiomyopathy. This may be especially true in patients with anxiodepressive disorders with recurrences. Given the prevalence of takotsubo cardiomyopathy, and the known risk factors, providers should remain vigilant for this condition in appropriate populations who show classic symptoms. Literature remains unclear whether high-risk populations entail simply the prototypical patient (ie, postmenopausal women) or whether all patients weaning off sedative hypnotics should be considered as high-risk populations. Further research is needed to further detail high-risk patient populations and risk factors for takotsubo cardiomyopathy. In addition, given the extensive literature on possible causes of takotsubo cardiomyopathy listed above, and recent literature showing that serotonin levels are found to be higher during an acute episode of the condition, further research should also focus on this physiology as a possible way to monitor for or treat the condition.11 In conclusion, we believe this condition is important, deserving of provider recognition and further scientific inquiry.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: CL, KL, PO: Data collection and manuscript writing. TB, AA: Critical revisions and draft approval. FD & DM: Critical revisions, guidance, and final draft approval.
Informed Consent: The authors provided and received informed consent from the patient for the writing and reproduction of this case report.
References
- 1. Ellison JM, Milofsky JE, Ely E. Fluoxetine-induced bradycardia and syncope in two patients. J Clin Psychiatry. 1990;51:385–386. [PubMed] [Google Scholar]
- 2. Arroyo Plasencia AM, Ballentine LM, Mowry JB, Kao LW. Benzodiazepine-associated atrioventricular block. Am J Ther. 2012;19:e48–e52. [DOI] [PubMed] [Google Scholar]
- 3. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–417. [DOI] [PubMed] [Google Scholar]
- 4. Koulouris S, Pastromas S, Sakellariou D, Kratimenos T, Piperopoulos P, Manolis AS. Takotsubo cardiomyopathy: the “broken heart” syndrome. Hellenic J Cardiol. 2010;51:451–457. [PubMed] [Google Scholar]
- 5. Delmas C, Lairez O, Mulin E, et al. Anxiodepressive disorders and chronic psychological stress are associated with Tako-Tsubo cardiomyopathy—new physiopathological hypothesis. Circ J. 2013;77:175–180. [DOI] [PubMed] [Google Scholar]
- 6. Corrigan FE, Kimmel MC, Jayaram G. Four cases of takotsubo cardiomyopathy linked with exacerbations of psychiatric illness. Innov Clin Neurosci. 2011;8:50–53. [PMC free article] [PubMed] [Google Scholar]
- 7. Narayanan A, Russell MD, Sundararaman S, Shankar KK, Artman B. Takotsubo cardiomyopathy following electroconvulsive therapy: an increasingly recognised phenomenon. BMJ Case Rep. 2014;2014: bcr2014206816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grubisha M, Gopalan P, Azzam PN. Takotsubo cardiomyopathy in a young man after maintenance electroconvulsive therapy and clozapine initiation: a case report. J ECT. 2014;30:e40–e41. [DOI] [PubMed] [Google Scholar]
- 9. Elesber AA, Prasad A, Lennon RJ, Wright RS, Lerman A, Rihal CS. Four-year recurrence rate and prognosis of the apical ballooning syndrome. J Am Coll Cardiol. 2007;50:448–452. [DOI] [PubMed] [Google Scholar]
- 10. Nayeri A, Rafla-Yuan E, Farber-Eger E, et al. Pre-existing psychiatric illness is associated with increased risk of recurrent Takotsubo cardiomyopathy. Psychosomatics. 2017;58:527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rouzaud Laborde C, Delmas C, Mialet-Perez J, et al. First evidence of increased plasma serotonin levels in Tako-Tsubo cardiomyopathy. Biomed Res Int. 2013;2013:847069. [DOI] [PMC free article] [PubMed] [Google Scholar]