Abstract
Objective
The purpose of this pilot study was to evaluate the feasibility and efficacy of adding cryostimulation to manual therapy in patients with chronic lateral epicondylitis.
Methods
The control group (n = 19) was treated with manual therapy consisting of soft-tissue therapy and radial head mobilizations. The experimental group (n = 18) received cryostimulation in addition to manual therapy care similar to that for the control group. Both protocols consisted of 8 treatments over a 4-week period. Outcome measures included pain intensity (visual analog scale), pain-free grip strength (handheld dynamometer), and functional index (Patient-Rated Tennis Elbow Evaluation questionnaire). Assessments were performed at baseline, postintervention, and 3-month follow-up. Adherence and dropout rates were also considered.
Results
Both groups exhibited significant improvements in pain intensity and functional index at postintervention assessments, which were maintained at follow-up. All participants attended the prescribed number of treatments, but 27% were lost at follow-up. Minor adverse events were reported after cryostimulation in 4 cases.
Conclusions
This study indicated that it is feasible to complete a clinical trial evaluating the efficacy of adding cryostimulation to manual therapy in patients with chronic lateral epicondylitis. On the basis of these preliminary data, the combination of cryostimulation and manual therapy care did not provide any additional benefits in both the short term and the long term. Manual myofascial point treatment and mobilization techniques yielded positive outcomes in chronic lateral epicondylitis. Further studies should focus on the sole therapeutic effect of cryostimulation in both patients with acute and those with chronic conditions.
Key Indexing Terms: Tendinopathy, Elbow, Cryotherapy, Musculoskeletal Manipulation, Trigger Points
Introduction
Lateral epicondylitis (LE) is one of the most frequently encountered lesions affecting the upper extremity.1 It is defined as an injury involving the wrist common extensor tendons, particularly the extensor carpi radialis brevis and extensor digitorum.2 The clinical presentation involves a sensation of pain or burn over the humeral insertion of the common extensor tendons. This pain can be exacerbated by wrist extensor activation, passive wrist flexion combined with passive elbow extension,3 and palpation over the lateral epicondyle or the origin of the wrist extensor muscle group. Patients affected by LE will commonly present with a loss of grip strength4 and will usually report pain during daily activities such as grasping objects, turning doorknobs, and shaking hands.5
Lateral epicondylitis is a frequent complaint among musculoskeletal disorders affecting the upper extremities, with an annual prevalence of 1% to 3% in the active population.4 Sanders et al, in a 13-year epidemiological study, reported an overall annual age- and sex-adjusted incidence of 3.4/1000 for lateral elbow tendinosis.6 A peak incidence is observed between 35 and 54 years of age, affecting slightly more women than men and having a higher prevalence for the dominant side.6, 7, 8, 9 The high prevalence of LE leads to a significant socioeconomic burden. Taylor and Hanaffin recently reported that taken together, medial epicondylitis and LE accounted for 11.7% of work-related injury claims, with an average cost of $6593 US per claim in Washington State from 1987 to 1995.4 Similar costs have been reported by the Quebec Province Workers Board of Compensation for 2008, with 739 workers having received compensation for LE, averaging 87 days in length and $5860 CAN in cost.10, 11
Pain around the lateral epicondyle has been, over the years, referred to as tennis elbow, epicondylalgia, epicondylitis, and epicondylosis, reflecting the evolution in the understanding of the pathomechanical mechanisms underlying this lesion. The most common and plausible explanation for LE is now believed to be a degenerative process in which the tendons manifest abundant fibroblastic activity, vascular hyperplasia, and the presence of unstructured collagen fibers.3 Therefore, it is believed that the tendinopathy results from repetitive strains or overuse of the forearm-extensor tendons rather than from a single trauma.12, 13, 14
Among the factors contributing to the chronic nature of the condition, tasks requiring forceful and repetitive recruitment of the extensors of the forearm, repetitive wrist and elbow motions such as flexion and extension for more than 2 hours a day, and forceful gripping such as lifting heavy objects (≥20 kg) more than 10 times a day are brought forward by many researchers.1, 15, 16, 17
Lateral epicondylitis remains a challenging condition to manage considering its high rate of recurrence and episodes that can last from 6 months to 2 years.6, 8, 18 Many conservative treatments used alone or in combinations have been reported to have modest effects, but no single option seems to be clearly superior.13, 18, 19, 20 This may be due to the lack of a definite understanding or identification of a clear pathophysiological mechanism, the lack of good-quality studies, or the presence of many confounding factors influencing the treatment outcome.21, 22
Many systematic reviews assessing the effectiveness of treatment modalities used for LE report a lack of evidence favoring one specific treatment option over another.18, 23, 24 For instance, a review by Dingemanse et al investigating the effectiveness of electrical modalities in the treatment of LE included the following modalities: ultrasound, lasers, extracorporeal shock wave therapy, transcutaneous electrical nerve stimulation (TENS), and pulsed electromagnetic field.25 The authors concluded that moderate evidence exists for the effectiveness of ultrasound and laser therapy, whereas the evidence for other modalities was inconclusive or mixed.25 A careful review of original studies, however, indicated that when included, exercises, whether as add-ons or as a control group, contributed to enhance patients’ recovery. This finding seems to be in agreement with recent reviews1, 26 and an individual article27 on the effectiveness of exercises in the treatment of LE.
Studies looking at the outcome of manual therapy, including myofascial treatment and manual mobilizations of the elbow and wrist joint, present a different treatment centered on myofascial and articular lesions found in patients with LE. Ajimsha et al reported a positive effect on self-reported functional capacity after a 4-week treatment protocol. Positive outcomes were significant in both the short (4 weeks) and long (12 weeks) term.28 Manual mobilization of the elbow and wrist joints has also been studied.21 Many types of mobilization exist, and an extensive literature review by Herd and Meserve revealed a significant effect in favor of manipulative therapy on a short-term basis even though many studies reviewed were of low quality.22
Clinicians facing LE are trying different approaches, and multimodality is often observed.29, 30, 31 It is with this idea in mind that our team wanted to test the addition of a new cryotherapy device to manual therapy commonly provided in the treatment of LE. Cryostimulation is believed to rapidly induce vasoconstriction and local analgesia. A fast drop in skin surface temperature is induced by vaporizing high-pressured cooled carbon dioxide on the skin.32 To our knowledge, no study has investigated the effects of cryostimulation on chronic injuries; thus, we decided to add it to already confirmed effects of manual therapy.
Given the current knowledge on treatments for LE, we hypothesized that the addition of cryostimulation to conservative care including tender point (trigger point) treatment with manual therapies and radial head mobilizations would improve the clinical outcomes—pain-free grip strength, perceived pain intensity, and functional level—in subjects affected by chronic LE. We hypothesized that like conventional ice, the temporary analgesia provided by cryostimulation would enhance patients' forearm mobility.33 Mobility has been used by many researchers to stimulate tendon healing.34 The purpose of this pilot study was to evaluate the feasibility and efficacy of adding cryostimulation to manual therapy in patients with chronic LE.
Methods
Study Design
This study is a pilot clinical trial focused on feasibility outcomes such as side effects related to cryostimulation, participants’ retention rate throughout the protocol, and challenges related to running the experiment in a university-based chiropractic clinic. The secondary objective was to provide estimates of treatment effect on common chronic LE clinical outcomes. One protocol consisted of manual therapy, and the second included manual therapy combined with cryostimulation. The study was designed to test the hypothesis that cryostimulation can be used (feasibility) and is effective as an adjunct therapy in the treatment of chronic LE.
Study Population
Potential participants were recruited through the university website, a billboard posting, and local newspapers. A total of 67 people manifested interest and were screened for eligibility. Inclusion and exclusion criteria are listed in Figure 1. Those criteria were consistent with those previously used in studies on LE10, 20, 35 and those recommended by the manufacturer of the cryostimulation device used in this trial.32
Fig 1.
Inclusion and exclusion criteria. ECBR, extensor carpi radialis brevis; PRTEE, Patient-Rated Tennis Elbow Evaluation.
Potential participants were invited to an initial visit, where they received information on the research project. After their eligibility was determined, a baseline evaluation was performed. All subjects signed an informed consent form before inclusion in the study, which was approved by the University Ethics Committee (CER-14-203-07.08). The clinical trial registry number is NCT02308514.
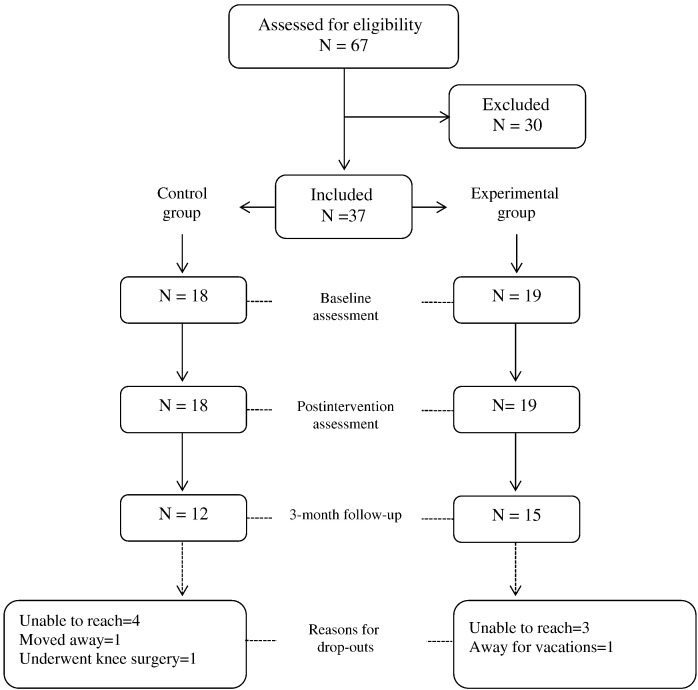
Of 67 people screened, 37 were deemed eligible. They were allocated to 1 of the 2 treatment groups based on a pairwise allocation so that the groups would remain comparable for sex and age. The recruitment and retention of participants are summarized in Figure 2.
Fig 2.
Flowchart.
Interventions
The control group was treated with manual therapy, which consisted of ischemic pressure on myofascial points36 located in the forearm musculature and radial head mobilizations.2, 13 The muscles treated included the flexor carpi radialis, flexor carpi ulnaris, pronator teres, brachioradialis, extensor carpi radialis longus and brevis, extensor indicis, and extensor digitorum communis and supinator. The mobilization technique used is Mill’s manipulation as described by James Cyriax (ie, patient is seated while a postero–anterior mobilization of the radial head is performed with the elbow in full extension and the wrist flexed and pronated).37, 38
The experimental group received cryostimulation in addition to manual therapy. Cryostimulation was delivered after the manual treatment of tender points because it is believed to transiently induce analgesia and to potentially impede patients’ perception of painful manual pressure.39, 40 Cryostimulation consisted of hyperbaric gaseous cryotherapy delivered by the use of a gun-shaped vaporizer projecting high-pressured refrigerated carbon dioxide microcrystals (–78°C) on the skin (50 bars at the pipe outlet and 3 bars at the skin level). The vaporizer nozzle was held at 15 cm from the skin as guided by the presence of a probe fixed to the tube outlet. Sublimation of the microcrystals on the skin has the ability to rapidly dissipate heat.32, 41 In line with the manufacturer’s recommendations,32 circular vaporization of the skin above the lateral elbow (12-15 cm2) was performed until a 4°C temperature recording was read by a laser thermometer, thus creating a so-called thermal shock. The local skin temperature decreased to 4°C in an average time of 30 seconds.
Both treatment protocols were delivered twice a week for 4 weeks, similar to a course of therapy commonly carried out with other conservative modalities.20
Each treatment lasted about 20 minutes and was delivered by a total of 9 experienced clinicians who had received 1 hour of training to optimize standardization of the treatment delivery. The training included the use of the cryostimulation device, the radial head mobilization, and myofascial therapy. A booklet containing all pertinent information was left available for clinicians’ use as needed. Clinicians could treat any participant with any treatment throughout the study. A total of 296 treatments were delivered over the span of the study.
At all times, participants were instructed to continue their normal activities and self-care (ie, orthotic brace, exercise, and medication). Patients were specifically asked not to undertake any other type of care throughout the protocol. Co-interventions were not recorded during the 4-week intervention period.
Outcome Measures
The clinical outcome measures included perceived pain intensity using a visual analog pain scale (VAS)5, 10 and pain-free grip strength (PFGS) for the painful arm. Pain-free grip strength was measured with a handheld dynamometer.35, 42 Specifically, patients were seated with the tested arm parallel to the trunk and the elbow extended, and were told to gradually increase their grip force and stop when they would feel pain or discomfort. Pain-free grip strength was measured 3 times with 30-second intervals between measurements. The average was used for better representation. Functional outcomes, namely disability and pain, were measured using the Patient Rated Tennis Elbow Evaluation questionnaire (PRTEE)43 cross-culturally adapted to the French Canadian population.44
Feasibility outcomes included any adverse reaction to gaseous cryotherapy, observance of the treatment protocol, and feasibility of such a clinical study in a university-based chiropractic clinic.
Data Collection
Both clinical and feasibility outcome measures were collected at baseline, after the 8 treatment sessions (postintervention assessment), and at the 3-month follow-up. Treating clinicians were not involved in the evaluation procedures and data analysis. The principal investigator and a research assistant performed the participants’ assessment and data extraction. Statistical analysis was performed by 2 other blinded researchers.
Statistical Analysis
The statistical analysis was performed using the Statistica data analysis software system, version 10 (StatSoft, Tulsa, Oklahoma). t-Tests for independent samples were conducted for baseline values of continuous variables. Pain intensity, PRTEE score, and mean PFGS for the painful arm were independently subjected to a repeated-measures analysis of variance having 2 levels of group (control and experimental) and 3 levels of time of measurements (baseline, postintervention, and 3-month follow-up). Whenever a main or interaction effect was observed, post hoc comparisons were made using Tukey’s test. Statistical significance was set, for all analyses, at P < .05.
Results
Feasibility
The conception and implementation of this pilot study proved to be realistic and efficient. The project was conducted through a university-based clinic, allowing chiropractic students to witness the implementation of clinical research as part of their learning experience.
Sixty-seven participants were recruited in less than 2 weeks, and 296 treatments were provided over a 3-month period with the collaboration of 9 clinicians. Adherence to protocols was excellent, with 100% of the participants attending the prescribed number of treatments, which were booked at the end of the initial assessment meeting.
Throughout the protocol, more than 144 cryostimulation treatments were delivered to 19 participants. It should be noted that 4 participants (21%) reported a skin rash around the sixth treatment. This irritation was considered a mild adverse reaction to cryostimulation, and those participants received the conservative part of the treatment only for the last 2 sessions. Otherwise, we did not experience any technical problems related to use of the cryostimulation device. Data of participants who partially completed the cryostimulation protocol because of side effects were analyzed according to their initial treatment allocation.
Participants
The t-test for independent samples revealed that both groups were comparable for age (P = .63), pain intensity (P = .59), PRTEE scores (P = .26), and mean PFGS (P = .69). Women represented 47% and 55% of participants in the control and experimental groups, respectively. The dominant side was affected in 68% of participants in the control group and 61% in the experimental group. A greater proportion of participants performed office-type (clerical) work in the control group (14/18) than in the experimental group (8/19). Similarly, a greater proportion of participants performed physical work in the experimental group (11/19) than in the control group (4/18). Symptom duration was 12.68 (range = 5–24) months in the experimental group and 21.66 (range = 6–84) months in control group. Participants’ baseline characteristics are listed in Table 1.
Table 1.
Participants’ Baseline Characteristics
| Variable | Control Group Mean (SD) | Experimental Group Mean (SD) | P |
|---|---|---|---|
| Age, y | 49.61 (8.45) | 51.05 (9.43) | .628 |
| Pain intensity, VAS | 6.13 (1.50) | 5.84 (1.87) | .599 |
| Strength,a N | 30.74 (13.34) | 32.50 (13.37) | .689 |
| PRTEE/100 | 41.80 (10.90) | 46.85 (15.36) | .259 |
| Sex ratio, W:M | 10:8 | 9:10 | — |
| Affected arm ratio, D:ND | 11:7 | 13:6 | — |
| Employment ratio, clerical:physical | 14:4 | 8:11 | — |
| Duration of symptoms, mo | 21.66 (25.52) | 12.68 (7.81) | .152 |
D, dominant; M, men; ND, non-dominant; PRTEE, Patient-Rated Tennis Elbow Evaluation Questionnaire; SD, standard deviation; VAS, visual analog scale; W, women.
Mean pain-free grip strength for painful arm.
Clinical Outcomes
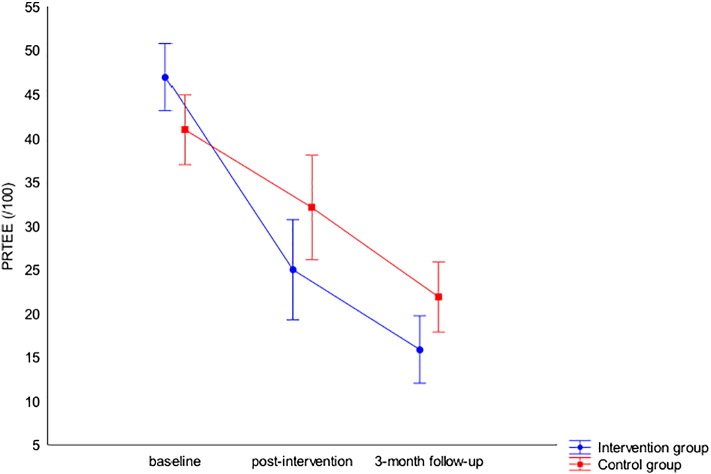
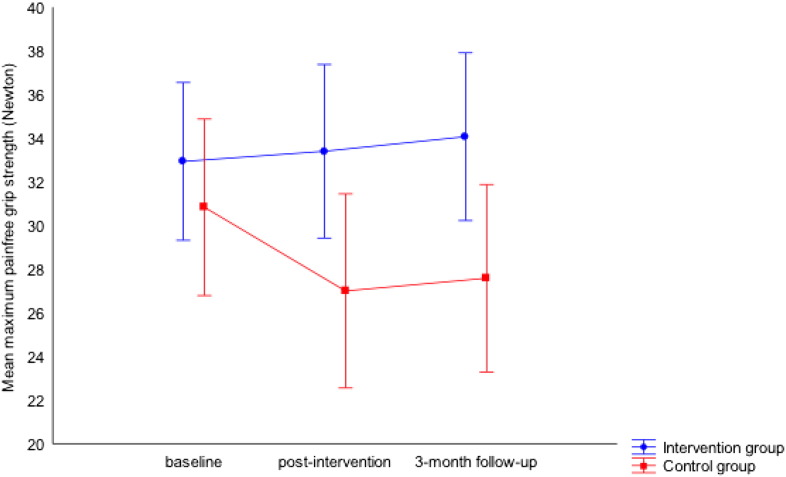
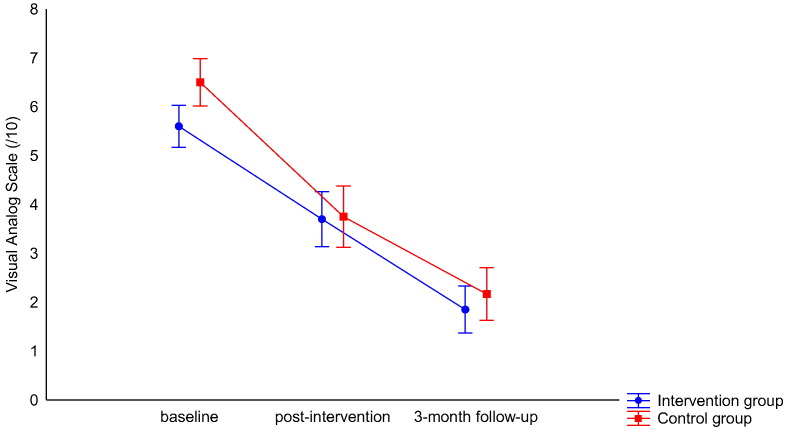
No main effect of group was observed for any of the clinical outcomes: pain intensity (F2,50 = 0.57, P = .45, ηp2 = 0.02), PRTEE score (F2,46 = 0.20, P = .65, ηp2 = 0.02), and mean maximum pain-free grip strength (F2,48 = 0.71, P = .40, ηp2 = 0.002). Similarly, no Group × Time interaction was found for pain intensity (F2,50 = 0.51, P = .59, ηp2 = 0.02), PRTEE score (F2,46 = 2.21, P = .12, ηp2 = 0.89), or mean maximum PFGS (F2,48 = 0.46, P = .63, ηp2 = 0.002). The analysis, however, revealed a main effect of Time for both pain intensity (F2,50 = 45.18, P < .001, ηp2 = 0.64) and PRTEE score (F2,46 = 26.72, P < .001, ηp2 = 0.54), but not for mean maximum PFGS (F2,48 = 0.48, P = .61, ηp2 = 0.38). The Tukey post hoc test revealed that both pain intensity and PRTEE scores were significantly lower from baseline to postintervention assessment, from baseline to 3-month follow-up, and from postintervention to 3-month follow-up. Mean values and standard deviations for all outcomes throughout assessments for both groups are listed in Table 2 and illustrated in Fig 3, Fig 4, Fig 5. Poltawsky et al compared the PRTEE with the DASH (Disabilities of the Arm, Shoulder and Hand) and other questionnaires.45 They found that the minimum clinically important difference (MCID) would be 37%, or a reduction of 11 points from the baseline score, to mark a significant improvement, and a change of 7 points (22%) is deemed necessary to detect a limited but meaningful improvement.45
Table 2.
Means and Standard Deviations for All Outcomes Throughout Assessments
| Experimental Group |
Control Group |
||||
|---|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | ||
| Pain intensity (0–10) | Baseline | 5.84 (1.87) | 4.94–6.74 | 6.14 (1.50) | 5.39–6.89 |
| Postintervention | 3.71 (2.19)a | 2.65–4.77 | 3.67 (1.82)a | 2.76–4.57 | |
| 3-month follow-up | 1.85 (1.85)a, b | 0.82–2.88 | 2.17 (1.89)a, b | 0.97–3.37 | |
| PRTEE (/100) | Baseline | 46.85 (15.36) | 39.45–54.26 | 41.81 (10.91) | 36.38–47.23 |
| Postintervention | 25.42 (19.20)a | 16.17–34.68 | 31.09 (18.68)a | 21.80–40.38 | |
| 3-month follow-up | 15.86 (12.25)a, b | 8.46–23.27 | 21.85 (15.37)a, b | 12.09–31.62 | |
| Mean maximum strength, painful arm (N) | Baseline | 32.50 (13.37) | 26.06–38.96 | 30.74 (13.35) | 24.10–37.38 |
| Postintervention | 32.47 (15.94) | 24.79–40.16 | 28.02 (13.07) | 21.52–34.52 | |
| 3-month follow-up | 32.17 (14.49) | 24.15–40.21 | 28.82 (12.90) | 20.15–37.48 | |
CI, confidence interval; PRTEE, Patient-Rated Tennis Elbow Evaluation Questionnaire; SD, standard deviation.
Statistically different from baseline.
Statistically different from postintervention.
Fig 3.
Change in patient-rated tennis elbow evaluation.
Fig 4.
Pain-free grip strength visual analog scale scores.
Fig 5.
Pain intensity.
Participants were asked about potential co-intervention undertaken for their LE during the 3-month postintervention period. Of the 27 participants who provided information, 9 reported doing nothing in particular (5 from the control group and 4 from the experimental group), whereas the other 18 (7 from the control group and 12 from the experimental group) initiated or pursued conservative care (chiropractic, physiotherapy, massage) sometimes combined with exercises, an orthotic brace, or nonprescribed medication (nonsteroidal anti-inflammatory drug). Seven of the 18 participants who underwent other interventions came from the control group, and 11 of them came from the experimental group.
Discussion
The main objective of this pilot study was to determine the feasibility outcomes related to cryostimulation and implementation of the protocol in a university-based chiropractic clinic. In addition, preliminary effects of using cryostimulation as an adjunct therapy in the conservative care of chronic LE of the elbow have been sought.
With respect to feasibility, the fact that treatments were free possibly helped in the recruitment and retention of participants. We also think that establishing a fixed schedule right from the start (all appointments were booked on the initial visit) helped patients attend all treatments. The study provides new information on the safety of cryostimulation. A skin reaction was reported in 4 of 19 patients. It is possible that the repeated application (twice a week for 4 weeks) of very cold air (–78°C) on a small skin area had a cumulative effect on skin sensitization.46 Because the goal of cryostimulation is to lower the skin temperature to near-freezing levels (4°C), it would be advisable to be cautious when reading skin temperature during cryostimulation applications and to ensure that circular motions are used as recommended by the device manufacturers.
Concerning the use of cryostimulation, our results indicated a statistically and clinically significant decrease in pain perception (VAS) and disability (PRTEE) scores at the postintervention assessment in both groups. Interestingly, those results were maintained at the 3-month follow-up. Pain-free grip measures did not improve in either group at any time point.
The results obtained herein agree with those of other studies reporting a positive effect of soft-tissue therapy in the treatment of LE.1, 20, 28, 47, 48 The review conducted by Shmushkevich et al49 reported positive effects on pain perception and function (PRTEE scores) at the end of experiments and at long-term follow-ups while using either manual therapy or augmented soft-tissue mobilization.10, 20, 28 Another systematic review presented by Herd et al focusing specifically on the effectiveness of manipulative therapy for LE concluded that elbow mobilizations provide immediate, short-term, and long-term benefits on pain and function, even though those conclusions are drawn from fair- and low-quality studies.22 A recent systematic review attempting to determine the effectiveness of soft-tissue therapy for the management of musculoskeletal disorders and injuries affecting upper and lower extremities50 concluded that myofascial therapy is effective in the treatment of LE. In light of this scientific evidence, it is possible to believe that the effect of myofascial therapy was important enough to obviate any effect of cryostimulation.
From an economical and quality-of-life standpoint, Coombes et al reported that conservative care (manual therapy and exercise) is superior to corticosteroid injections.51 Those results favor manual therapy as an effective way of decreasing LE symptoms.
Limitations
Because no published study could provide sufficient evidence regarding the effects of cryostimulation on chronic lesions,52 we decided to offer conservative care to both groups based on previously reported positive effects.22, 23, 28 Hence, our protocol did not allow for measurement of the isolated effects of cryotherapy on LE.
Another limitation is the fact that participants could not be blinded to the application of cold air on their skin. However, if the “thermal shock” phenomenon allegedly produced by the cryostimulation had been well documented and its physiological effect known, we could have used conventional ice application or vapocoolant sprays as a placebo treatment in the control group.53, 54 Moreover, clinicians could not be blinded to the treatment they executed, and even though they treated participants from both groups, we cannot estimate the impact of their influence on the treatment outcome. Nonetheless, data collection and statistical analysis were conducted by researchers blinded to the treatment allocation.
In addition, the pairwise allocation yielded some difference between groups for occupation (22% of physical workers in the control group versus 58% in the experimental group), which could have been minimized by using a larger sample size and a random allocation process.
Moreover, that patients were asked to continue their normal activity and self-care throughout the study and that we did not keep a record of possible co-interventions prevent us from concluding on the outcomes of manual therapy alone. Another limitation is that no directives were given for participants to follow between the end of the protocol and the follow-up assessment. As often seen in private practice,22, 25, 30, 55, 56 participants used a wide variety of modalities to lessen symptoms of LE. We therefore cannot exclude that some of the reported improvements were related to co-intervention and not only to the experimental treatment. Finally, 10 participants were lost at follow-up; perhaps we could have used an incentive measure to maximize the number of participants returning for the last assessment.
Conclusions
In this study, we found few adverse effects related to the biweekly use of cryostimulation and good feasibility in a university-based environment. In this precise protocol, no effect could be directly attributed to the addition of cryostimulation to conservative care for chronic LE treatments. The improvement seen in PRTEE scores and pain intensity for both groups reinforces that myofascial and mobilization techniques may yield positive outcomes in the care of LE. Further studies are needed to investigate the therapeutic effects of cryostimulation used either as a single treatment option or in acute conditions.57, 58, 59, 60
Acknowledgments
Acknowledgments
The authors thank Maude-Hélène Benoit and the university clinic staff for their contributions to this project.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): M.D., N.R.
Design (planned the methods to generate the results): N.R., M.D., A.A.M.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): N.R.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): N.R.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): M.D., A.A.M.
Literature search (performed the literature search): N.R.
Writing (responsible for writing a substantive part of the manuscript): N.R., M.D., A.A.M.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): M.D., A.A.M.
Practical Applications
-
•
Use of manual therapy has been found to improve clinical outcomes such as perceived pain level and functional level in the care of LE.
-
•
Local cryostimulation does not seem to have an effect on chronic conditions like LE.
-
•
Repeated local cryostimulation can cause skin irritations and should be used carefully.
Alt-text: Image 1
References
- 1.Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BM. Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review. Br J Sports Med. 2013;47(17):1112–1119. doi: 10.1136/bjsports-2012-091990. [DOI] [PubMed] [Google Scholar]
- 2.Fernández-Carnero J, Fernández-de-las-Peñas C, de la Llave-Rincón AI, Ge HY, Arendt-Nielsen L. Bilateral myofascial trigger points in the forearm muscles in patients with chronic unilateral lateral epicondylalgia: a blinded, controlled study. Clin J Pain. 2008;24(9):802–807. doi: 10.1097/AJP.0b013e31817bcb79. [DOI] [PubMed] [Google Scholar]
- 3.Waseem M, Nuhmani S, Ram CS, Sachin Y. Lateral epicondylitis: a review of the literature. J Back Musculoskelet Rehabil. 2012;25(2):131–142. doi: 10.3233/bmr-2012-0328. [DOI] [PubMed] [Google Scholar]
- 4.Taylor SA, Hannafin JA. Evaluation and management of elbow tendinopathy. Sports Health. 2012;4(5):384–393. doi: 10.1177/1941738112454651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rompe JD, Overend TJ, MacDermid JC. Validation of the patient-rated tennis elbow evaluation questionnaire. J Hand Ther. 2007;20(1):3–10. doi: 10.1197/j.jht.2006.10.003. quiz 11. [DOI] [PubMed] [Google Scholar]
- 6.Sanders TL, Jr., Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med. 2015;43(5):1066–1071. doi: 10.1177/0363546514568087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164(11):1065–1074. doi: 10.1093/aje/kwj325. [DOI] [PubMed] [Google Scholar]
- 8.Melchior M, Roquelaure Y, Evanoff B. Why are manual workers at high risk of upper limb disorders? The role of physical work factors in a random sample of workers in France (the Pays de la Loire study) Occup Environ Med. 2006;63(11):754–761. doi: 10.1136/oem.2005.025122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vicenzino B, Coombes BK. A single botulinum toxin injection at a precise anatomic point on the forearm reduces pain at rest, compared to placebo injection in patients with chronic refractory lateral epicondylitis. Evid Based Med. 2010;15(5):149–150. doi: 10.1136/ebm1115. [DOI] [PubMed] [Google Scholar]
- 10.Blanchette MA, Normand MC. Augmented soft tissue mobilization vs natural history in the treatment of lateral epicondylitis: a pilot study. J Manipulative Physiol Ther. 2011;34(2):123–130. doi: 10.1016/j.jmpt.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Lamarche D, Provencher J, Boucher P. Québec, QC; Commission de la santé et de la sécurité du travail du Québec: 2009. Statistiques sur les lésions en «ITE» du système musculo-squelettique 2005–2008. [Google Scholar]
- 12.Peterson M, Butler S, Eriksson M, Svärdsudd K. A randomized controlled trial of eccentric vs. concentric graded exercise in chronic tennis elbow (lateral elbow tendinopathy) Clin Rehabil. 2014;28(9):862–872. doi: 10.1177/0269215514527595. [DOI] [PubMed] [Google Scholar]
- 13.Radpasand M. Combination of manipulation, exercise, and physical therapy for the treatment of a 57-year-old woman with lateral epicondylitis. J Manipulative Physiol Ther. 2009;32(2):166–172. doi: 10.1016/j.jmpt.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004;51(4):642–651. doi: 10.1002/art.20535. [DOI] [PubMed] [Google Scholar]
- 15.van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford) 2009;48(5):528–536. doi: 10.1093/rheumatology/kep013. [DOI] [PubMed] [Google Scholar]
- 16.Walker-Bone K, Reading I, Coggon D, Cooper C, Palmer KT. Risk factors for specific upper limb disorders as compared with non-specific upper limb pain: assessing the utility of a structured examination schedule. Occup Med (Lond) 2006;56(4):243–250. doi: 10.1093/occmed/kql016. [DOI] [PubMed] [Google Scholar]
- 17.Kivi P. The etiology and conservative treatment of humeral epicondylitis. Scand J Rehabil Med. 1983;15(1):37–41. [PubMed] [Google Scholar]
- 18.Hong QN, Durand MJ, Loisel P. Treatment of lateral epicondylitis: where is the evidence? Joint Bone Spine. 2004;71(5):369–373. doi: 10.1016/j.jbspin.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Amro A, Diener I, Bdair WO, Hameda IM, Shalabi AI, Ilyyan DI. The effects of Mulligan mobilisation with movement and taping techniques on pain, grip stregth, and function in patients with lateral epicondylitis. Hong Kong Physiother J. 2010;28(1):19–23. [Google Scholar]
- 20.Nourbakhsh MR, Fearon FJ. The effect of oscillating-energy manual therapy on lateral epicondylitis: a randomized, placebo-control, double-blinded study. J Hand Ther. 2008;21(1):4–13. doi: 10.1197/j.jht.2007.09.005. quiz 14. [DOI] [PubMed] [Google Scholar]
- 21.Gliedt JA, Daniels CJ. Chiropractic treatment of lateral epicondylitis: a case report utilizing active release techniques. J Chiropr Med. 2014;13(2):104–109. doi: 10.1016/j.jcm.2014.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herd CR, Meserve BB. A systematic review of the effectiveness of manipulative therapy in treating lateral epicondylalgia. J Man Manip Ther. 2008;16(4):225–237. doi: 10.1179/106698108790818288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smidt N, van der Windt DA, Assendelft WJ, Devillé WL, Korthals-de Bos IB, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet. 2002;359(9307):657–662. doi: 10.1016/S0140-6736(02)07811-X. [DOI] [PubMed] [Google Scholar]
- 24.Struijs PA, Smidt N, Arola H, van Dijk CN, Buchbinder R, Assendelft WJ. Orthotic devices for tennis elbow: a systematic review. Br J Gen Pract. 2001;51(472):924–929. [PMC free article] [PubMed] [Google Scholar]
- 25.Dingemanse R, Randsdorp M, Koes BW, Huisstede BM. Evidence for the effectiveness of electrophysical modalities for treatment of medial and lateral epicondylitis: a systematic review. Br J Sports Med. 2014;48(12):957–965. doi: 10.1136/bjsports-2012-091513. [DOI] [PubMed] [Google Scholar]
- 26.Cullinane FL, Boocock MG, Trevelyan FC. Is eccentric exercise an effective treatment for lateral epicondylitis? A systematic review. Clin Rehabil. 2014;28(1):3–19. doi: 10.1177/0269215513491974. [DOI] [PubMed] [Google Scholar]
- 27.Martinez-Silvestrini JA, Newcomer KL, Gay RE, Schaefer MP, Kortebein P, Arendt KW. Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther. 2005;18(4):411–419. doi: 10.1197/j.jht.2005.07.007. quiz 420. [DOI] [PubMed] [Google Scholar]
- 28.Ajimsha MS, Chithra S, Thulasyammal RP. Effectiveness of myofascial release in the management of lateral epicondylitis in computer professionals. Arch Phys Med Rehabil. 2012;93(4):604–609. doi: 10.1016/j.apmr.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 29.Olaussen M, Holmedal Ø, Mdala I, Brage S, Lindbæk M. Corticosteroid or placebo injection combined with deep transverse friction massage, Mills manipulation, stretching and eccentric exercise for acute lateral epicondylitis: a randomised, controlled trial. BMC Musculoskelet Disord. 2015;16:122. doi: 10.1186/s12891-015-0582-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radpasand M, Owens E. Combined multimodal therapies for chronic tennis elbow: pilot study to test protocols for a randomized clinical trial. J Manipulative Physiol Ther. 2009;32(7):571–585. doi: 10.1016/j.jmpt.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 31.Papa JA. Two cases of work-related lateral epicondylopathy treated with Graston Technique® and conservative rehabilitation. J Can Chiropr Assoc. 2012;56(3):192–200. [PMC free article] [PubMed] [Google Scholar]
- 32.Cluzeau C. MTM cryo. Cryonic Medical France: Cryonic Medical. Available at: http://www.cryonic.ca/pdf/fr/dossier_de_presse.pdf. Accessed August 14, 2014.
- 33.Bleakley CM, O’Connor SR, Tully MA. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ. 2010;340:c1964. doi: 10.1136/bmj.c1964. [DOI] [PubMed] [Google Scholar]
- 34.Malliaras P, Maffulli N, Garau G. Eccentric training programmes in the management of lateral elbow tendinopathy. Disabil Rehabil. 2008;30(20-22):1590–1596. doi: 10.1080/09638280701786195. [DOI] [PubMed] [Google Scholar]
- 35.Coombes BK, Bisset L, Vicenzino B. Cold hyperalgesia associated with poorer prognosis in lateral epicondylalgia: a 1-year prognostic study of physical and psychological factors. Clin J Pain. 2015;31(1):30–35. doi: 10.1097/AJP.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 36.Simons DG, Travell JG, Simons LS. 2nd ed. Lippincott Williams & Wilkins; Baltimore, MD: 1999. Travell & Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual. [Google Scholar]
- 37.Bergmann TF, Peterson DH. 3rd ed. Mosby; St. Louis, MO: 2011. Chiropractic Technique: Principles and Procedures; p. 484. [Google Scholar]
- 38.Manias P, Stasinopoulos D. A controlled clinical pilot trial to study the effectiveness of ice as a supplement to the exercise programme for the management of lateral elbow tendinopathy. Br J Sports Med. 2006;40(1):81–85. doi: 10.1136/bjsm.2005.020909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Park KN, Kwon OY, Weon JH, Choung SD, Kim SH. Comparison of the effects of local cryotherapy and passive cross-body stretch on extensibility in subjects with posterior shoulder tightness. J Sports Sci Med. 2014;13(1):84–90. [PMC free article] [PubMed] [Google Scholar]
- 40.Swenson C, Swärd L, Karlsson J. Cryotherapy in sports medicine. Scand J Med Sci Sports. 1996;6(4):193–200. doi: 10.1111/j.1600-0838.1996.tb00090.x. [DOI] [PubMed] [Google Scholar]
- 41.Demoulin C, Brouwers M, Darot S, Gillet P, Crielaard JM, Vanderthommen M. Comparison of gaseous cryotherapy with more traditional forms of cryotherapy following total knee arthroplasty. Ann Phys Rehabil Med. 2012;55(4):229–240. doi: 10.1016/j.rehab.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 42.Blanchette MA, Normand MC. Impairment assessment of lateral epicondylitis through electromyography and dynamometry. J Can Chiropr Assoc. 2011;55(2):96–106. [PMC free article] [PubMed] [Google Scholar]
- 43.Bisset L, Coombes B, Vicenzino B. Tennis elbow. BMJ Clin Evid. 2011;2011 [PMC free article] [PubMed] [Google Scholar]
- 44.Blanchette MA, Normand MC. Cross-cultural adaptation of the patient-rated tennis elbow evaluation to Canadian French. J Hand Ther. 2010;23(3):290–299. doi: 10.1016/j.jht.2010.01.003. quiz 300. [DOI] [PubMed] [Google Scholar]
- 45.Poltawski L, Watson T. Measuring clinically important change with the patient-rated tennis elbow evaluation. Hand Ther. 2011;16(3):52–57. [Google Scholar]
- 46.Morrison SA, Gorjanc J, Eiken O, Mekjavic IB. Finger and toe temperature responses to cold after freezing cold injury in elite alpinists. Wilderness Environ Med. 2015;26(3):295–304. doi: 10.1016/j.wem.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 47.Vicenzino B, Paungmali A, Buratowski S, Wright A. Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Man Ther. 2001;6(4):205–212. doi: 10.1054/math.2001.0411. [DOI] [PubMed] [Google Scholar]
- 48.Paungmali A, O'Leary S, Souvlis T, Vicenzino B. Hypoalgesic and sympathoexcitatory effects of mobilization with movement for lateral epicondylalgia. Phys Ther. 2003;83(4):374–383. [PubMed] [Google Scholar]
- 49.Shmushkevich Y, Kalichman L. Myofascial pain in lateral epicondylalgia: a review. J Bodyw Mov Ther. 2013;17(4):434–439. doi: 10.1016/j.jbmt.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 50.Piper S, Shearer HM, Côté P. The effectiveness of soft-tissue therapy for the management of musculoskeletal disorders and injuries of the upper and lower extremities: a systematic review by the Ontario Protocol for Traffic Injury management (OPTIMa) collaboration. Man Ther. 2016;21:18–34. doi: 10.1016/j.math.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 51.Coombes BK, Connelly L, Bisset L, Vicenzino B. Economic evaluation favours physiotherapy but not corticosteroid injection as a first-line intervention for chronic lateral epicondylalgia: evidence from a randomised clinical trial. Br J Sports Med. 2016;50(22):1400–1405. doi: 10.1136/bjsports-2015-094729. [DOI] [PubMed] [Google Scholar]
- 52.Guillot X, Tordi N, Mourot L. Cryotherapy in inflammatory rheumatic diseases: a systematic review. Expert Rev Clin Immunol. 2014;10(2):281–294. doi: 10.1586/1744666X.2014.870036. [DOI] [PubMed] [Google Scholar]
- 53.Demoulin C, Vanderthommen M. Cryotherapy in rheumatic diseases. Joint Bone Spine. 2012;79(2):117–118. doi: 10.1016/j.jbspin.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 54.Mawhorter S, Daugherty L, Ford A, Hughes R, Metzger D, Easley K. Topical vapocoolant quickly and effectively reduces vaccine-associated pain: results of a randomized, single-blinded, placebo-controlled study. J Travel Med. 2004;11(5):267–272. doi: 10.2310/7060.2004.19101. [DOI] [PubMed] [Google Scholar]
- 55.Bisset LM, Vicenzino B. Physiotherapy management of lateral epicondylalgia. J Physiother. 2015;61(4):174–181. doi: 10.1016/j.jphys.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 56.Coombes BK, Bisset L, Vicenzino B. Management of lateral elbow tendinopathy: one size does not fit all. J Orthop Sports Phys Ther. 2015;45(11):938–949. doi: 10.2519/jospt.2015.5841. [DOI] [PubMed] [Google Scholar]
- 57.Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251–261. doi: 10.1177/0363546503260757. [DOI] [PubMed] [Google Scholar]
- 58.Guilhem G, Hug F, Couturier A. Effects of air-pulsed cryotherapy on neuromuscular recovery subsequent to exercise-induced muscle damage. Am J Sports Med. 2013;41(8):1942–1951. doi: 10.1177/0363546513490648. [DOI] [PubMed] [Google Scholar]
- 59.Khoshnevis S, Craik NK, Diller KR. Cold-induced vasoconstriction may persist long after cooling ends: an evaluation of multiple cryotherapy units. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2475–2483. doi: 10.1007/s00167-014-2911-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hubbard TJ, Denegar CR. Does cryotherapy improve outcomes with soft tissue injury? J Athl Train. 2004;39(3):278–279. [PMC free article] [PubMed] [Google Scholar]