Abstract
Background
Patients with Parkinson’s disease (PD) experience debilitating motor symptoms as well as non-motor symptoms, such as cognitive dysfunction and sleep disorders. This constellation of symptoms has the potential to negatively influence pedestrian safety.
Objective
Investigate the association of motor symptoms, daytime sleepiness, impaired vigilance, and cognitive dysfunction on pedestrian behavior in patients with PD and healthy older adults. Methods: Fifty PD and 25 control participants were evaluated within a virtual reality pedestrian environment and completed assessments of motor performance, daytime sleepiness (Epworth Sleepiness Scale), vigilance (psychomotor vigilance task), and visual processing speed (Useful Field of View: UFOV®) outside of the virtual reality environment. The primary outcome measure was Time to Contact (TTC), defined as the time remaining until a participant would have been hit by an approaching vehicle while crossing the virtual street.
Results
The virtual reality pedestrian environment was feasible in all participants. Patients with PD demonstrated riskier pedestrian behavior compared to controls. Among PD participants, walking speed, objective measures of vigilance, and visual processing speed were correlated with pedestrian behavior, with walking speed being the strongest predictor of Time to Contact, explaining 48% of the variance. Vigilance explained an additional 8% of the variance. In controls, vigilance was also important for street-crossing safety, but older age was the most robust predictor of pedestrian safety.
Conclusion
Walking speed is associated with unsafe pedestrian behavior in patients with PD. In contrast, age was the strongest predictor of pedestrian safety in healthy older adults.
Keywords: Parkinson’s disease, vigilance, virtual reality, safety, visual processing
INTRODUCTION
Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by motor symptoms of bradykinesia, tremor, rigidity, and postural instability. Additionally, non-motor symptoms such as cognitive impairment and sleep dysfunction are increasingly recognized as a source of disability among PD patients(1, 2). Sleep disorders, including excessive daytime sleepiness (EDS), are particularly common, affecting 74–98% of patients(3, 4). EDS is associated with impaired vigilance and can negatively impact safe completion of tasks such as driving or crossing a street(5, 6).
Pedestrian injury is a significant risk for older individuals(7). In fact, 20% of pedestrian fatalities and 11% of injuries in the United States in 2014 and 42% of pedestrian fatalities in Europe in 2009 involved persons 65 or older(7, 8). Successful pedestrian behavior requires integration of motor function, perceptual ability/vigilance, and cognitive function (particularly visual processing and attention(9, 10). Changes that can occur in normal aging, such as reduced stride length and acceleration capacity, slowed visual processing speed, and cognitive changes, can impair safe pedestrian behavior(10, 11). These changes are more pronounced and occur at younger ages in PD. In fact, PD patients have more gait impairment, EDS, cognitive dysfunction, and visual processing deficits compared to age-matched controls(12, 13). Although the prevalence of pedestrian injury in PD is not known, this constellation of deficits increases risk of unsafe pedestrian behavior in these patients(14). This case-control, cross-sectional study evaluates the association of motor function, EDS, vigilance, and visual processing speed with pedestrian safety as measured within a validated virtual reality (VR) pedestrian environment(15) in patients with PD compared to healthy controls (HC). We hypothesized that EDS and impaired vigilance would negatively affect pedestrian behavior and we also explored the association of walking speed, motor symptoms, dopaminergic medications, and demographics with street-crossing safety in the VR environment.
METHODS
Participants
This case-control, cross-sectional, observational study enrolled 51 PD and 25 HC participants. Fifty PD participants were included in the final analyses after excluding one participant due to monocular blindness. PD participants were recruited from the University of Alabama at Birmingham (UAB) Movement Disorders Center and HC were recruited from patient family members and from the community through flyers and recruitment fairs. Inclusion required age 45–85, ability to ambulate without assistance, and ability to walk up and down a small set of stairs. PD participants had a clinical diagnosis of idiopathic PD-Hoehn and Yahr stages 1–4. Participants were excluded for symptoms or history indicative of atypical or secondary Parkinsonism, blindness, or cognitive dysfunction that would prevent completion of study procedures. There were no significant differences in age, sex, or race between PD and HC groups (Table 1). For participants with PD, dopaminergic therapy usage (levodopa equivalent dose or LED) was calculated as previously described(16). The UAB IRB approved the study and all participants consented to participation through written informed consent.
Table 1.
Participant Demographics
| Total Sample | Parkinson’s Disease |
Control | p-value^ | |
|---|---|---|---|---|
| N | 75 | 50 | 25 | -- |
|
| ||||
| Age in years: | ||||
| Mean ± SD | 62.32 ± 8.50 | 62.54 ± 8.04 | 61.88 ± 9.51 | 0.754 |
| Range | 43–83 | 43–83 | 47–78 | |
|
| ||||
| Sex: N (%) | ||||
| Male | 42 (56.0) | 29 (58.0) | 13 (52.0) | 0.632 |
| Female | 33 (44.0) | 21 (42.0) | 12 (48.0) | |
|
| ||||
| Race: N (%) | ||||
| Caucasian | 69 (92.0) | 47 (94.0) | 22 (88.0) | 0.204+ |
| African American | 2 (2.7) | 1 (2.0) | 1 (4.0) | |
| Hispanic | 2 (2.7) | 2 (4.0) | 0 (0.0) | |
| Asian | 2 (2.7) | 0 (0.0) | 2 (8.0) | |
|
| ||||
| Duration of Disease (years): | ||||
| Mean ± SD | -- | 5.98 ± 3.91 | -- | -- |
|
| ||||
| UPDRS Part III*: | ||||
| Mean ± SD | -- | 24.16 ± 7.65 | -- | -- |
|
| ||||
| Hoehn & Yahr* | ||||
| Median (IQR) | -- | 2 (2–3) | -- | -- |
| Stage 2: N (%) | 24 (64.9) | |||
| Stage 3: N (%) | 12 (32.4) | |||
| Stage 4: N (%) | 1 (2.7) | |||
|
| ||||
| Side of Symptom Onset N (%) | ||||
| Left | -- | 23 (46.9) | -- | -- |
| Right | 26 (53.1) | |||
|
| ||||
| Levodopa Equivalent Dose (LED) Total | ||||
| Mean ± SD | -- | 691.78 ± 624.62 | -- | -- |
| Median (IQR) | 500 (273–1015) | |||
|
| ||||
| Levodopa only LED | ||||
| Mean ± SD | -- | 487.65 ± 575.37 | -- | -- |
| Median (IQR) | 337.5 (0–798) | |||
|
| ||||
| Dopamine agonist LED | ||||
| Mean ± SD | -- | 118.30 ± 162.01 | -- | -- |
| Median (IQR) | 40 (0–180) | |||
Parkinson’s disease versus control participants;
Fisher’s exact test;
N=37
Participant Evaluations
All participants were evaluated during a single visit, which included gathering demographic information, participation within the semi-immersive VR pedestrian environment, and evaluation of motor symptoms, visual processing speed, objective vigilance, and subjective sleepiness.
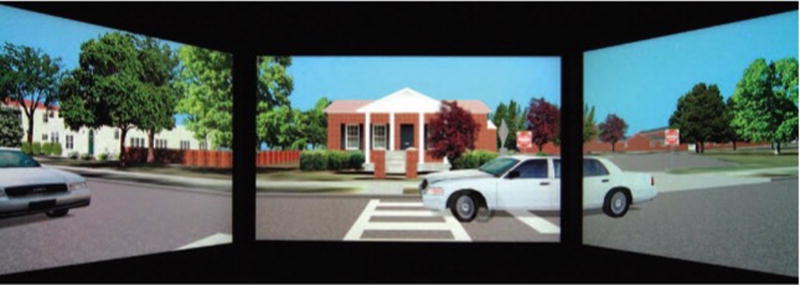
The VR pedestrian environment is a validated measure of “real-world” street-crossing behavior(15). The system is composed of an elevated platform, which simulates a street-side curb, and 3 monitors (arranged in a semi-circle) on which participants view the virtual environment of bidirectional traffic on a moderately busy suburban road with a 25-foot crosswalk (Figure 1). When participants feel they can safely make it across the virtual street, they step off the platform/curb onto a trigger plate, which activates a cartoon representation of the participant (avatar) to cross the street. The time to contact (TTC) is measured within this environment. TTC is defined as the shortest time remaining until a participant would have been hit by an approaching vehicle during the crossing within the virtual pedestrian environment (distance of the participant from oncoming virtual vehicle divided by speed of vehicle). A lower number on this task indicates riskier pedestrian behavior. The number of times a participant is hit by an approaching vehicle or has a close call to being hit is also measured. Each participant performed 12 orientation trials within the VR simulator to become familiar with the environment, and 12 data collection trials. This number of orientation trials minimizes practice effects in the simulator(17). The speed at which the avatar crosses the street is determined by each participant’s walking speed, which is measured at a 25-foot distance, averaged over 4-trials, prior to participation in the VR pedestrian environment.
Figure 1. Virtual reality pedestrian environment.
Virtual reality pedestrian environment: Screenshot of bidirectional traffic viewed on 3 monitors within the virtual reality pedestrian environment
Motor symptoms were evaluated in PD participants with Hoehn and Yahr stage and with the Unified Parkinson’s Disease Rating Scale (UPDRS), part III (motor examination)(18). Higher scores on these assessments indicate more severe motor symptoms.
Visual processing speed was measured independent of the VR simulator with the Useful Field of View(19) (UFOV®) test. This assessment has three subtests: stimulus identification, divided attention, and selective attention. The UFOV® uses a touch screen monitor on which participants identify a central target (subtest 1); a central target concurrent with a peripheral target simultaneously presented at one of 8 radial locations on the screen (subtest 2); or a central and concurrent peripheral target displayed with distractors on the screen (subtest 3). The difficulty of each test is altered based on participant response until the participant’s threshold (stimulus display time at which participant can correctly identify the stimulus 75% of the time) is determined. Lower scores on this assessment indicate better visual processing speed.
To evaluate subjective sleepiness and objective vigilance, we administered the Epworth Sleepiness Scale(20) (ESS) and the psychomotor vigilance task(21) (PVT-192, Ambulatory Monitoring, Inc. Ardsley, NY). The ESS is a questionnaire through which participants rate their likelihood of falling asleep in 8 different situations (each item ranges from 0–), with higher scores indicating more subjective sleepiness and a maximum score of 24. A score >10 indicates excessive daytime sleepiness. The PVT is a handheld device that displays a light at a random inter-stimulus interval over 10 minutes. Participants push a button as quickly as possible when the stimulus appears. The reciprocal reaction time (RRT) and lapses measured by the PVT are demonstrated to be sensitive to partial and total sleep deprivation(22). Higher mean RRT and fewer lapses indicate better vigilance. The psychomotor vigilance task measuring reciprocal reaction time (RRT) was not performed on all participants because it was added after study recruitment began.
Statistical Analysis
This is a cross-sectional study conducted in PD and HC participants. The primary outcome measure is the TTC, which was computed as an average TTC across the 12 data collection trial crossings. Secondary outcomes included walking speed and motor score of the UPDRS; subjective sleepiness as measured by the Epworth sleepiness scale; vigilance as measured by the PVT (mean RRT and lapses); visual processing speed as measured by the UFOV; and other outcomes measured within the virtual reality pedestrian environment, including hits and close calls to collision and direction of hit. Summary statistics were calculated and compared between the two groups using 2-tailed t-tests. Bivariate correlation analyses, using Pearson correlation coefficients, were performed to evaluate relationships amongst variables. We performed a stepwise multiple linear regression analysis to evaluate predictors of pedestrian safety. In this model, TTC was the dependent variable, and we applied a forward selection procedure that included age, sex, duration of disease, LED (total, levodopa only, and dopamine agonist only), UPDRS score, PVT mean RRT, ESS, UFOV®, and walking speed as potential predictors for PD participants, and age, sex, PVT mean RRT, ESS, UFOV®, and walking speed as potential predictors for HC. We then performed a sensitivity analysis using a backward selection procedure to verify the consistency of the selection of predictors. Statistical significance was considered achieved at p <0.05.
RESULTS
Performance in the virtual reality pedestrian environment
All PD and HC participants successfully completed the VR task. Compared to HC, participants with PD demonstrated riskier pedestrian behavior, with significantly shorter TTC (less time between the participant and an approaching vehicle) and significantly more hits and close calls (Table 2). Similar to prior studies, all participants who were hit by an approaching vehicle were more likely to be hit by a vehicle in the far lane (car approaching from the right)(11). Participants with PD had significantly slower walking speed compared to HC.
Table 2.
Outcome measures for PD and control subjects
| Total Sample | Parkinson’s Disease |
Control | p-value^ | |
|---|---|---|---|---|
| Time to Contact (sec) | ||||
| Mean ± SD | 4.13 ± 1.24 | 3.94 ±1.38 | 4.51 ± 0.81 | 0.025+ |
|
| ||||
| Hits + Close Calls | ||||
| Median (IQR) | 1 (0–2) | 2 (0–3) | 1 (0–1) | 0.0004+ |
|
| ||||
| Side of Hit N (%) | ||||
| Right | 17 (65.4) | 12 (60) | 5 (83.3) | |
| Left | 5 (19.2) | 4 (20) | 1 (16.7) | 0.793^^ |
| Both | 4 (15.4) | 4 (20) | 0 (0) | |
|
| ||||
| Walking Speed miles/hr | ||||
| Mean ± SD | 2.82 ± 0.49 | 2.74 ± 0.53 | 3.00 ± 0.35 | 0.013+ |
|
| ||||
| ESS | ||||
| Mean ± SD | 8.88 ± 4.92 | 10.2 ± 4.98 | 6.24 ± 3.65 | 0.0007 |
|
| ||||
| Subjects with ESS >10 | ||||
| N (%) | 30 (40) | 26 (52) | 4 (16) | 0.002^^ |
|
| ||||
| PVT Mean RRT | ||||
| Mean ± SD | 3.57 ± 0.49 | 3.44 ± 0.52* | 3.75 ± 0.38 | 0.017 |
|
| ||||
| PVT Lapses | ||||
| Mean ± SD | 2.42 ± 3.07 | 3.26 ± 3.59* | 1.28 ± 1.65 | 0.013 |
|
| ||||
| UFOV® Total | ||||
| Mean ± SD | 342.4 ± 225.4 | 350.1 ± 226.2** | 327.3 ± 227.6 | 0.684 |
| Median (IQR) | 285 (160–478.5) | 330 (165–480) | 261 (145–464) | |
|
| ||||
| UFOV Stimulus Identification | ||||
| Median (IQR) | 17 (17–20) | 17 (17–23) | 17 (17–17) | 0.215++ |
|
| ||||
| UFOV Divided Attention | ||||
| Median (IQR) | 47 (23–157) | 47 (23–161) | 53 (21.5–173.5) | 0.978++ |
|
| ||||
| UFOV Selective Attention | ||||
| Median (IQR) | 213 (104.8–277) | 220 (111.5–275) | 143 (88.5–287) | 0.486++ |
Parkinson’s disease vs. Control subjects
N=34;
N=49
Fisher’s exact test (two-tailed),
Unequal variance t-test,
Wilcoxon
Subjective and objective sleepiness outcomes
Participants with PD were significantly more subjectively sleepy than HC and more PD participants scored in the range of excessive daytime sleepiness on the ESS (score >10) (Table 2). PD participants also had significantly more impairment in objective vigilance (PVT) with lower reciprocal reaction time (mean RRT) and more attentional lapses.
Visual processing outcomes
PD and HC participants did not demonstrate any significant differences in visual processing speed, as measured by UFOV® total score, subtest 1 (processing speed), subtest 2 (divided attention), or subtest 3 (selective attention) (Table 2).
Correlations
Among PD participants, bivariate analyses demonstrated a significant correlation between walking speed and pedestrian safety (TTC). However, there was no correlation between TTC and motor symptoms measured by MDS-UPDRS, indicating that gait impairment has a stronger association with performance within the VR pedestrian environment than does global motor function (Table 3). Objective vigilance as measured by the PVT (mean RRT) was also significantly correlated with pedestrian safety (TTC) and negatively correlated with hits and close calls, suggesting that patients with impaired vigilance have riskier street-crossing behavior (Table 3). There was also a negative, but not statistically significant correlation between subjective sleepiness (ESS) and pedestrian safety, such that more sleepiness was associated with riskier behavior in the PD cases (r= −0.223), but no correlation (r=0.026) in the HC. Additionally, there was a significant negative correlation between visual processing speed (UFOV®) and pedestrian safety, suggesting that those with more impaired visual processing have riskier pedestrian behavior. Dopaminergic medications, as measured by total LED, levodopa only LED, or dopamine agonist LED, did not correlate with pedestrian behavior.
Table 3.
Correlations amongst variables: Control (black, below diagonal); Parkinson’s Disease (red, above diagonal)
| TTC | Hits + Close Calls |
ESS | PVT Mean RRT |
PVT Lapses |
UFOV | Age | Walking Speed |
|
|---|---|---|---|---|---|---|---|---|
| TTC | -- | −0.787** | −0.224 | 0.552** | −0.530** | −0.404** | −0.151 | 0.684** |
| Hits + Close Calls | −0.403* | -- | 0.106 | −0.476** | 0.540** | 0.417** | 0.262 | −0.596** |
| ESS | 0.026 | −0.086 | -- | −0.493** | 0.357* | 0.179 | 0.197 | −0.178 |
| PVT Mean RRT | 0.443* | −0.212 | −0.203 | -- | −0.630** | −0.378* | −0.085 | 0.467** |
| PVT Lapses | −0.207 | 0.197 | −0.129 | −0.451* | -- | 0.546** | 0.291 | −0.426* |
| UFOV | −0.315 | 0.307 | −0.388 | −0.363 | 0.225 | -- | 0.341* | −0.266 |
| Age | −0.507** | 0.279 | −0.290 | −0.253 | 0.183 | 0.642** | -- | −0.058 |
| Walking Speed | 0.397 | −0.189 | −0.017 | 0.475* | −0.205 | −0.408* | −0.437* | -- |
Values are Pearson correlation coefficients (r)
p-value <0.01 (two-tailed)
p-value <0.05 (two-tailed)
Similar to PD participants, HCs demonstrated a significant correlation between pedestrian safety (TTC) and vigilance (PVT mean RRT). In contrast to PD, pedestrian safety among HCs was significantly correlated with age. Additionally, HC participant pedestrian safety had only a trend toward a negative correlation with visual processing speed and a trend toward a positive correlation with walking speed. As expected based on prior studies(23), visual processing speed was significantly negatively correlated with age among PD and HC participants.
The psychomotor vigilance task measuring reciprocal reaction time (RRT) was not performed on all participants because it was added after study recruitment began. To determine if the significant correlation noted between RRT and other variables in 34 PD participants could be extrapolated to the entire PD sample (n=50), an imputation was used to assess the overall dataset. A linear regression model was fit with the dependent variable as mean RRT and predictor variables of Time to Contact, Useful Field of View, Epworth Sleepiness Scale, and walking speed (F=7.164, p =0.0004). This model was used to predict reaction time for participants without observed psychomotor vigilance task values. Predicted values of reaction time correlated with the observed values (r =0.705, p <0.0001) in the 34 cases with complete data. When using the predicted values for multivariable correlation analysis, there were similar but as expected more robust correlations between all variables that showed a significant correlation with RRT in the observed values resulting from the use of RRT in the prediction of the missing values.
Predictors of Pedestrian Safety
In a stepwise multiple regression model, using a forward selection procedure, two variables were identified as being significant predictors of pedestrian safety (TTC) among PD participants. As shown in Table 4, the strongest predictor of TTC among PD patients was walking speed, accounting for 48% of variance, followed by vigilance as measured by the observed values of PVT (additional 8% of variance). As a sensitivity analysis, we ran the same model using all variables with a backward selection procedure and confirmed that the predictor variables were independent of the method of selection. Using the same approach on the HC participants, the strongest predictor of pedestrian safety among HCs was age, accounting for 27% of variance in TTC, followed by vigilance as measured by the PVT, which was selected with a p-value <0.10, and accounted for an additional 10% of variance.
Table 4.
Multiple Linear Regression with Time to Contact as dependent variable
| Parkinson’s Disease | Healthy Control | ||||||
|---|---|---|---|---|---|---|---|
| Variable | β | t | p-value | Variable | β | t | p-value |
| Walking Speed | 1.31 | 4.03 | <0.001 | Age | −0.04 | −2.40 | 0.009 |
| PVT mean RRT | 0.76 | 2.14 | 0.04 | PVT mean RRT | 0.70 | 1.91 | 0.08 |
DISCUSSION
This case-control study demonstrates that PD patients have riskier pedestrian behavior compared to age-and sex-matched HC participants when assessed within a validated pedestrian environment. This riskier behavior among PD patients is most strongly related to their slower walking speed. Additionally, PD patients have more excessive daytime sleepiness, impaired vigilance, and slower walking speed compared to controls. Among PD participants, slower walking speed, impaired vigilance, and impaired visual processing were significantly correlated with riskier pedestrian behavior; with walking speed being the most robust predictor of pedestrian safety within this environment. While impaired vigilance also correlated with riskier pedestrian behavior among HCs, age was the strongest predictor of pedestrian safety in these participants.
To our knowledge, only one other study has investigated pedestrian behavior in Parkinson’s disease(14). Similar to our findings, that study found riskier pedestrian behavior in PD compared to controls and pedestrian behavior was influenced by impaired visual processing(14). In contrast to our findings, the study by Lin and colleagues found that UPDRS motor score predicted pedestrian safety in their sample. Although walking speed was also measured in that study, the impact of this outcome on street-crossing behavior was not reported(14). Regardless, the idea that slower speed of walking could be associated with riskier pedestrian behavior is not surprising. In fact, pedestrian crosswalks in the United States assume a minimum walking speed of 3.5 feet/second (equivalent to 2.4 miles/hour)(24). In our sample, none of the HC participants, but 15 of the 50 PD participants (30%) walked slower than this speed and therefore would have difficulty safely crossing a conventional crosswalk in the United States. This suggests that public safety and traffic adjustments could improve pedestrian safety for patients with PD or other conditions that slow walking speed. This type of change is not without precedent. In fact, the 2009 parameters were changed from the 2003 rules, which assumed a minimum walking speed of 4.0 feet/sec (equivalent to 2.7 miles/hour)(25). The importance of walking speed to PD patient safety is not limited to street-crossing behavior, but prior research has also shown that this is an important predictor of fall risk(26). Therefore, patient specific interventions, such as exercise and adjustment of dopaminergic medications, both of which can improve gait speed in PD, are potential interventions for improving pedestrian safety and falls in PD(27–29).
Our study is the first to investigate correlations between pedestrian behavior and measures of vigilance and subjective sleepiness in PD. Although objective vigilance measured by PVT was significantly correlated with TTC and predicted safe pedestrian behavior in both groups, subjective sleepiness had only a trend toward a significant correlation with TTC in PD, and no correlation in HC. One potential explanation for this difference may be that participants underestimate their degree of sleepiness or the association is of a minor magnitude to be detected in a study of this size. There is slightly over 80% power to detect a correlation of 0.40 versus no correlation with a sample size N=50. Discrepancies between objective and subjective measures of sleepiness have been previously reported(30). Another possible explanation is that performance on PVT relies not only on sleepiness, but also on other cognitive aspects of attention that were not independently measured. The correlations identified in this study highlight the importance of the integration of motor function, vigilance, cognition, and visual processing for street-crossing safety.
Our findings also identify variables that differentially predict pedestrian behavior in PD and HC participants. The effects of aging on safe street-crossing behavior and on visual processing are well established(9, 10, 23), and are supported by this study as well. However, while age was the most robust predictor of pedestrian safety among HCs, this variable was not a significant predictor of pedestrian behavior among PD participants. This difference can be explained by the relative sparing of motor (walking speed) and non-motor (vigilance) functions in healthy older adults until advanced age. However, in PD, these deficits are apparent earlier as a manifestation of the disease, explaining the relative impairment of safe pedestrian behavior in PD compared to age-matched healthy adults. This idea is supported by our findings that age and walking speed were significantly correlated in HC but not PD participants, because the slowed walking was due to PD rather than age in PD participants. Another potential influence on pedestrian behavior that was not measured in this study but that could affect PD participants more than HCs includes impaired inhibition response (impulsivity)(31).
One unexpected finding in this sample was that visual processing, as measured by the UFOV®, was not significantly impaired in PD relative to HC. This is in contrast to prior studies of this outcome in PD(12, 14). Potential explanations for this difference are that, compared to these prior studies, our sample was slightly younger and had lower (better) mean total UFOV® scores for both PD and HC participants. Another possibility is that the sample size was not large enough to detect a difference, since there seems to be a trend toward poorer visual processing among PD participants. Regardless, poor performance on the UFOV® was significantly correlated with unsafe pedestrian behavior in PD participants. This was expected in light of prior studies demonstrating that deficits in visual processing and attention predict unsafe driving behavior in healthy older adults and patients with PD(32–35).
Strengths of this study include inclusion of a healthy control group and the use of the semi-immersive, validated, interactive pedestrian environment, which has been demonstrated to be a reliable measure of real-world street-crossing behavior without the dangers associated with real traffic(15). There were also potential limitations to the study. First, we had some concern that the PVT might be impaired in PD due to bradykinesia affecting reaction time. However, there was no correlation between performance on the PVT and motor scores on the UPDRS, consistent with our findings in a different sample of PD patients(36). Another limitation was that there was missing data on the PVT for several participants. Additionally, we did not measure level of education among our participants, and therefore we did not control for this factor which has influenced performance on the UFOV® in past research(23). Further, although this study measured a range of assessments that might influence pedestrian behavior, we did not include detailed cognitive assessments (such as executive function and visuospatial function), evaluation of mood, measures of freezing of gait or motor fluctuations, assessments of impulsivity or decision-making, or other variables that might affect pedestrian behavior. Also, because this pedestrian environment uses a pre-set walking speed for participants rather than having them actually walk within the VR environment, this assessment cannot measure the influence of freezing of gait or alterations in walking speed once the crossing is initiated. Finally, due to the nature of the VR pedestrian environment that required stepping up and down off the simulated curb, we excluded participants who required the use of a walking aid, such as a cane or walker, and those who are non-ambulatory. This selected for a sample of participants with somewhat less severe motor symptoms, potentially making this study less generalizable to the PD population as a whole.
In conclusion, this study evaluated the association of motor performance, vigilance, and visual processing speed with pedestrian safety in patients with PD, demonstrating that PD patients have riskier pedestrian behavior compared to age-matched healthy older adults when tested in a VR pedestrian environment. In contrast to HC participants in whom age is the most important factor, deficits in street-crossing safety in PD are related to impairments in walking speed. Therefore, interventions to improve balance and walking speed in PD may have potential to improve street-crossing behavior as well. Additionally, the correlation between visual processing deficits and pedestrian safety provides an additional avenue for exploration of tools such as speed of processing training, which have been shown to improve performance on UFOV®(37), as interventions for improving pedestrian safety in these patients. These outcomes point to the importance of optimizing motor performance and treating sleep and vigilance deficiencies in patients with PD in order to improve safety.
Acknowledgments
Study Funding: Supported by NIH grant funding from the National Institute of Neurological Disorders and Stroke (K23NS080912: AWA), National Institute on Aging (P30 AG022838, Roybal Center: AWA and KB) and National Institute of Child Health and Human Development (T32 HD071866: KHW)
We are grateful to the research participants, without whom this study would not have been possible. We would also like to thank Anna Johnston (UAB Department of Psychology) and the UAB Youth Safety Lab for assistance with data collection and Joan Severson and Digital Artefacts (Iowa City, IA) for support of the VR environment.
Dr. Ball owns stock in the Visual Awareness Research Group (formerly Visual Awareness, Inc.), and Posit Science, Inc., the companies that market the Useful Field of View Test and speed of processing training software. Posit Science acquired Visual Awareness, and Dr. Ball continues to collaborate on the design and testing of these assessments and training programs as a member of the Posit Science Scientific Advisory Board. These stocks are not publicly traded.
She has Intellectual Property Rights through patents assigned to Visual Awareness Research Group, Inc. She has Consultancies to Visual Awareness Research Group, Inc. She is employed by University of Alabama at Birmingham and has grant funding through NIH: P30 AG022838: Center for Translational Research on Aging and Mobility (PI); R01 AG021958: Predicting Long-Term Mobility Outcomes for Older Adults (PI); P30 AG031054: Deep South Resource Center for Minority Aging Research, (PI of Investigator Development Core); and DTMC7514D0001 IL-706: Examining FMCSA Vision Standard for CMV Drivers and Waiver Program (PI of Subcontract from VTTI). She has no disclosures related to expert testimony, partnerships, contracts, honoraria, or royalties.
Dr. Cutter: Data and Safety Monitoring Boards: AMO Pharmaceuticals, Apotek, Gilead Pharmaceuticals, Horizon Pharmaceuticals, Modigenetech/Prolor, Merck, Merck/Pfizer, Opko Biologics, Neuren, Sanofi-Aventis, Reata Pharmaceuticals, Receptos/Celgene, Teva pharmaceuticals, NHLBI (Protocol Review Committee), NICHD (OPRU oversight committee).Consulting or Advisory Boards: Atara Biotherapeutics, Bioeq GmBH, Cerespir Inc, Consortium of MS Centers (grant), Genzyme, Genentech, Innate Therapeutics, Jannsen Pharmaceuticals, Klein-Buendel Incorporated, Medimmune, Medday, Nivalis, Novartis, Opexa Therapeutics, Roche, Savara Inc., Somahlution, Teva pharmaceuticals, Transparency Life Sciences, TG Therapeutics. Dr. Cutter is employed by the University of Alabama at Birmingham and President of Pythagoras, Inc. a private consulting company located in Birmingham AL.
Dr. Schwebel had research funding from the following entities: National Institutes of Health, US Department of Transportation (passing through STRIDE Consortium at University of Florida), and Vipaar, Inc. (small business in Birmingham, Alabama). He has been compensated for invited lectures by Central South University (Changsha, China). He has completed paid consulting work for Marshfield Clinics (medical complex in Marshfield, Wisconsin), Harrison & Hull, LLP (law firm near Dallas, Texas), NeuRA (research institute in Sydney, Australia), Crandall & Katt (law firm in Roanoke, Virginia), and A.I.S.E. (international association based in Brussels, Belgium). He owns a variety of stocks and mutual funds for publicly traded companies as personal investments.
Dr. Amara receives grant funding from the NIH NINDS (K23 NS080912), National Institute on Aging (P30 AG022838) and the UAB Center for Clinical and Translational Science (UL1 TR00141), and is an investigator for studies sponsored by the Michael J. Fox Foundation for Parkinson’s Research and Abbvie. She serves on an advisory board for Jazz Pharmaceuticals.
Footnotes
Financial Relationships relevant to manuscript:
Miss Ford reports no disclosures.
Mr. Joop reports no disclosures.
Dr. Memon reports no disclosures.
Dr. Wood reports no disclosures.
Dr. Cutter reports no disclosures.
Dr. Schwebel reports no disclosures.
Dr. Amara reports no disclosures.
AUTHOR ROLES:
Kristin J. Ford: Research Project: organization and execution; Statistical Analysis: review and critique; Manuscript Preparation: writing the first draft and review and critique.
Allen Joop: Research Project: organization and execution; Statistical Analysis: review and critique; Manuscript Preparation: review and critique.
Raima A. Memon: Statistical Analysis: review and critique; Manuscript Preparation: review and critique.
Kimberly H. Wood: Statistical Analysis: review and critique; Manuscript Preparation: review and critique.
Karlene Ball: Research Project: conception; Statistical Analysis: review and critique; Manuscript Preparation: review and critique.
Gary R. Cutter: Research Project: conception; Statistical Analysis: design, execution, review and critique; Manuscript Preparation: review and critique.
David C. Schwebel: Research Project: conception; Statistical Analysis: review and critique; Manuscript Preparation: review and critique.
Amy W. Amara: Research Project: conception, organization and execution; Statistical Analysis: design, execution, review and critique; Manuscript Preparation: review and critique.
Disclosures last 12 months:
Miss Ford: nothing to disclose
Mr. Joop: nothing to disclose
Dr. Memon: nothing to disclose
Dr. Wood: nothing to disclose
References
- 1.Barone P, Antonini A, Colosimo C, Marconi R, Morgante L, Avarello TP, et al. The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson's disease. Mov Disord. 2009;24(11):1641–9. doi: 10.1002/mds.22643. [DOI] [PubMed] [Google Scholar]
- 2.Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR, Group NV. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson's disease. Movement disorders : official journal of the Movement Disorder Society. 2011;26(3):399–406. doi: 10.1002/mds.23462. [DOI] [PubMed] [Google Scholar]
- 3.Lees AJ, Blackburn NA, Campbell VL. The nighttime problems of Parkinson's disease. Clin Neuropharmacol. 1988;11(6):512–9. doi: 10.1097/00002826-198812000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Nausieda PA, Weiner WJ, Kaplan LR, Weber S, Klawans HL. Sleep disruption in the course of chronic levodopa therapy: an early feature of the levodopa psychosis. Clin Neuropharmacol. 1982;5(2):183–94. doi: 10.1097/00002826-198205020-00003. [DOI] [PubMed] [Google Scholar]
- 5.Naismith SL, Terpening Z, Shine JM, Lewis SJ. Neuropsychological functioning in Parkinson's disease: differential relationships with self-reported sleep-wake disturbances. Movement disorders : official journal of the Movement Disorder Society. 2011;26(8):1537–41. doi: 10.1002/mds.23640. [DOI] [PubMed] [Google Scholar]
- 6.Uc EY, Rizzo M, Anderson SW, Sparks JD, Rodnitzky RL, Dawson JD. Driving with distraction in Parkinson disease. Neurology. 2006;67(10):1774–80. doi: 10.1212/01.wnl.0000245086.32787.61. [DOI] [PubMed] [Google Scholar]
- 7.Transportation Do, editor. Analysis NCfSa. Pedestrians: 2014 data. Washington DC: National Highway Traffic Safety Administration; 2016. [Google Scholar]
- 8.European Commission D-GfMT, editor. DaCoTA. Traffic Safety Basic Facts 2011. European Road Safety Observatory; 2011. [Google Scholar]
- 9.Dommes A, Cavallo V. The role of perceptual, cognitive, and motor abilities in street-crossing decisions of young and older pedestrians. Ophthalmic Physiol Opt. 2011;31(3):292–301. doi: 10.1111/j.1475-1313.2011.00835.x. [DOI] [PubMed] [Google Scholar]
- 10.Oxley JA, Ihsen E, Fildes BN, Charlton JL, Day RH. Crossing roads safely: an experimental study of age differences in gap selection by pedestrians. Accid Anal Prev. 2005;37(5):962–71. doi: 10.1016/j.aap.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Tournier I, Dommes A, Cavallo V. Review of safety and mobility issues among older pedestrians. Accid Anal Prev. 2016;91:24–35. doi: 10.1016/j.aap.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 12.Uc EY, Rizzo M, Anderson SW, Qian S, Rodnitzky RL, Dawson JD. Visual dysfunction in Parkinson disease without dementia. Neurology. 2005;65(12):1907–13. doi: 10.1212/01.wnl.0000191565.11065.11. [DOI] [PubMed] [Google Scholar]
- 13.Knipe MD, Wickremaratchi MM, Wyatt-Haines E, Morris HR, Ben-Shlomo Y. Quality of life in young- compared with late-onset Parkinson's disease. Movement disorders : official journal of the Movement Disorder Society. 2011;26(11):2011–8. doi: 10.1002/mds.23763. [DOI] [PubMed] [Google Scholar]
- 14.Lin CH, Ou YK, Wu RM, Liu YC. Predictors of road crossing safety in pedestrians with Parkinson's disease. Accid Anal Prev. 2013;51:202–7. doi: 10.1016/j.aap.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Schwebel DC, Gaines J, Severson J. Validation of virtual reality as a tool to understand and prevent child pedestrian injury. Accid Anal Prev. 2008;40(4):1394–400. doi: 10.1016/j.aap.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson's disease. Mov Disord. 2010;25(15):2649–53. doi: 10.1002/mds.23429. [DOI] [PubMed] [Google Scholar]
- 17.O'Neal EE, King R, Shingareva K, Davis AL, Schwebel DC. Participant familiarization and orientation in virtual reality environments. International Society for Child and Adolescent Injury Prevention. 2010 [Poster presentation]. In press. [Google Scholar]
- 18.Fahn S, Elton RL. Members of the UPDRS Development Committee: The Unified Parkinson's Disease Rating Scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M, editors. Recent Developments in Parkinson's Disease. Florham Park: Macmillan Healthcare Information; 1987. pp. 153–63. [Google Scholar]
- 19.Ball K, Owsley C, Beard B. Clinical Visual Perimetry Underestimates Peripheral Field Problems in Older Adults. Clinical Vision Sciences. 1990;5(2):113–25. [Google Scholar]
- 20.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 21.Dinges DF. Microcomputer analysis of performance on a portable, simple visual RT task during sustained operations. Behavioral Research Methods, Instruments, & Computers. 1985;17(6):652–5. [Google Scholar]
- 22.Basner M, Dinges DF. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep. 2011;34(5):581–91. doi: 10.1093/sleep/34.5.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edwards JD, Ross LA, Wadley VG, Clay OJ, Crowe M, Roenker DL, et al. The useful field of view test: normative data for older adults. Arch Clin Neuropsychol. 2006;21(4):275–86. doi: 10.1016/j.acn.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Administration USDoTFH, editor. Manual on Uniform Traffic Control Devices (MUTCD) Washington, DC: 2009. [Google Scholar]
- 25.Administration USDoTFH, editor. Manual on Uniform Traffic Control Devices (MUTCD) Washington, DC: 2003. [Google Scholar]
- 26.Nemanich ST, Duncan RP, Dibble LE, Cavanaugh JT, Ellis TD, Ford MP, et al. Predictors of gait speeds and the relationship of gait speeds to falls in men and women with Parkinson disease. Parkinsons Dis. 2013;2013:141720. doi: 10.1155/2013/141720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bryant MS, Rintala DH, Hou JG, Lai EC, Protas EJ. Effects of levodopa on forward and backward gait patterns in persons with Parkinson's disease. NeuroRehabilitation. 2011;29(3):247–52. doi: 10.3233/NRE-2011-0700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Combs SA, Diehl MD, Chrzastowski C, Didrick N, McCoin B, Mox N, et al. Community-based group exercise for persons with Parkinson disease: a randomized controlled trial. NeuroRehabilitation. 2013;32(1):117–24. doi: 10.3233/NRE-130828. [DOI] [PubMed] [Google Scholar]
- 29.Allen NE, Sherrington C, Paul SS, Canning CG. Balance and falls in Parkinson's disease: a meta-analysis of the effect of exercise and motor training. Mov Disord. 2011;26(9):1605–15. doi: 10.1002/mds.23790. [DOI] [PubMed] [Google Scholar]
- 30.Chung S, Bohnen NI, Albin RL, Frey KA, Muller ML, Chervin RD. Insomnia and sleepiness in Parkinson disease: associations with symptoms and comorbidities. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2013;9(11):1131–7. doi: 10.5664/jcsm.3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hart RP, Wade JB, Calabrese VP, Colenda CC. Vigilance performance in Parkinson's disease and depression. J Clin Exp Neuropsychol. 1998;20(1):111–7. doi: 10.1076/1380-3395(199802)20:1;1-P;FT111. [DOI] [PubMed] [Google Scholar]
- 32.Bowers AR, Anastasio RJ, Sheldon SS, O'Connor MG, Hollis AM, Howe PD, et al. Can we improve clinical prediction of at-risk older drivers? Accid Anal Prev. 2013;59:537–47. doi: 10.1016/j.aap.2013.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clay OJ, Wadley VG, Edwards JD, Roth DL, Roenker DL, Ball KK. Cumulative meta-analysis of the relationship between useful field of view and driving performance in older adults: current and future implications. Optom Vis Sci. 2005;82(8):724–31. doi: 10.1097/01.opx.0000175009.08626.65. [DOI] [PubMed] [Google Scholar]
- 34.Classen S, McCarthy DP, Shechtman O, Awadzi KD, Lanford DN, Okun MS, et al. Useful field of view as a reliable screening measure of driving performance in people with Parkinson's disease: results of a pilot study. Traffic Inj Prev. 2009;10(6):593–8. doi: 10.1080/15389580903179901. [DOI] [PubMed] [Google Scholar]
- 35.Uc EY, Rizzo M, Johnson AM, Dastrup E, Anderson SW, Dawson JD. Road safety in drivers with Parkinson disease. Neurology. 2009;73(24):2112–9. doi: 10.1212/WNL.0b013e3181c67b77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amara AW, Walker HC, Joop A, Cutter G, DeWolfe JL, Harding SM, et al. Effects of Subthalamic Nucleus Deep Brain Stimulation on Objective Sleep Outcomes in Parkinson's Disease. Movement Disorders Clinical Practice. 2016 doi: 10.1002/mdc3.12375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Edwards JD, Hauser RA, O'Connor ML, Valdes EG, Zesiewicz TA, Uc EY. Randomized trial of cognitive speed of processing training in Parkinson disease. Neurology. 2013;81(15):1284–90. doi: 10.1212/WNL.0b013e3182a823ba. [DOI] [PMC free article] [PubMed] [Google Scholar]