Abstract
Background
This study analyzed the effect of preoperative T1 slope on cervical alignment and range of motion (ROM) after cervical disc arthroplasty (CDA) in patients with cervical degenerative disease.
Material/Methods
This retrospective study included 32 patients with single-level symptomatic cervical disc disease who underwent CDA with the Mobi-C cervical disc prosthesis and had a mean follow-up of 26.8±6.4 months. Standing lateral, flexion, and extension X-rays of the cervical spine were obtained preoperatively and postoperatively at 24-month follow-up. Simple linear regression analysis was used to assess the impact of preoperative T1 slope on changes from preoperative values in radiologic parameters.
Results
Compared to preoperative values, at 24-month follow-up, there was a significant increase in mean functional spinal unit (FSU) angle (+7.4°), upper adjacent segment (UAS) angle (+3.1°), and overall cervical alignment (C2–C7 angle) (+6.3°), and a significant decrease in mean lower adjacent segment (LAS) angle (−2.4°). Mean ROM of the FSU (−3.6°), LAS (−3.0°), and overall cervical spine (−11.5°) significantly decreased, and mean ROM of the UAS (+1.6°) significantly increased. There were significant correlations between preoperative T1 slope and mean change from preoperative value in FSU angle, C2–C7 angle, and ROM of the overall cervical spine (C2–C7).
Conclusions
T1 slope is useful for evaluating changes in the FSU angle, C2–C7 angle, and ROM of the overall cervical spine following CDA with the Mobi-C disc. Patients with a large preoperative T1 slope may be good candidates for CDA with the Mobi-C prosthesis due its motion maintenance and the fact that it has little adverse impact on sagittal alignment. It also could be a good option in terms of sagittal alignment improvement or motion maintenance for patients with kyphosis.
MeSH Keywords: Radiculopathy; Range of Motion, Articular; Total Disc Replacement
Background
Cervical disc arthroplasty (CDA) is a safe and effective alternative to anterior cervical discectomy and fusion (ACDF) for single-level cervical radiculopathy or myelopathy due to disc herniation or focal uncovertebral osteophyte formation [1–3]. Compared to ACDF, CDA preserves motion of the operative level, with the hope that may reduce adjacent level degeneration [4–6].
Normal cervical alignment is critically important for maintaining neutral head position, and malalignment is usually associated with neck pain and functional disability [7,8]. Many radiological parameters have been used to evaluate cervical spine sagittal balance, including C2–C7 lordosis, C0–C2 lordosis, and the sagittal vertical axis (SVA), as well as T1 slope [8–10]. T1 slope is considered critical to cervical sagittal balance [3], and several studies have shown correlations between preoperative T1 slope and cervical spine sagittal balance after laminoplasty [11,12] or posterior atlantoaxial fusion [13]. To the best of our knowledge, no study has investigated the relationship between preoperative T1 slope and postoperative cervical sagittal balance and range of motion (ROM) following CDA. Therefore, the objective of this study was to analyze the effect of preoperative T1 slope on cervical balance and ROM after CDA with the Mobi-C prosthesis.
Material and Methods
Patients with single-level symptomatic cervical disc disease who underwent CDA with the Mobi-C cervical disc prosthesis (LDR Spine USA, Inc., Austin, TX, USA) were eligible for this retrospective radiologic study. Inclusion criteria were: 1) radiculopathy or myelopathy secondary to single-level cervical disc herniation between C3/C4 and C6/C7; 2) no or small (an osteophyte did not influence the ROM of the functional spinal unit [FSU]) osteophytes; 3) resistant to conservative treatment for more than 3 months; and 4) follow-up ≥24 months. Exclusion criteria were: 1) severe disc calcification; 2) ossification of the posterior longitudinal ligament; 3) osteoporosis or metabolic bone disease; 4) previous cervical spine surgery; 5) traumatic or tumoral disease; or 6) instability.
Standing lateral radiographs of the cervical spine in neutral position, full flexion and extension were obtained through Penning’ method preoperatively and postoperatively at 24-month follow-up. Lateral radiographs in neutral position were obtained with the patient standing in an upright position, head facing forward with a horizontal gaze, and upper extremities falling naturally at the side of the trunk. Full flexion-extension radiographs were obtained with the patients bending the head forward and extending backward as much as possible without moving the thoracic spine [14]. Measurements were performed using the hospital’s Picture Archiving and Communication System (PACS). All radiologic parameters were measured twice at 1-month intervals by 2 researchers who were not involved in the surgical procedures. Mean values were calculated and used in the statistical analyses.
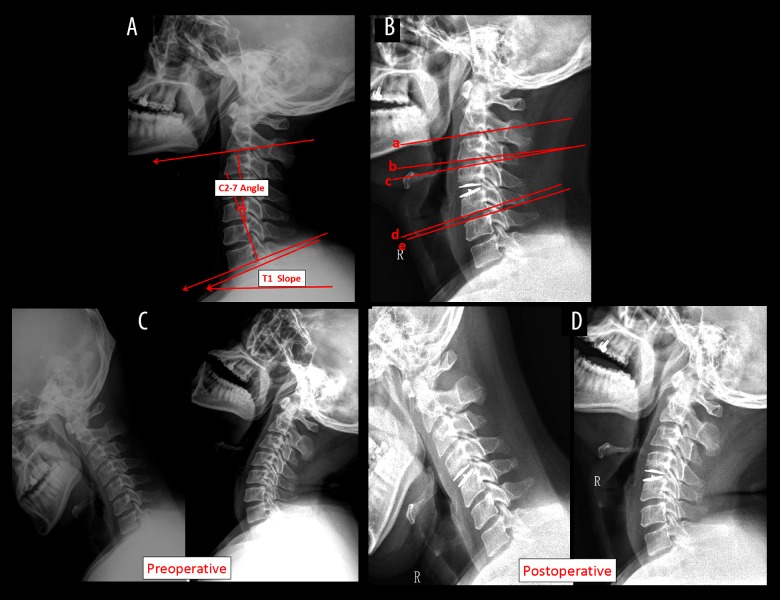
Preoperative T1 slope, preoperative and postoperative overall cervical alignment (C2–C7 angle), FSU angle, and upper and lower adjacent segment (UAS/LAS) angles were measured on lateral radiographs. Preoperative and postoperative ROM of the FSU, UAS, LAS, overall upper segment, and overall cervical spine (C2–C7) were measured on extension-flexion radiographs. T1 slope was defined as the angle between the upper endplate of T1 and the horizontal line. The C2–C7 angle was defined by the Cobb angle between the lower endplates of C2 and C7. The FSU angle was defined by the Cobb angle between the superior endplate of the cephalad vertebral body and the inferior endplate of the caudal vertebral body with the disc prosthesis. The UAS angle was defined by the Cobb angle between the superior endplate of the cephalad vertebral body with the disc prosthesis and the inferior end plate of the upper adjacent vertebral body. The LAS angle was defined by the Cobb angle between the inferior endplate of the caudal vertebral body with the disc prosthesis and the superior endplate of the lower adjacent vertebral body. ROM was measured in full flexion and full extension radiographs (Figure 1).
Figure 1.
Lateral radiograph: (A) T1 slope and C2–C7 angle. (B) FSU angle: angle between c and d; UAS angle: angle between b and c; LAS angle: angle between d and e. (C) Preoperative ROM. (D) Postoperative ROM. FSU – functional spinal unit; UAS – upper adjacent segment; LAS – lower adjacent segment; ROM – range of motion.
Statistical analyses
Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS) 17.0. Results are reported as mean ± standard deviation. For each radiographic parameter, the paired-samples t test was used to compare preoperative and postoperative values. Pearson line correlation analysis was used to assess the correlation between preoperative and postoperative values. Simple linear regression analysis was conducted to assess the impact of preoperative T1 slope on change from preoperative values in radiologic parameters. Statistical significance was set at P<0.05. The intraclass correlation coefficient (ICC) for intra- and inter-observer reliability was evaluated by a one-way random effects model to assess the reproducibility of each researcher and the overall agreement among the researchers for each parameter measured. A post hoc statistical power analysis was performed using G*Power 3.1 [15].
Results
This study included 32 patients (18 males and 14 females) with single-level cervical disc herniation who underwent CDA. Mean age of the patients was 43.5±4.7 years (range: 36–51 years), and mean follow-up was 26.8±6.4 months (range: 24–32 months). There were 29 patients with no osteophytes and 3 patients with small osteophytes. Twelve patients had preoperative FSU kyphosis (positive conversion of angle amount measured through lateral radiography), 16 patients had preoperative UAS kyphosis, 2 patients had preoperative LAS kyphosis, and 9 patients had preoperative C2–C7 kyphosis. Eight patients underwent single-level CDA at C4–C5, 22 patients underwent single-level CDA at C5–C6, and 2 patients underwent single-level CDA at C6–C7. No patient had postoperative FSU or C2–C7 kyphosis, 5 patients had postoperative UAS kyphosis, and 4 patients had postoperative LAS kyphosis. No complications occurred in any patient in the present study (Table 1).
Table 1.
Patients’ demographic and clinical characteristics.
| Mean | SD | Min | Max | |
|---|---|---|---|---|
| Age (years) | 43.5 | 4.7 | 36 | 51 |
| Gender | 18 Male, 14 Female | |||
| Follow-up (months) | 26.8 | 6.4 | 24 | 32 |
| Surgery duration (min) | 72.4 | 17.7 | 45 | 110 |
| Blood loss (ml) | 56.2 | 25.3 | 20.6 | 105 |
| Hospital stay (days) | 4.4 | 1.6 | 2 | 7 |
| Reoperation(s) | – | – | – | – |
Postoperatively, at 24-month follow-up, the FSU angle (preoperative −0.68±6.66° vs. postoperative 7.36±3.29°, P=0.001), UAS angle (preoperative 0.53±5.65° vs. postoperative 3.68 ± 5.40°, P<0.001), and overall cervical alignment (C2–C7 angle; preoperative 11.51±13.45° vs. postoperative 17.83±8.69°, P<0.001) were significantly increased, and the LAS angle (preoperative 4.22±2.62° vs. postoperative 1.82±2.81°, P<0.0001) was significantly decreased, compared to preoperative values (Table 2).
Table 2.
Paired-samples T test analysis at last follow-up.
| Variables (degrees) | Preoperative period | Last follow-up | P* | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N=32 | Mean | Min | Max | SD | Mean | Min | Max | SD | |
| FSU alignment | −0.68 | −14.0 | 12.6 | 6.66 | 7.36 | 3 | 15 | 3.29 | 0.001 |
| UAS alignment | 0.53 | −7.5 | 12.2 | 5.65 | 3.68 | −5 | 13.6 | 5.40 | <0.001 |
| LAS alignment | 4.22 | −2 | 7.5 | 2.62 | 1.82 | −5.3 | 5.5 | 2.81 | <0.001 |
| C2–C7 alignment | 11.51 | −7.1 | 29.5 | 13.45 | 17.83 | 0.5 | 28.5 | 8.69 | <0.001 |
| ROM of FSU | 13.31 | 4.5 | 27.5 | 7.11 | 9.70 | 4.0 | 21.2 | 5.52 | <0.001 |
| ROM of UAS | 9.18 | 2.7 | 17.7 | 4.84 | 10.77 | 4.8 | 18.7 | 4.36 | <0.001 |
| ROM of LAS | 8.56 | 4.0 | 16.5 | 3.63 | 5.53 | 2.0 | 8.9 | 1.98 | <0.001 |
| ROM of C2–C7 | 51.03 | 32.5 | 79.1 | 13.72 | 39.57 | 19.7 | 60.5 | 10.69 | 0.001 |
P values are from T test.
Max – maximum; Min – minimum; FSU – functional spinal unit; UAS – upper adjacent segment; LAS – lower adjacent segment; ROM – range of motion.
Postoperatively, at the last follow-up, mean ROM of the FSU (preoperative 13.31±7.11° vs. postoperative 9.70±5.52°, P<0.001), LAS (preoperative 8.56±3.63° vs. postoperative 5.53±1.98°, P<0.001) and C2–C7 (preoperative 51.03±13.72° vs. postoperative 39.57±10.69°, P=0.001) was significantly decreased, and mean ROM of the UAS (preoperative 9.18±4.84° vs. postoperative 10.77±4.36°, P<0.001) was significantly increased, compared to preoperative values.
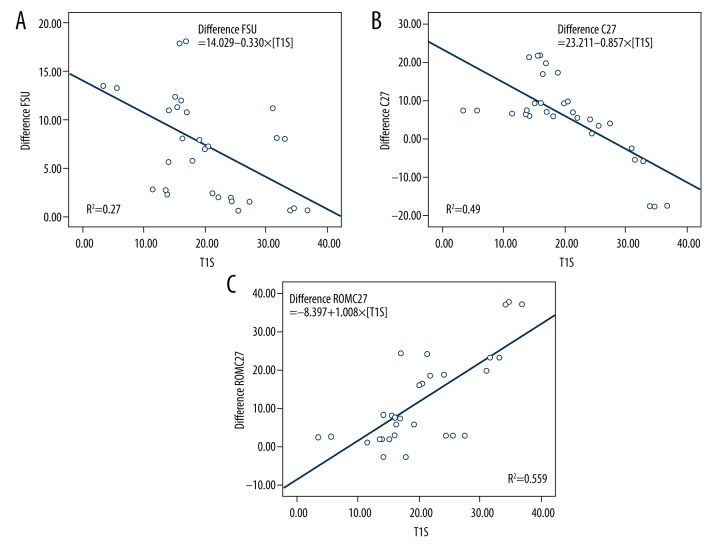
There was a significant negative correlation between preoperative T1 slope and the change from preoperative value in the FSU angle (R2=0.270, P=0.002) and C2–C7 angle (R2=0.490, P<0.001), and a significant positive correlation between preoperative T1 slope and the change from preoperative value in ROM of the overall cervical spine (R2=0.559, P<0.001) (Table 3, Figure 2).
Table 3.
Linear regression analysis of the effects of preoperative T1 slope on the change from preoperative value in various parameters.
| Difference of parameter | R2 | Adjusted R2 | P* |
|---|---|---|---|
| FSU alignment | 0.270 | 0.246 | 0.002 |
| UAS alignment | 0.035 | 0.003 | 0.305 |
| LAS alignment | 0.024 | −0.008 | 0.396 |
| C2–C7 alignment | 0.490 | 0.473 | <0.001 |
| ROM of FSU | 0.063 | 0.032 | 0.166 |
| ROM of UAS | 0.001 | −0.032 | 0.836 |
| ROM of LAS | 0.013 | −0.020 | 0.533 |
| ROM of C2–C7 | 0.559 | 0.544 | <0.001 |
FSU – functional spinal unit; UAS – upper adjacent segment; LAS – lower adjacent segment; ROM – range of motion.
Figure 2.
Linear regression analysis: (A) T1 slope vs. change from preoperative value in FSU angle; (B) T1 slope vs. change from preoperative value in C2–C7 alignment; (C) T1 slope vs. change from preoperative value in C2–C7 ROM. FSU – functional spinal unit; ROM – range of motion.
Intra-observer reliability ranged from 0.91 to 0.94 and inter-observer reliability ranged from 0.82 to 0.91. Post hoc statistical power analysis showed a power >0.9 for all the differences between preoperative and postoperative parameters except for ROM of UAS (0.6). Power for the correlations between preoperative T1 slope and the change from preoperative value in the FSU angle, C2–C7 angle, and ROM of the overall cervical spine was 0.84, 0.99, and 0.99, respectively.
Discussion
ACDF is the current criterion standard for surgical management of patients with single-level cervical disc disease and cervical spondylosis. CDA is an advanced alternative technique that is increasingly used in degenerative disc disease, especially in young patients [5,16]. Compared to ACDF, CDA reduces the incidence of long-term complications associated with spinal fusion procedures and preserves motion. The effectiveness of CDA in cervical degenerative disc disease is widely reported [5,17–19]. Many researchers have focused on the change in cervical alignment after CDA [4,18,20]. Early follow-up outcomes after treatment of degenerative cervical disc disease with the Discover cervical disc prosthesis [5] showed that CDA increased ROM of the FSU and maintained the FSU angle postoperatively. T1 slope is increasingly recognized as an important factor that influences cervical spine sagittal balance. Previous studies have evaluated correlations between T1 slope and cervical spine sagittal balance after laminoplasty [10,11] and posterior atlantoaxial fusion [12]. The current study aimed to investigate the correlations between preoperative T1 slope and change from preoperative values in radiologic parameters after CDA.
Evidence suggests that sagittal balance makes a more important contribution to operative and adjacent segmental longevity than preservation of ROM [21]; therefore, cervical disc prostheses must maintain cervical lordosis. Although most artificial cervical prosthetics are not intended to restore lordosis, restoration of cervical lordosis after CDA has been reported [22]. In the current study, there were significant negative correlations between preoperative T1 slope and changes in FSU and C2–C7 angle. We speculate that the Mobi-C disc distracts the intervertebral space and restores cervical lordosis. Patients with preoperative kyphosis, whether it is regional or overall, tend to have lower T1 slope compared with those without kyphosis. This kyphotic phenomenon was expected to improve through CDA switching. According to our analytics, patients with low T1 slope had larger changes in the FSU and C2–C7 angle, which was helpful to restore sagittal alignment in patients with kyphosis. Patients with good T1 slope usually had good cervical lordosis [12]. As such, the Mobi-C disc may be a good candidate for use in patients with a larger preoperative T1 slope, as they had smaller changes in the FSU and C2–C7 angle. It also could be a good option for patients with kyphosis in terms of restoration of sagittal alignment.
In the current study, there was a significant positive correlation between preoperative T1 slope and the change from preoperative value in the ROM of the overall cervical spine after CDA; a larger preoperative T1 slope resulted in a greater change in C2–C7 ROM. Because an important advantage of CDA is preserving motion, these data also support the use of the Mobi-C prosthesis in patients with a large preoperative T1 slope.
Maintenance of spinal motion is a primary goal and a fundamental benefit of CDA. Previous studies have shown increased motion, whereas others have shown no change or decreased motion following CDA [22]. In our study, mean ROM of the FSU, LAS, and C2–C7 decreased postoperatively, while mean ROM of the UAS increased. The Mobi-C CDA procedure is associated with high rates of heterotopic ossification (HO) [23]. HO, a well-known complication of CDA, is defined as formation of bone outside the skeletal system, with unknown etiology. In a retrospective study, Yi et al. [24] reported male sex (odds ratio [OR] of 2.117) and device type (OR of 5.262 and 7.449 for Mobi-C and ProDisc-C, respectively) were correlated with rate of HO [25]. In a recently published review of CDA, the Mobi-C disc had the highest rate of HO (n=7 studies; 62–94.1%), followed by the ProDisc-C disc (n=11 studies; 2.9–88%), the Bryan disc (n=40 studies; 0–17.8%), and the Prestige disc (n=7 studies; 0–3.2%) [26]. In the current study, ROM of the FSU was decreased at the last follow-up potentially due to HO; to compensate, ROM of the UAS increased, which may contribute to the development of ASD as the fusion operation. However, as it preserves a portion of the operative-level ROM, CDA may have less contribution to the ASD than fusion operation.
This study has several limitations. First, although the power sample analysis showed the results are reliable, the number of the patients included is small; therefore, the data should be interpreted with caution. Second, the follow-up period of the patients in this study was short, and a longer follow-up period is required to confirm our findings.
Conclusions
The results of this study suggest that T1 slope is useful for evaluating changes in the FSU angle, C2–C7 angle, and ROM of the overall cervical spine following CDA with the Mobi-C disc. Patients with good preoperative T1 slope may be good candidates for CDA with the Mobi-C prosthesis due to its motion maintenance and the fact that it has little adverse impact on sagittal alignment. It also could be a good option in terms of sagittal alignment improvement or motion maintenance for patients with kyphosis.
Footnotes
Source of support: Departmental sources
References
- 1.Heller JG, Sasso RC, Papadopoulos SM, et al. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: Clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 2009;34(2):101–7. doi: 10.1097/BRS.0b013e31818ee263. [DOI] [PubMed] [Google Scholar]
- 2.Mummaneni PV, Burkus JK, Haid RW, et al. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: A randomized controlled clinical trial. J Neurosurg Spine. 2007;6(3):198–209. doi: 10.3171/spi.2007.6.3.198. [DOI] [PubMed] [Google Scholar]
- 3.Murrey D, Janssen M, Delamarter R, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9(4):275–86. doi: 10.1016/j.spinee.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Kim SW, Paik SH, Castro PA, et al. Analysis of factors that may influence range of motion after cervical disc arthroplasty. Spine J. 2010;10(8):683–88. doi: 10.1016/j.spinee.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 5.Du J, Li M, Liu H, et al. Early follow-up outcomes after treatment of degenerative disc disease with the discover cervical disc prosthesis. Spine J. 2011;11(4):281–89. doi: 10.1016/j.spinee.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 6.Buckland AJ, Baker JF, Roach RP, Spivak JM. Cervical disc replacement – emerging equivalency to anterior cervical discectomy and fusion. Int Orthop. 2016;40(6):1329–34. doi: 10.1007/s00264-016-3181-8. [DOI] [PubMed] [Google Scholar]
- 7.Ma Z, Liu P, Liu J, et al. Kinematic analysis of the relationship between Modic changes and sagittal balance parameters in the cervical spine. Medicine (Baltimore) 2017;96(33):e7699. doi: 10.1097/MD.0000000000007699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang ZL, Xiao JL, Mou JH, et al. Analysis of cervical sagittal balance parameters in MRIs of patients with disc-degenerative disease. Med Sci Monit. 2015;21:3083–88. doi: 10.12659/MSM.893715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10(11):994–98. doi: 10.1016/j.spinee.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 10.Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: Comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38(22 Suppl 1):S149–60. doi: 10.1097/BRS.0b013e3182a7f449. [DOI] [PubMed] [Google Scholar]
- 11.Cho JH, Ha JK, Kim DG, et al. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine (Phila Pa 1976) 2014;39(26):E1575–81. doi: 10.1097/BRS.0000000000000614. [DOI] [PubMed] [Google Scholar]
- 12.Kim TH, Lee SY, Kim YC, et al. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 2013;38(16):E992–97. doi: 10.1097/BRS.0b013e3182972e1b. [DOI] [PubMed] [Google Scholar]
- 13.Guo Q, Deng Y, Wang J, et al. Influence of the T1-slope on sagittal alignment of the subaxial cervical spine after posterior atlantoaxial fusion in os odontoideum. Clin Neurol Neurosurg. 2016;149:39–43. doi: 10.1016/j.clineuro.2016.07.025. [DOI] [PubMed] [Google Scholar]
- 14.Dvorak J1, Froehlich D, Penning L, et al. Functional radiographic diagnosis of the cervical spine: Flexion/extension. Spine (Phila Pa 1976) 1988;13(7):748–55. doi: 10.1097/00007632-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 16.Yan SZ, Di J, Shen Y. Adjacent segment degeneration following anterior cervical discectomy and fusion versus the bryan cervical disc arthroplasty. Med Sci Monit. 2017;23:2692–700. doi: 10.12659/MSM.905178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sasso RC, Smucker JD, Hacker RJ, Heller JG. Artificial disc versus fusion: A prospective, randomized study with 2-year follow-up on 99 patients. Spine (Phila Pa 1976) 2007;32(26):2933–40. doi: 10.1097/BRS.0b013e31815d0034. discussion 9941–42. [DOI] [PubMed] [Google Scholar]
- 18.Sasso WR, Smucker JD, Sasso MP, Sasso RC. Long-term clinical outcomes of cervical disc arthroplasty: A prospective, randomized, controlled trial. Spine (Phila Pa 1976) 2017;42(4):209–16. doi: 10.1097/BRS.0000000000001746. [DOI] [PubMed] [Google Scholar]
- 19.Li J, Liang L, Ye XF, et al. Cervical arthroplasty with Discover prosthesis: Clinical outcomes and analysis of factors that may influence postoperative range of motion. Eur Spine J. 2013;22(10):2303–9. doi: 10.1007/s00586-013-2897-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zang L, Ma M, Hu J, et al. Comparison of hybrid surgery incorporating anterior cervical discectomy and fusion and artificial arthroplasty versus multilevel fusion for multilevel cervical spondylosis; A meta-analysis. Med Sci Monit. 2015;21:4057–67. doi: 10.12659/MSM.896584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fong SY, DuPlessis SJ, Casha S, Hurlbert RJ. Design limitations of Bryan disc arthroplasty. Spine J. 2006;6(3):233–41. doi: 10.1016/j.spinee.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Park DK, Lin EL, Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion: In vivo quantitative radiographic analysis. Spine (Phila Pa 1976) 2011;36(9):721–30. doi: 10.1097/BRS.0b013e3181df10fc. [DOI] [PubMed] [Google Scholar]
- 23.Alvin MD, Mroz TE. The Mobi-C cervical disc for one-level and two-level cervical disc replacement: A review of the literature. Med Devices (Auckl) 2014;7:397–403. doi: 10.2147/MDER.S54497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yi S, Kim KN, Yang MS, et al. Difference in occurrence of heterotopic ossification according to prosthesis type in the cervical artificial disc replacement. Spine (Phila Pa 1976) 2010;35(16):1556–61. doi: 10.1097/BRS.0b013e3181c6526b. [DOI] [PubMed] [Google Scholar]
- 25.Yi S, Shin DA, Kim KN, et al. The predisposing factors for the heterotopic ossification after cervical artificial disc replacement. Spine J. 2013;13(9):1048–54. doi: 10.1016/j.spinee.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 26.Alvin MD, Abbott EE, Lubelski D, et al. Cervical arthroplasty: A critical review of the literature. Spine J. 2014;14(9):2231–45. doi: 10.1016/j.spinee.2014.03.047. [DOI] [PubMed] [Google Scholar]