Abstract
Purpose:
Choledochocystolithiasis and its associated complications such as cholangitis and pancreatitis are managed by endoscopic retrograde cholangiography (ERC), with endoscopic stone extraction followed by laparoscopic cholecystectomy (LC). However, affected patients present with complex conditions linked to operative difficulties in performing LC. The aim of this study was to elucidate the predictive factors for a prolonged LC procedure following ERC for treating patients with choledochocystolithiasis.
Materials and Methods:
The medical records of 109 patients who underwent LC after ERC for choledochocystolithiasis from September 2012 to August 2014 were evaluated retrospectively. The cases were divided into long and short operative duration groups using a cutoff operative time of 90 minutes. We used univariate and multivariate analyses to investigate predictive factors associated with long operative duration according to clinical variables, ERC-related factors, and peak serum levels of laboratory test values between the initial presentation and LC (intervening period).
Results:
Seventeen patients needed >90 min to complete LC. The presence of acute cholecystitis, placement of percutaneous transhepatic gallbladder drainage, higher peak serum white blood cell count and levels of C-reactive protein (CRP), and lower peak serum levels of lipase during the intervening period were associated with prolonged operative duration. Multivariate analysis showed that the independent predictive factors for long operative duration were the presence of acute cholecystitis (hazard ratio, 5.418; P=0.016) and higher peak levels of CRP (hazard ratio, 1.077; P=0.022).
Conclusion:
When patients with choledochocystolithiasis are scheduled for LC after ERC, the presence of acute cholecystitis and high CRP levels during the intervening period could predict a protracted operation.
Key Words: choledochocystolithiasis, laparoscopic cholecystectomy, operative duration
Although some alternative approaches have been proposed for the treatment of patients with combined choledochocystolithiasis, endoscopic retrograde cholangiography (ERC) with endoscopic stone extraction followed by laparoscopic cholecystectomy (LC) is the preferred treatment. Baucom et al1 has conducted a web-based survey regarding on the management of choledochocystolithiasis and showed that most surgeons preferred preoperative ERC rather than performing laparoscopic common bile duct (CBD) exploration for preoperatively known CBD stones.
When performing LC after ERC, conditions of adhesion, inflammation, and fibrosis near the gallbladder generate difficulties for surgeons2,3 for the following reasons. First, stones in the CBD may induce acute cholangitis and pancreatitis, leading to difficulties in dissection of the gallbladder. Second, endoscopic procedures such as contrast infusion, sphincterotomy, stent insertion, and repeated procedures can be applied in different manners according to each patient’s situation, and these can induce biliary contamination. In addition, such procedures can evoke more intense inflammatory reactions than that of the initial presentation. Last, acute cholecystitis can develop concomitantly with stones in the CBD before ERC or after endoscopic stone removal, which is another cause of a difficult cholecystectomy. Therefore, all of these situations should be considered when aiming to perform successful LC, and the clinical effects of ongoing inflammatory events and the intensity of inflammation in cases of LC after ERC need to be clearly demonstrated.
The aim of this retrospective study was to identify factors predicting long operations in patients who underwent preoperative ERC for coexisting gallbladder and CBD stones. In addition, peak levels of laboratory test parameters reflecting the intensity of inflammation were evaluated to clarify their clinical significance as predictive factors.
MATERIALS AND METHODS
Patients
The records of 109 patients who underwent LC following ERC with endoscopic stone removal for choledochocystolithiasis from September 2012 to August 2014 were included in this study. We excluded patients with biliary malignancy or any inflammatory diseases affecting systemic inflammatory responses. Before or after ERC for CBD stones, a percutaneous transhepatic gallbladder drainage (PTGBD) catheter was placed selectively when the patients presented with moderate to severe acute cholecystitis meeting the 2007 Tokyo guidelines.4 In cases of mild cholecystitis, a PTGBD was inserted in patients with comorbidities needing further evaluations or with serum levels of >200 IU/L of aspartate aminotransferase (AST) or alanine aminotransferase (ALT). A PTGBD was also placed in some patients to decompress obstructed biliary tract, regardless of the presence of cholecystitis.5
Acute cholecystitis and cholangitis were defined according to the Tokyo guidelines,6,7 and acute pancreatitis was diagnosed when the patients presented with >2 of the following 3 features: upper abdominal pain; serum lipase or amylase activity at least 3 times greater than the upper limits of normal; and characteristic findings of acute pancreatitis on imaging studies.8 White blood cell (WBC) counts and serum levels of AST, ALT, alkaline phosphatase, amylase, lipase, total bilirubin, and C-reactive protein (CRP) were measured routinely immediately before ERC. These laboratory parameters were followed up serially until the patients showed clinical improvements. When the gallbladder-linked and CBD stone-induced symptoms recurred before performing LC, these parameters were checked again.
ERC and LC Procedures
A single expert endoscopist performed all ERC procedures. In all patients, a cholangiogram was obtained using fluoroscopy (SonialVision Safire 17; Shimadzu Co., Kyoto, Japan), and endoscopic sphincterotomy was performed to extract the CBD stones using a basket or balloon catheter. Endoscopic nasobiliary drainage or endoscopic retrograde biliary drainage was done if there was a possibility of retained stones or for biliary decompression in patients who had evidence of obstructive jaundice or severe cholangitis at the time of ERC. In addition, pancreatic stent placement was performed for patients at high risk of pancreatitis after ERC.9
LC was performed with the patient under general anesthesia by 1 surgeon who had experience in ≥200 laparoscopic cholecystectomies annually. Most patients received classic 3-port LC with retrograde dissection. When the operation needed a clearer surgical view because of adhesions or inflammatory changes around the gallbladder, another 5-mm trocar was placed below the right costal margin in the midaxillary line. Antegrade gallbladder dissection was performed for those patients with severe inflammation or fibrotic changes that obscured the surgical anatomy at Calot’s triangle.10 The cystic duct was mostly closed by double clipping using 2 different materials: nonabsorbable polymeric clips (Hem-o-lok; Weck Closure Systems, Research Triangle Park, NC) or titanium surgical clips. When the cystic duct was too wide for clipping, an endoloop was used for secure closure.
Predictive Factors for Long Operative Duration
The patients were divided into long and short operative duration groups using a cutoff operative time of 90 minutes which was associated with increased infectious complication rates after LC11 and we evaluated predictive factors for a long operative duration. Medical information including age, gender, body mass index, presence of CBD stone-induced complications such as acute pancreatitis or acute cholangitis, presence of acute cholecystitis, and placement of PTGBD were reviewed. To clarify the clinical influence of laboratory changes on operative duration, peak serum levels of laboratory tests obtained between the initial presentation and LC (defined here as the intervening period) were analyzed. ERC procedure-related factors such as the numbers of attempts, any insertion of stents, and the time interval between ERC and LC were included for the analysis of prolonged operative durations.
Statistical Analysis
Student independent t tests were used to compare the differences between means of continuous variables, and categorical variables were subjected to χ2 analysis if the sample size was adequate, or Fisher exact test if the sample was small. Variables with P-values <0.2 by univariate analysis were further analyzed by logistic regression analysis to identify independent predictors for a prolonged operation. All variables were checked for multicollinearity to guarantee independence of the predictors. Subsequently, a cutoff point for an independent predicting factor for long operative duration was determined using a receiver-operating characteristic (ROC) curve. The best cutoff value was defined as the value with the highest sum of sensitivity and specificity on the ROC curve. Statistical analyses were performed using IBM SPSS statistics for Windows (version 20.0; IBM Corp., Armonk, NY), and P<0.05 was considered statistically significant. Results are presented as the hazard ratio (HR) and 95% confidence interval (CI) or as means±SD of the mean.
RESULTS
Patient Characteristics
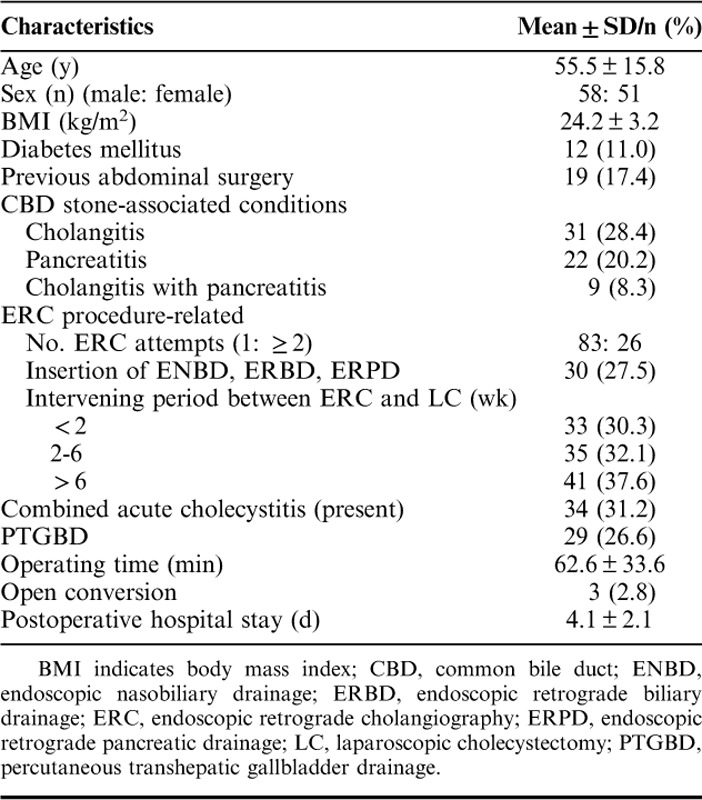
The clinical features of the 109 patients are listed in Table 1. A total of 62 patients initially presented with CBD stone-induced complications: acute cholangitis in 31, acute pancreatitis in 22, and acute cholangitis with acute pancreatitis in 9. Twenty-six patients underwent ≥2 sessions of ERC procedures for clearing the CBD. Endoscopic stents were placed in 30 patients and these were left in situ for a mean duration of 32.0±41.7 days. LC was performed within 2 weeks after ERC in 33 patients and 41 patients underwent LC 6 weeks after ERC.
TABLE 1.
Baseline Characteristics of Patients and Surgical Outcomes
Before the ERC, PTGBD catheter insertion was performed in 17 patients. Of these, 9 showed acute cholecystitis: 5 with moderate to severe cholecystitis and 4 with mild cholecystitis. The other 8 patients received PTGBD for biliary decompression. After the ERC procedure, 25 patients developed acute cholecystitis and PTGBD was inserted for 12 patients before performing LC: 4 showed moderate to severe acute cholecystitis and 8 had mild acute cholecystitis. The other 13 patients underwent emergency LC (Fig. 1).
FIGURE 1.
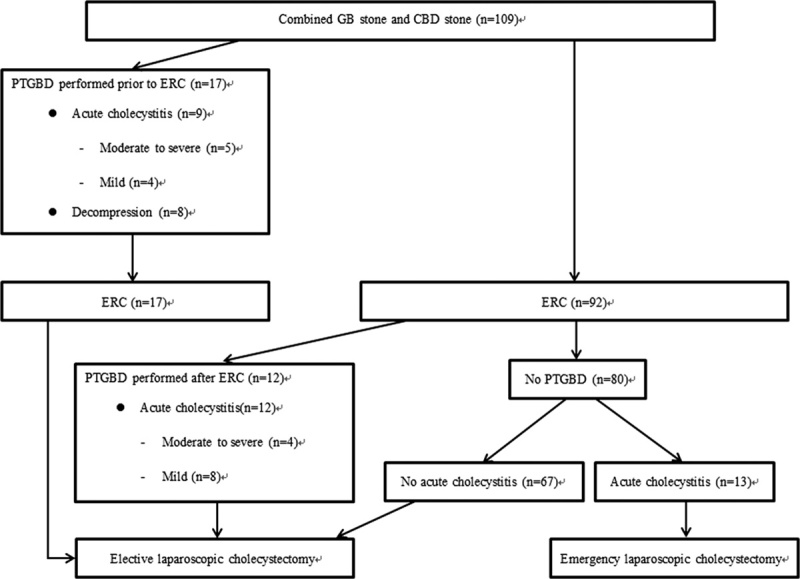
Flow diagram of the laparoscopic cholecystectomy procedure for patients with combined choledochocystolithiasis at our institute. CBD indicates common bile duct; ERC, endoscopic retrograde cholangiography; GB, gall bladder; PTGBD, percutaneous transhepatic gallbladder drainage.
Operative Results
The mean operative time was 62.6±33.6 minutes and 17 patients needed >90 min to complete the cholecystectomy. Three patients were converted to an open cholecystectomy. The causes of conversion were severe adhesions making laparoscopic dissection nearly impossible in 2 patients; the other patient had chronic inflammation with fibrosis near Calot triangle, which increased the risk of injury to the CBD during dissection. The mean hospital stay after surgery was 4.1±2.1 days and there were no surgical complications requiring surgical or radiologic interventions.
Factors Predictive of Long Operative Duration
Table 2 lists the predictive factors associated with prolonged operative duration identified from univariate analyses. In this analysis, initial diagnoses of acute cholangitis or of pancreatitis itself were not risk factors for a prolonged operation. In addition, ERC procedure-related factors such as the intervening period, the need for stenting, and the numbers of ERC attempts did not show statistical differences between the 2 groups. The presence of acute cholecystitis, placement of PTGBD, higher peak WBC counts and levels of CRP and lower peak levels of serum lipase during the intervening period showed P-values of <0.2, and were further included in multivariate logistic regression analysis. Before this, we tested for but found no multicollinearity between the variables. In the multivariate analysis, the presence of acute cholecystitis (HR, 5.418; 95% CI, 1.374-21.366; P=0.016) and a higher peak level of serum CRP (HR, 1.077; 95% CI, 1.011-1.147; P=0.022) were independent predictive factors for a prolonged operative duration (Table 3). In addition, the ROC analysis revealed that a cutoff point of the peak level of CRP at 15.3 mg/dL gave a sensitivity of 64.7% and a specificity of 88% for predicting a long operative duration (Fig. 2).
TABLE 2.
Univariate Analysis of Predictive Factors Associated with Prolonged Operative Durations for Laparoscopic Cholecystectomy Performed After Endoscopic Stone Removal for Choledochocystolithiasis
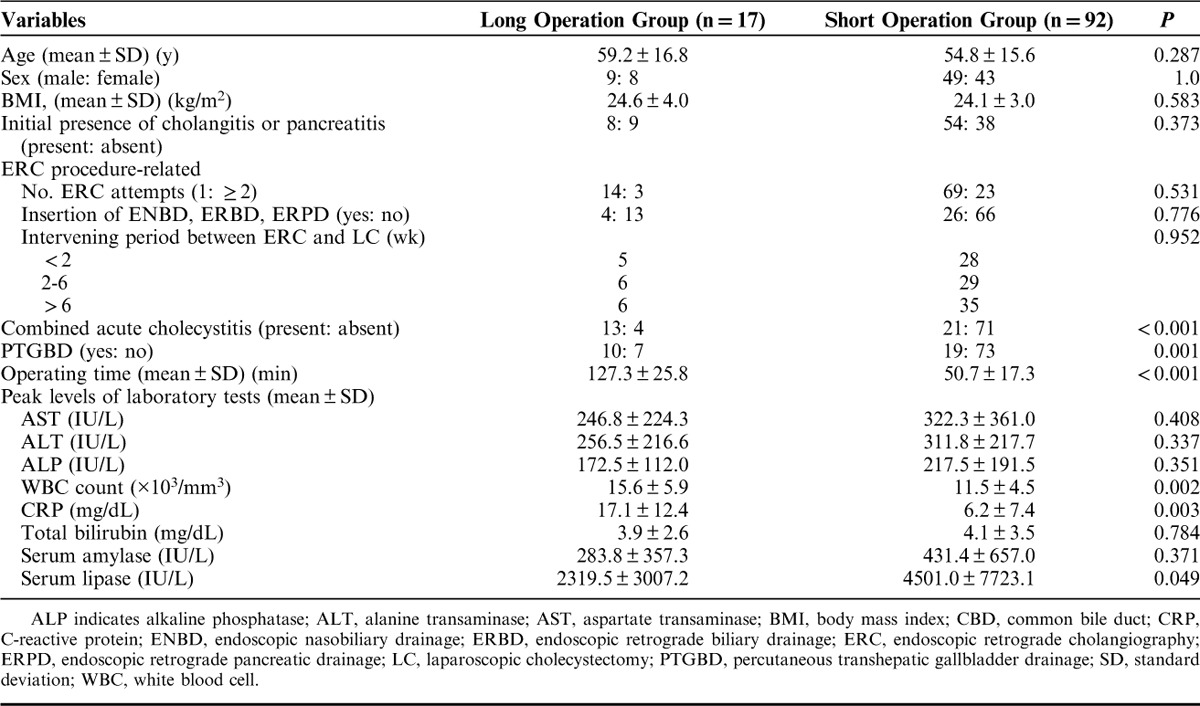
TABLE 3.
Multivariate Analysis of Independent Predictive Factors Linked to Prolonged Operative Durations for Laparoscopic Cholecystectomy Performed After Endoscopic Stone Removal for Choledochocystolithiasis
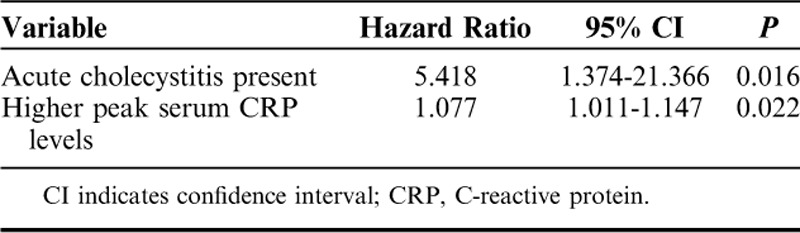
FIGURE 2.
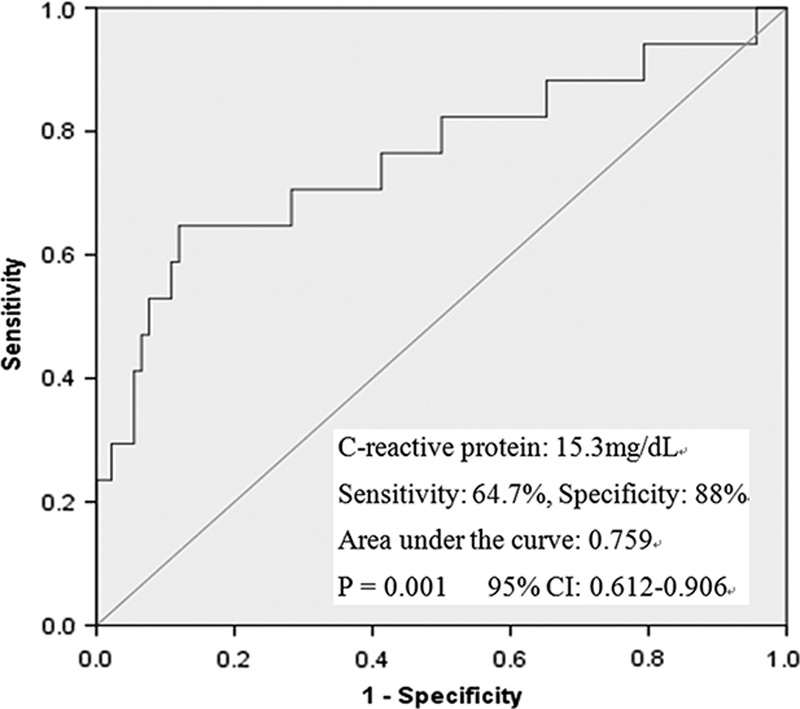
The results of the receiver-operating characteristic curve analysis of the C-reactive protein levels. CI indicates confidence interval.
DISCUSSION
For patients with coexisting gallbladder and CBD stones, most centers prefer endoscopic intervention and removal of the stones followed by subsequent LC as the first line of therapy. However, LC after ERC is regarded as a more difficult operation than standard LC because of the destruction of Oddi sphincter by endoscopic sphincterotomy, which potentially leads to bacterial colonization of the CBD, inflammation and scarring of the hepatoduodenal ligament.12 These problems are not only caused by the ERC procedure, but can also be influenced by the intensity of ongoing inflammation between the initial presentation and LC. During this interval, more intense inflammatory reactions than that of the initial presentation can develop after the ERC procedure and acute cholecystitis, acute cholangitis, or pancreatitis might worsen or develop. Therefore, we analyzed the peak levels of laboratory test values including inflammatory parameters such as WBC count and CRP levels during this intervening period. As shown in our results, 56.9% of the patients presented with acute pancreatitis and cholangitis, but these diagnoses by themselves were not risk factors for a prolonged operation. However, the peak serum level of CRP measured during the intervening period was a statistically significant predictive factor for a prolonged operation. We believe that conditions such as previous cholecystitis, aggravation of cholangitis and pancreatitis, and the development of acute cholecystitis can intensify inflammatory reactions near the gallbladder and hepatoduodenal ligament, and these can be reflected by elevated serum CRP levels.
Our results also revealed that the insertion of PTGBD was not a risk factor for a prolonged operation and had no influence on postoperative complications. Preoperative PTGBD can be applied in patients with moderate to severe cholecystitis or comorbidities. However, there is controversy regarding the effects of PTGBD on surgical outcomes such as operative durations or conversion rates. Mizrahi et al13 reported greater conversion rates and longer operative times in patients with acute cholecystitis receiving PTGBD when compared with the No-PTGBD patient cohort, and attributed this result to more advanced acute cholecystitis or possibly to the ongoing inflammatory processes and adhesions that might develop during the intervening period. Conversely, Kim et al14 reported that when elective delayed LC after PTGBD was performed on patients with complicated acute cholecystitis, surgical outcomes were better than that of patients who underwent an LC without PTGBD. It is not clear whether early decompression and drainage of infected gallbladder fluids using PTGBD alleviated the inflammation or, conversely, whether a PTGBD catheter left in situ could exacerbate inflammation of the gallbladder resulting in more severe fibrosis of Calot’s triangle. Nevertheless, from our results it appears that PTGBD can be applied without concern for the surgical outcomes in patients with stones in both the gallbladder and the CBD.
Regarding the ERC procedures, we compared the 2 groups according to the insertion of a biliary stent, and the timing of cholecystectomy after ERC. Nair et al15 reported that the presence of a CBD stent was a risk factor for long operative duration and conversion to an open cholecystectomy. However, Verzhbitsky et al16 showed no differences in the conversion rate in a stent insertion group and argued that having the stent in the CBD for a shorter period before surgery might eliminate the risk of conversion to an open operation. Here we also found that the insertion of a stent was not a predictor of long operative duration, and the stents were left in situ for a mean duration of 32.0±41.7 days, which was shorter than the mean duration in the study of Nair and colleagues. In addition, the interval between ERC and LC did not have any significance for predicting a prolonged operative time in the present study. De Vries et al17 reported conversion rate was higher when LC was performed 2 to 6 weeks after ERC. However, they also reported that the severity of adhesions and the time needed to perform the laparoscopic procedure were not influenced by the interval between ERC and LC and postulated that adhesions at 2 to 6 weeks after ERC had more potentially dangerous characteristics leading to conversion. We think that these problems might be overcome with refinements in laparoscopic technique and increased surgical experience.
In this study, the most potent predictive factor for a prolonged operation was the presence of acute cholecystitis. As discussed previously, ERC can induce local inflammation and this can be more intensified during the intervening period. When these changes are combined with acute inflammation of the gallbladder, surgical dissection near Calot triangle can be more difficult. Therefore, although acute cholecystitis that developed before an ERC was not preventable, early LC after an ERC should be recommended to prevent development of acute cholecystitis.
Both choledochocystolithiasis and acute cholecystitis increase the risk of bile leakage from the cystic stump. Reinders et al18 reported a higher incidence of such leakage resulting from a wide cystic duct in patients who had undergone a preoperative ERC for choledochocystolithiasis. Donkervoort et al19 also reported that cholecystitis was a risk factor for cystic stump leakage because of high rate of slippage of clips caused by edema and fibrosis of the cystic duct wall. However, we experienced no cystic duct leakages despite combining choledochocystolithiasis with cholecystitis. We skeletonized the cystic duct as much as possible and mostly ligated it using double clipping with 2 different materials, and sometimes used an endoloop for large diameter ducts. These cautious approaches might have helped in obtaining our good results.
Our study had some limitations. First, because of the small number of patients, we did not include the presence of cirrhosis or a history of upper abdominal surgery as predictive variables, although these are well-known risk factors for a difficult operation.20,21 Actually, only 3 patients had liver cirrhosis with Child class A severity and, of 19 patients with previous abdominal surgery, none had received upper abdominal surgery. Second, we focused on surgical difficulties according to various conditions linked to ERC. Therefore, we did not analyze the cost-effectiveness of the procedure or total hospital stay with respect to diverse clinical situations. Third, a considerable number of patients received PTGBD before LC because of institutional logistical considerations. Also, PTGBD was placed for the purpose of biliary decompression in 8 patients, and we knew, which did not meet standard practice.5 However, the aim of this study is not to justify its use, but to predict the factors related to prolonged operative duration. Although a larger scale study is needed to overcome these limitations, our study is unique in considering the intensity of inflammation during the intervening period, and we included clinical and laboratory test variables as much as possible to clarify the clinical significance of prolonged LC.
CONCLUSIONS
Our analyses suggest that higher peak levels of CRP during the intervening period and the presence of acute cholecystitis predict prolonged LC procedure after ERC. When the likelihood of a difficult operation is suspected, surgeons should prepare for it with caution, and an early LC might reduce operative difficulty because it helps prevent any new acute cholecystitis after ERC.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Baucom RB, Feurer ID, Shelton JS, et al. Surgeons, ERCP, and laparoscopic common bile duct exploration: do we need a standard approach for common bile duct stones? Surg Endosc. 2016;30:414–423. [DOI] [PubMed] [Google Scholar]
- 2.Ann KS, Kim YH, Kang KJ, et al. Impact of preoperative ERCP on laparoscopic cholecystectomy: a case-controlled study with propensity score matching. World J Surg. 2015;39:2235–2242. [DOI] [PubMed] [Google Scholar]
- 3.Ishizaki Y, Miwa K, Yoshinmoto J, et al. Conversion of elective laparoscopic cholecystectomy to open cholecystectomy between 1993 and 2004. Br J Surg. 2006;93:987–991. [DOI] [PubMed] [Google Scholar]
- 4.Miura F, Takada T, Kawarada Y, et al. Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo guidelines. J Hepatobiliary Panceat Surg. 2007;14:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saad WEA, Wallace MJ, Wojak J, et al. Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystostomy. J Vasc Interv Radiol. 2010;21:789–795. [DOI] [PubMed] [Google Scholar]
- 6.Hirota M, Takada T, Kawarada Y, et al. Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg. 2007;14:78–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wada K, Takada T, Kawarada Y, et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo guidelines. J Hepatobiliary Panceat Surg. 2007;14:52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Banks PA, Bollen TL, Dervenis C, et al. Acute Pancreatitis Classification Working Group Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. [DOI] [PubMed] [Google Scholar]
- 9.Williams EJ, Green J, Beckingham I, et al. Guidelines on the management of common bile duct stones (CBDS). Gut. 2008;57:1004–1021. [DOI] [PubMed] [Google Scholar]
- 10.Mahmud S, Masaud M, Canna K, et al. Fundus first laparoscopic cholecystectomy. Surg Endosc. 2002;16:581–584. [DOI] [PubMed] [Google Scholar]
- 11.Procter LD, Davenport DL, Bernard AC, et al. General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg. 2010;210:60–65. [DOI] [PubMed] [Google Scholar]
- 12.Boerma D, Rauws EA, Keulemans YC, et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile duct stones: a randomized trial. Lancet. 2002;360:761–765. [DOI] [PubMed] [Google Scholar]
- 13.Mizrahi I, Mazeh H, Yuval JB, et al. Perioperative outcomes of delayed laparoscopic cholecystectomy for acute calculous cholecystitis with and without percutaneous cholecystostomy. Surgery. 2015;158:728–735. [DOI] [PubMed] [Google Scholar]
- 14.Kim HO, Byung HS, Yoo CH, et al. Impact of delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage for patients with complicated acute cholecystitis. Surg Laparosc Endosc Percutan Tech. 2009;19:20–24. [DOI] [PubMed] [Google Scholar]
- 15.Nair MS, Uzzaman MM, Fafemi O, et al. Elective laparoscopic cholecystectomy in the presence of common bile duct stent. Surg Endosc. 2011;25:429–436. [DOI] [PubMed] [Google Scholar]
- 16.Verzhbitsky V, Zeina AR, Depsames R, et al. Does prophylactic stent insertion to the common bile duct during endoscopic retrograde cholangiopancreatography (ERCP) before cholecystectomy have any impact on the rate of biliary complications? Surg Endosc. 2013;27:4620–4624. [DOI] [PubMed] [Google Scholar]
- 17.de Vries A, Donkervoor SC, van Geloven AAW, et al. Conversion rate of laparoscopic cholecystectomy after endoscopic retrograde cholangiography in the treatment of choledocholithiasis. Does the time interval matter? Surg Endosc. 2005;19:996–1001. [DOI] [PubMed] [Google Scholar]
- 18.Reinders JSK, Goud A, Timmer R, et al. Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. Gastroenterology. 2010;138:2315–2320. [DOI] [PubMed] [Google Scholar]
- 19.Donkervoort SC, Kortram K, Dijksman LM, et al. Anticipation of complications after laparoscopic cholecystectomy: prediction of individual outcome. Surg Endosc. 2016;30:5388–5394. [DOI] [PubMed] [Google Scholar]
- 20.Quillin RC, Burns JM, Pineda JA, et al. Laparoscopic cholecystectomy in the cirrhotic patient: predictors of outcome. Surgery. 2013;153:634–640. [DOI] [PubMed] [Google Scholar]
- 21.Harboe KM, Bardram L. The quality of cholecystectomy in Denmark: outcome and risk factors for 20,307 patients from the national database. Surg Endosc. 2011;25:1630–1641. [DOI] [PubMed] [Google Scholar]


