Supplemental Digital Content is available in the text.
Abstract
Background:
Flexor tenolysis surgery for flexor digitorum profundus and superficialis adhesions is a common procedure performed by hand surgeons. Releasing these adhered tendons can greatly improve hand function and improve quality of life. Recent evidence, however, has shown that the outcomes of tenolysis surgeries are often suboptimal and can result in relapsing adhesions or even tendon ruptures.
Methods:
This article describes a new technique with potential for reduced complication rates: The Fine Wire Technique for Flexor Tenolysis (FWT).
Results:
Following FWT, the patient detailed in this article had an excellent recovery of function and no complications: including tendon rupture, infection, hematomas, or any other complications. She reported a major improvement from her preoperative functionality and continues to have this level of success. The wire’s thinness allows for a swift tenolysis.
Conclusions:
The FWT is a new option available to the hand surgeon associated with good functional results. The wire is readily available to the clinician and is also inexpensive.
INTRODUCTION
The repair of flexor tendon injuries is a challenge that hand surgeons commonly face, and one that can have an important impact on patient’s quality of life and hand function.1–3,5 Importantly, over the last 20 years, the literature reports a 5% rate of primary tendon repair failure, commonly resulting in adhesions, readhesions, and recurrent ruptures that lead to suboptimal outcomes.4 Similarly, current literature reports varying degrees of success following surgical release of adhesions, with one large, retrospective study placing only 23% of patients in a functional outcome category of “excellent,” whereas 10% of the patients were described as having “poor” outcomes following primary flexor tenolysis.4 In this article, we describe our experience with the Fine Wire Technique for flexor tenolysis (FWT) in a single patient to report this new technique.
SURGICAL TECHNIQUE AND CASE PRESENTATION
We present our most recent case of a patient undergoing the FWT, which demonstrated excellent results. To protect the patient’s privacy, identifying features have been eliminated. The patient was a 67-year-old female who presented with adhesions of the left little finger (LLF) profundus and superficialis flexor tendons 6 months after a previous zone 2 dual-tendon injury repair. She was unable to actively flex the proximal interphalangeal (PIP) joint but was able to fully flex the metacarpophalangeal joint and the distal interphalangeal (DIP) joint a total of 30 degrees. Preoperatively, she had a full passive range of motion of the PIP. After extensive hand therapy, she demonstrated little improvement in her active LLF PIP range of motion, and flexor tenolysis was recommended. The patient was informed of the risks of infection, tendon rupture, readhesion, the need for prolonged therapy, and the potential for delayed rupture. All the images included in this article were obtained from the patient in compliance with our institutional review board guidelines, and the video demonstrating the technique was obtained during a cadaveric dissection in compliance with our institution anatomical gift program guidelines.
The Fine Wire Technique
At our institution, we perform this procedure under a Bier block using Lidocaine 0.5% (Hospira Inc., 2016). First, the hand is prepped and draped in the usual sterile fashion using 70% isopropyl alcohol (Hydrox Labs, Elgin, Ill., 2016) followed by 10% betadine (Povidine-iodine, Purdue Products L.P., Stamford, Conn., 2016).
A Bruner incision is placed on the volar aspect of the affected digit from the DIP joint and extending to the distal palmar crease (Fig. 1); this is followed by blunt dissection of the subcutaneous tissue. The neurovascular bundles are identified and protected bilaterally. The A1 pulley is opened partially, and both flexor tendons are identified. It is common at this point to note significant adhesions that limit the movement of both the profundus and superficialis flexor tendons.
Fig. 1.

A Bruner incision placed on the volar aspect of the affected digit from the DIP joint to the distal palmar crease.
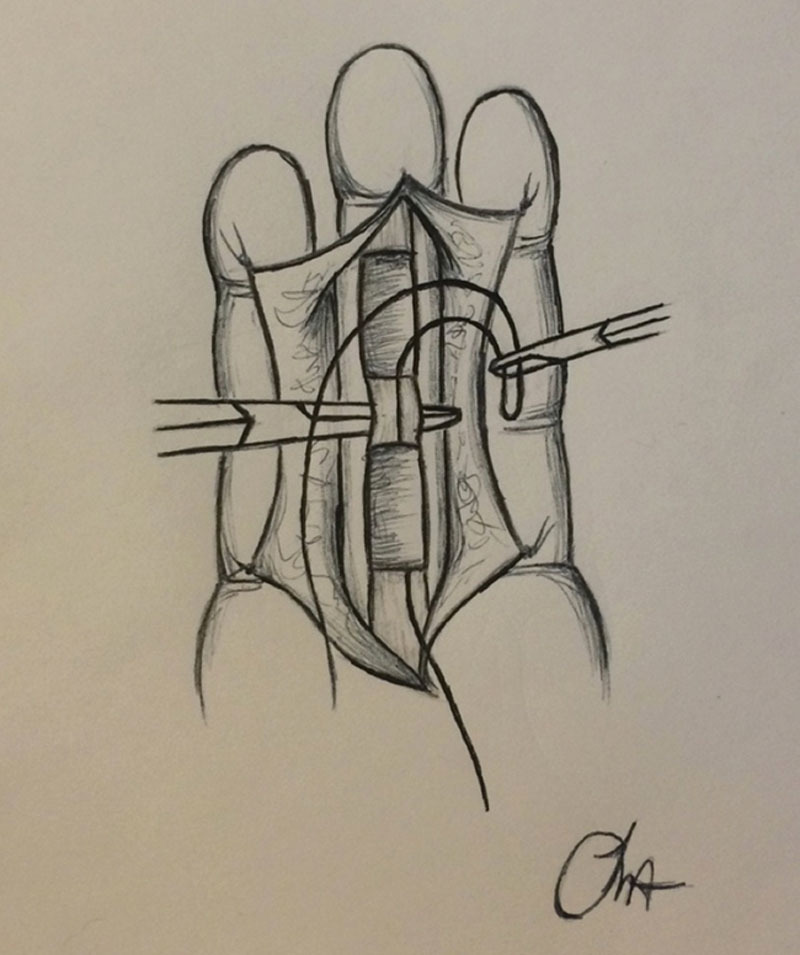
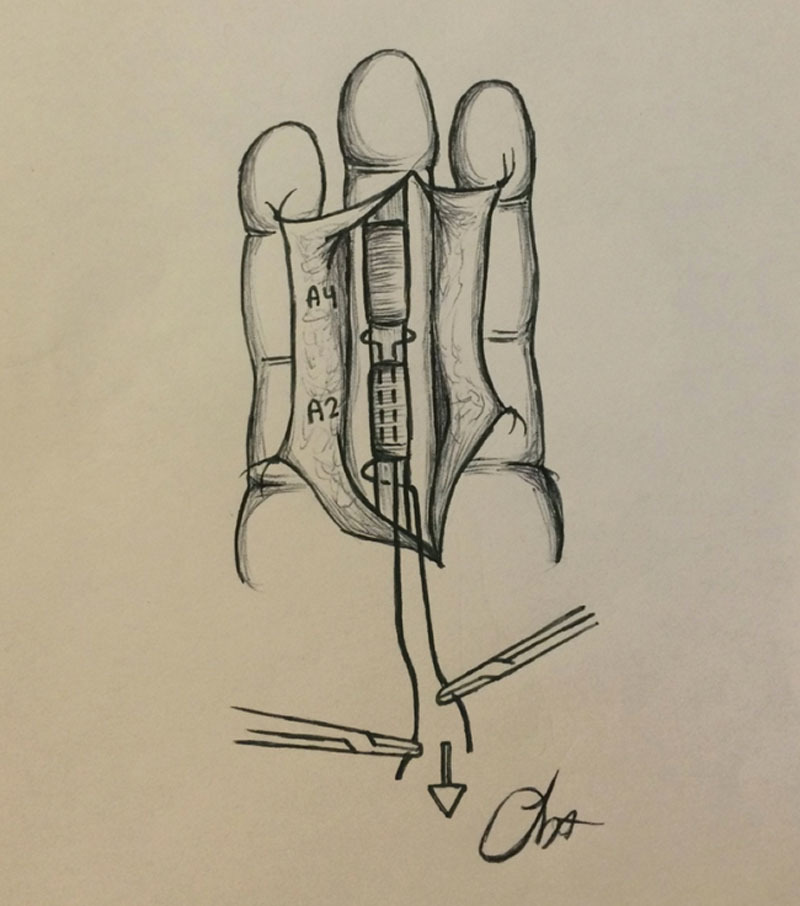
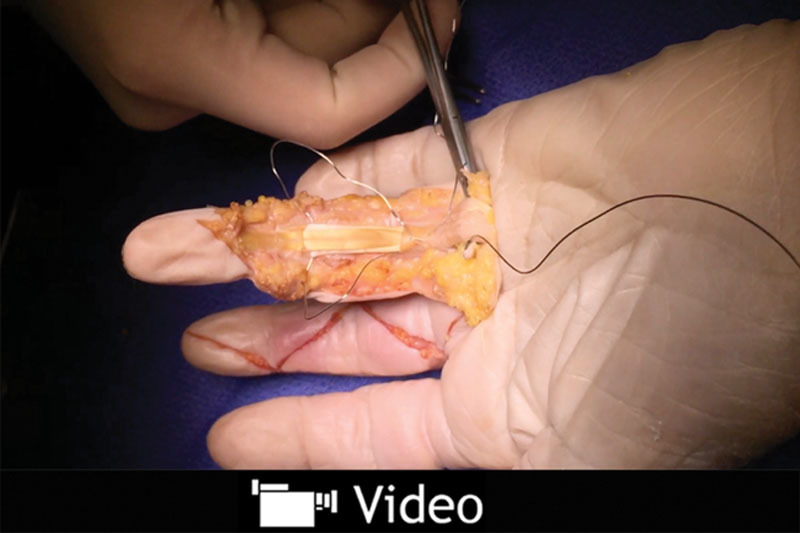
Wire use: A #25 gauge wire with the end folded back on itself to create a stiffer, blunt tip is used to perform the tenolysis (Figs. 2, 3). The wire is passed underneath the A1, A2, and A3 pulleys on the volar radial superficial surface to the flexor tendons and brought out through the distal aspect of the A3 pulley volarly (Fig. 4; see video, Supplemental Digital Content 1, which is a demonstration of the wire passing underneath the A1-3 pulleys, available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A604).
Fig. 2.
A #25 gauge wire folded onto itself to create a smooth, blunt end is used for the procedure.
Fig. 3.
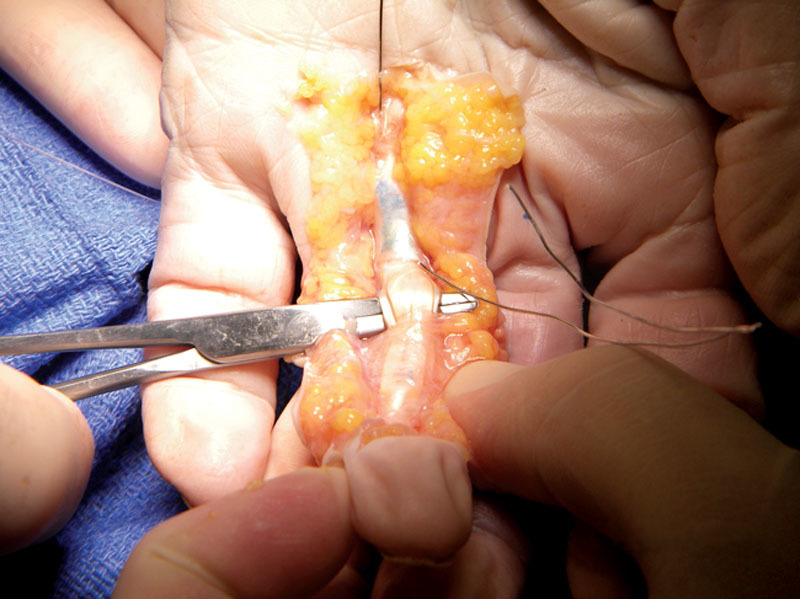
The #25 gauge wire used for the procedure.
Fig. 4.
The wire is passed underneath the A1, A2, and A3 pulleys on the volar radial superficial surface to the flexor tendons and brought out through the distal aspect of the A3 pulley volarly.
Video Graphic 1.
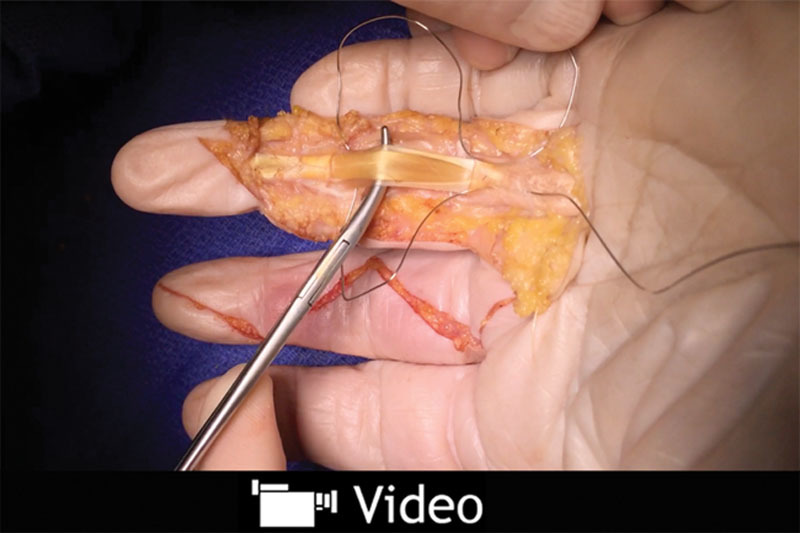
See video, Supplemental Digital Content 1, which is a demonstration of the wire passing underneath the A1-3 pulleys, available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A604.
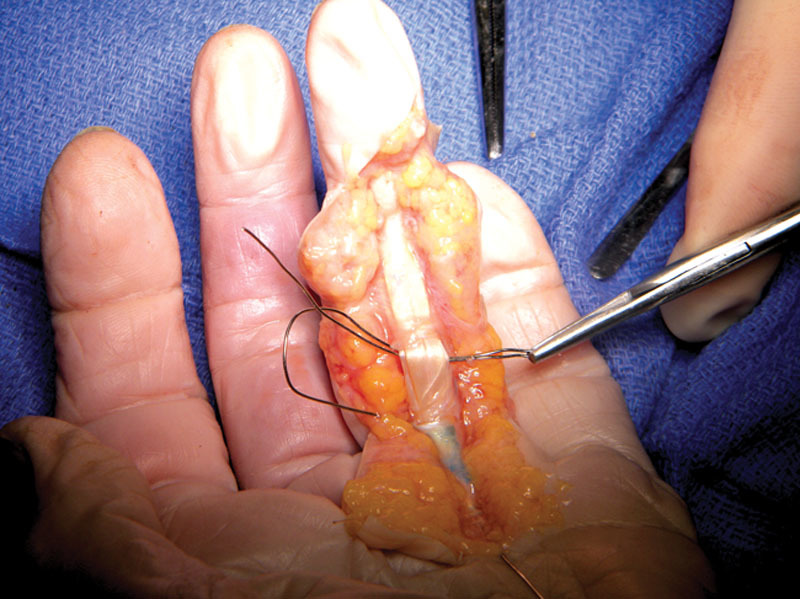
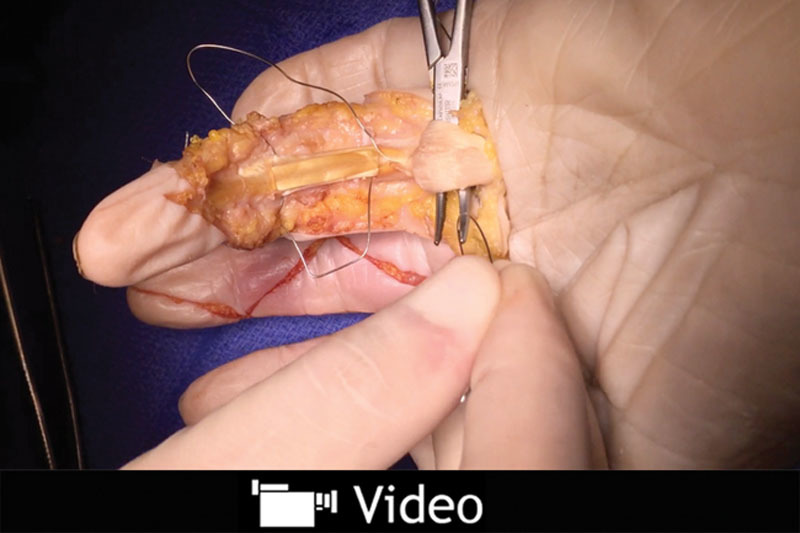
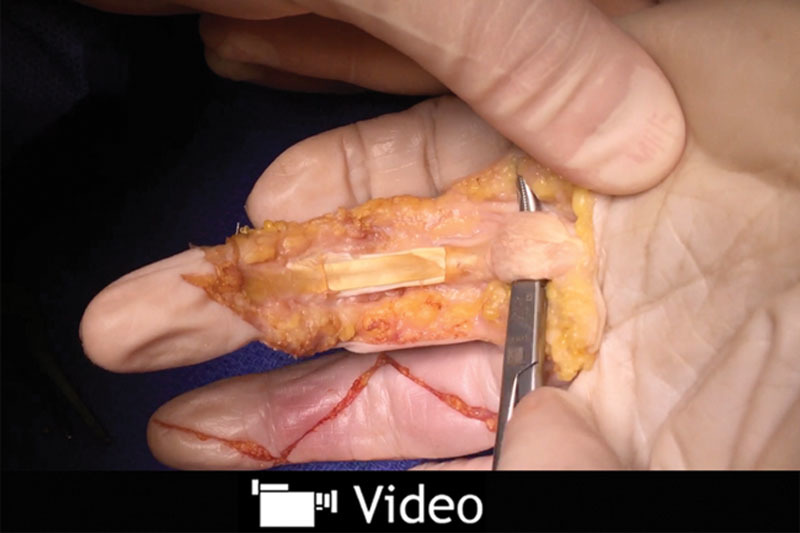
The wire is then passed underneath the profundus and the superficialis tendons from the radial side of the digit to the ulnar side, and then brought back up to the volar surface (Fig. 4). Then, the wire is passed along the volar ulnar side of the flexor sheath under the A3, A2, and then out through the region of the A1 pulley (Fig. 5). Then the wire is passed under both flexor tendons and brought out on the same radial side through which the wire was initially introduced (see video, Supplemental Digital Content 2, which is a demonstration of the wire passing under the flexor tendons and out through the radial side, available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A605). Tension is then placed on the #25 gauge wire, keeping it parallel to the proximal phalanx (see video, Supplemental Digital Content 3, which is a demonstration of tendon lysis (1), available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A606). The wire is pulled and watched as it sweeps around posteriorly and lyses all the adhesions around the profundus and superficialis tendons (Fig. 6) (see video, Supplemental Digital Content 4, which is a demonstration of tendon lysis (2), available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A607).
Fig. 5.

The wire passing along the volar ulnar side of the flexor sheath under the A3, A2, and then out through the region of the A1 pulley.
Fig. 6.
The wire is pulled and watched as it sweeps around posteriorly and lyses all the adhesions around the profundus and superficialis tendons.
Video Graphic 2.
See video, Supplemental Digital Content 2, which is a demonstration of the wire passing under the flexor tendons and out through the radial side, available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A605.
Video Graphic 3.
See video, Supplemental Digital Content 3, which is a demonstration of tendon lysis (1), available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A606.
Video Graphic 4.
See video, Supplemental Digital Content 4, which is a demonstration of tendon lysis (2), available in the “Related Videos” section of the Full-Text article on PRSGO.com or at http://links.lww.com/PRSGO/A607.
Following this, gentle traction on the flexor digitorum superficialis tendon in the palm results in finger flexion at the PIP (Fig. 7).
Fig. 7.

Gentle intraoperative traction of the flexor digitorum superficialis tendon results in flexion at the PIP joint.
To accomplish tenolysis of the flexor digitorum profundus (FDP) distal to the A3 pulley, the technique is repeated from the A4 pulley all the way underneath the A5 pulley, but this time going around the FDP tendon only. Once tenolysis of the FDP distal to the A3 pulley is completed following the same steps described for wire-based tenolysis proximal to the A3 pulley, then gentle traction on the FDP tendon in the palm results in improved flexion of the DIP.
The patient is then given a digital block with 0.25% plain Marcaine (Pfizer Inc, 2016). The Bier Block is reversed. All small bleeders are controlled with electrocautery to achieve optimal hemostasis before proceeding with skin closure. Closure of the skin is completed with 4-0 nylon and sutures.
A light dressing is then applied followed by a dorsal splint holding the wrist in 45 degrees of flexion and the interphalangeal joints in full extension. The patient begins an immediate range of motion program and is advised not to do any heavy weight lifting or tense gripping. Postoperative hand rehabilitation program consists of 11 sessions of Occupational Therapy, starting 24 hours postprocedure and ending 5 weeks postprocedure. The patient was seen 3 times a week for the first 2.5 weeks, then 2 times a week, then once the final 2 weeks.
At completion of the procedure, the patient described in this article was able to actively flex the finger all the way into her palm and extend it. The patient tolerated the procedure well and was able to repeat this full flexion and extension multiple times.
RESULTS
Immediately after operation, the patient was satisfied with the results of the surgery. She was capable of full flexion and extension of her LLF (Fig. 8). This was an improvement over the complete lack of flexion preoperatively at the PIP joint and an improved outcome compared with those reported in current literature.1–4,6 The Upper Limb Functional Index increased from 0 preoperative to 64 postoperatively. Total active range of motion increased 125 degrees. Six weeks postoperatively, the patient has retained this full flexion with no decline in function following the completion of her physical therapy regimen.
Fig. 8.

Full, active extension and flexion of the LLF postoperatively.
Complications
The patients did not experience any complications as a result of the surgery, including but not limited to infection, adhesion reformation, or tendon rupture.
DISCUSSION
Flexor tenolysis procedures often result in unsatisfactory results for both patients and surgeons alike, with readhesions and other complications occurring.1–5 The time for the operation is 1 hour. The wire technique avoids the use of the traditional freer, which exposes the patient to the risk for scar tissue build up, subsequent readhesions, and pulley ruptures.4
The wire is an optimal tool for this procedure for several reasons. It is inexpensive and easily available, making this procedure feasible in a variety of locations and practice settings. Due to its thinness, the wire is able to glide through the adhesions with little friction. It completely lyses both anterograde and retrograde adhesions.
The next step in evaluating this technique will be to conduct a prospective study to quantify the long-term outcomes and results of the technique and to compare its efficacy to the existing techniques. For now, the technique appears to be a promising solution to one of the most difficult problems in hand surgery.
The FWT provides an alternative method to traditional flexor tenolysis procedures being performed by hand surgeons around the world today. The procedure has been observed to be successful in the patient described in this report, as well as several other patients in our practice. The use of the #25 gauge wire allows for swift, total lysis of adhesions without excessive tissue irritation, making it an improved alternative to the current standard tenolysis procedure. High patient satisfaction following the Fine Wire Technique has been observed in our clinic.
ACKNOWLEDGMENTS
The authors thank everyone who made this project possible: Dr. Michael Smith, PhD, for his assistance in procuring the cadaver used in the figures included in this article. Ms. Celeste Freeman, OT, for her assistance in providing information regarding the postoperative outcomes and the rehabilitation programs.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Elliot D, Giesen T. Avoidance of unfavourable results following primary flexor tendon surgery. Indian J Plast Surg. 2013;46:312–324.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kawakatsu M, Ishikawa K, Terai T, et al. Distraction arthrolysis using an external fixator and flexor tenolysis for proximal interphalangeal joint extension contracture after severe crush injury. J Hand Surg Am. 2010;35:1457–1462.. [DOI] [PubMed] [Google Scholar]
- 3.Breton A, Jager T, Dap F, et al. Effectiveness of flexor tenolysis in zone II: a retrospective series of 40 patients at 3 months postoperatively. Chir Main. 2015;34:126–133.. [DOI] [PubMed] [Google Scholar]
- 4.Feldscher SB, Schneider LH. Flexor tenolysis. Hand Surg. 2002;7:61–74.. [DOI] [PubMed] [Google Scholar]
- 5.Battiston PF, Triolo A. Secondary repair of flexor tendon injuries. Injury. 2013;44:340–345.. [DOI] [PubMed] [Google Scholar]
- 6.Elliot D, Giesen T. Treatment of unfavourable results of flexor tendon surgery: ruptured repairs, tethered repairs and pulley incompetence. Indian J Plast Surg. 2013;46:458. [DOI] [PMC free article] [PubMed] [Google Scholar]


