Abstract
Orally administered devices could enable the systemic uptake of biologic therapeutics by engineering around the physiological barriers present in the gastrointestinal (GI) tract. Such devices aim to shield cargo from degradative enzymes and increase the diffusion rate of medication through the GI mucosa. In order to achieve clinical relevance, these designs must significantly increase systemic drug bioavailability, deliver a clinically relevant dose and remain safe when taken frequently. Such an achievement stands to reduce our dependence on needle injections, potentially increasing patient adherence and reducing needle-associated complications. Here we discuss the physical and chemical constraints imposed by the gastrointestinal organs and use these to develop a set of boundary conditions on oral device designs for the delivery of macromolecules. We critically examine how device size affects the rate of intestinal obstruction and hinders the loading capacity of poorly soluble protein drugs. We then discuss how current orally administered devices could solve the problem of tissue permeation and conclude that these physical methods stand to provide an efficacious alternative to the classic hypodermic needle.
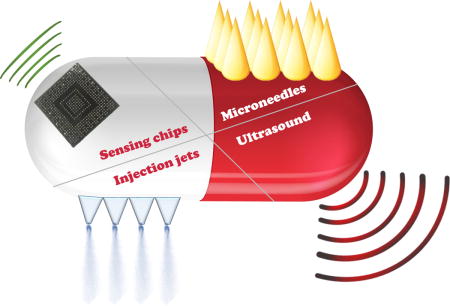
Graphical abstract
Introduction
Biologic drugs–including peptides, monoclonal antibodies, and nucleic acids–are revolutionizing the standard of care across many diseases. In general, patients must inject biologic drugs, rather than orally ingest them, because they degrade in the gastrointestinal space and do not easily permeate across biological barriers. However, administration via hypodermic needles requires training, causes pain, and leads to needle injuries as well as transmission of infectious diseases [1–3]. In addition, needle-phobia, suffered by 10% of all individuals, may cause certain patients to forgo treatment or skip doses [4,5]. These potential hazards affect clinicians’ opinions of injectable medications, which manifest in lower prescription rates particularly in pediatric populations [6]. Here we discuss some of the fundamental challenges and realizable benefits of developing drug-device combinations to enable the systemic delivery of biologics via the gastrointestinal (GI) tract.
When compared to injectable drugs, oral formulations acting in the same biologic pathway and for the same indications are more commonly prescribed. This is so even when the injectable drugs demonstrate clinically superior results. For example, in the treatment of type 2 diabetes, several clinical trials have shown that glucagon-like peptide-1 (GLP-1) receptor agonists (injectable) result in superior glycemic control and greater weight loss than dipeptidyl peptidase-4 (DPP-4) inhibitors (orally delivered), yet many patients and healthcare providers opt for the DDP-4 inhibitors because of the administration route [7–10]. Last year DPP-4 inhibitor and GLP-1 agonist sales were $10 billion and $4 billion, respectively [11].
Efforts have been made for almost a century to address the problem of delivering biologics orally. In 1923 (2 years after the discovery of insulin), Harrison administered high concentrations of insulin in an alcohol solution orally with apparent success in only one of four patients [12]. Since, numerous scientists have attempted to increase the oral bioavailability of biologic drugs. The strategies used to optimize protein and peptide delivery focus on two main goals: tissue wall localization and enhanced permeation. Chemical modification strategies including mutagenesis, proteinylation, glycosylation, PEGylation and prodrugs as well as formulation strategies based on the use of absorption enhancers like nanoparticles, microspheres, liposomes and emulsions, have been used to increase the bioavailability to between 1–2% [13–21]. This threshold allowed for the development of oral vaccines using hydrogel-carriers and nanoparticle-based techniques to protect the antigen from the hostile environment of the GI tract [20,22–24]. In this article we focus on new device-based strategies for drug delivery, which use physical means of tissue interaction coupled with chemical modifications in order to supply protein drugs with higher and narrower dose requirements than vaccines.
Understanding anatomy for successful drug delivery
The GI tract is comprised by the oral cavity, esophagus, stomach, small intestine and colon. The hostility of the GI tract, including its extreme pHs and high degradative enzymatic activity, hinder the delivery of many active pharmaceutical ingredients (APIs) (Figure 1). Furthermore, the physical properties of the GI organs including muscle contractions, variable membrane permeability, short residence times, and thick mucus coatings loaded with bacteria add additional challenges. When dealing with drug permeation it is important to ensure that the molecule overcomes the mucus coating and reaches the appropriate tissue layer to be taken up by the blood stream prior to enzymatic degradation [25].
Figure 1.
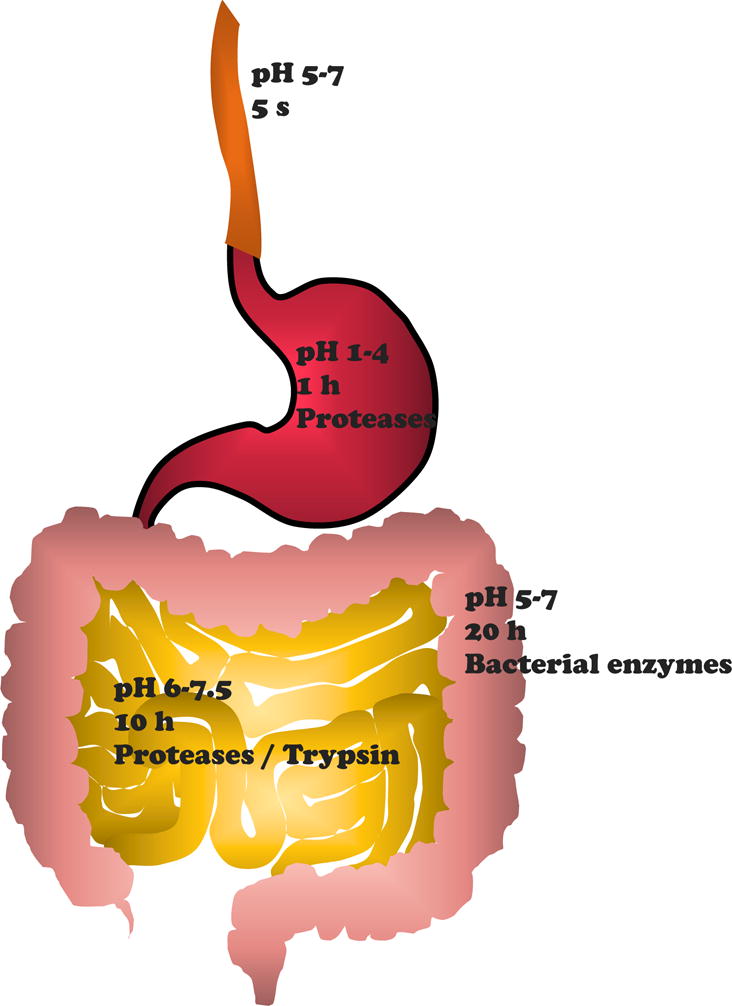
Schematic of the GI tract with corresponding pH ranges, average transit times and predominant protein degradative enzymatic activity [26–29].
The high heterogeneity of the GI organs confers advantages and disadvantages for delivering drugs. The esophagus and the stomach provide quickly accessible delivery sites; however, rapid transit times through the esophagus and low pH conditions in the stomach add extra engineering constraints. In order to deliver an API in the stomach, it must avoid digestion, pass through the thickest mucus layer in the GI tract spanning 40–450 μm and transport para- (across the tight junctions) or trans-cellularly through the tissue [29]. The longer transit times and extended surface area in the small intestine favor its use as a delivery site. Additionally, specific areas in the organ, called Peyer’s patches, are covered with less mucus allowing for a quicker absorption of hydrophobic formulations [16]; however, targeting this organ delays drug uptake and still requires overcoming the presence of mucus and degradative enzymes. Finally, the colon provides residence times of up to 20 hours, yet the presence of stool and the bacteria-rich environment pose limitations to the delivery of biologics.
Devices to address biologic drug delivery
The need to overcome the challenges posed by the GI tract along with the growing demand for non-invasive methods have led the healthcare industry to invest in a range of novel technologies for the oral administration of biologics. These devices, expected to reach $3.83 billion in sales by 2020 [30], resemble conventional capsules but carry small electronic and/or mechanical elements. Device size, which is directly related to drug loading capacity, acts as a major boundary condition towards designing an oral drug delivery device, and information gathered from clinical correlates helps set dimensional restrictions and drug load per ingested device. Additionally, tissue localization of the device and enhanced permeation or penetration represent significant challenges that will have to be addressed.
Boundary Conditions
Device Size
Devices that target areas of the GI tract other than the oral cavity must adhere to strict size constraints. Researchers should limit the volume of a solid, non-disintegrating device to something easily ingestible that poses a vanishingly rare risk of mechanical obstruction. To ensure the absence of clinical obstructive symptoms, a device must dissolve completely within approximately 1 day. The upper boundary for dimensions of ingestible devices has been established by clinical experience with video capsule endoscope (VCE) systems. VCEs, measuring 11 mm by 26 mm, allow for easy ingestion; however, an analysis of 2300 patients showed a retention rate of 1.3% [31]. In order to identify patients at risk of obstruction, doctors can prescribe a patency capsule of the same size that degrades within 80 hours and tests for possible retention beforehand. If the capsule passes intact within 30 hours, then doctors consider the VCE safe to dose [32]. Drug delivery devices should also pass or degrade within a timescale consistent with this safely proven range of gastrointestinal transit times [33]. However, even though this capsule size passes FDA regulations as an infrequently dosed diagnostic device, it is not practical for a therapeutic that would require regular administration.
The OROS system, an osmotic extended drug release capsule that leaves an indigestible shell measuring 9 mm by 15 mm, provides a broader patient experience data set with respect to GI retention rates. Interestingly, the rate of GI retention is on the order of only one in 29 million in a sample size of almost 13 billion [34]. The OROS system has been on the market for dozens of years and is approved by the FDA for daily use. Shrinking a device mitigates obstruction risk, but size constraints then raises the issue of another important boundary condition, drug loading.
Drug Loading
In order for a drug delivery device to gain commercial use, it should deliver a relevant amount of API that must remain stable throughout the manufacturing process, on the shelf, and inside of the digestive tract. This poses a substantial challenge to the delivery of biologic macromolecules, which generally require a significant mass to exert a therapeutic effect, and are highly susceptible to degradation. While scientists have shown that certain vaccines remain stable in various shelf life temperature settings after immobilization in trehalose [35], biologic molecules demonstrate a high vulnerability to degradation in the GI tract due to the presence of enzymes. A decrease in bioavailability by 50% requires a 100% increase of loaded API.
Delivering relevant doses of several biologic drugs in their current formulations will be very challenging due to volume constraints. Table 1 details the solution strength of several biologic drugs as well as the volume required to deliver a relevant injected dose. Capsules the size of the OROS system allow just under one mL of space for both the device and loaded drug. The development of novel drug-device combinations will require careful consideration of the pharmacokinetics of this delivery route and moreover require significant formulation development to ensure the appropriate dose and activity of the API are maintained.
Table 1.
Biologic Drugs – Molecular Weight, Dose, Solubility and Volume
| Octreotide | Teriperatide | Insulin | Filgastrim | Somatropin | Adalimumab | Infliximab | Etanercept | |
|---|---|---|---|---|---|---|---|---|
| Disease Indication | acromegaly, carcinoid and VIP tumors | osteoporosis | hyperglycemia | neutropenia | growth hormone deficiency | anti-TNF (RA, CD, psoriasis) | anti-TNF (RA, CD, UC, psoriasis) | anti-TNF (RA, psoriasis) |
| Molecular Weight (KDa) | 1.0 | 4.1 | 5.8 | 18.8 | 22.1 | 148.0 | 149.1 | 150.0 |
| Solution Strength (mg/mL) | 1 | 0.25 | 3.5 | .3 | 10 | 50 | 10 | 50 |
| Dose (mg) | 0.05–0.6 | 0.02 | 0.1–2 | 0.35 | 0.2–0.4 | 40 (RA)–160 (CD) | 210–350 | 50 |
| Dose Frequency | 2x–4x daily | daily | Daily and before meals | Daily | Daily | Every two week | Every eight weeks | Weekly |
| Vol Required (mL) | 0.05–0.6 | 0.08 | 0.03–0.57 | 1.2 | 0.02–0.04 | 0.8–3.2 | 21–35 | 1 |
The following table contains a list of currently marketed biologic drugs and shows how the required dosage volumes change with molecular weight and solution strength. All dosages were calculated using a height of 180 cm and a weight of 70 kg. [36] Abbreviations: VIP-vasoactive intestinal peptide. TNF – tumor necrosis factor. RA – rheumatoid arthritis. CD – Crohn’s Disease. UC – Ulcerative Colitis.
Tissue Localization
The challenges associated with tissue wall localization stem from the constant motility and open geometries in the gastrointestinal tract, yet the presence of degradative enzymes requires that all devices prevent elution of drug into the luminal space. Smooth muscle contractions from peristalsis constantly push luminal content through the upper GI tract causing nonlinear, convective flows up to 4 cm/s [37,38]. Such flow patterns cause mixing, uniformly distributing a drug throughout the entire cavity and increasing its likelihood of binding with an enzyme. Since the radius of the GI tract ranges anywhere from 2 cm in the small intestine up to 25 cm in the stomach, at least 90% of the drug will sit further than 1 mm away from the tissue wall at any given moment in a well-mixed system. This number climbs to 99% in the stomach. Because the kcat for pepsin is 45/s, and other degradation enzymes possess similar or faster velocities, drugs delivered to sites other than the tissue wall degrade without a chance for uptake.
Devices solve the tissue localization issue by taking advantage of the same concepts that prevent the use of traditional tablets. In particular, they target the small intestine due to its smaller radius. For example, a carboxymethyl cellulose/poly(acrylic acid) hydrogel was reported to swell up against the tissue walls when exposed to near neutral pH, entirely filling the space inside of the small intestine with a drug loaded substance rather than chyme. Enzymatic degradation of the gel and diffusion of insulin into the small intestine yielded a bioavailability of 6.6% in rabbits [39].
Other methods, such as mucoadhesion and nanostraw patterning, take advantage of the random flow patterns inside of the GI tract. Researchers designed these devices to stick to the tissue wall through chemical bonding or surface adhesion, and constant mixing ensures eventual contact with the mucosal barrier. Once attached to the tissue, these devices create privileged regions enabling insulin delivery with a concomitant hypoglycemic effect demonstrated in rats over the course of 8 hours. Because these devices rely on random flow patterns several do not attach correctly. On average around 25% of nanostraw devices land on the wrong side or never attach at all. While dose variability is inevitable in such a situation, researchers mitigate the concern by dosing several, sometimes thousands, of devices at a time [40–42]. Researchers should move away from a dependence on unpredictable forces in order to ensure tissue localization and standardized drug uptake profiles. Only in this way can they avoid the degree of variability observed by Harrison in his experiments reported in 1923.
Tissue Permeation and Penetration
Once drug formulations localize to the tissue wall, they must then pass through the mucus barrier of the gastrointestinal tract to achieve systemic uptake. Devices aid in this process through both physical and biochemical means. Biochemical approaches such as polymer/liquid/inorganic nanocarriers, nanotubes, cell penetrating peptides, pore-forming proteins, vesicles, viral vectors, ligand conjugates and detergents chemically alter the cellular environment to open up new permeation pathways and can be delivered with anatomic selectivity through enterically coated devices [43] or smart ingestible pills like ChipRx and IntelliCap [44,45]. Physical modes of delivery use devices to directly penetrate through or remove tight junctions blocking drug uptake; methods include micro/nano-needles, ultrasound, microinjection, electroporation, cavitation, ballistics, scrapers, thermal enhancers, microjets and optoporation [41,46]. The newest of these technologies, microneedles, microjets, and ultrasound, all require quick and precise tissue localization.
Microneedles have been used over the last two decades to breach the stratum corneum and enhance permeation across the skin. The incorporation of this technology into an ingestible capsule could also increase tissue permeability in the GI tract. Scientists are currently developing a ‘Robotic pill’ consisting of drug-coated microneedles which will be pushed past the mucus into the small intestine epithelium via a gas based reaction between citric acid and sodium bicarbonate [47]. Since the small intestine has a mucus layer which is 200 μm thick and its wall measures 1.2 mm, microneedles will have to be designed taking into consideration these parameters to ensure penetration of the mucus layer while avoiding serious clinical complications such as perforation. Nevertheless, our group has previously shown capability of a capsule coated in 25 gauge metal microneedles protruding 5mm from a device to pass through the GI tract without perforating tissue [48].
Other devices in development use transient methods of tissue interaction to avoid possible complications in the lower GI tract. For example, microjet injectors powered by gas reactions have delivered viral vectors in the oral cavity [49]. By propelling a jet into the buccal tissue of rabbits, the antibodies pass through the disturbed mucus layer at high levels. Ultrasound has also been shown to enhance permeation of biologics in the GI tract [50,51]. Additionally, needle-free drug delivery systems have been used to deliver APIs in liquid forms by means of spring systems, lasers and energy propelled systems across the skin and to the oral mucosa [52]. In general, these physical penetrators significantly increase drug bioavailability, but they must localize to the tissue wall in order to work. Likely, a marketable version of an oral biologic device will be a combination of permeation enhancers, localization mechanisms, and machines used to cross the epithelial barrier of the GI tract.
Conclusion
While oral drug delivery devices have been shown to effectively release medications with a higher bioavailability than reformulations alone, there remains several challenges in the way of a marketable device. The oral route submits drugs to the heterogeneous GI environment inducing an uncertainty which complicates the dosage of drugs with narrow therapeutic indexes [12]. The new generation of orally administered devices avoids the uncontrollable forces in the GI tract and therefore lowers dosing variability by bypassing the gastric cavity and focusing on physical tissue wall interaction. There exists the potential for even greater standardized dosing if devices use their own forces for the process of tissue wall localization rather than relying on random fluid motion. Moreover, even the best devices provide bioavailabilities lower than 10% which necessitates large volumes dedicated to drug storage [53], yet capsules on the order of 11 mm by 26 mm show rates of intestinal obstruction too high for daily dosing. Additionally, large capsules in general are associated with lower adherence rates in certain populations, especially children [54,55]. Device miniaturization to maximize safety and drug reformulation to maximize API loading will be significant and essential development tasks. Scientists must focus on these efforts to finally realize the 100 yearlong quest for orally deliverable biologics.
HIGHLIGHTS.
The anatomy and physiology of the gastrointestinal tract defines boundary conditions for orally administered devices.
Device dimensions are related to intestinal obstruction rates and can complicate safe daily dosing.
Low protein solubility can hamper encapsulation of biologics in a liquid formulation.
Oral devices increase bioavailability by localizing to the tissue and increasing permeability.
Acknowledgments
This work was supported in part by a grant from Novo Nordisk, a grant from the National Institutes of Health (EB-000244).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
All authors are co-inventors on multiple patent applications describing systems for the delivery of macromolecules via the gastrointestinal tract. G.T. and R.L. also receive consulting fees from Novo Nordisk.
References
- 1.Carlson B. Ousting the “ouch factor” in drug delivery. Biotechnol Healthc. 2007;4:15–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Dallel N, Kacem M, Nabouli RMEMM. Managment of syringes of insulin by diabetic patients. About 100 patients. Tunisie Medicale. 2005;83:390–392. [PubMed] [Google Scholar]
- 3.Miller MA, Pisani E. The cost of unsafe injections. Bull World Health Organ. 1999;77:808–811. [PMC free article] [PubMed] [Google Scholar]
- 4.Sokolowski CJ, Giovannitti JA, Boynes SG. Needle phobia: Etiology, adverse consequences, and patient management. Dent Clin North Am. 2010;54:731–744. doi: 10.1016/j.cden.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 5.Gilroy CA, Luginbuhl KM, Chilkoti A. Controlled release of biologics for the treatment of type 2 diabetes. J Control Release. 2015 doi: 10.1016/j.jconrel.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carino GPG, Mathiowitz E. Oral insulin delivery. Adv Drug Deliv Rev. 1999;35:249–257. doi: 10.1016/s0169-409x(98)00075-1. [DOI] [PubMed] [Google Scholar]
- 7.Buse JB, Rosenstock J, Sesti G, Schmidt WE, Montanya E, Brett JH, Zychma M, Blonde L, LEAD-6 Study Group Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6) Lancet. 2009;374:39–47. doi: 10.1016/S0140-6736(09)60659-0. [DOI] [PubMed] [Google Scholar]
- 8.DeFronzo RA, Okerson T, Viswanathan P, Guan X, Holcombe JH, MacConell L. Effects of exenatide versus sitagliptin on postprandial glucose, insulin and glucagon secretion, gastric emptying, and caloric intake: a randomized, cross-over study. Curr Med Res Opin. 2008;24:2943–2952. doi: 10.1185/03007990802418851. [DOI] [PubMed] [Google Scholar]
- 9.Pratley RE, Nauck M, Bailey T, Montanya E, Cuddihy R, Filetti S, Thomsen AB, Søndergaard RE, Davies M, 1860-LIRA-DPP-4 Study Group Liraglutide versus sitagliptin for patients with type 2 diabetes who did not have adequate glycaemic control with metformin: a 26-week, randomised, parallel-group, open-label trial. Lancet. 2010;375:1447–1456. doi: 10.1016/S0140-6736(10)60307-8. [DOI] [PubMed] [Google Scholar]
- 10.Brunton S. GLP-1 receptor agonists vs. DPP-4 inhibitors for type 2 diabetes: is one approach more successful or preferable than the other? Int J Clin Pract. 2014;68:557–67. doi: 10.1111/ijcp.12361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Non-Insulin Therapies for Diabetes: GLP-1 Agonists, DPP4 Inhibitors and SGLT2 Inhibitors. URL: http://www.prnewswire.com/news-releases/non-insulin-therapies-for-diabetes-glp-1-agonists-dpp4-inhibitors-and-sglt2-inhibitors-2016—2026-300317435.html.
- 12.Harrison G. Insulin in alcoholic solution by the mouth. Br Med J. 1923;2:1204–5. doi: 10.1136/bmj.2.3286.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aguirre TAS, Teijeiro-Osorio D, Rosa M, Coulter IS, Alonso MJ, Brayden DJ. Current status of selected oral peptide technologies in advanced preclinical development and in clinical trials. Adv Drug Deliv Rev. 2016 doi: 10.1016/j.addr.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Pawar VK, Meher JG, Singh Y, Chaurasia M, Surendar Reddy B, Chourasia MK. Targeting of gastrointestinal tract for amended delivery of protein/peptide therapeutics: Strategies and industrial perspectives. J Control Release. 2014;196:168–183. doi: 10.1016/j.jconrel.2014.09.031. [DOI] [PubMed] [Google Scholar]
- 15.Tang BC, Dawson M, Lai SK, Wang Y-Y, Suk JS, Yang M, Zeitlin P, Boyle MP, Fu J, Hanes J. Biodegradable polymer nanoparticles that rapidly penetrate the human mucus barrier. Proc Natl Acad Sci U S A. 2009;106:19268–19273. doi: 10.1073/pnas.0905998106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ensign LM, Cone R, Hanes J. Oral drug delivery with polymeric nanoparticles: The gastrointestinal mucus barriers. Adv Drug Deliv Rev. 2012;64:557–570. doi: 10.1016/j.addr.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17*.He Z, Santos JL, Tian H, Huang H, Hu Y, Liu L, Leong KW, Chen Y, Mao H-Q. Scalable fabrication of size-controlled chitosan nanoparticles for oral delivery of insulin. Biomaterials. 2017;130:28–41. doi: 10.1016/j.biomaterials.2017.03.028. The authors describe a new method, termed flash nanocomplexation, for encapsulation of insulin into nanoparticles. Using this method, the insulin-loaded nanoparticles are smaller in size, have a narrower size distribution and possess an encapsulation efficiency up to 90%. In addition, these nanoparticles control blood glucose levels in rats more efficiency than the larger nanoparticles. [DOI] [PubMed] [Google Scholar]
- 18.Leonaviciute G, Bernkop-Schnürch A. Self-emulsifying drug delivery systems in oral (poly)peptide drug delivery. Expert Opin Drug Deliv. 2015;12:1703–1716. doi: 10.1517/17425247.2015.1068287. [DOI] [PubMed] [Google Scholar]
- 19.Taverner A, Dondi R, Almansour K, Laurent F, Owens S-E, Eggleston IM, Fotaki N, Mrsny RJ. Enhanced paracellular transport of insulin can be achieved via transient induction of myosin light chain phosphorylation. J Control Release. 2015;210:189–97. doi: 10.1016/j.jconrel.2015.05.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yoshida M, Kamei N, Muto K, Kunisawa J, Takayama K, Peppas NA, Takeda-Morishita M. Complexation hydrogels as potential carriers in oral vaccine delivery systems. Eur J Pharm Biopharm. 2017;112:138–142. doi: 10.1016/j.ejpb.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 21.Gupta V, Hwang BH, Doshi N, Mitragotri S. A permeation enhancer for increasing transport of therapeutic macromolecules across the intestine. J Control Release. 2013;172:541–549. doi: 10.1016/j.jconrel.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Marasini N, Skwarczynski M, Toth I. Oral delivery of nanoparticle-based vaccines. Expert Rev Vaccines. 2014;13:1361–1376. doi: 10.1586/14760584.2014.936852. [DOI] [PubMed] [Google Scholar]
- 23.Nakamura K, Murray RJ, Joseph JI, Peppas NA, Morishita M, Lowman AM. Oral insulin delivery using P(MAA-g-EG) hydrogels: effects of network morphology on insulin delivery characteristics. J Control Release. 2004;95:589–599. doi: 10.1016/j.jconrel.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 24.des Rieux A, Fievez V, Garinot M, Schneider Y-J, Préat V. Nanoparticles as potential oral delivery systems of proteins and vaccines: A mechanistic approach. J Control Release. 2006;116:1–27. doi: 10.1016/j.jconrel.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 25.Tortora GJ. Principles of Human Anatomy. Wiley; 2010. [Google Scholar]
- 26.Metcalf AM, Phillips SF, Zinsmeister AR, MacCarty RL, Beart RW, Wolff BG. Simplified assessment of segmental colonic transit. Gastroenterology. 1987;92:40–7. doi: 10.1016/0016-5085(87)90837-7. [DOI] [PubMed] [Google Scholar]
- 27.Degen LP, Phillips SF. Variability of gastrointestinal transit in healthy women and men. Gut. 1996;39:299–305. doi: 10.1136/gut.39.2.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Derrickson BH, Tortora GJ. Principles of anatomy and physiology. Wiley; 2008. [Google Scholar]
- 29.Hall JE, John E, Guyton AC. Guyton and Hall textbook of medical physiology. Saunders Elsevier; 2011. [Google Scholar]
- 30.Smart pills market by application (capsule endoscopy, drug delivery, patient monitoring), target area (esophagus, stomach, small intestine, large intestine) & geography - global forecast to 2024. Research and Markets. 2015 doi:3616568. [Google Scholar]
- 31.Höög CM, Bark L-Å, Arkani J, Gorsetman J, Broström O, Sjöqvist U. Capsule retentions and incomplete capsule endoscopy examinations: an analysis of 2300 examinations. Gastroenterol Res Pract. 2012;2012:518718. doi: 10.1155/2012/518718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Delvaux M, Ben Soussan E, Laurent V, Lerebours E, Gay G. Clinical evaluation of the use of the M2A patency capsule system before a capsule endoscopy procedure, in patients with known or suspected intestinal stenosis. Endoscopy. 2005;37:801–807. doi: 10.1055/s-2005-870241. [DOI] [PubMed] [Google Scholar]
- 33.Chaddock G, Lam C, Hoad CL, Costigan C, Cox EF, Placidi E, Thexton I, Wright J, Blackshaw PE, Perkins AC, et al. Novel MRI tests of orocecal transit time and whole gut transit time: studies in normal subjects. Neurogastroenterol Motil. 2014;26:205–214. doi: 10.1111/nmo.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bass DM, Prevo M, Waxman DS. Gastrointestinal safety of an extended-release, nondeformable, oral dosage form (OROS): a retrospective study. Drug Saf. 2002;25:1021–1033. doi: 10.2165/00002018-200225140-00004. [DOI] [PubMed] [Google Scholar]
- 35.Alcock R, Cottingham MG, Rollier CS, Furze J, De Costa SD, Hanlon M, Spencer AJ, Honeycutt JD, Wyllie DH, Gilbert SC, et al. Long-term thermostabilization of live poxviral and adenoviral vaccine vectors at supraphysiological temperatures in carbohydrate glass. Sci Transl Med. 2010;2 doi: 10.1126/scitranslmed.3000490. [DOI] [PubMed] [Google Scholar]
- 36.Drugs@FDA: FDA Approved Drug Products. https://www.accessdata.fda.gov/scripts/cder/daf/
- 37.Ferrua MJ, Singh RP. Modeling the fluid dynamics in a human stomach to gain insight of food digestion. J Food Sci. 2010;75:R151–62. doi: 10.1111/j.1750-3841.2010.01748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sher Akbar N, Nadeem S. Simulation of peristaltic flow of chyme in small intestine for couple stress fluid. Meccanica. 2014;49:325–334. [Google Scholar]
- 39.Gao X, Cao Y, Song X, Zhang Z, Zhuang X, He C, Chen X. Biodegradable, pH-responsive carboxymethyl cellulose/poly(acrylic acid) hydrogels for oral insulin delivery. Macromol Biosci. 2014;14:565–75. doi: 10.1002/mabi.201300384. [DOI] [PubMed] [Google Scholar]
- 40.Andrews GP, Laverty TP, Jones DS. Mucoadhesive polymeric platforms for controlled drug delivery. Eur J Pharm Biopharm. 2009;71:505–518. doi: 10.1016/j.ejpb.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 41*.Fox CB, Cao Y, Nemeth CL, Chirra HD, Chevalier RW, Xu AM, Melosh NA, Desai TA. Fabrication of sealed nanostraw microdevices for oral drug delivery. ACS Nano. 2016;10:5873–5881. doi: 10.1021/acsnano.6b00809. The authors demonstrate that patterning microdevices with nanostraw membranes can help tune the drug release and increase oral drug delivery due to its potential to bind the gastrointestinal tissue and capacity to deliver high drug concentrations locally for extended time periods. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42*.Banerjee A, Lee J, Mitragotri S. Intestinal mucoadhesive devices for oral delivery of insulin. Bioeng Transl Med. 2016 doi: 10.1002/btm2.10015. The oral intestinal mucoadhesive device reported by Banerjee et al. prepared by combining a permeation enhancer and intestinal devices loaded with insulin, demonstrated to significantly decrease the blood glucose levels in rats. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sharma M, Sharma V, Panda AK, Majumdar DK. Development of enteric submicron particle formulation of papain for oral delivery. Int J Nanomedicine. 2011;6:2097–111. doi: 10.2147/IJN.S23985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cui J, Zheng X, Hou W, Zhuang Y, Pi X, Yang J. The study of a remote-controlled gastrointestinal drug delivery and sampling system. Telemed e-Health. 2008;14:715–719. doi: 10.1089/tmj.2007.0118. [DOI] [PubMed] [Google Scholar]
- 45.Becker D, Zhang J, Heimbach T, Penland RC, Wanke C, Shimizu J, Kulmatycki K. Novel orally swallowable IntelliCap(®) device to quantify regional drug absorption in human GI tract using diltiazem as model drug. AAPS PharmSciTech. 2014;15:1490–7. doi: 10.1208/s12249-014-0172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stewart MP, Sharei A, Ding X, Sahay G, Langer R, Jensen KF. In vitro and ex vivo strategies for intracellular delivery. Nature. 2016;538:183–192. doi: 10.1038/nature19764. [DOI] [PubMed] [Google Scholar]
- 47.Can “Robotic” Pills Replace Injections? URL https://www.wsj.com/articles/can-8216robotic8217-pills-replace-injections-1392681501?tesla=y.
- 48*.Traverso G, Schoellhammer CM, Schroeder A, Maa R, Lauwers GY, Polat BE, Anderson DG, Blankschtein D, Langer R, Anderson D. Microneedles for drug delivery via the gastrointestinal tract HHS public access. J Pharm Sci. 2015;104:362–367. doi: 10.1002/jps.24182. This paper reports an in vivo proof-of-concept of the feasibility and safety of microneedles-based systems to deliver macromolecules in the gastrointestinal tract. In addition, this is the first study to note that the administration of insulin directly to the gastrointestinal tract led to a more robust hypoglycemic effect than a subcutaneous injection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49*.Aran K, Chooljian M, Paredes J, Rafi M, Lee K, Kim AY, An J, Yau JF, Chum H, Conboy I, et al. An oral microjet vaccination system elicits antibody production in rabbits. Sci Transl Med. 2017;9 doi: 10.1126/scitranslmed.aaf6413. This research paper shows the potential of MucoJet, a high pressure liquid jet, to deliver vaccines and other drugs into the buccal mucosa without the need of needles. In particular, a high immune response against ovalbumin was obtained using this technology in rabbits. [DOI] [PubMed] [Google Scholar]
- 50*.Schoellhammer CM, Schroeder A, Maa R, Lauwers GY, Swiston A, Zervas M, Barman R, DiCiccio AM, Brugge WR, Anderson DG, et al. Ultrasound-mediated gastrointestinal drug delivery. Sci Transl Med. 2015;7 doi: 10.1126/scitranslmed.aaa5937. Ultrasound has been shown to increase drug delivery in the gastrointestinal tract. In particular, it enhanced one order of magnitude delivery of mesalamine in pigs as well as achieved systemic delivery macromolecules such as insulin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schoellhammer CM, Lauwers GY, Goettel JA, Oberli MA, Cleveland C, Park JY, Minahan D, Chen Y, Anderson DG, Jaklenec A, et al. Ultrasound-mediated delivery of RNA to colonic mucosa of live mice. Gastroenterology. 2017;152:1151–1160. doi: 10.1053/j.gastro.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ravi AD, Sadhna D, Nagpaal D, Chawla L. Needle free injection technology: A complete insight. Int J Pharm Investig. 2015;5:192–9. doi: 10.4103/2230-973X.167662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ahmad N, Mohd Amin MCI, Ismail I, Buang F. Enhancement of oral insulin bioavailability: in vitro and in vivo assessment of nanoporous stimuli-responsive hydrogel microparticles. Expert Opin Drug Deliv. 2016;13:621–632. doi: 10.1517/17425247.2016.1160889. [DOI] [PubMed] [Google Scholar]
- 54.Nahata MC, Allen LV. Extemporaneous drug formulations. Clin Ther. 2008;30:2112–2119. doi: 10.1016/j.clinthera.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 55.Diamond S, Lavallee DC. Experience with a pill-swallowing enhancement aid. Clin Pediatr (Phila) 2010;49:391–393. doi: 10.1177/0009922809355313. [DOI] [PubMed] [Google Scholar]


