Abstract
Objective
To characterize lifetime and current rates of attention-deficit/hyperactivity disorder (ADHD) treatments among US children and adolescents with current ADHD and describe the association of these treatments with demographic and clinical factors.
Study design
Data are from the 2014 National Survey of the Diagnosis and Treatment of ADHD and Tourette Syndrome, a follow-back survey of parents from the 2011–2012 National Survey of Children’s Health. Weighted analyses focused on receipt of ADHD treatment among children aged 4–17 years with current ADHD (n = 2495) by 4 treatment types: medication, school supports, psychosocial interventions, and alternative treatments.
Results
Medication and school supports were the most common treatments received, with two-thirds of children and adolescents with ADHD currently receiving each treatment. Social skills training was the most common psychosocial treatment ever received (39%), followed by parent training (31%), peer intervention (30%), and cognitive behavioral therapy (20%). Among alternative treatments, 9% were currently taking dietary supplements, and 11% had ever received neurofeedback. Most children (67%) had received at least 2 of the following: current medication treatment, current school supports, or lifetime psychosocial treatment; 7% had received none of these 3 treatment types.
Conclusions
A majority of school-aged children and adolescents with ADHD received medication treatment and school supports, whereas fewer received recommended psychosocial interventions. Efforts to increase access to psychosocial treatments may help close gaps in service use by groups currently less likely to receive treatment, which is important to ensure that the millions of school-aged US children diagnosed with ADHD receive quality treatment.
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that begins in childhood, results in pervasive functional impairment, and has been diagnosed in 11% of children aged 4–17 years in the US.1,2 Children with ADHD are more likely than their peers to experience adverse long-term outcomes, including poor school outcomes, more frequent injury, higher rates of co-occurring psychiatric disorders, and greater healthcare utilization.3–6 Treatment guidelines recommend management of patients with ADHD according to the chronic care model.7
Medication treatment and parent- and teacher-delivered behavior therapy are evidence-based strategies for ADHD treatment; behavior therapy is recommended as the first-line treatment for children younger than 6 years, whereas combination therapy (behavior therapy and medication treatment) is recommended for children aged 6–11 years and preferred for children aged 12 years and older.7–9 A previous study of national parent survey data indicated that less than one-half of children with current ADHD (44%) received behavior therapy within the past year, whereas 74% received medication in the past week, with differences in treatment receipt by demographic factors such as age, race/ethnicity, and poverty status.10 However, these data did not allow for estimates by particular type of behavioral intervention (eg, peer interventions, parent training, school-based treatments), specifically forms that have empirical support as ADHD treatment.8,11–13 Other studies have shown trends in psychotherapy use relative to medication usage among children with ADHD,14–16 though there is limited published information available regarding specific types of psychological treatment received by children and adolescents with ADHD in the community.
The purpose of the present study is to characterize lifetime and current rates of pharmacologic and nonpharmacologic ADHD treatments overall and by demographic and clinical factors among a nationally drawn sample of children and adolescents with ADHD. This information can be used to describe the current status of ADHD treatment relative to best practices and may inform future research that seeks to identify barriers to receipt of recommended treatments as well as policy and programmatic efforts to promote more widespread use of recommended treatments for children with ADHD.
Methods
This study used data from the ADHD module of the 2014 National Survey of the Diagnosis and Treatment of ADHD and Tourette Syndrome (NS-DATA), a follow-back survey of a nationally drawn subgroup of respondent households from the 2011–2012 US National Survey of Children’s Health (NSCH). This survey was sponsored by the Centers for Disease Control and Prevention’s National Center on Birth Defects and Developmental Disabilities and National Center for Health Statistics. A complete description of this survey and sample population has been published elsewhere.17,18 Briefly, NS-DATA was a follow-up survey of respondent parents and guardians (hereafter referred to as parents) who reported that their child had ever received an ADHD diagnosis by a doctor or healthcare provider on the 2011–2012 NSCH. The response rate for NS-DATA was 47%; when combined with the 23% response rate from the 2011–2012 NSCH, the final NS-DATA response rate was 11%. There were 2966 completed interviews overall for the ADHD module of NS-DATA; however, the analyses for this study were restricted to the sample of parents with children aged 4–17 years who had current ADHD based on parent report at the time of NS-DATA (n = 2495). Secondary analysis of these existing deidentified survey data was considered exempt from Centers for Disease Control and Prevention institutional review board review.
This study focused on NS-DATA questions related to lifetime and current treatment received for ADHD. Specifically, parents were asked whether their child had ever taken medication for ADHD, and whether their child had ever received any of the following 7 types of other treatments for ADHD or difficulties with their child’s emotions, concentration or behavior: (1) “school-based educational support, intervention, or accommodation, such as tutoring, extra help from a teacher, preferential seating, extra time to complete work, or being enrolled in special education”; (2) “classroom management, such as reward systems, behavior modification, or a daily report card”; (3)“peer interventions, such as peer tutoring or the Good Behavior Game”19; (4) “social skills training, such as support in how to interact with others”; (5) “cognitive behavioral therapy” (CBT); (6) “dietary supplements, herbal supplements, or other nonprescription medications” (dietary supplements); or (7) “electroencephalogram neurofeedback or other kinds of biofeedback” (neurofeedback). If parents reported that their child had ever received any of these treatments or interventions, they were asked a follow-up question on whether the child was currently receiving the indicated treatment or intervention. Parents were also asked whether they had ever or were currently receiving parent training to help manage their child’s ADHD. For this analysis, school-based educational support, intervention, or accommodation and classroom management were grouped into a single category of school supports, and peer interventions, social skills training, CBT, and parent training were grouped into a psychosocial treatment category. To compare combinations of treatments, we focused on 3 categories: current medication, current school supports, and lifetime receipt of psychosocial treatments. The lifetime indicator was used for psychosocial treatments because of longer expected duration of effectiveness for these interventions20 compared with the expectation for medication or school supports.
Comparisons were made across the following child-level demographic characteristics: sex, age (4–11 years, 12–17 years), race (white, black, other), ethnicity (Hispanic/Latino, non-Hispanic/Latino), primary language in the household (English, other language), household poverty status (<100% of federal poverty level, 100%–199% of federal poverty level, ≥200% of federal poverty level), health insurance status (private, public, uninsured), continuous health insurance during previous 12 months (yes, no), and region of residence (Northeast, Midwest, South, West). Additional factors for comparison included current parent-reported ADHD severity (mild, moderate, severe), age when the child was first diagnosed with ADHD (before 6 years, 6–10 years, 11 years or older), and lifetime or current presence of any of the following co-occurring conditions: oppositional defiant disorder, conduct disorder, obsessive compulsive disorder, post-traumatic stress disorder, anxiety, bipolar disorder, other mood disorder such as depression, autism spectrum disorder or pervasive developmental disorder, sleep disorder, intellectual disability, learning disorder, language disorder, and tics. Treatment rates were also compared by whether the child had a medical home. The medical home indicator used by the National Center on Health Statistics incorporates the framework developed by the American Academy of Pediatrics.21 Medical homes are intended to optimize the effectiveness and efficiency of healthcare received by children by providing comprehensive and coordinated care. Individual indicators required to meet medical home criteria include having a personal physician or nurse, a usual place for care when sick, the ability to obtain needed referrals, family-centered care, and effective care coordination.22 Most demographic indicators and medical home status were from the 2011–2012 NSCH; poverty status, insurance status, and all other clinical indicators were collected in the 2014 NS-DATA survey.
Subgroup comparisons were tested for statistical significance using χ2 tests. All analyses were completed using SAS-callable SUDAAN v 11.0.1 (RTI International, Cary, North Carolina) to take into account the complex sample design and sampling weights to adjust for selection probability, noncoverage, and nonresponse to minimize potential bias related to these factors.
Results
There were survey responses for 2495 children and adolescents with current ADHD reported in this survey. The demographic description of the sample can be found in Table I (available at www.jpeds.com).
Table I.
Demographic and clinical characteristics of children with current ADHD (NS-DATA 2014)
| Characteristics | Unweighted N |
Weighted % (95% CI) |
|---|---|---|
| Sex* | ||
| Male | 1762 | 70.3 (67.1–73.4) |
| Female | 733 | 29.7 (26.6–32.9) |
| Age group | ||
| 4–11 y | 768 | 34.0 (30.7–37.4) |
| 12–17 y | 1727 | 66.0 (62.6–69.3) |
| Race* | ||
| White | 1940 | 71.7 (68.3–74.9) |
| Black | 232 | 16.2 (13.6–19.1) |
| Multiracial/other | 312 | 12.1 (9.9–14.7) |
| Ethnicity* | ||
| Non-Hispanic/Latino | 2276 | 84.8 (81.7–87.4) |
| Hispanic/Latino | 213 | 15.2 (12.6–18.3) |
| Primary language in the home* | ||
| English | 2462 | 96.7 (94.7–97.9) |
| Any other language | 32 | 3.3 (2.1–5.3) |
| Poverty status | ||
| <100% of federal poverty level | 350 | 28.0 (24.6–31.7) |
| 100%-199% of federal poverty level | 460 | 22.3 (19.4–25.5) |
| ≥200% of federal poverty level | 1559 | 49.7 (46.1–53.2) |
| Any healthcare coverage | ||
| Public insurance | 953 | 49.7 (46.2–53.2) |
| Private insurance | 1467 | 48.6 (45.2–52.1) |
| No insurance | 37 | 1.6 (0.9–2.9) |
| Continuous insurance over past year | ||
| Yes | 2316 | 93.6 (91.5–95.3) |
| No | 117 | 6.4 (4.7–8.6) |
| Receives care in a medical home* | ||
| Yes | 1218 | 43.5 (40.0–46.9) |
| No | 1208 | 56.6 (53.1–60.0) |
| Region* | ||
| Northeast | 422 | 15.3 (13.5–17.3) |
| Midwest | 592 | 22.5 (20.5–24.7) |
| South | 990 | 44.0 (41.5–46.6) |
| West | 491 | 18.2 (16.3–20.2) |
| Current ADHD severity | ||
| Mild | 814 | 30.3 (27.3–33.5) |
| Moderate | 1247 | 49.9 (46.4–53.4) |
| Severe | 416 | 19.9 (17.1–23.0) |
| Age at diagnosis | ||
| Diagnosed before age 6 y | 719 | 32.2 (29.0–35.6) |
| Diagnosed at age 6-10 y | 1535 | 59.6 (56.1–63.0) |
| Diagnosed at or after age 11 y | 208 | 8.2 (6.6–10.3) |
| Ever co-occurring condition† | ||
| None | 637 | 23.9 (21.1–26.9) |
| Any | 1858 | 76.1 (73.1–78.9) |
| Current co-occurring condition† | ||
| None | 935 | 34.3 (31.1–37.6) |
| Any | 1560 | 65.7 (62.4–68.9) |
Indicator collected during 2011-2012 NSCH interview.
Co-occurring conditions included oppositional defiant disorder, conduct disorder, obsessive compulsive disorder, post-traumatic stress disorder, anxiety, bipolar disorder, other mood disorder such as depression, autism spectrum disorder or pervasive developmental disorder, sleep disorder, intellectual disability, learning disorder, language disorder, and/or tics.
Medication was the most commonly received ADHD treatment, with 90.8% of children in this study with current ADHD having ever received medication for ADHD (Figure, Table II). The second most common treatment ever received was school supports, with 85.8% of children with ADHD having received school accommodations and/or classroom management at some point in their lives. Nearly two-thirds of children (62.2%) had ever received at least 1 of the 4 psychosocial treatments. Specifically, approximately one-third of children with ADHD had ever received social skills training (38.7%), parent training (30.9%), or peer intervention (30.2%), whereas 19.8% had ever received CBT. Just under one-fifth of children with ADHD had ever received dietary supplements (17.8%) and approximately one-tenth had ever received neurofeedback (11.4%).
Figure.
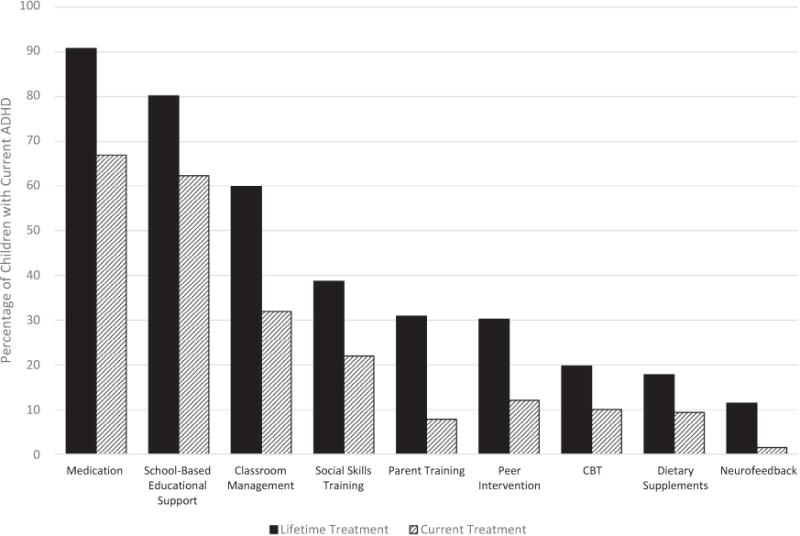
Graph showing percentage of children 4–17 years of age with current ADHD receiving treatment, by treatment type (medication, school-based educational support, classroom management, social skills training, parent training, peer intervention, cognitive behavioral therapy, dietary supplements, and neurofeedback) (NS-DATA 2014).
Table II.
Weighted prevalence of types of treatment currently and ever received (lifetime) by children and adolescents aged 4–17 years with current ADHD (NS-DATA 2014)
| Currently receiving…
|
Lifetime… |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medication |
School support*
|
Psychosocial treatments†
|
Medication |
School support*
|
Psychosocial treatments†
|
|||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Overall | 66.9 | (63.5–70.2) | 64.7 | (61.4–68.0) | 32.5 | (29.2–36.0) | 90.8 | (88.4–92.7) | 85.8 | (83.2–88.0) | 62.2 | (58.8–65.5) |
| Sex‡ | ||||||||||||
| Male | 67.3 | (63.2–71.3) | 65.2 | (61.2–69.0) | 33.9 | (29.9–38.1) | 90.8 | (87.8–93.1) | 86.8 | (83.8–89.3) | 63.9 | (59.9–67.8) |
| Female | 66.0 | (59.6–71.9) | 63.6 | (57.3–69.6) | 29.3 | (23.7–35.5) | 90.7 | (86.2–93.8) | 83.3 | (77.8–87.6) | 58.0 | (51.7–64.1) |
| Age group | ||||||||||||
| 4–11 y | 76.1 | (70.4–80.9) | 71.7 | (66.0–76.7) | 44.7 | (38.7–50.9) | 88.5 | (83.8–92.0) | 85.8 | (81.1–89.5) | 69.6 | (63.9–74.7) |
| 12–17y | 62.3 | (57.9–66.4) | 61.2 | (56.9–65.2) | 26.1 | (22.5–30.2) | 91.9 | (89.0–94.1) | 85.7 | (82.5–88.5) | 58.4 | (54.1–62.6) |
| Race‡ | ||||||||||||
| White | 69.2 | (65.2–72.8) | 63.3 | (59.5–67.0) | 29.5 | (25.9–33.4) | 93.3 | (90.9–95.2) | 84.0 | (80.8–86.7) | 59.6 | (55.7–63.5) |
| Black | 61.6 | (51.8–70.6) | 68.0 | (58.2–76.5) | 44.8 | (35.3–54.7) | 83.3 | (74.7–89.5) | 89.4 | (81.9–94.0) | 65.2 | (55.3–74.0) |
| Multiracial/other | 61.1 | (50.2–70.9) | 67.3 | (56.5–76.6) | 32.5 | (23.4–43.1) | 86.4 | (77.2–92.2) | 91.0 | (83.0–95.4) | 73.4 | (63.6–81.3) |
| Ethnicity‡ | ||||||||||||
| Non-Hispanic/Latino | 68.8 | (65.2–72.2) | 64.6 | (61.0–68.0) | 31.4 | (28.0–35.1) | 92.3 | (90.0–94.0) | 85.0 | (82.2–87.4) | 60.6 | (56.9–64.2) |
| Hispanic/Latino | 56.9 | (46.2–67.0) | 64.5 | (53.8–73.9) | 35.9 | (26.2–46.9) | 83.3 | (73.1–90.1) | 89.3 | (79.9–94.6) | 69.6 | (59.4–78.1) |
| Primary language in the home‡ | ||||||||||||
| English | 67.5 | (64.0–70.8) | 64.3 | (60.9–67.6) | 31.6 | (28.3–35.0) | 91.6 | (89.3–93.4) | 85.3 | (82.6–87.6) | 61.7 | (58.2–65.1) |
| Any other language | 50.8 | (28.4–72.9) | 76.9 | (53.4–90.6) | 61.1 | (36.6–81.0) | 68.4 | (42.6–86.3) | 99.9 | (99.2–100.0) | 76.7 | (52.9–90.6) |
| Percentage of federal poverty level | ||||||||||||
| <100% | 63.8 | (55.9–71.0) | 66.4 | (58.4–73.5) | 44.1 | (36.3–52.2) | 85.2 | (78.7–90.0) | 88.1 | (81.7–92.4) | 73.2 | (65.5–79.7) |
| 100%-199% | 63.6 | (55.6–70.9) | 66.2 | (58.5–73.1) | 34.8 | (27.7–42.6) | 92.2 | (86.7–95.5) | 85.7 | (79.3–90.3) | 62.9 | (55.0–70.1) |
| ≥200% | 69.4 | (64.9–73.6) | 62.0 | (57.6–66.3) | 23.8 | (20.2–27.8) | 93.0 | (90.0–95.1) | 83.8 | (80.1–86.9) | 56.0 | (51.4–60.4) |
| Any healthcare coverage | ||||||||||||
| Public insurance | 67.9 | (62.6–72.9) | 68.7 | (63.4–73.5) | 41.9 | (36.6–47.5) | 89.7 | (85.8–92.6) | 87.9 | (83.9–91.0) | 70.1 | (64.8–74.8) |
| Private insurance | 66.7 | (62.0–71.0) | 62.2 | (57.7–66.5) | 23.4 | (19.7–27.6) | 91.9 | (88.6–94.3) | 84.4 | (80.8–87.4) | 55.5 | (50.9–60.0) |
| Uninsured | 48.6 | (23.5–74.4) | 36.1§ | (17.1–60.8) | 11.6¶ | (4.1–29.0) | 91.8 | (77.6–97.3) | 75.6 | (43.3–92.6) | 26.0§ | (11.9–47.6) |
| Continuous insurance over past year | ||||||||||||
| No | 45.4 | (31.1–60.4) | 59.0 | (43.2–73.2) | 27.2 | (16.2–42.1) | 86.9 | (71.2–94.7) | 82.2 | (66.0–91.6) | 51.2 | (36.0–66.2) |
| Yes | 69.0 | (65.5–72.3) | 65.6 | (62.1–68.9) | 33.0 | (29.6–36.7) | 91.1 | (88.6–93.0) | 86.1 | (83.5–88.4) | 63.7 | (60.2–67.1) |
| Receives care in a medical home‡ | ||||||||||||
| No | 64.8 | (59.9–69.4) | 69.5 | (64.8–73.8) | 36.7 | (32.1–41.6) | 89.9 | (86.4–92.6) | 89.9 | (86.6–92.4) | 68.8 | (64.2–73.1) |
| Yes | 70.4 | (65.3–75.0) | 57.6 | (52.4–62.6) | 25.7 | (21.3–30.7) | 93.1 | (89.8–95.3) | 80.2 | (75.6–84.0) | 53.2 | (48.0–58.4) |
| Region‡ | ||||||||||||
| Northeast | 67.5 | (58.3–75.6) | 71.3 | (62.5–78.8) | 36.7 | (28.3–46.0) | 87.2 | (79.8–92.2) | 85.9 | (77.4–91.6) | 65.8 | (56.7–73.8) |
| Midwest | 69.0 | (62.0–75.3) | 68.1 | (61.8–73.9) | 38.2 | (31.4–45.4) | 94.9 | (91.1–97.2) | 87.0 | (82.4–90.5) | 61.9 | (55.0–68.3) |
| South | 66.4 | (60.9–71.5) | 64.0 | (58.7–69.1) | 32.1 | (27.1–37.6) | 91.1 | (87.0–94.0) | 85.2 | (81.1–88.6) | 59.6 | (54.1–64.8) |
| West | 65.1 | (57.0–72.5) | 56.6 | (48.5–64.3) | 22.9 | (16.8–30.4) | 87.7 | (80.7–92.4) | 85.4 | (78.2–90.5) | 65.9 | (58.2–73.0) |
| Current ADHD severity | ||||||||||||
| Mild | 53.8 | (47.6–59.8) | 53.9 | (47.8–59.9) | 21.3 | (16.5–27.1) | 84.9 | (79.8–88.9) | 83.0 | (78.0–87.1) | 51.1 | (44.9–57.3) |
| Moderate | 69.7 | (64.7–74.2) | 65.8 | (61.0–70.3) | 34.3 | (29.6–39.3) | 92.5 | (88.9–95.0) | 84.9 | (81.1–88.1) | 65.5 | (60.7–70.0) |
| Severe | 79.8 | (71.7–86.0) | 78.9 | (70.5–85.3) | 44.8 | (36.7–53.2) | 95.4 | (89.9–97.9) | 92.8 | (86.2–96.4) | 71.2 | (62.7–78.5) |
| Age of diagnosis | ||||||||||||
| Before 6 y | 73.3 | (67.3–78.5) | 72.2 | (66.1–77.6) | 47.5 | (41.1–54.0) | 91.7 | (88.0–94.3) | 88.6 | (83.9–92.0) | 74.7 | (68.8–79.9) |
| 6–10 y | 64.8 | (60.1–69.1) | 62.4 | (57.9–66.6) | 25.6 | (21.8–29.9) | 90.0 | (86.4–92.7) | 85.4 | (81.9–88.4) | 57.3 | (52.7–61.7) |
| 11 y or older | 59.5 | (47.7–70.4) | 52.7 | (41.0–64.1) | 23.1 | (14.2–35.2) | 92.2 | (82.8–96.7) | 76.1 | (65.1–84.4) | 49.1 | (37.5–60.8) |
| Ever co-occurring condition** | ||||||||||||
| None | 62.4 | (55.1–69.1) | 43.3 | (36.5–50.3) | 12.8 | (8.6–18.6) | 90.4 | (84.9–94.0) | 75.2 | (68.6–80.8) | 38.2 | (31.6–45.3) |
| Any | 68.4 | (64.4–72.1) | 71.5 | (67.7–74.9) | 38.7 | (34.8–42.8) | 90.9 | (88.1–93.1) | 89.1 | (86.3–91.3) | 69.8 | (65.9–73.3) |
| Current co-occurring condition** | ||||||||||||
| None | 63.5 | (57.6–69.0) | 40.4 | (35.0–46.1) | 13.3 | (9.7–18.0) | 90.4 | (86.0–93.5) | 74.7 | (69.3–79.4) | 42.3 | (36.7–48.1) |
| Any | 68.7 | (64.4–72.8) | 77.4 | (73.6–80.8) | 42.5 | (38.2–47.0) | 91.0 | (87.9–93.3) | 91.5 | (88.8–93.7) | 72.6 | (68.5–76.4) |
Bold = overall χ2 test was statistically significant (P < .05).
Underline = overall χ2 test approached statistical significance (.05 ≤ P < .10).
School supports include school-based educational support and/or classroom management.
Psychosocial treatments include peer interventions, social skills training, cognitive behavioral therapy, and/or parent training.
Subgroup classification data from 2011–2012 NSCH.
Estimate is unstable and may be unreliable. It has a relative SE between 30% and 50% and should be interpreted with caution.
Estimate is unreliable. It has a relative SE larger than 50% and should not be used except for inferential statistics (eg, comparisons with other estimates).
Co-occurring conditions included oppositional defiant disorder, conduct disorder, obsessive compulsive disorder, post-traumatic stress disorder, anxiety, bipolar disorder, other mood disorder such as depression, autism spectrum disorder or pervasive developmental disorder, sleep disorder, intellectual disability, learning disorder, language disorder, and/or tics.
Approximately two-thirds of children with current ADHD were currently receiving medication (66.9%), and a similar percentage (64.7%) were receiving school supports (Figure, Table II). About one-third of children with current ADHD were currently receiving at least 1 of the psychosocial treatments (32.5%) at the time of the survey; 22.0% were receiving social skills training, 12.0% were receiving peer interventions, 10.1% were receiving CBT, and 7.9% had parents receiving parent training. Approximately 1 in 10 children were currently receiving dietary supplements (9.3%), and few children were currently receiving neurofeedback (1.5%).
Considering the combination of current medication treatment, current school supports, and lifetime psychosocial treatment, one-third of children with ADHD (33.6%) had received all three treatments, and another one third (33.2%) had received 2 of the 3. Of the remaining treatment combinations, 13.4% were receiving only current medication, 6.7% were receiving only current school supports, 6.3% had received only lifetime psychosocial treatment, and 6.9% had received none of the 3 treatment types.
Rates of lifetime and current treatments are presented in Table II. Demographic comparisons are discussed below using the indicators of current medication and school supports, and lifetime services for all psychosocial interventions, with the time frame used for each treatment type being selected based on duration of anticipated treatment effectiveness. Rates of lifetime psychosocial interventions by type (social skills training, peer interventions, CBT, parent training) are presented in Table III.
Table III.
Weighted prevalence of types of lifetime psychosocial treatment received by children and adolescents aged 4–17 years with current ADHD (NS-DATA 2014)
| Social skills training
|
Parent training |
Peer interventions |
Cognitive behavioral therapy
|
|||||
|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Overall | 38.7 | (35.4–42.2) | 30.9 | (27.7–34.2) | 30.2 | (27.0–33.6) | 19.8 | (17.0–22.8) |
| Sex* | ||||||||
| Male | 39.3 | (35.3–43.5) | 30.8 | (27.1–34.8) | 31.6 | (27.7–35.8) | 19.4 | (16.2–23.1) |
| Female | 37.3 | (31.5–43.5) | 31.1 | (25.5–37.3) | 26.9 | (21.7–32.9) | 20.7 | (15.9–26.5) |
| Age group | ||||||||
| 4–11 y | 47.4 | (41.4–53.5) | 34.0 | (28.4–40.0) | 34.4 | (28.7–40.5) | 25.0 | (19.9–31.0) |
| 12–17 y | 34.2 | (30.3–38.3) | 29.3 | (25.6–33.3) | 28.1 | (24.3–32.2) | 17.0 | (14.0–20.5) |
| Race* | ||||||||
| White | 37.2 | (33.3–41.2) | 29.5 | (25.9–33.2) | 26.6 | (23.1–30.4) | 16.9 | (14.0–20.2) |
| Black | 44.9 | (35.6–54.6) | 31.5 | (23.3–41.0) | 43.4 | (34.0–53.2) | 32.2 | (23.7–42.0) |
| Multiracial/other | 38.8 | (29.5–49.1) | 39.3 | (29.6–50.0) | 33.4 | (24.2–44.1) | 20.7 | (13.2–30.9) |
| Ethnicity* | ||||||||
| Non-Hispanic/Latino | 38.6 | (35.1–42.2) | 29.9 | (26.7–33.4) | 30.0 | (26.6–33.6) | 19.6 | (16.7–22.8) |
| Hispanic/Latino | 39.9 | (30.1–50.6) | 36.8 | (27.3–47.4) | 30.6 | (21.5–41.4) | 19.8 | (12.6–29.6) |
| Primary language in the home* | ||||||||
| English | 38.0 | (34.6–41.4) | 30.3 | (27.2–33.7) | 29.9 | (26.7–33.3) | 19.2 | (16.5–22.2) |
| Any other language | 60.2 | (36.3–80.0) | 46.3 | (24.6–69.5) | 38.8† | (18.9–63.4) | 39.5† | (18.3–65.5) |
| Percentage of federal poverty level | ||||||||
| <100% | 47.5 | (39.7–55.4) | 41.4 | (33.8–49.3) | 42.8 | (35.2–50.7) | 25.0 | (18.6–32.7) |
| 100%-199% | 41.0 | (33.7–48.8) | 28.8 | (22.6–35.9) | 27.5 | (21.1–35.0) | 19.2 | (13.8–26.3) |
| ≥200% | 32.1 | (28.2–36.4) | 26.7 | (23.0–30.8) | 23.9 | (20.1–28.2) | 17.7 | (14.4–21.5) |
| Any healthcare coverage | ||||||||
| Public insurance | 47.5 | (42.2–52.9) | 35.9 | (30.9–41.2) | 38.9 | (33.7–44.3) | 25.0 | (20.5–30.2) |
| Private insurance | 30.6 | (26.6–34.9) | 26.9 | (23.0–31.2) | 21.4 | (17.8–25.5) | 15.0 | (11.9–18.8) |
| Uninsured | 15.6† | (6.5–33.0) | 9.1‡ | (2.9–25.0) | 17.2† | (7.2–35.8) | 11.6† | (4.2–28.1) |
| Continuous insurance over past year | ||||||||
| No | 29.3 | (18.2–43.5) | 29.6 | (17.7–45.2) | 24.0 | (13.9–38.4) | 14.0† | (7.1–25.9) |
| Yes | 39.7 | (36.2–43.4) | 31.5 | (28.2–35.0) | 30.7 | (27.3–34.2) | 20.4 | (17.5–23.7) |
| Receives care in a medical home* | ||||||||
| No | 43.6 | (38.9–48.5) | 35.5 | (30.9–40.3) | 34.0 | (29.5–38.9) | 23.3 | (19.3–27.8) |
| Yes | 31.2 | (26.7–36.2) | 26.1 | (21.9–30.9) | 24.9 | (20.6–29.9) | 15.3 | (11.8–19.7) |
| Region* | ||||||||
| Northeast | 49.1 | (40.1–58.2) | 34.8 | (26.6–44.0) | 28.0 | (20.8–36.5) | 25.2 | (17.9–34.3) |
| Midwest | 41.8 | (35.2–48.8) | 32.5 | (26.4–39.2) | 31.8 | (25.4–38.9) | 22.7 | (17.2–29.4) |
| South | 34.9 | (29.9–40.4) | 27.3 | (22.8–32.4) | 32.4 | (27.4–37.8) | 17.9 | (14.0–22.6) |
| West | 35.2 | (27.9–43.2) | 34.1 | (26.7–42.4) | 24.8 | (18.2–32.9) | 16.1 | (10.6–23.6) |
| Current ADHD severity | ||||||||
| Mild | 26.2 | (21.2–32.0) | 26.5 | (21.5–32.1) | 27.1 | (21.7–33.3) | 13.9 | (9.9–19.1) |
| Moderate | 41.3 | (36.5–46.2) | 30.9 | (26.4–35.7) | 28.8 | (24.4–33.6) | 19.5 | (15.7–23.9) |
| Severe | 51.6 | (43.2–59.9) | 38.2 | (30.5–46.4) | 38.7 | (30.9–47.1) | 30.3 | (23.1–38.6) |
| Age of diagnosis | ||||||||
| Before 6 y | 53.7 | (47.3–60.0) | 38.4 | (32.4–44.7) | 38.6 | (32.5–45.0) | 28.6 | (23.0–34.9) |
| 6–10 y | 32.8 | (28.7–37.2) | 28.3 | (24.4–32.5) | 27.4 | (23.4–31.8) | 14.9 | (11.9–18.4) |
| 11 y or older | 23.3 | (14.5–35.3) | 20.0 | (12.3–30.8) | 17.3 | (9.7–28.9) | 23.0 | (13.8–35.8) |
| Ever co-occurring condition§ | ||||||||
| None | 15.1 | (10.9–20.7) | 19.0 | (14.1–25.1) | 16.4 | (11.8–22.4) | 3.6† | (1.8–7.1) |
| Any | 46.2 | (42.2–50.2) | 34.6 | (30.9–38.5) | 34.6 | (30.8–38.7) | 25.0 | (21.6–28.8) |
| Current co-occurring condition§ | ||||||||
| None | 18.2 | (14.4–22.9) | 19.5 | (15.4–24.3) | 17.2 | (13.2–22.2) | 6.6 | (4.4–9.9) |
| Any | 49.4 | (45.0–53.8) | 36.8 | (32.7–41.2) | 37.1 | (32.9–41.5) | 26.9 | (23.1–31.2) |
Bold = overall χ2 test was statistically significant (P < .05).
Underline = overall χ2 test approached statistical significance (.05 ≤ P < .10).
Subgroup classification data from 2011-12 NSCH.
Estimate is unstable and may be unreliable. It has a relative standard error between 30% and 50% and should be interpreted with caution.
Estimate is unreliable. It has a relative standard error larger than 50% and should not be used except for inferential statistics (e.g., comparisons with other estimates).
Co-occurring conditions included oppositional defiant disorder, conduct disorder, obsessive compulsive disorder, post-traumatic stress disorder, anxiety, bipolar disorder, other mood disorder such as depression, autism spectrum disorder or pervasive developmental disorder, sleep disorder, intellectual disability, learning disorder, language disorder, and/or tics.
Treatment rates varied for most demographic groups (Table II and III), though no differences were found for treatment rates by child sex or primary language used in the home. Younger children (4–11 years of age) were significantly more likely than older children (12–17 years of age) to receive each type of treatment with the exception of lifetime parent training (P = .19) and lifetime peer interventions (P = .08). Treatment rates were generally similar across ethnic groups except for current medication treatment, which was more common among non-Hispanic children than Hispanic children with ADHD (P = .04). Rates of lifetime peer interventions and CBT were significantly associated with race, with the highest rates among black children. Increasing poverty was associated with higher lifetime rates of peer interventions, social skills training, and parent training. Treatment rates were also strongly associated with healthcare coverage type for all treatments except for current medication treatment for which differences did not reach statistical significance. For school supports and psychosocial treatments, rates were highest among children with public insurance and lowest among children without insurance. With the exception of current medication treatment, treatment rates were significantly lower among children with a medical home; differences in medication rates did not reach statistical significance for children by medical home status. Regional differences were detected for receipt of social skills training, with the highest rates seen among children with ADHD in the Northeast.
The percentage of children receiving each ADHD treatment increased with parent-reported severity of the child’s ADHD (Tables II and III); this association between treatment rates and ADHD severity reached statistical significance for all but lifetime peer interventions and parent training, for which differences approached statistical significance (.05 ≤ P < .10). Of all the subgroups, children with severe ADHD were the most likely to receive medication (79.8%) and school supports (78.9%). In fact, these rates were the highest rates of any of the demographic or clinical indicator subgroups for any ADHD treatment.
The percentage of children receiving each treatment was significantly associated with age of diagnosis (Tables II and III). For all but CBT, there was an inverse relationship between age of diagnosis and the percentage receiving each treatment, with children receiving a diagnosis at a younger age being more likely to receive each treatment. For CBT, the lowest rate of treatment was among those diagnosed from 6 to 10 years of age (14.9%).
Children without a co-occurring disorder were as likely to receive medication treatment as children with a current or lifetime report of a co-occurring condition (Tables II and III). Children with a co-occurring condition were more likely than children with ADHD alone to be receiving school supports and each of the 4 types of psychosocial treatments (peer interventions, social skills training, CBT, and parent training).
Discussion
This study describes patterns of ADHD treatment for children aged 4–17 years with current ADHD using a large nationally drawn sample. The results suggest that the 2 most common types of ADHD treatments were current medication and school supports, with a minority of children with ADHD receiving other recommended treatments (eg, lifetime receipt of peer interventions or parents having received parent training) and a small percentage receiving alternative treatments such as dietary supplements and neurofeedback. When considering combinations of treatment, approximately two-thirds of children were receiving treatment from at least 2 categories (current medication, current school supports, or lifetime psychosocial treatments), and one-quarter were receiving treatment from only 1 category. Approximately 7% were not receiving treatment from any of these 3 categories.
Treatment rates varied independently by child age, race, ethnicity, socioeconomic status, and health insurance status but were similar across child sex and primary language in the home. Younger children and those who had received the ADHD diagnosis at a younger age were generally more likely to receive each type of treatment, suggesting a potential gap in services for adolescents and children diagnosed at older ages, particularly for lifetime receipt of psychosocial treatment. Similar to prior investigations,23 Hispanic children were less likely to receive medication than non-Hispanic children, possibly attributable to cultural attitudes toward ADHD medication use. Interestingly, black children and those from families with lower socioeconomic status were more likely to have received peer interventions and CBT, perhaps as a function of public insurance coverage. Not surprisingly, treatment rates were highest for children with severe ADHD, although approximately 20% of children with severe symptoms did not currently receive medication or school supports and more than one-quarter had never received psychosocial treatment. Receipt of care in a medical home was associated with lower rates of psychosocial treatment and school supports, potentially because of the previously documented inverse relationship of having a medical home and severity of condition; children without a medical home were more likely to have severe or multiple behavioral health conditions.24 Children with severe ADHD have more complex healthcare needs than children with milder ADHD and may benefit more from having patient-centered, comprehensive, and coordinated care, yet these are the children with ADHD least likely to have a medical home.
The low rates of lifetime behavioral parent training are of particular concern, particularly given the recommendation for parent training before medication in children younger than 6 years of age and the recommendation for combination therapy for older children.7 We have previously discussed the barriers to receipt of parent training such as lack of awareness about the benefits of behavior training, difficulty in identifying or accessing appropriate providers, and the initial cost and time investment needed for behavior training.16 Efforts to reduce these barriers and increase family access to parent training could increase the opportunity to improve the functional outcomes13 of nearly 1 million school-aged children with ADHD whose parents had not received behavioral parent training.
The NS-DATA represents the largest nationally drawn sample specifically of children with ADHD collected in the past 2 decades. Given the significant changes in treatment patterns over this time period,2 these unique data provide an opportunity to gain a deeper understanding of treatment patterns for the most common neurodevelopmental disorder of childhood. However, findings of this study should be taken within the context of several considerations. First, the NS-DATA included a predominantly school-aged sample (6–17 years), with very few 4- to 5-year-olds eligible for this survey. Second, this study followed up a cohort of children diagnosed with ADHD at the time of the 2011–2012 NSCH and, therefore, had the diagnosis for at least 2–3 years when NS-DATA was conducted. Therefore, the sample did not include children who were newly diagnosed and cannot describe treatment patterns among those who were recently diagnosed. A related limitation is that the follow-up survey did not collect information on all variables of interest, so some indicators (eg, having a medical home) were taken from the 2011–2012 NSCH survey and may not reflect the child’s current status. Third, this study was intended to provide a descriptive characterization of demographic and clinical factors related to treatment of ADHD, and the statistics presented do not adjust for these factors when considered together, which may limit interpretation of the strength of these associations overall. Fourth, the combined overall response rate for NS-DATA was low and may be subject to bias; however, the cooperation rate among successfully re-contacted eligible households was high (81%), and sampling weights were applied to attempt to mitigate nonresponse bias.17
There are some additional limitations related to the treatment variables specifically. First, the data in this study were collected from a single respondent and have not been validated against medical or school records. Second, we used the lifetime indicator for psychosocial treatments, which may have longer-term effectiveness, but for those not currently receiving each treatment, the data do not specify how long since the treatment was last received. Third, although this study included a more expansive list of ADHD treatments than previously collected in national surveys,2,10 the survey did not include some other treatment types that might be commonly used in practice such as play therapy and talk therapy. Finally, there may have been some variation in the type, length, quality, and status of the evidence base for some of the treatments reported in each question (particularly for school-based supports), and as such, this study’s estimates may not reflect the current prevalence of high quality, evidence-based treatments received by children with ADHD.
This national profile of ADHD treatment suggests that a majority of school-aged children with ADHD receive medication treatment and school services. However, fewer children receive recommended psychosocial interventions, including parent behavior training, which has the greatest strength of evidence for the treatment of ADHD in children younger than 6 years.8 Efforts to increase access to psychosocial treatments may help close gaps in service use by groups currently less likely to receive treatment, such as adolescents, those diagnosed later in childhood, and children without public health insurance. These efforts could include training paraprofessionals, using telehealth or mobile technology, or other innovative delivery methods. Additional research that further characterizes the types of psychosocial treatment and school supports received and how these services vary by children’s demographic, insurance, diagnostic, and impairment status as well as reasons why certain treatments are less likely to be received by specific subgroups could further inform policy efforts to ensure that quality treatment is received by the 5.1 million children and adolescents with current ADHD in the US.2
Glossary
- ADHD
Attention-deficit/hyperactivity disorder
- CBT
Cognitive behavioral therapy
- NSCH
National Survey of Children’s Health
- NS-DATA
National Survey of the Diagnosis and Treatment of ADHD and Tourette Syndrome
Footnotes
The authors declare no conflicts of interest.
Portions of this study were presented at the 6th World Congress on ADHD in Vancouver, Canada, April 20-23, 2017.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington (VA): American Psychiatric Association Publishing; 2013. [Google Scholar]
- 2.Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention- deficit/hyperactivity disorder: United States, 2003-2011. J Am Acad Child Adolesc Psychiatry. 2014;53:34–46, e32. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131:637–44. doi: 10.1542/peds.2012-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Merrill R, Lyon J, Baker R, Gren L. Attention Deficit Hyperactivity Disorder and increased risk of injury. Adv Med Sci. 2009;54:20–6. doi: 10.2478/v10039-009-0022-7. [DOI] [PubMed] [Google Scholar]
- 5.Pastor PN, Reuben CA. Identified attention-deficit/hyperactivity disorder and medically attended, nonfatal injuries: US school-age children, 1997-2002. Ambul Pediatr. 2006;6:38–44. doi: 10.1016/j.ambp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Long-term school outcomes for children with attention-deficit/hyperactivity disorder: a population-based perspective. J Dev Behav Pediatr. 2007;28:265–73. doi: 10.1097/DBP.0b013e31811ff87d. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1007–22. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charach A, Dashti B, Carson P, Booker L, Lim CG, Lillie E, et al. Attention deficit hyperactivity disorder: effectiveness of treatment in at-risk preschoolers; long-term effectiveness in all ages; and variability in prevalence, diagnosis, and treatment. Rockville (MD): Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 9.American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with attention- deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- 10.Visser SN, Bitsko RH, Danielson ML, Ghandour RM, Blumberg SJ, Schieve LA, et al. Treatment of attention-deficit/hyperactivity disorder among children with special health care needs. J Pediatr. 2015;166:1423–30. doi: 10.1016/j.jpeds.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DuPaul GJ, Eckert TL, Vilardo B. The effects of school-based interventions for Attention Deficit Hyperactivity Disorder: a meta-analysis 1996-2010. School Psych Rev. 2012;41:387–412. [Google Scholar]
- 12.Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA. 2016;315:1997–2008. doi: 10.1001/jama.2016.5453. [DOI] [PubMed] [Google Scholar]
- 13.Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with Attention-Deficit/Hyperactivity Disorder. J Clin Child Adolesc Psychol. 2014;43:527–51. doi: 10.1080/15374416.2013.850700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leslie LK, Wolraich ML. ADHD service use patterns in youth. J Pediatr Psychol. 2007;32:695–710. doi: 10.1093/jpepsy/jsm023. [DOI] [PubMed] [Google Scholar]
- 15.Hoagwood KE, Kelleher K, Zima BT, Perrin JM, Bilder S, Crystal S. Ten-year trends in treatment services for children with attention deficit hyperactivity disorder enrolled in Medicaid. Health Aff (Millwood) 2016;35:1266–70. doi: 10.1377/hlthaff.2015.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Visser SN, Danielson ML, Wolraich ML, Fox MH, Grosse SD, Valle LA, et al. Vital signs: national and state-specific patterns of attention deficit/hyperactivity disorder treatment among insured children aged 2–5 years - United States, 2008–2014. MMWR Morb Mortal Wkly Rep. 2016;65:443–50. doi: 10.15585/mmwr.mm6517e1. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. National survey of the diagnosis and attention-deficit/hyperactivity disorder and tourette syndrome: frequently asked questions [Internet] Hyattsville (MD): National Center for Health Statistics; 2015. http://www.cdc.gov/nchs/slaits/ns_data.htm. Accessed July 12, 2017. [Google Scholar]
- 18.Visser SN, Zablotsky B, Holbrook JR, Danielson ML, Bitsko RH. Diagnostic experiences of children with attention-deficit/hyperactivity disorder. Natl Health Stat Report. 2015;81 [PubMed] [Google Scholar]
- 19.Embry DD. The good behavior game: a best practice candidate as a universal behavioral vaccine. Clin Child Fam Psychol Rev. 2002;5:273–97. doi: 10.1023/a:1020977107086. [DOI] [PubMed] [Google Scholar]
- 20.Fabiano GA, Pelham WE, Jr, Coles EK, Gnagy EM, Chronis-Tuscano A, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clin Psychol Rev. 2009;29:129–40. doi: 10.1016/j.cpr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Bethell CD, Read D, Brockwood K. Using existing population-based data sets to measure the American Academy of Pediatrics definition of medical home for all children and children with special health care needs. Pediatrics. 2004;113:1529–37. [PubMed] [Google Scholar]
- 22.Policy statement. organizational principles to guide and define the child health care system and/or improve the health of all children. Pediatrics. 2004;113:1545–7. [PubMed] [Google Scholar]
- 23.Morgan PL, Staff J, Hillemeier MM, Farkas G, Maczuga S. Racial and ethnic disparities in ADHD diagnosis from kindergarten to eighth grade. Pediatrics. 2013;132:85–93. doi: 10.1542/peds.2012-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knapp C, Woodworth L, Fernandez-Baca D, Baron-Lee J, Thompson L, Hinojosa M. Factors associated with a patient-centered medical home among children with behavioral health conditions. Matern Child Health J. 2013;17:1658–64. doi: 10.1007/s10995-012-1179-4. [DOI] [PubMed] [Google Scholar]


