Abstract
Objective
Fundamentals of Laparoscopic Surgery (FLS) was developed by the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) to teach the physiology, fundamental knowledge, and technical skills required for basic laparoscopic surgery. We hypothesize that residents are doing more laparoscopic surgery earlier in residency and therefore would benefit from an earlier assessment of basic laparoscopic skills. Here we examine FLS test results and ACGME case logs to determine if it is practical to administer FLS earlier in residency.
Design
FLS test results were reviewed for the 42 residents completing FLS between July 2011 and July 2016. ACGME case logs for current and former residents were reviewed for laparoscopic cases logged by each postgraduate year. Basic and complex laparoscopic cases were determined by ACGME General Surgery Defined Category and Minimums Report. Descriptive statistics were used for analysis.
Setting
Academic general surgery residency, Washington University in St. Louis School of Medicine
Participants
Current and former general surgery residents
Results
42 residents took and passed FLS between July 2011 and July 2016. All residents successfully passed the FLS knowledge and skills examinations on the first attempt regardless of their postgraduate year (PGY 3 n=13, PGY 4 n=15, PGY 5 n=14).
Total laparoscopic case volume has increased over time. Residents who graduated in 2012 or 2013 completed 229 laparoscopic cases compared to 267 laparoscopic cases for those who graduated in 2014-2016 (p=0.02). Additionally, current residents completed more laparoscopic cases in the first two years of residency than residents who graduated from 2012-2016 (median current: 38; former: 22; p<0.001)
Examining laparoscopic case numbers for current residents by PGY demonstrated the number of total and complex laparoscopic cases increased in each of the first three years of residency with the largest increase occurring between the PGY 2 and PGY 3 years. In the PGY 4 and PGY 5 years the majority of laparoscopic cases were complex.
Conclusion
Increased utilization of laparoscopic surgery has led to a corresponding increase in laparoscopic case volume among general surgery residents. We would advocate for FLS testing to serve as an early assessment of laparoscopic knowledge and skill and should be performed prior to a significant increase in complex laparoscopic surgery during training.
Keywords: Fundamentals of laparoscopic surgery, ACGME case log, laparoscopic surgery, general surgery residency
Introduction
Fundamentals of Laparoscopic Surgery (FLS) was developed by the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) to “teach a standard set of cognitive and psychomotor skills to practitioners of laparoscopic surgery.”1 The FLS curriculum was released in 2004 with a corresponding knowledge and technical assessment leading to FLS certification. The importance of standardization in training was identified by the American Board of Surgery (ABS), and in 2008 the ABS made passage of FLS a requirement to achieve certification in general surgery.2
To standardize simulation across residency programs, the American College of Surgeons (ACS) and Association of Program Directors in Surgery (APDS) released a national skills curriculum in 2007 which includes modules for open, laparoscopic, and endoscopic skills. The laparoscopic skills are divided into basic and advanced laparoscopic modules, with the FLS suturing tasks falling in the advanced category.3 Based on these recommendations, most programs have developed laparoscopic curricula for their residency programs, with many utilizing a tiered approach where junior residents, postgraduate year (PGY) 1 and PGY 2, learn basic laparoscopic tasks such as camera driving and hand-eye coordination while senior residents, PGY 3 and above, focus on more complex tasks such as laparoscopic suturing.4
While FLS is required by all residents applying for certification in general surgery, no recommendations exist on the timing of FLS testing during residency. We hypothesize that residents would benefit from an earlier assessment of basic laparoscopic knowledge and skills. Here we examine FLS test results and ACGME case logs from a single institution to determine if it is practical to administer FLS earlier in residency as well as when it is appropriate to perform FLS testing.
Methods
Following IRB approval, we examined the written and practical portions of the FLS test results for our residents between July 2011 and July 2016. This time frame was chosen as it captures the period where our FLS testing was transitioned from a PGY 4 and PGY 5 objective to a PGY 3 objective within our training program.
ACGME case logs were reviewed for current and former residents during the noted time period. Basic and complex laparoscopic case numbers were collected from the ACGME case log system using the General Surgery Defined Category and Minimums Report.
Data was tested for normality using a Pearson test for normality. Unpaired t-tests and one-way analysis of variance (ANOVA) were used to test for differences between two and multiple normally distributed groups, respectively. Wilcoxon-Mann-Whitney tests were used for comparisons between two non-parametric groups, and Kruskal-Wallis tests were used for multiple non-parametric groups. Statistical analysis was performed using GraphPad Prism 7 (La Jolla, CA).
Results
Between July 2011 and July 2016, 42 residents took FLS with a nearly equal distribution of residents among PGY 3, 4, and 5 (PGY 3: 13, PGY 4: 15, PGY 5: 14). All residents took and passed both the written and the practical portions of the FLS test on the first attempt. We examined the total laparoscopic cases performed prior to taking FLS and, as expected, PGY 3 residents had completed significantly fewer laparoscopic cases prior to taking FLS compared to PGY 4 or 5 residents (mean PGY 3: 42 +/- 11, PGY 4: 107 +/- 22, PGY 5: 170 +/- 36; p < 0.0001) (Table 1). However, this did not impact the ability of PGY 3 residents to gain FLS certification.
Table 1. Distribution of residents by PGY and FLS pass rates.
| Postgraduate Year | Number | Male (%) | Passed FLS Written (%) | Passed FLS Practical (%) | Lap cases completed prior to FLS (mean) |
|---|---|---|---|---|---|
| PGY 3 | 13 | 8 (62%) | 13 (100%) | 13 (100%) | 42 |
| PGY 4 | 15 | 9 (60%) | 15 (100%) | 15 (100%) | 107 |
| PGY 5 | 14 | 10 (71%) | 14 (100%) | 14 (100%) | 170 |
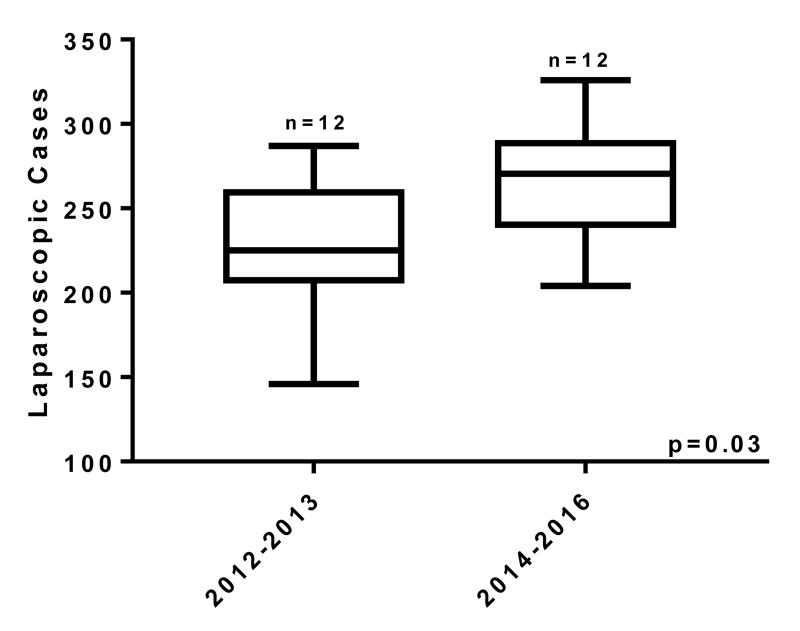
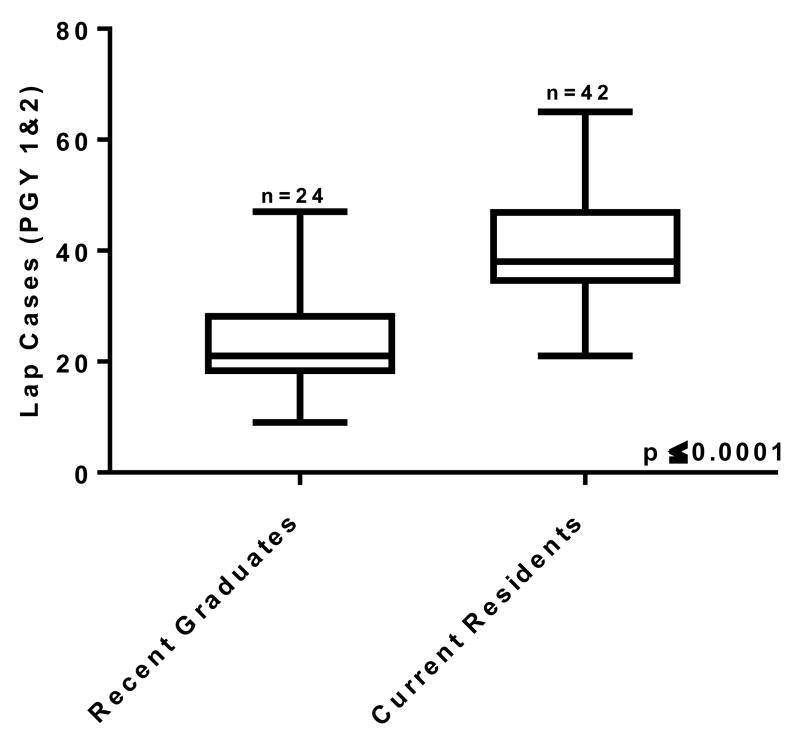
Examining ACGME case logs, residents who graduated in 2012 or 2013 completed an average of 229 laparoscopic cases; this was significantly less than the average of 267 cases for those who graduated in the following three years, from 2014-2016 (p=0.03; Figure 1A). Additionally, we examined the number of laparoscopic cases logged by our current residents during their PGY 1 and PGY 2 years and compared them to the number of laparoscopic cases the recent graduates performed during their first two years of general surgery residency. The current residents completed 38 laparoscopic cases during their first two postgraduate years, while those who completed their training in 2012-2016 had performed 22 laparoscopic cases, which was significantly fewer, over the same time frame (p<0.001; Figure 1B).
Figure 1A.
Comparison of total laparoscopic cases for residents graduating between 2012 and 2013 and those graduating between 2014 and 2016.
Figure 1B.
Number of laparoscopic cases during the PGY 1 and PGY 2 years comparing graduates from 2012 through 2016 versus current residents.
We next examined the laparoscopic case volume for our current residents to determine the appropriate time for FLS testing. We analyzed the case logs by PGY and by complexity of cases based on the ACGME case log report. There was a significant increase in total and complex laparoscopic case volumes in each of the first three years of residency. The most significant increase came between the PGY 2 and PGY 3 years where total laparoscopic cases more than doubled (median PGY 2: 27.5; PGY 3: 59.5; p<0.0001) and complex laparoscopic cases tripled (median PGY 2: 8, PGY 3: 24; p=0.001). Importantly, after the PGY 3 year, the majority of laparoscopic cases performed by residents are complex (Figure 2).
Figure 2.
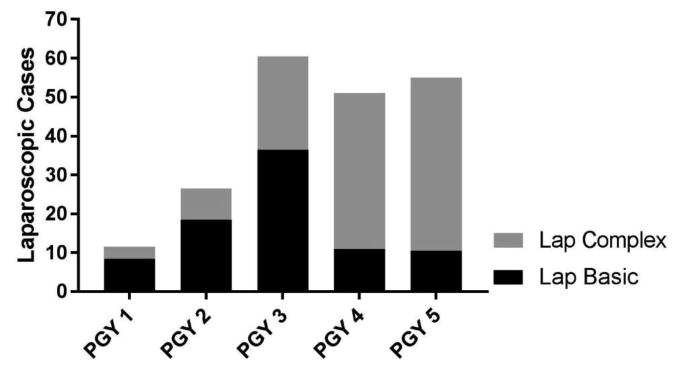
Laparoscopic cases of current residents by PGY divided into basic and complex procedures. Data are expressed as medians.
Discussion
While FLS certification is a requirement of the ABS for certification in general surgery, there is no recommendation on the timing of FLS testing for residents. Analysis of our FLS testing results demonstrated all residents who were PGY 3 and above were able to pass FLS on the first attempt. This is in concordance with the results published by SAGES looking at the early experience of FLS test results across the country, prior to the ABS mandate. Those results demonstrated no statistical difference in the pass rates of residents after PGY 2. However, in that sample, only 12% of test takers were PGY 3 or earlier in their training.5
Since the initiation of FLS in 2004, there has been a significant increase in the utilization of laparoscopic surgery across the field of general surgery. Schlottmann, et al. recently reported a national cohort study evaluating rates of laparoscopic versus open antireflux surgery. In this study, from 2004 to 2005 there was a dramatic increase in the rate of laparoscopic antireflux surgery compared to open.6 A similar increase in laparoscopic treatment of colorectal cancer was seen in 2009 following the Clinical Outcomes in Surgical Therapy (COST) Study Group report which demonstrated that there was no difference in oncologic outcomes for laparoscopic compared to open surgery.7, 8 These trends are mirrored in our data, even only across a five-year period, with more recent graduates performing more laparoscopic surgery than their predecessors and junior residents performing more laparoscopic cases than they have in the past. In response to increased utilization of laparoscopic techniques, the ACGME has increased the laparoscopic case minimums for 2018 graduates. The minimum for basic laparoscopic procedures increases from 60 to 100, and the minimum for complex procedures increases from 25 to 75.9
Finally, this raises the question of the most appropriate timing for FLS testing during residency. We suggest that the use of FLS testing prior to residents performing many complex laparoscopic cases serves as an early assessment of laparoscopic knowledge and skill. Furthermore, establishing the timing of FLS testing earlier in residency may itself serve as a motivation for junior residents to hone their laparoscopic skills and for programs to further formalize their instruction in laparoscopy in the PGY 1 and 2 years of residency. Our case log data revealed a significant increase in total and complex laparoscopic cases between PGY 2 and PGY 3. Additionally, the majority of laparoscopic surgery performed by PGY 4 and PGY 5 residents are complex cases. Based on these results, we have transitioned our FLS testing to the PGY 2 year. During the 2016-2017 academic year, six of eight PGY 2 residents have taken and passed the FLS test on the first attempt; the other two residents have yet to attempt the exam. Taking the exam after the PGY 1 year gives residents one year to gain familiarity with laparoscopy in preparation for the FLS examination.
An important concern with moving FLS testing to earlier in residency is that it has the potential to increase the failure rate and thus increase the cost to programs for retakes. The cost of FLS testing is $595 for ACS or SAGES members and $755 for nonmembers, so even a small increase in the failure rate could have a significant effect on a residency program's budget for FLS. As FLS is designed to focus on basic knowledge and skills largely addressed in the junior curriculum, this failure rate should theoretically be minimally effected. To date, we have not seen this concern born out as moving FLS testing earlier has not resulted in an increase failure rate at our institution.
A limitation of this study is its single institution design with a dependence on accurately entered ACGME case log data. Additionally, our program performs a large amount of complex laparoscopic surgery and may not be representative of all general surgery training programs. However, the trend of increasing and earlier laparoscopic exposure is occurring nationwide and will be soon be mandated by the ACGME.
Conclusion
Increased utilization of laparoscopic surgery has led to a corresponding increase in laparoscopic case volume among general surgery residents. The largest increase in both total volume and complexity in our program comes between PGY 2 and PGY 3, and the majority of laparoscopic surgery performed by PGY 4 and PGY 5 residents are complex cases. We would advocate for FLS testing to serve as an early assessment of laparoscopic knowledge and skill, and it should, therefore, be performed prior to a significant increase in complex laparoscopic surgery.
Highlights.
PGY 3 and above residents all passed FLS on the first attempt
The largest increase in laparoscopic case volume in our program comes between PGY 2 and PGY 3 years
Using FLS as an early assessment of laparoscopic proficiency assures basic laparoscopic safety and skill as case volume and complexity increase
Acknowledgments
Funding: This work was supported by the National Institutes of Health [DRC: T32-CA009621, UL1-TR000448; MRS: T32-HL007776]. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations
- ABS
American Board of Surgery
- ACS
American College of Surgeons
- APDS
Association of Program Directors in Surgery
- ACGME
Accreditation Council for Graduate Medical Education
- ANOVA
Analysis of variance
- FLS
Fundamentals of laparoscopic surgery
- IRB
Institutional review boards
- PGY
Postgraduate year
- SAGES
Society of Gastrointestinal and Endoscopic Surgeons
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Peters JH, Fried GM, Swanstrom LL, et al. Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery. 2004;135:21–27. doi: 10.1016/s0039-6060(03)00156-9. [DOI] [PubMed] [Google Scholar]
- 2.Brunt LM. FLS: Celebrating a decade of innovation in surgical education. Bulletin of the American College of Surgeons. http://bulletin.facs.org/2014/11/fls-celebrating-a-decade-of-innovation-in-surgical-education/2014. [PubMed]
- 3.Scott DJ, Dunnington GL. The new ACS/APDS Skills Curriculum: moving the learning curve out of the operating room. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2008;12:213–221. doi: 10.1007/s11605-007-0357-y. [DOI] [PubMed] [Google Scholar]
- 4.Stefanidis D, Acker CE, Swiderski D, Heniford BT, Greene FL. Challenges during the implementation of a laparoscopic skills curriculum in a busy general surgery residency program. Journal of surgical education. 2008;65:4–7. doi: 10.1016/j.jsurg.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Okrainec A, Soper NJ, Swanstrom LL, Fried GM. Trends and results of the first 5 years of Fundamentals of Laparoscopic Surgery (FLS) certification testing. Surgical endoscopy. 2011;25:1192–1198. doi: 10.1007/s00464-010-1343-0. [DOI] [PubMed] [Google Scholar]
- 6.Schlottmann F, Strassle PD, Patti MG. Comparative Analysis of Perioperative Outcomes and Costs Between Laparoscopic and Open Antireflux Surgery. Journal of the American College of Surgeons. 2017;224:327–333. doi: 10.1016/j.jamcollsurg.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Julien M, Dove J, Quindlen K, et al. Evolution of Laparoscopic Surgery for Colorectal Cancer: The Impact of the Clinical Outcomes of Surgical Therapy Group Trial. The American surgeon. 2016;82:685–691. [PubMed] [Google Scholar]
- 8.Fleshman J, Sargent DJ, Green E, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Annals of surgery. 2007;246:655–662. doi: 10.1097/SLA.0b013e318155a762. discussion 662-654. [DOI] [PubMed] [Google Scholar]
- 9.Defined Category Minimum Numbers: General Surgery Effective for Program Graduates Beginning Academic Year 2017-2018. Review Committee for Surgery, Accreditation Council for Graduate Medical Education (ACGME) 2017 https://www.acgme.org/Portals/0/UPDATED_DEFINED_CATEGORY_MINIMUM_NUMBERS_EFFECTIVE_ACADEMIC_YEAR_2017-2018_GENERAL_SURGERY.pdf.