Abstract
Recently, the focus of funding mechanisms associated with clinical trials has changed to be consistent with an experimental therapeutics approach. While this approach holds considerable promise, the paradigm shift has presented challenges for behavioral trials in complex psychiatric illness such as schizophrenia, as molecular targets – the classic focus in experimental therapeutics paradigms – may not represent logical targets for many psychosocial interventions designed to treat multifaceted, multiply determined symptoms. Clear guidelines for alternate models have not been offered, leaving large numbers of clinical trials researchers unclear about how to frame their work. We address some of the challenges for behavioral interventions research, and offer guidance for the development of novel approaches to the application of a target engagement framework to behavioral clinical trials.
In 2014 the NIMH instituted an experimental therapeutics approach for clinical trials research (Insel and Gogtay, 2014), in which interventions probe disease mechanisms by defining relevant targets, then evaluate efficacy not of the intervention on distal clinical outcomes but of the intervention to engage the identified target. While this approach holds considerable promise, the paradigm shift has presented challenges for behavioral trials, as molecular targets – the classic focus in experimental therapeutics paradigms – may not represent logical targets for many psychosocial interventions. Given this model shift and the considerable unmet clinical need for the development of more robust and effective behavioral treatments for many symptom dimensions (e.g. cognition in psychosis), novel approaches to the identification of actionable targets in behavioral interventions is critical.
Of the more than 250 clinical trials supported by the NIMH in 2012, over half were focused on psychological or psychosocial treatments (https://www.nimh.nih.gov/funding/opportunities-announcements/clinical-trials-foas/changing-nimh-clinical-trials-efficiency-transparency-and-reporting.shtml). Thus, a shift to an experimental therapeutics model affects considerable efforts at treatment development. However, this approach does not map as easily to psychosocial treatments as it does to the development of biologics, as behavioral interventions are rarely thought to act focally at the molecular level and identification of appropriate targets and the measurement of target engagement is thus less straightforward. Indeed, The National Advisory Mental Health Council's Workgroup Report on accelerating discovery of novel interventions in mental health states that, “The workgroup’s…recommendations are intended to be applicable to developing interventions in all modalities, but members recognize that much of the report is in the language of drug development. In that the workgroup heartily endorses the development of better non-pharmacological treatments…it also encourages alternate and efficient models of development appropriate for these domains.” (From Discovery to Cure, 2010, Page i.) Unfortunately, clear guidelines for alternate models have not been offered, leaving large numbers of clinical trials researchers in behavioral science unclear about how to frame their work.
Identifying Targets in Behavioral Interventions
The model for the development of therapeutics used in most other areas of medicine begins with knowledge of molecular pathophysiology, which is used to generate novel targets; screens for small molecules are then developed based on these targets (Insel and Scolnick, 2006). However, such an approach is not necessarily amenable to behavioral target identification. How, then, should we select rational, relevant targets that are a) selectively perturbed by a behavioral intervention, and b) likely to be directly and causally related to both pathophysiology and outcomes?
Toward An Experimental Therapeutics Framework for Behavioral Interventions
If behavioral trials are to keep pace with the evolving focus of clinical trials research, there is an urgent need to develop meaningful methods for the application of a target engagement approach to this work. Several recent reports may provide guidance for moving away from classic outcome studies into an experimental therapeutics framework for behavioral interventions in schizophrenia and other psychiatric illnesses (see Table 1). These studies show that this approach can be used to develop hypothesis-driven bases for target selection and evaluation of target engagement after behavioral intervention, and that paradigms can effectively define targets, interventions, and target engagement in behavioral terms (e.g. Freeman et al., 2015). Additionally, they demonstrate both the promise and the importance of careful definition and conceptual separation of mechanism, target and proximal and distal outcomes.
Table 1.
Experimental Therapeutics Framework for Behavioral Interventions
| Study | Domain of Interest |
Proposed Mechanism |
Target (proximal outcome based on hypothesized mechanism of action) |
Selective Intervention (to engage the target) |
Evidence of Target Engagement |
Distal Outcomes (linking target engagement to clinical outcomes) |
|---|---|---|---|---|---|---|
| Granholm et al., 2009 | Independent living skills in schizophrenia | Social disinterest leads to poor community functioning | Social disinterest attitudes | Cognitive behavioral social skills training (CBSST) | CBSST led to reduced social disinterest attitudes | Reduced social disinterest associated with improved independent living skills |
| Medalia and Choi, 2010 | Engagement in cognitive training in schizophrenia spectrum disorders | Diminished motivation leads to decreased engagement with challenging tasks | Intrinsic motivation | CR plus motivational paradigm vs. CR only | CR + motivation increased intrinsic motivation compared to CR only | Increased intrinsic motivation associated with greater cognitive gains during CR |
| Freeman et al., 2015 | Persecutory delusions in psychosis | Worry thoughts increase persecutory delusions | Worry thoughts | CBT | CBT targeting worry thoughts led to decreased worry | Decreased worry associated with reductions in persecutory delusions |
| Schlosser et al., 2016 | Functional outcomes and quality of life in early course schizophrenia | Reward and motivation impairments associated with poor outcomes in early psychosis | Reward processing and motivation | Mobile interface targeting motivational and reward deficits | Use of mobile device associated with increased motivation and improved reward processing* | Changes in motivation and reward processing lead to improved community functioning and reported quality of life* |
| Zilverstand et al., 2016 | Craving in Addiction | Inhibitory control is associated with affect regulation and craving | Inhibitory control network | CBT or MI | CBT and MI increase recruitment of inhibitory control network | Recruitment of inhibitory control network associated with both affect regulation and control of craving |
| Stange et al., 2017 | Mood and anxiety symptoms in social anxiety or depression | Enhanced attention to aversive stimuli increases mood and anxiety symptoms | ERP-measured index of attention to aversive images | CBT | CBT associated with changes in ERP-measured attention to aversive images | ERP measured attention to aversive images associated with reductions in depression and anxiety |
CR: cognitive remediation; TAU: treatment as usual; CBT: cognitive behavioral therapy; MI: motivational interviewing; ERP: event related potential
Please Note: evidence of target engagement and distal outcomes presented for this study are hypothetical and for illustrative purposes only; actual findings have not yet been reported.
Considerable challenges remain in the identification of actionable targets in behavioral research. First, interventions with multiple components, as is common in behavioral treatments (e.g. CBT involving individual, family, and group components; cognitive remediation targeting multiple cognitive domains) may obscure active treatment ingredients and do not allow for disentangling of treatment effects (Penn et al., 2004). Careful definition and separation of mechanisms, targets, interventions, evidence of target engagement, and links between target engagement and clinical outcomes may actually facilitate this process. Second, because the intervention may be less proximal to the target than is common in biological trials, thoughtful metrics for determining whether or not the intervention “hit the target” are critical to define.
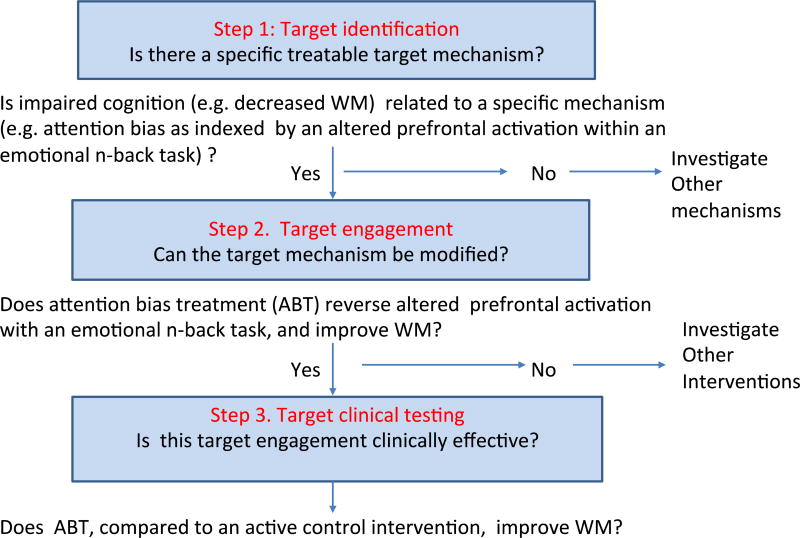
Efforts to disentangle the therapeutic mechanisms of any treatment must consider the heterogeneity of cognitive/ affective processes that may underlie therapeutic change. For example, working memory (WM) impairments in schizophrenia may result from primary deficits in neural processes subserving WM, aberrant effortful neural activation due to cognitive bias toward negative, threatening stimuli, or both (Browning et al., 2010; Eack et al., 2016). Traditional efficacy studies may find treatment effects on WM without being able to determine through which mechanism the treatment acts. It is therefore valuable to identify the target (e.g. attention bias in cognitively impaired patients) and selectively engage this target by an intervention specifically designed to address this deficit. If target engagement is confirmed, the next step would be to move to confirmation of efficacy of the intervention in a controlled clinical trial by linking evidence of target engagement to relevant outcomes. Each of these steps would lead to a go/no go decision such that the investigator can move to testing alternative targets and/or interventions (see Figure 1).
Figure 1.
Experimental therapeutics for developing novel psychological interventions: A hypothetical example
Lastly, an important paradigm shift under this approach is an explicit emphasis on target engagement first, and clinical outcomes that have historically been the primary metrics of efficacy second (e.g. community functioning; psychotic symptoms) and only insofar as they are linked to evidence of target engagement. Decades of efficacy-focused studies have often resulted in a confusing and conflicting body of work on behavioral interventions in psychiatry. For example, studies of CBT for psychosis (CBTp) have shown that most interventions are moderately effective (Wykes et al., 2008), but may not differ in terms of symptom reduction from other psychosocial interventions (Jones et al., 2012). Because the focus of these trials has been on symptom reduction versus mechanisms of action, we are unable to evaluate how each brand of treatment affects symptoms and for whom. That is, CBTp may lead to reduced positive symptoms, but without identifying a specific target and evaluating the links from intervention to target engagement to symptom reduction we may conclude the study with no greater understanding of whether or how any given aspect of CBTp creates change. If target engagement is established first, however, trials are better positioned to empirically test not only whether an intervention “works,” but whether it works through the hypothesized mechanism of action, and – in the inevitable case of heterogeneity of treatment response (here: target engagement) – which factors contribute to this heterogeneity. Elegant follow-up designs then become possible: for example, head to head trials of interventions presumed to act on similar or distinct targets; effects of medication titration in connection with a behavioral intervention targeting the same system; evaluation of additive versus redundant effects of multimodal interventions on key outcomes.
Conclusions
In a recent message, NIMH Director Dr. Joshua Gordon reaffirmed the Institute’s commitment to psychosocial interventions research, and pointed to reworked funding mechanisms aimed at supporting this work, including separating mechanisms testing early stage drug/device interventions from those that test psychosocial interventions, and rewording of the FOAs (Gordon, 2017). However, challenges remain. For many of the complex symptoms of major mental illnesses like schizophrenia such as thought disorder, negative symptoms, and cognitive deficits, adequate treatments are not yet available and are urgently needed. Interestingly, in other fields of medicine efforts to define pathways from disease to treatment to outcome have struggled with an overemphasis on "surrogate endpoints, " risking losing sight of clinical outcomes (Strimbu and Tavel, 2010). The current challenge in behavioral psychiatric intervention studies, conversely, is the identification of biomarkers (or "phenomarkers") first, rather than jumping straight to clinical outcomes without understanding the mechanisms. While there is great promise in this strategy to make faster, broader gains in treatment development and evaluation, we must continue to work to define actionable targets – particularly non-biological targets – and assess target engagement in a way that facilitates rather than hinders development of these key interventions.
Acknowledgments
Funding Body
This work was supported by the National Institute of Mental Health (K.E.L, grant number R21MH110699, and D.O., grant number K24MH104449).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
D.O. served on the Advisory Board for Neurocrine Inc. in 2017. The authors declare that they have no other conflicts of interest in connection with this project.
Contributors
All authors were involved in the development of this project. KEL wrote the first draft of the manuscript and conducted the literature review. MSK drafted portions of the manuscript. all authors contributed to and have approved the final manuscript.
References
- Browning M, Holmes EA, Murphy SE, Goodwin GM, Harmer CJ. Lateral prefrontal cortex mediates the cognitive modification of attentional bias. Biol. Psychiatry. 2010;67(10):919–925. doi: 10.1016/j.biopsych.2009.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Medalia A. Intrinsic motivation and learning in a schizophrenia spectrum sample. Schizophr Res. 2010;118(1–3):12–19. doi: 10.1016/j.schres.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eack SM, Wojtalik JA, Barb SM, Newhill CE, Keshavan MS, Phillips ML. Fronto-Limbic Brain Dysfunction during the Regulation of Emotion in Schizophrenia. PLoS One. 2016;11(3):e0149297. doi: 10.1371/journal.pone.0149297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D, Dunn G, Startup H, Pugh K, Cordwell J, Mander H, Kingdon D. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): a parallel, single-blind, randomised controlled trial with a mediation analysis. Lancet Psychiatry. 2015;2(4):305–313. doi: 10.1016/S2215-0366(15)00039-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon JA. An Experimental therapeutic approach to psychosocial interventions. NIMH Director’s Message, March 20, 2017. 2017 ( www.nimh.nih.gov)
- Granholm E, Ben-Zeev D, Link PC. Social disinterest attitudes and group cognitive-behavioral social skills training for functional disability in schizophrenia. Schizophr. Bull. 2009;35(5):874–883. doi: 10.1093/schbul/sbp072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel TR, Gogtay N. National Institute of Mental Health clinical trials: new opportunities, new expectations. JAMA Psychiatry. 2014;71(7):745–746. doi: 10.1001/jamapsychiatry.2014.426. [DOI] [PubMed] [Google Scholar]
- Insel TR, Scolnick EM. Cure therapeutics and strategic prevention: raising the bar for mental health research. Mol. Psychiatry. 2006;11(1):11–17. doi: 10.1038/sj.mp.4001777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C, Hacker D, Cormac I, Meaden A, Irving CB. Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia. Schizophr. Bull. 2012;38(5):908–910. doi: 10.1093/schbul/sbs090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Advisory Mental Health Council's Workgroup Report. From Discovery to Cure: Accelerating the development of new and personalized interventions for mental illness. 2010. [Google Scholar]
- Penn DL, Mueser KT, Tarrier N, Gloege A, Cather C, Serrano D, Otto MW. Supportive therapy for schizophrenia: possible mechanisms and implications for adjunctive psychosocial treatments. Schizophr. Bull. 2004;30(1):101–112. doi: 10.1093/oxfordjournals.schbul.a007055. [DOI] [PubMed] [Google Scholar]
- Schlosser D, Campellone T, Kim D, Truong B, Vergani S, Ward C, Vinogradov S. Feasibility of PRIME: A cognitive neuroscience-informed mobile app intervention to enhance motivated behavior and improve quality of life in recent onset schizophrenia. JMIR Res. Protoc. 2016;5(2):e77. doi: 10.2196/resprot.5450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stange JP, MacNamara A, Barnas O, Kennedy AE, Hajcak G, Phan KL, Klumpp H. Neural markers of attention to aversive pictures predict response to cognitive behavioral therapy in anxiety and depression. Biol. Psychol. 2017;123:269–277. doi: 10.1016/j.biopsycho.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strimbu K, Tavel JA. What are Biomarkers? Curr. Opin. HIV AIDS. 2010;5(6):463–466. doi: 10.1097/COH.0b013e32833ed177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr. Bull. 2008;34(3):523–537. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilverstand A, Parvaz MA, Moeller SJ, Goldstein RZ. Cognitive interventions for addiction medicine: Understanding the underlying neurobiological mechanisms. Prog. Brain Res. 2016;224:285–304. doi: 10.1016/bs.pbr.2015.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]