Abstract
Aronia melanocarpa has attracted scientific interest due to its dense contents of different polyphenols. We aimed to analyse effects of Aronia melanocarpa (AME) extract on blood pressure (BP), lipid peroxidation, cytokine level, total NOS activity in the left ventricle (LV), and aorta of L-NAME-induced hypertensive rats. 12-week-old male WKY rats were assigned to the control group and groups treated with AME extract (57.90 mg/kg/day), L-NAME (40 mg/kg/day), or combination of L-NAME (40 mg/kg/day) and AME (57.90 mg/kg/day) in tap water for 3 weeks. NOS activity, eNOS protein expression, and conjugated diene (CD) concentration were determined in the LV and aorta. After 3 weeks of L-NAME treatment, BP was increased by 28% and concomitant treatment with AME reduced it by 21%. NOS activity of the LV and aorta in the L-NAME group was decreased by about 40%, while AME increased it almost on the control level. AME-induced eNOS upregulation may contribute to increase NOS activity. Moreover, AME decreased CD concentration in the LV and aorta and TNF-α and IL-6 production in the plasma were increased by L-NAME treatment. In conclusion, our results showed that active substances of Aronia melanocarpa may have a positive effect on blood pressure, NOS activity, and proinflammatory processes in L-NAME-induced hypertension.
1. Introduction
Hypertension is a cardiovascular risk factor associated with endothelial dysfunction and oxidative stress as well. This can lead to a reduction of NO availability and vasodilatation. Those processes participate in increasing systemic blood pressure and myocardial remodelling and in the development of cardiac hypertrophy [1, 2]. Inhibition of nitric oxide synthase by NG-nitro-L-arginine methyl ester (L-NAME) is a well-established rat model of experimental hypertension with increased blood pressure and contractility in different parts of the vasculature, attenuated vascular relaxation, and decreased heart rate [3, 4]. The structural changes after long-term NO synthase inhibition in the cardiovascular system included left ventricle hypertrophy, remodelling of coronary arteries and aorta, as well as extensive areas of fibrosis and necrosis [4–6]. In hypertension, the increased production of oxygen-free radicals is a generally accepted fact. Usually, there is a balance between the antioxidants and the prooxidants in vivo, but several factors like stress, radiation, and nutrition may lead to the so-called oxidative stress, which imposes the necessity to contribute exogenous antioxidants with the diet. The injury caused by oxidative stress can affect all organ systems. Therefore, many studies are oriented on antioxidant treatment that may prevent the hypertension and associated organ alterations.
Increasing consumption of polyphenol-rich foods is a promising strategy to reduce cardiovascular risk. Increased flavonoid consumption correlated with positive effect on low-density lipoproteins, blood pressure, and flow-mediated dilation [7]. Polyphenols with numerous biological activities are used for their ability to act as an antioxidant either by scavenging reactive oxygen species (ROS) or inhibiting enzymes involved in the ROS production [1, 8, 9].
Aronia melanocarpa, also known as black chokeberry, belongs to the Rosaceae family, originally coming from North America. Nowadays, it is commonly used also in Europe due to a high content of nutrients being beneficial for the health. The components of the aronia are dependent on many factors such as cultivar, fertilization, maturation of the berries, harvest date, or habitat/location [10, 11]. The most abundant components are anthocyanins and flavonoids [12]. Chokeberries with high resistance to frost and mechanized harvesting are widely used in processed and derived products including juices, wines, jellies, and tea [13, 14]. The protective role of the main components from aronia against cardiovascular diseases came up from clinical trials [15, 16] and animal studies [17–19]. Attention has been also focused on chokeberries due to their antioxidant properties related to the high polyphenolic content [20, 21].
The aim of our study was to determine the effect of nonalcohol Aronia melanocarpa extract on NO synthase activity, particularly NO synthase isoform protein expressions in the aorta and left ventricle, as well as their immunohistochemistry and on cytokine and conjugated diene levels on L-NAME-induced experimental model of arterial hypertension.
2. Materials and Methods
2.1. Chemicals
Most of the chemicals and reagents were obtained from Sigma-Aldrich; when not, the company is indicated.
2.2. Aronia melanocarpa Extract
Samples of Aronia melanocarpa wine (Winery Pereg Ltd.) were subjected to the process of dealcoholisation and concentration, producing an alcohol-free Aronia melanocarpa extract (AME) (previously described by Kondrashov [22]). The total phenolic content of AME was assessed according to the Folin-Ciocalteu method. Briefly, 1 mL of AME, 1 mL of Folin-Ciocalteu's reagent, and 5 mL of distilled water were mixed together. The solution was incubated for 5 min at a room temperature in the darkness. Then, 1 mL of 20% Na2CO3 was added. The solution was made up to 10 mL, mixed, and incubated for 1 h at a room temperature in the darkness. The absorbance of AME sample was measured at 765 nm against a blank (corresponding extraction mixture was used instead of algal extract) on UV/VIS spectrometer Lambda 25 (PerkinElmer, Waltham, MA, USA). Gallic acid was used as a standard to construct the calibration curve (20, 40, 60, 80, and 100 mg·L−1). The total phenolic content of AME is expressed in mg·g−1 of gallic acid equivalent (GAE).
2.3. Animal Study
2.3.1. Animals and Treatment
All procedures and experimental protocols were approved by the Ethical Committee of the Institute of Normal and Pathological Physiology SAS and conform to the European Convention on Animal Protection and Guidelines on Research Animal Use.
12-week-old male Wistar Kyoto rats were divided into the control group, the group treated with AME in the dose 57.90 mg/kg/day, the group treated with NG-nitro-L-arginine methyl ester (L-NAME) in the dose 40 mg/kg/day, and the group treated with L-NAME in the dose 40 mg/kg/day + AME 57.90 mg/kg/day. Each group obtained 6 animals. L-NAME and AME were administered via the drinking water from the 12th week of age for 3 weeks. Daily water consumption was estimated individually for every animal and adjusted, if necessary. All animals were housed at a temperature of 22–24°C and fed with a regular pellet diet ad libitum. Blood pressure (BP) was measured noninvasively, using tail-cuff plethysmography weekly. At the end of treatment, the animals were sacrificed; body weight (BW) and heart weight (HW) were determined. The HW/BW ratio was calculated. Samples of the left ventricle and aorta were used to determine NO synthase activity, eNOS and iNOS protein expressions (Western blot and immunohistochemistry), and conjugated diene level. Cytokine levels were measured in the plasma.
2.3.2. Total NOS Activity and Protein Expression
Total NO synthase activity was determined in crude homogenates of the left ventricle and aorta by measuring the formation of [3H]-L-citrulline from [3H]-L-arginine (ARC, Montana, USA) as previously described and slightly modified by Pechanova [23]. [3H]-L-citrulline was measured with the Quanta Smart TriCarb Liquid Scintillation Analyzer (Packard Instrument Company, Meriden, CT).
Protein expressions of eNOS and iNOS were determined in the aorta and left ventricle by Western blot analysis. The samples were probed with polyclonal rabbit, anti-eNOS, anti-iNOS, and anti-GAPDH antibodies (Abcam, Cambridge, UK). The intensity of bands was visualized using the enhanced chemiluminescence system (ECL, Amersham, UK), quantified by using ChemiDoc™ Touch Imagine System (Image Lab™ Touch software, Bio-Rad), and normalized to GAPDH bands.
2.3.3. Cytokine Level and CD Determination
Cytokine levels were determined by Bio-Plex Pro™ rat cytokine, chemokine, and growth factor assays in plasma.
The concentration of conjugated dienes (CD) was measured in lipid extracts of the left ventricle homogenates [24]. After chloroform evaporation under inert atmosphere and addition of cyclohexane, conjugated diene concentrations were determined spectrophotometrically (λ = 233 nm, GBC 911A, Bio-Rad Laboratories).
2.3.4. Immunohistochemical Analysis of eNOS and iNOS in LV
The tissue samples were processed in a standard manner, embedded in paraffin, and sectioned; 3 μm thick slices were deparaffinized and rehydrated in phosphate-buffered physiological saline solution (10 mM, pH 7.2). The tissue epitopes were damasked using the automated water bath heating process in Dako PT Link (Agilent, Santa Clara, California); the slides were incubated in citrate retrieval solution (10 mM citrate, pH 6.0) at 98°C for 20 minutes. The slides were subsequently incubated 2 hours at room temperature with the primary mouse monoclonal IgG2a antibody against eNOS or iNOS (Santa Cruz Biotechnology, Dallas, USA, sc-376751) diluted 1 : 100. The samples were immunostained using anti-mouse anti-rabbit immune-peroxidase polymer (Histofine, Nichirei Biosciences, Tokyo, Japan) for 30 minutes at a room temperature according to the manufacturer's instructions. For visualization, the diaminobenzidine substrate-chromogen solution was used (DAB, Agilent, Santa Clara, California) for 5 minutes. The slides were counterstained with hematoxylin. The DAB positivity was evaluated by light microscopy and measured by histomorphometry using the Fiji morphometric software [25] based on ImageJ 1.51n platform [26]. The final results are expressed as proportional ratio comparing to the mean DAB positivity of evaluated marker in WKY controls (expressed as 1.00).
2.4. Statistics
The results are expressed as mean ± SEM. One-way analysis of variance and Duncan test were used for statistical analysis. Values were considered significant with a probability value p < 0.05.
3. Results
3.1. AME Content
The total content of nonalcohol extract of Aronia melanocarpa is shown in Table 1. The total phenolic content adjusted on gallic acid equivalent was 57,870 mg/L.
Table 1.
Components of Aronia melanocarpa extract (in μg/g).
| Component | (μg·g−1) |
|---|---|
| Gallic acid | 2.24 ± 0.01 |
| Protocatechuic acid | 340.86 ± 7.70 |
| 4-Hydroxybenzoic acid | 21.44 ± 0.31 |
| Epigallocatechin | 354.81 ± 11.19 |
| Catechin | 149.68 ± 1.91 |
| Chlorogenic acid | 1948.60 ± 0.59 |
| Vanillic acid | 14.61 ± 0.11 |
| Caffeic acid | 4.78 ± 0.09 |
| Syringic acid | 4.32 ± 0.29 |
| Epicatechin | 29.24 ± 0.52 |
| Trans-p-coum acid | 19.37 ± 1.32 |
| Ferulic acid | 173.90 ± 1.94 |
| Ellagic acid | 42.78 ± 0.14 |
| Rutin | 17.44 ± 0.00 |
| T-2-hydroxycinnamic acid | 1.18 ± 0.12 |
| Protocatechuic acid etylester | 11.55 ± 0.39 |
| Resveratrol | 16.65 ± 0.32 |
| Cinnamic acid | 2.35 ± 0.00 |
| Kaempferol | 23.09 ± 0.79 |
| Quercetin | 0.00 ± 0.00 |
Data are expressed as mean values (n = 3) ±SD.
The most predominant mineral elements detected in AME were ferrum (Fe), zinc (Zn), and cuprum (Cu). The results are visualized in Table 2.
Table 2.
Elemental profile of Aronia melanocarpa extract (in ng/mL).
| Sample | K | Mg | P | Fe | Cu | Pb | Zn | Na |
|---|---|---|---|---|---|---|---|---|
| AME | 12.12 ± 0.09 | 85.41 ± 0.82 | 14.47 ± 0.12 | 1960.71 ± 11.05 | 405.14 ± 2.87 | 28.62 ± 2.15 | 950.34 ± 4.35 | 12.19 ± 0.13 |
Data are expressed as mean values (n = 3) ± SD.
3.2. Animal Studies
3.2.1. Cardiovascular Parameters and Plasma Cytokine Level
After three weeks of L-NAME treatment, BP was increased by 28% in comparison to the control group. Concomitant treatment by AME reduced BP by 21% (Table 3). At the end of the experiment, HW/BW ratio (mg/g) was 2.72 ± 0.05 in the control group. This ratio was increased in L-NAME group (2.95 ± 0.10) versus control rats. AME was able to decrease this value on the control level (2.77 ± 0.02) (Table 3).
Table 3.
Blood pressure (BP), relative heart weight (HW/BW), TNFα (pg/mL), and IL-6 level (pg/mL) of Wistar Kyoto rats treated with AME (57.90 mg/kg/day), with L-NAME (40 mg/kg/day), and with L-NAME (40 mg/kg/day) + AME (57.90 mg/kg/day) for 3 weeks and age-matched controls.
| Group | BP (mmHg) | Hw/Bw (mg/g) | TNFα (pg/mL) | IL-6 (pg/mL) |
|---|---|---|---|---|
| WKY | 118.39 ± 4.29 | 2.72 ± 0.05 | 12.11 ± 2.41 | 23.41 ± 3.78 |
| WKY + AME | 122.04 ± 1.81 | 2.55 ± 0.05 | 7.32 ± 2.12 | 22.14 ± 5.22 |
| WKY + L-NAME | 155.11 ± 3.71∗ | 2.95 ± 0.10∗ | 18.19 ± 1.38∗ | 36.43 ± 3.08∗ |
| WKY + L-NAME + AME | 129.22 ± 2.51 | 2.77 ± 0.02# | 13.89 ± 1.29# | 25.13 ± 2.11# |
Data are means ± SEM, significant differences: ∗P < 0.05 compared to age-matched controls; #P < 0.05 compared to L-NAME group.
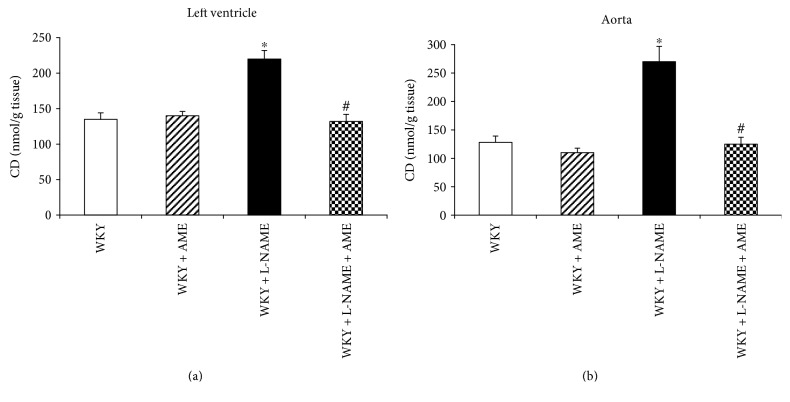
3.2.2. Cytokine and CD Concentration
AME was able to inhibit TNFα, and IL-6 production increased in the L-NAME group (Table 3). L-NAME administration increased the level of CD in both investigated tissues. Furthermore, AME was able to decrease the level of CD almost on the level of controls (Figures 1(a) and 1(b)).
Figure 1.
Conjugate diene (CD) level of the left ventricle (a) and aorta (b) of Wistar Kyoto rats treated with AME (57.90 mg/kg/day), with L-NAME (40 mg/kg/day), and with L-NAME (40 mg/kg/day) + AME (57.90 mg/kg/day) for 3 weeks and age-matched controls. Data are means ± SEM, significant differences: ∗P < 0.05 compared to age-matched controls; #P < 0.05 compared to L-NAME group.
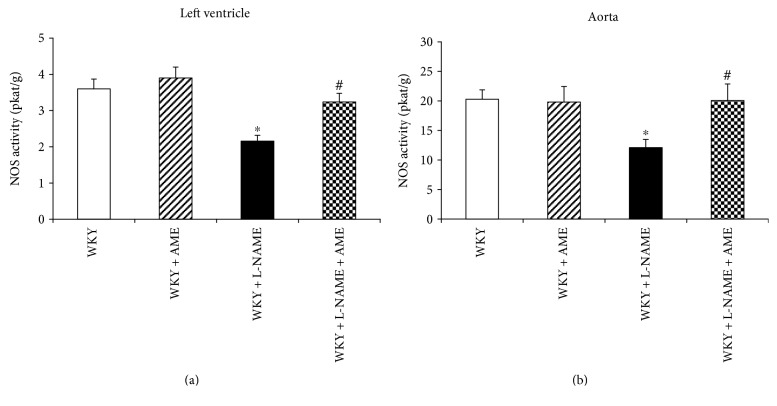
3.2.3. Total NO Synthase Activity and Protein Expression
The total NO synthase activity was decreased after 3 weeks of L-NAME treatment in both the left ventricle and aorta. However, AME was able to increase NO synthase activity in the left ventricle on 90% of the control value (Figure 2(a)) and on control value in the aorta (Figure 2(b)).
Figure 2.
Nitric oxide synthase (NOS) activity of the left ventricle (a) and aorta (b) of Wistar Kyoto rats treated with AME (57.90 mg/kg/day), with L-NAME (40 mg/kg/day), and with L-NAME (40 mg/kg/day) + AME (57.90 mg/kg/day) for 3 weeks and age-matched controls. Data are means ± SEM, significant differences: ∗P < 0.05 compared to age-matched controls; #P < 0.05 compared to L-NAME group.
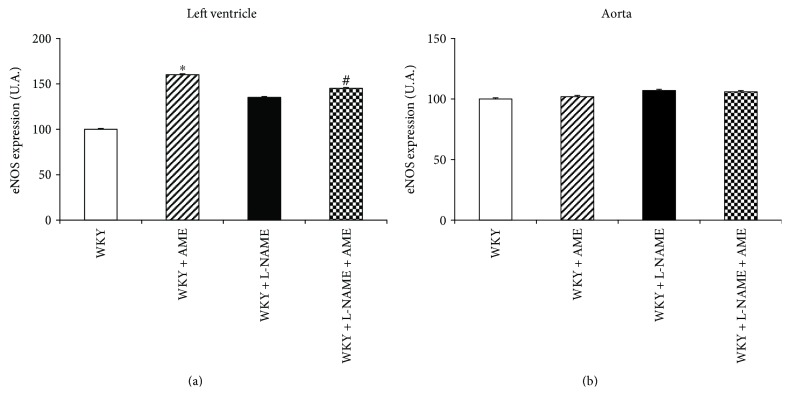
Endothelial NOS protein expression was upregulated only in LV of AME group (Figure 3). The L-NAME administration alone and concomitant treatment with AME had the tendency to increase eNOS expression as well. We did not observe any changes of eNOS expression in the aorta.
Figure 3.
Endothelial NOS (eNOS) expression of the left ventricle (a) and aorta (b) of Wistar Kyoto rats treated with AME (57.90 mg/kg/day), with L-NAME (40 mg/kg/day), and with L-NAME (40 mg/kg/day) + AME (57.90 mg/kg/day) for 3 weeks and age-matched controls. Data are means ± SEM, significant differences: ∗P < 0.05 compared to age-matched controls; #P < 0.05 compared to L-NAME group.
Inducible NOS protein expression was not changed in any investigated tissue and group (data are not shown).
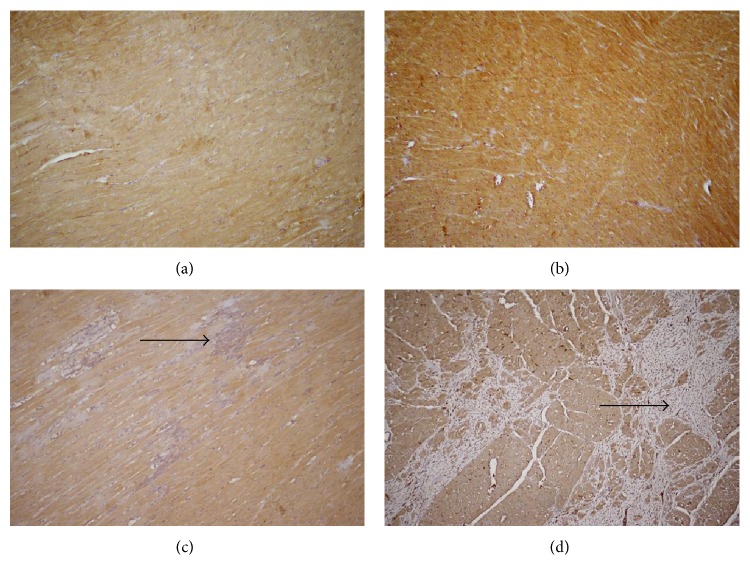
3.2.4. Immunohistochemical Analysis of eNOS and iNOS in LV
The eNOS showed diffuse and regular cytoplasmic positivity in cardiomyocytes of all experimental animals. Only the AME treatment without the L-NAME administration significantly increased the eNOS expression (Figures 4(a)–4(d)). Positivity of eNOS is well correlated with its protein expression analysed by Western blot. Similarly, as Western blot, immunohistochemistry did not show any changes in iNOS protein expression between the groups (data are not shown).
Figure 4.
eNOS expression in heart tissue. Diffuse cytoplasmic positivity of eNOS was found in all samples. Only the AME treatment without the L-NAME administration significantly increased the eNOS expression. (a) WKY, (b) AME, (c) L-NAME, (d) L-NAME + AME, eNOS, Ab-Poly, DAB, 200x.
4. Discussion
Long-lasting inhibition of NO synthase induces hypertension, endothelial and contractile dysfunction, inflammation, and fibrosis enlargement [27]. Chronic inhibition of NO synthase by L-NAME causes increase of blood pressure associated with vascular structural changes [4, 28]. It has been also shown that L-NAME increased fibrosis and left ventricular hypertrophy [3, 29]. Thus, L-NAME-induced hypertension represents a useful tool for studying increase of blood pressure associated with inflammatory processes and fibrosis. Lowering blood pressure is one of the most important means to reduce cardiovascular morbidity and mortality. Our study showed that Aronia melanocarpa extract resulted in significant reduction of blood pressure in L-NAME-treated rats that may be due to high polyphenolic content. In our previous study, we have shown that polyphenols can act as antioxidants, due to their functional groups and aromatic structure [30]. Our finding is in agreement with Ciocoiu [31] in experimental hypertension in rats. They found reduction of systolic and diastolic pressures after treatment with Aronia melanocarpa extract. Other authors showed decreased blood pressure in SHR after the commercial Aronia melanocarpa extract Aronox treatment [32]. The hypotensive effect was revealed also by Naruszewicz [33] in patients after myocardial infarction with statin therapy and by Tjelle [34] in hypertensive volunteers.
Several studies showed that hypertension may lead to overproduction of free radicals, which could be the reason of biochemical, molecular, and behavioural changes [35, 36]. In this study, concentration of conjugated dienes (CD) was determined as a marker of oxidative damage and lipid peroxidation. Our previous results observed increased production of free radicals in the L-NAME model of hypertension [37]. We confirmed increased concentration of CD in the aorta and left ventricle after L-NAME treatment. AME extract was able to decrease the CD on the control level. Similarly, improved plasma and hepatic antioxidant function were found in apo E−/− mice after chokeberry extract treatment [38]. In the same pattern, IL-6 and TNF- α levels were decreased in the hypertensive group treated with AME. Han and Nicholson [39] showed significant drop of IL-6 as well as reduction in the level of oxidative stress in cardiac patients after chokeberry treatment. Nowadays, chokeberry consumption is in good relation with human immune system. Mechanisms of action are mediated by inhibition of cytokine IL-6, IL-8, and TNF-α in human monocytes as well as by activation of NFκB and prostaglandin E2 [40].
The antioxidant activity of Aronia melanocarpa is mostly contributed by the phenolic compounds [40] and depends on the structure of polyphenol functional groups [41]. It is also known from the literature that an increased level of free radicals leads to uncoupling of the NOS dimer to a monomer form, and an activity of this enzyme as well as production of NO is decreased. Moreover, under conditions of oxidative stress, NO synthase synthesizes rather superoxide radical than NO [37, 42]. This, besides direct L-NAME inhibition, may be one of the reasons of decreased NO synthase activity in our experiment. AME treatment in our experiment directly increased NO synthase activity probably by both decreasing oxidative stress by polyphenolic group function and stabilizing NO synthase dimer by addition of Zn.
This study provides also the evidence that active compounds of AME are likely to stimulate the expression of eNOS in myocardium; however, in combination with L- NAME, this stimulation is not significant. Those results are in good agreement with Wallerath [43] who found increased eNOS expression in humans after polyphenol treatment. The positive effect on endothelial formation of NO in coronary arteries was observed also by Kim [38]. Authors showed that phosphorylation of eNOS via redox-sensitive activation of Src/PI3/Akt pathway is mostly by conjugated cyanidins and chlorogenic acids, which are also the most, represented content of our extract.
5. Conclusions
In conclusion, AME treatment was able to reduce blood pressure in L-NAME-induced hypertension by decreasing oxidative stress and increasing NO production. Both direct contribution of polyphenolic groups and Zn addition may be responsible for NO synthase upregulation in LV. Moreover, in the same tissue, AME alone was able to increase eNOS protein expression and had a tendency to increase it during the concomitant treatment with L-NAME which may further contribute to NO synthase activity increase.
Acknowledgments
The study was supported by Scientific Grant Agency VEGA (nos. 2/0170/17 and 2/0165/15) and Slovak Research and Development Agency APVV (no. APVV-14-0932).
Disclosure
An earlier version of this work was presented before at the “25th Anniversary of the FEPS, 168th Anniversary of French Physiological Society, 2016,” and published as an abstract in the “Acta Phyiologica” Official Journal of the Federation of European Physiological Societies in 2016.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Pechanova O., Varga Z. V., Cebova M., Giricz Z., Pacher P., Ferdinandy P. Cardiac NO signalling in the metabolic syndrome. British Journal of Pharmacology. 2015;172(6):1415–1433. doi: 10.1111/bph.12960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez-Porcel M., Zhu X. Y., Chade A. R., et al. Functional and structural remodeling of the myocardial microvasculature in early experimental hypertension. American Journal of Physiology: Heart and Circulatory Physiology. 2006;290(3):H978–H984. doi: 10.1152/ajpheart.00538.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babal P., Pechanova O., Bernatova I. Long-term administration of D-NAME induces hemodynamic and structural changes in the cardiovascular system. Physiological Research. 2000;49(1):47–54. [PubMed] [Google Scholar]
- 4.Kristek F., Cebova M. Experimental Hypertension and Ischemic Heart Diseases. Bratislava: Publishing House of the Slovak Academy of Sciences; 2005. Long-term effect of exogenous NO donors on geometry of conduit arteries in NO-deficient and spontaneously hypertensive rats; pp. 175–191. [Google Scholar]
- 5.Kristek F., Gerova M. Long-term NO synthase inhibition affects heart weight and geometry of coronary and carotid arteries. Physiological Research. 1996;45(5):361–367. [PubMed] [Google Scholar]
- 6.Babal P., Pechanova O., Bernatova I., Stvrtina S. Chronic inhibition of NO synthesis produces myocardial fibrosis and arterial media hyperplasia. Histology and Histopathology. 1997;12(3):623–629. [PubMed] [Google Scholar]
- 7.Hooper L., Kroon P. A., Rimm E. B., et al. Flavonoids, flavonoid-rich foods, and cardiovascular risk: a meta-analysis of randomized controlled trials. The American Journal of Clinical Nutrition. 2008;88(1):38–50. doi: 10.1093/ajcn/88.1.38. [DOI] [PubMed] [Google Scholar]
- 8.Agouni A., Mostefai H. A., Lagrue A. H., et al. Paradoxical effect of nonalcoholic red wine polyphenol extract, Provinols™, in the regulation of cyclooxygenases in vessels from Zucker fatty rats (fa/fa) Oxidative Medicine and Cellular Longevity. 2017;2017:12. doi: 10.1155/2017/8536910.8536910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ross J. A., Kasum C. M. Dietary flavonoids: bioavailability, metabolic effects, and safety. Annual Review of Nutrition. 2002;22(1):19–34. doi: 10.1146/annurev.nutr.22.111401.144957. [DOI] [PubMed] [Google Scholar]
- 10.Jeppsson N., Johansson R. Changes in fruit quality in black chokeberry (Aronia melanocarpa) during maturation. The Journal of Horticultural Science and Biotechnology. 2000;75(3):340–345. doi: 10.1080/14620316.2000.11511247. [DOI] [Google Scholar]
- 11.Skupien K., Oszmianski J. The effect of mineral fertilization on nutritive value and biological activity of chokeberry fruit. Agricultural and Food Science. 2007;16:46–55. doi: 10.2137/145960607781635822. [DOI] [Google Scholar]
- 12.Kulling S. E., Rawel H. M. Chokeberry (Aronia melanocarpa) – a review on the characteristic components and potential health effects. Planta Medica. 2008;74(13):1625–1634. doi: 10.1055/s-0028-1088306. [DOI] [PubMed] [Google Scholar]
- 13.Ochmian I., Grajkowski J., Smolik M. Comparison of some morphological features, quality and chemical content of four cultivars of chokeberry fruits (Aronia melanocarpa) Notulae Botanicae Horti Agrobotanici Cluj-Napoca. 2012;40:253–260. [Google Scholar]
- 14.Wilkes K., Howard L. R., Brownmiller C., Prior R. L. Changes in chokeberry (Aronia melanocarpa L.) polyphenols during juice processing and storage. Journal of Agricultural and Food Chemistry. 2014;62(18):4018–4025. doi: 10.1021/jf404281n. [DOI] [PubMed] [Google Scholar]
- 15.Broncel M., Kozirog M., Duchnowicz P., Koter-Michalak M., Sikora J., Chojnowska-Jezierska J. Aronia melanocarpa extract reduces blood pressure, serum endothelin, lipid, and oxidative stress marker levels in patients with metabolic syndrome. Medical Science Monitor. 2010;16(1):CR28–CR34. [PubMed] [Google Scholar]
- 16.Pascual-Teresa S., Sanchez-Ballesta M. T. Anthocyanins: from plant to health. Phytochemistry Reviews. 2008;7(2):281–299. doi: 10.1007/s11101-007-9074-0. [DOI] [Google Scholar]
- 17.Valcheva-Kuzmanova S., Kuzmanov K., Tancheva S., Belcheva A. Hypoglycemic effects of Aronia melanocarpa fruit juice in streptozotocin-induced diabetic rats. Methods and Findings in Experimental and Clinical Pharmacology. 2007;29(2):101–105. doi: 10.1358/mf.2007.29.2.1075349. [DOI] [PubMed] [Google Scholar]
- 18.Mennen L. I., Sapinho D., de Bree A., et al. Consumption of foods rich in flavonoids is related to a decreased cardiovascular risk in apparently healthy French women. The Journal of Nutrition. 2004;134(4):923–926. doi: 10.1093/jn/134.4.923. [DOI] [PubMed] [Google Scholar]
- 19.Cebova M., Barta A., Matuskova Z., Rehakova R., Kosutova M., Pechanova O. The effect of bioactive compound of Aronia melanocarpa on cardiovascular system in experimental hypertension. Acta Physiologica. 2016;217(Supplement 708):p. 49. [Google Scholar]
- 20.Bolling B. W., Taheri R., Pei R., et al. Harvest date affects aronia juice polyphenols, sugars, and antioxidant activity, but not anthocyanin stability. Food Chemistry. 2015;187:189–196. doi: 10.1016/j.foodchem.2015.04.106. [DOI] [PubMed] [Google Scholar]
- 21.Jurikova T., Mlcek J., Skrovankova S., et al. Fruits of black chokeberry Aronia melanocarpa in the prevention of chronic diseases. Molecules. 2017;22(6):p. 944. doi: 10.3390/molecules22060944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kondrashov A., Vrankova S., Dovinova I., et al. The effects of new Alibernet red wine extract on nitric oxide and reactive oxygen species production in spontaneously hypertensive rats. Oxidative Medicine and Cellular Longevity. 2012;2012:8. doi: 10.1155/2012/806285.806285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pechanova O., Bernatova I., Pelouch V., Simko F. Protein remodelling of the heart in NO-deficient hypertension: the effect of captopril. Journal of Molecular and Cellular Cardiology. 1997;29(12):3365–3374. doi: 10.1006/jmcc.1997.0566. [DOI] [PubMed] [Google Scholar]
- 24.Kogure K., Watson B. D., Busto R., Abe K. Potentiation of lipid peroxides by ischemia in rat brain. Neurochemical Research. 1982;7(4):437–454. doi: 10.1007/BF00965496. [DOI] [PubMed] [Google Scholar]
- 25.Schindelin J., Arganda-Carreras I., Frise E., et al. Fiji: an open-source platform for biological-image analysis. Nature Methods. 2012;9(7):676–682. doi: 10.1038/nmeth.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abramoff M. D., Magelhaes P. J., Ram S. J. Image processing with ImageJ. Biophotonics International. 2004;11(7):36–42. [Google Scholar]
- 27.Moncada S., Palmer R. M., Higgs E. A. Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacological Reviews. 1991;43(2):109–142. [PubMed] [Google Scholar]
- 28.Pechánová O., Bernátová I. Effect of long-term NO synthase inhibition on cyclic nucleotide content in rat tissues. Physiological Research. 1996;45(4):305–309. [PubMed] [Google Scholar]
- 29.Michalska A., Schechter A. N. Dietary nitrite and nitrate: a review of potential mechanisms of cardiovascular benefits. European Journal of Nutrition. 2011;50:293–303. doi: 10.1007/s00394-011-0192-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pechánová O., Rezzani R., Babál P., Bernátová I., Andriantsitohaina R. Beneficial effects of Provinols™: cardiovascular system and kidney. Physiological Research. 2006;55(Supplement 1):S17–S30. doi: 10.33549/physiolres.930000.55.S1.17. [DOI] [PubMed] [Google Scholar]
- 31.Ciocoiu M., Badescu M., Badulescu O., Tutunaru D., Badescu L. Polyphenolic extract association with renin inhibitors in experimental arterial hypertension. Journal of Biomedical Science and Engineering. 2013;6(4):5. doi: 10.4236/jbise.2013.64062.30525 [DOI] [Google Scholar]
- 32.Hellstrom J. K., Shikov A. N., Makarova M. N., et al. Blood pressure-lowering properties of chokeberry (Aronia mitchurinii, var. Viking) Journal of Functional Food. 2010;2(2):163–169. doi: 10.1016/j.jff.2010.04.004. [DOI] [Google Scholar]
- 33.Naruszewicz M., Laniewska I., Millo B., Dłuzniewski M. Combination therapy of statin with flavonoids rich extract from chokeberry fruits enhanced reduction in cardiovascular risk markers in patients after myocardial infraction (MI) Atherosclerosis. 2007;194(2):e179–e184. doi: 10.1016/j.atherosclerosis.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 34.Tjelle T. E., Holtung L., Bøhn S. K., et al. Polyphenol-rich juices reduce blood pressure measures in a randomised controlled trial in high normal and hypertensive volunteers. The British Journal of Nutrition. 2015;114(07):1054–1063. doi: 10.1017/S0007114515000562. [DOI] [PubMed] [Google Scholar]
- 35.Berg D., Youdim M. B., Riederer P. Redox imbalance. Cell and Tissue Research. 2004;318(1):201–213. doi: 10.1007/s00441-004-0976-5. [DOI] [PubMed] [Google Scholar]
- 36.Kohen R., Nyska A. Oxidation of biological systems: oxidative stress phenomena, antioxidants, redox reactions, and methods for their quantification. Toxicologic Pathology. 2002;30(6):620–650. doi: 10.1080/01926230290166724. [DOI] [PubMed] [Google Scholar]
- 37.Pechanova O., Matuskova J., Capikova D., Jendekova L., Paulis L., Simko F. Effect of spironolactone and captopril on nitric oxide and S-nitrosothiol formation in kidney of L-NAME-treated rats. Kidney International. 2006;70(1):170–176. doi: 10.1038/sj.ki.5001513. [DOI] [PubMed] [Google Scholar]
- 38.Kim J. H., Auger C., Kurita I., et al. Aronia melanocarpa juice, a rich source of polyphenols, induces endothelium-dependent relaxations in porcine coronary arteries via the redox-sensitive activation of endothelial nitric oxide synthase. Nitric Oxide. 2013;35:54–64. doi: 10.1016/j.niox.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 39.Han J., Nicholson A. C. Lipoproteins modulate expression of the macrophage scavenger receptor. The American Journal of Pathology. 1998;152(6):1647–1654. [PMC free article] [PubMed] [Google Scholar]
- 40.Appel K., Meiser P., Millán E., et al. Chokeberry (Aronia melanocarpa (Michx.) Elliot) concentrate inhibits NF-κB and synergizes with selenium to inhibit the release of pro-inflammatory mediators in macrophages. Fitoterapia. 2015;105:73–82. doi: 10.1016/j.fitote.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 41.Hussain T., Tan B., Yin Y., Blachier F., Tossou M. C., Rahu N. Oxidative stress and inflammation: what polyphenols can do for us? Oxidative Medicine and Cellular Longevity. 2016;2016:9. doi: 10.1155/2016/7432797.7432797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Landmesser U., Dikalov S., Price S. R., et al. Oxidation of tetrahydrobiopterin leads to uncoupling of endothelial cell nitric oxide synthase in hypertension. The Journal of Clinical Investigation. 2003;111(8):1201–1209. doi: 10.1172/JCI200314172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wallerath T., Poleo D., Li H., Förstermann U. Red wine increases the expression of human endothelial nitric oxide synthase: a mechanism that may contribute to its beneficial cardiovascular effects. Journal of the American College of Cardiology. 2003;41(3):471–478. doi: 10.1016/S0735-1097(02)02826-7. [DOI] [PubMed] [Google Scholar]