Abstract
Purpose
To determine visual acuity and rates of post-operative cystoid macular oedema (CMO) in an ethnically diverse and predominantly diabetic population.
Methods
The study was undertaken over a one year period. Snellen visual acuity (VA) was measured pre and 4–8 weeks post-operatively and optical coherence topography (OCT) was performed at baseline and post-operatively. No eyes received prophylactic non-steroidal anti-inflammatory drugs (NSAIDs) prior to or after surgery.
Results
Out of 262 eyes, 59% were in the Black, Asian and minority ethnic group (BAME), 57% had a history of diabetes mellitus and 34% had pre-existing diabetic retinopathy. 76% of all eyes achieved 6/12 post-operative VA at the first postoperative review and the incidence of post-operative CMO within the study population was 7.6%. In patients with a history of diabetes mellitus the incidence of post-operative CMO was 10.7% compared to 3.5% in those without diabetes. This was found to be clinically significant (P=0.0297).
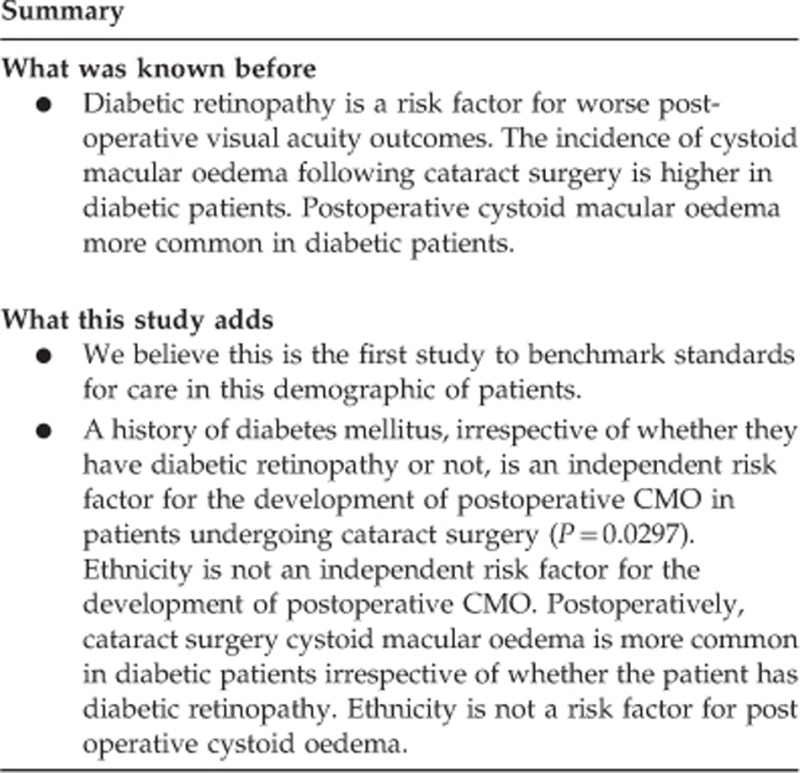
Conclusion
We believe this is the first study to benchmark standards for care in this demographic of patients. A history of diabetes mellitus, irrespective of whether there is diabetic retinopathy or not, is an independent risk factor for the development of post-operative CMO in patients undergoing cataract surgery (P=0.0297). Ethnicity is not an independent risk factor for the development of post-operative CMO.
Introduction
The Royal College of Ophthalmologists National Ophthalmology Database Audit (RCOphth NOD Audit) aims to analyse a nationally agreed cataract surgery data set and update the benchmark standards of care originally published through the Cataract National Database (CND) reports.1 However, both the CND and RCOphth NOD audit populations had much lower percentages of eyes with pre-existing diabetic retinopathy undergoing cataract surgery than our study population.1, 2 The study population of the CND was also ethnically less diverse with only 2.6% from the Black, Asian and minority ethnic group (BAME).
This difference in baseline characteristics of patients undergoing cataract surgery is important for several reasons. Diabetic retinopathy is a known risk indicator for worse visual acuity outcomes following cataract surgery.3 The Diabetic Retinopathy In Various Ethnic groups in UK (DRIVE UK) Study found a higher prevalence of both diabetic retinopathy (DR) and sight threatening DR in minority ethnic groups (South Asian, African and Afro-Caribbean).4 In addition, post-operative cystoid macular oedema (CMO), associated with worse visual outcomes, occurs more frequently in eyes with diabetic retinopathy.5 The published rates for post-operative CMO from the CND analysis of 16731 cataract operations was 1.62 vs 16.7% reported in a study of eyes with pre-existing diabetic retinopathy (3 and 19). We could find no published data comparing post-cataract surgery CMO rates in BAME vs white ethnic groups.
Given that our study population had a higher percentage of patients with diabetes mellitus and a greater BAME group than the published audits, we postulated that the incidence of post-cataract surgery CMO would be higher in our study population. Therefore the final post-operative visual acuity would be worse than those published in the CND and RCOphth NOD reports. As secondary outcome we wanted to determine whether ethnicity was a contributory factor in the development of post-operative CMO.
Materials and methods
Study population
The study was undertaken in a busy inner city eye unit in London. The catchment area included the London boroughs of Waltham Forest, Redbridge, and Newham. The patients were recruited exclusively from the Retina firm and were under the care of a single Consultant surgeon. The cataract surgery was performed either by a Consultant or a senior trainee. Cases complicated by posterior capsule rupture (PCR) were excluded as it is a known risk factor for CMO and likely to confound the results. No eyes received pre or post-operative prophylaxis with non-steroidal anti-inflammatory drugs (NSAIDs).
Outcome measures
The primary outcomes analysed in this study population were: (a) the percentage of eyes achieving a final post-operative Snellen acuity of 6/12 or better and (b) the percentage of eyes developing CMO following cataract surgery. The secondary outcomes included visual acuity outcomes and rates of post-operative CMO in the study sub-groups and statistical analysis of potential risk factors for post-operative CMO.
Data collection
The data was extracted from a single electronic medical records database (Medisoft Ophthalmology, Medisoft Ltd, Leeds, UK) over a 12 month period. The pre and post-operative Snellen visual acuity, ethnicity, diabetic status, grade of diabetic retinopathy, progression of diabetic maculopathy or retinopathy, development, treatment and outcome of post-operative CMO were recorded. The best recorded and pinhole visual acuity scores were used for both pre and post-operative vision. The optical coherence tomography (OCT) measurements were recorded from the macular volume scans taken on the Zeiss Cirrus OCT machine.
Diagnosis of post-operative CMO
A baseline macular OCT scan was performed pre-operatively in all eyes if the patient had a history of diabetes mellitus or there was pre-existing maculopathy of any aetiology such a retinal vascular disease or AMD.
In non-diabetic patients and if the eye to be operated was clinically normal on slit-lamp examination with a Volk Digital High Mag lens then a macular volume OCT scan was not routinely performed. All eyes had a macular volume OCT scan performed 4–8 weeks post-operatively to aid the diagnosis of post-operative CMO and differentiate between post-operative CMO and progression of pre-existing macular pathology. Post-operative CMO was diagnosed if the post-operative OCT scan showed typical features of intraretinal cysts and retinal thickening in an eye with either a normal macula on the pre-operative macular OCT scan or on slit-lamp examination with a Volk Digital High Mag lens. In eyes with abnormal pre-operative macular volume OCT scans, fundus fluorescein angiography was used to make the diagnosis.
Statistics
Statistical analysis was performed by using software SPSS ver (IBM SPSS Statistics for Windows, Version 19.0, IBM Corp, Armonk, NY, USA). Descriptive statistics including percentages and mean values were calculated for each group. Univariate analysis (two-sided χ2-test, or where appropriate Fischer’ s exact test) was performed to identify factors associated with post-operative CMO in different groups. A P-value <0.05 was considered statistically significant. Due to the relatively small sample size the power to detect a difference was small, and so a type 2 error cannot be excluded.
Results
Study demographics
The data of 282 eyes of 245 patients was extracted over a 12 month period. Of these 20 eyes were excluded as 16 did not attend their post-operative follow-up, 2 had incomplete records and 2 had posterior capsule ruptures (PCR). The total number of eyes included in the results analysis was 262. The mean age was 71 years (range 39–95) and the male to female ratio was 2:3. The ratio of Consultant to senior trainee operated eyes was 2:1.
Ethnicity
The study population was ethnically diverse with 40% (105/262) Asian, 18% (47/262) African or Caribbean, 35% (93/262) Caucasian and 6% classified as undefined. The Black, Asian, and minority ethnic group (BAME) was 59% accounting for over half the study population.
Diabetic status
The study population was predominantly diabetic with 57% (149/262) having a diagnosis of diabetes mellitus and 34% (88/262) having diabetic retinopathy. In the sub-group of the 149 eyes with a history of diabetes mellitus, 26 eyes had confirmed pre-operative diabetic macular oedema (DMO).
Baseline visual acuity
The pre-operative baseline Snellen visual acuity was 6/12 or better in 26.3% of eyes and worse than 6/60 in 6.5% of eyes.
Management of the pre-existing maculopathy in eyes undergoing cataract surgery
Of the 26 eyes that had pre-operative macular oedema, 15 were given 1–2 mg of intra-operative triamcinolone by intravitreal injection and 2 were given 0.5 mg of intra-operative ranibizumab by intravitreal injection. The remaining nine eyes did not receive any intravitreal therapy as they were outside the treatment guidelines or there were contraindications such as glaucoma. The 17 eyes that received intra-operative intravitreal triamcinolone or ranibizumab to manage pre-existing maculopathy were excluded from the statistical analysis.
Management of post-operative CMO in eyes undergoing cataract surgery
No eyes received pre or post-operative prophylaxis with non-steroidal anti-inflammatory drugs (NSAIDs). Of the 20 eyes that developed OCT confirmed post-operative CMO, 19 were treated with a 6–8 week course of Acular eye drops three times a day to the affected eye combined with dexamethasone 0.1% eye drops four times a day to the affected eye. One eye was treated with post-operative intravitreal triamcinolone.
Final post-operative visual acuity outcomes
In the total study population the number of eyes that achieved 6/12 or better Snellen acuity at the first post-operative review between 4–8 weeks was 76% (198/262). This increased to 79% (207/262) after adjusting for the improved VA scores achieved following completion of treatment for the eyes that had developed post-operative CMO. Within the study population subgroups, patients with no history of diabetes mellitus had better visual acuity outcomes with 84% achieving a post operative visual acuity of 6/12 or better, but this figure dropped to 68% in patients with diabetic retinopathy. Four eyes (1.5%), found to have post-operative visual acuity 6/60 or worse, had a guarded visual prognosis due to pre-existing co-morbidities and there was no deterioration in VA despite the surgical intervention. Five eyes (1.9%) lost three or more lines of Snellen visual acuity following surgery. All these eyes had underlying pathologies which included pre-existing DMO, age-related macular degeneration, uveitis and refractive error in an amblyopic eye. Of the 20 eyes that developed post-operative CMO only two failed to achieve a final post-operative visual acuity of 6/12 or better despite treatment. One of the two eyes with a poor visual outcome was later diagnosed as having CMO secondary to chronic uveitis rather than post-operative CMO.
Incidence of post-operative CMO
The incidence of post-operative CMO within the study population was 20 eyes out of 262 (7.6%). This does not include 17 eyes with a pre-existing macular oedema secondary to either diabetes (14 eyes) or retinal vein occlusion (3 eyes) that had been treated intra- operatively with either triamcinolone or ranibizumab. In eyes without a history of diabetes mellitus the incidence of postoperative CMO was 3.5% and in eyes with a history of diabetes mellitus the incidence of post-operative CMO was 10.7%. This difference was found to be clinically significant (P=0.0297). The post-operative CMO rate by surgeon grade was 6.3% for Consultants and 10% for senior trainees but this difference did not reach statistical significance. The rate of post-operative CMO by ethnic group was 10.5% in the BAME group vs 2.6% in the white ethnic group. The high prevalence of diabetes mellitus in the BAME ethnic group was found to be a confounding factor, which when adjusted for revealed that ethnicity was not an independent risk factor for post-operative CMO in our study population.
Discussion
We report the post-operative visual acuity and incidence of post-operative CMO following uncomplicated phacoemulsification cataract extraction and lens implantation in an urban, predominately Black, Asian, and minority Ethnic (BAME) and diabetic population.
Within our study cohort 76% had a visual acuity (VA) equal to or better than 6/12 post operatively increasing to 79% when including VA scores after completion of treatment for post operative CMO. This was lower than the reported VA outcomes for both the RCOphth NOD and the CND audit.
The overall incidence of post-operative CMO within the study group was 7.6%. It was 10.7% in patients with a history or diabetes mellitus regardless of whether or not they had diabetic retinopathy and much lower, only 3.5%, in patients with no history of diabetes mellitus. These rates were higher than the incidence of post-operative CMO reported in the CND audit.
One of the main reasons for these observed differences in VA outcomes and post-op CMO rates was postulated to be the wide difference in the baseline demographics of our study population as demonstrated in Table 1.
Table 1. This table compares key differences in the baseline characteristics and outcomes between our study population the Royal College of Ophthalmologists NOD audit and the Cataract National Database audit.
| Study cohort all eyes (%) | RCOphth NOD audit all eyes (%) | CND audit all eyes (%) | |
|---|---|---|---|
| Baseline VA equal to or better than 6/12 | 26.3 | 32 (first eye) 47.7 (second eye) | 42.9 |
| Diabetic retinopathy | 34 | 4.7 | 3.3 |
| Post-op VA equal to or better 6/12 | 79 | 89.9 | 91 |
| Post op CMO | 7.6 | Not reported | 1.62 |
In our study population over half or 57% had a history of diabetes mellitus with 34% having diabetic retinopathy at the time of surgery, compared to the RCOphth NOD audit and CND audit of 4.7 and 3.3% with diabetic retinopathy, respectively. Diabetic retinopathy is a known risk indicator for worse visual acuity outcomes following cataract surgery.3
In addition, within the RCOphth NOD audit 32% of first eyes and 47.7% of second eyes had a pre-operative VA equal to or better than 6/12. Similarly 42.9% had a VA equal to or better than 6/12 in the CND audit. Within our study population only 26.3% had a VA equal to or better than 6/12 pre-operatively. The Early treatment Diabetic Retinopathy Study (ETDRS) identified poor pre-operative VA as a risk factor for poor postoperative outcome, possibly attributed to macular oedema, macular ischaemia or traction.5 In addition, they reported that the severity of DR at the time of cataract surgery affected the post operative outcome suggesting that this could be associated with an increased incidence of macular ischaemia.5
Our study population consisted of 59% Black, Asian and minority ethnic groups compared to 2.6% in the CND audit. Although ethnicity was not found to be an independent risk factor for post operative CMO within our study, the Diabetic Retinopathy In Various Ethnic groups in UK (DRIVE UK) study found a higher prevalence of both diabetic retinopathy (DR) and sight threatening DR in minority ethnic groups (South Asian, African, and Afro-Caribbean).4 Diabetes has been associated with poorer outcomes post-cataract surgery. Post-operative inflammation is thought to be the most important factor in the development of postoperative complications within diabetic subjects. Menchini et al reported intraocular inflammation and its sequelae as the most common complication in their study.6 Similarly, Ivancic et al. reported that inflammatory reactions and bleeding were more common in diabetic patients post-cataract surgery resulting in anterior segment complications including post-operative keratopathy, fibrinous uveitis and posterior capsule opacity.7 Greenberg et al8 showed that of 45 082 patients undergoing cataract extraction, subjects with diabetic retinopathy had a 33% higher operative complication risk compared with those without diabetic retinopathy. Furthermore several studies have shown that diabetic patients are at higher risk of, DMO worsening,9, 10, 11 DR progression,12 and CMO.13
Risk factors for postoperative complications have been linked to the severity of retinopathy and maculopathy prior to cataract surgery, higher HbA1c levels,14 and type 2 diabetes.15 Our findings demonstrated that a history of diabetes mellitus in patients undergoing cataract surgery is an independent risk factor for the development of post-operative CMO (P=0.0297).
This supports published data that macular changes are more likely to occur in diabetic patients following uncomplicated cataract surgery with incidences reported as ranging from 31 to 81%.16, 17, 18 It is believed that release of prostaglandins in the postoperative inflammatory process causes fluid leakage from perifoveal capillaries into the extra cellular space within the retina. Muller cell lysis occurs secondary to excessive fluid accumulation with fluid collecting in the outer plexiform and inner nuclear layers of the retina. It is likely that diabetic patients are more susceptible to this postoperative inflammatory response due to an already altered blood retinal barrier secondary to hyperglycaemia and sub-clinical inflammation.
Following treatment for CMO with topical keratolac and dexamethasone for 6–8 weeks, 90% eyes that developed post-operative CMO regained a VA of equal to or better than 6/12 with resolution of CMO on the macular OCT scans. No prophylaxis therapy was used in the study cohort. However a recent study has clearly demonstrated that in diabetic patients with non-proliferative diabetic retinopathy, treatment with the NSAID Nepafenac 0.1% eye drops 1 day prior to surgery through to day 90 post operatively can significantly reduce the incidence of post-operative CMO from 16.7 to 3.2%.19 A more recent meta-analysis showed that in diabetic patients with or without diabetic retinopathy the optimum treatment regime to reduce the incidence of post-operative CMO was a combination of topical dexamethasone and NSAID post operatively in diabetic patients.20
It will be soon be mandatory for individual surgeons to publish cataract surgery outcomes. Given the differences in the demographic make up within different parts of the UK is it possible to compare such different population groups?
Footnotes
The authors declare no conflict of interest.
References
- Day AC, Donachie PH, Sparrow JM, Johnston RL Royal College of Ophthalmologists' National Ophthalmology database. The Royal College of Ophthalmologists, National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications. Eye 2015; 29: 552–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, Galloway P et al. The Cataract national dataset electronic multi-centre audit of 55 567 operations: updating benchmark standards of care in the United Kingdom and Internationally. Eye 2009; 23: 38–49. [DOI] [PubMed] [Google Scholar]
- Sparrow JM, Taylor H, Qureshi K, Smith R, Birnie K, Johnston RL. The Cataract National Dataset electronic multi centre audit of 55567 operations: risk indicators for monocular visual acuity outcome. Eye 2012; 26: 821–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivaprasad S, Gupta B, Gulliford MC, Dodhia H, Mann S, Nagi D et al. Ethnic Variations in the Prevalence of Diabetic Retinopathy in People attending Screening in the United Kingdom (DRIVE UK). PLoS One 2012; 7(3): e32182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew EY, Benson WE, Remaley NA, Lindley AA, Burton TC, Csaky K et al. Results after lens extraction in patients with diabetic retinopathy: early treatment diabetic retinopathy study report number 25. Arch Ophthalmol 1999; 117(12): 1600–1606. [DOI] [PubMed] [Google Scholar]
- Mechini U, Cappelli S, Virgili G. Cataract surgery and diabetic retinopathy. Semin Ophthalmol 2003; 18: 103–108. [DOI] [PubMed] [Google Scholar]
- Ivancic D, Mandic Z, Barac C, Kopic M. Cataract surgery and post operative complication in diabetic patients. Coll Antropol 2005; 29(Suppl 1): 55–58. [PubMed] [Google Scholar]
- Greenberg PB, Tseng VL, Wu WC, Liu J, Jiang L, Chen CK et al. Prevalence and predictors of ocular complications associated with cataract surgery in United States veterans. Ophthalmology 2011; 118(3): 507–514. [DOI] [PubMed] [Google Scholar]
- Kim SJ, Equi R, Bressler NM. Analysis of macuar oedema after cataract surgery in patients with diabetes using optical coherence tomography. Ophthalmology 2007; 114(5): 881–889. [DOI] [PubMed] [Google Scholar]
- Pate JL, Hykin PG, Cree IA. Diabetic cataract removal: Postoperative progression of maculopathy: Growth factor and clinical analysis. Br J Ophthalmology 2006; 90(6): 697–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SJ, Belair ML, Bressler NM, Dunn JP, Thorne JE, Kedhar SR et al. A method of reporting macular oedema after cataract surgery using optical coherence tomography. Retina 2008; 28(6): 870–876. [DOI] [PubMed] [Google Scholar]
- Gupta A, Gupta V. Diabetic maculopathy and cataract surgery. Ophthalmol Clin North Am 2001; 14(4): 625–637. [DOI] [PubMed] [Google Scholar]
- Mechini, Bandello F, Brancato R, Camesasca FI, Galdini M. Cystoid macular oedema after extracapsular cataract extraction and lens implantation in diabetic patients without retinopathy. Br J Ophthalmol 1993; 77(4): 208–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diabetes Control and Complications Trial Research Group. The Diabetes Control and Complications Trial. The effect of intensive diabetes treatment on the progression of diabetic retinopathy in insulin-dependent diabetes mellitus. Arch Ophthalmol 1995; 113(1): 36–51. [DOI] [PubMed] [Google Scholar]
- Flesner P, Sander B, Henning V, Parving HH, Dornonville de la Cour M, Lund-Andersen H. Cataract surgery on diabetic patients: a prospective evaluation of risk factors and complications. Acta Ophthalmol Scand 2002; 80(1): 19–24. [DOI] [PubMed] [Google Scholar]
- Tranos PG, Wickremasinghe SS, Stangos NT, Topouzis F, Tsinopoulos I, Pavesio CE. Macular oedema. Surv Ophthalmol 2004; 49: 470–490. [DOI] [PubMed] [Google Scholar]
- Ursell PG, Spalton DJ, Whitcup SM, Nussenblatt RB. Cystoid macular oedema after phacoemulsification: relationship to blood-aqueous barrier damage and visual acuity. J Cataract Refract Surg 1999; 25: 1492–1497. [DOI] [PubMed] [Google Scholar]
- Hayashi K, Igarashi C, Hirata A, Hayashi H. Changes in diabetic macular oedema after phacoemulsification surgery. Eye (Lond) 2009; 23: 389–396. [DOI] [PubMed] [Google Scholar]
- Singh R, Alpern L, Jaffe GJ, Lehmann RP, Lim J, Reiser HJ et al. Evaulation of nepafenac in prevention of macular edema following cataract surgery in patients with diabetic retinopathy. Clin Ophthalmol 2012; 6: 1259–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wielders L, Lambermont VA, Schouten JS, van den Biggelaar FJ, Worthy G, Simons RW et al. Prevention of cystoid macular Edema after cataract surgery in nondiabetic and diabetic patients; a systemic review and meta-analysis. Am J Ophthalmol 2015; 160(5): 968–981. [DOI] [PubMed] [Google Scholar]


