Abstract
Background:
Psychological factors have been prominently implicated in the causation as well as maintenance of irritable bowel syndrome (IBS). Studies comparing psychiatric morbidity in IBS with healthy controls have reported contrasting findings. The current study was undertaken to assess the prevalence of anxiety and depression in patients with IBS in comparison to healthy controls and to explore the relationship, if any, of anxiety and depression with various subtypes of IBS.
Materials and Methods:
Fifty consecutive patients of IBS (diagnosed as per Rome III criteria) between 18 and 65 years of age and fifty age- and sex-matched healthy controls were assessed for the presence of anxiety and depression using Hamilton Rating Scale for Anxiety (HAMA) and Hamilton Rating Scale for Depression (HAMD), respectively.
Results:
The patient group scored higher than controls (P < 0.001) in both HAMA and HAMD scores. The HAMA scores were significantly higher (P < 0.001) in the severe IBS group compared to those with moderate IBS. HAMA scores predicted 25.6% (R2 = 0.256) of variance in IBS severity scores. However, there was no significant difference between the two groups in terms of HAMD scores.
Conclusion:
The high prevalence of psychiatric comorbidities such as anxiety and depression in IBS samples in our study provides evidence in favor of proper screening for these disorders in gastrointestinal clinics. Recognition and treatment for these comorbidities can improve the quality of life as well as overall outcomes.
Keywords: Anxiety, depression, irritable bowel
INTRODUCTION
Irritable bowel syndrome (IBS) is a chronic disorder characterized by abdominal pain or discomfort and alteration in bowel habits in the absence of an organic disorder. IBS is one of the most common gastrointestinal (GI) disorders and its prevalence varies from 4% to 22% in the general population.[1,2] Indian studies have shown this condition to be a fairly common GI condition, accounting for 30%–50% of referrals to gastroenterology clinics.[3] Although the exact pathophysiology of IBS is not known, psychological factors have been prominently implicated in its causation as well as maintenance. As per the biopsychosocial model, IBS results from an interaction of the central nervous system, various psychological factors as well as altered intestinal motility and sensitivity. Traumatic life events such as early maternal separation and sexual abuse have been found to play an important role in the subsequent development of IBS.[4] Thus, it becomes important to explore psychiatric conditions associated with IBS.
The prevalence of psychiatric conditions in IBS ranges from 40% to 100%. Several studies have assessed the prevalence of anxiety and depression in IBS and compared them to healthy controls. While some studies reported elevated levels of anxiety and depression in IBS compared to healthy controls,[5,6,7] other studies have found no such association.[8,9] Moreover, contrasting findings have also been reported regarding the association of various subtypes of IBS with anxiety and depression. Some studies have reported the association of constipation predominant variety of IBS (IBS-C) with higher levels of anxiety[10] while other studies have found no such association.[7] Hence, the current study was undertaken to assess the prevalence of anxiety and depression in patients with IBS in comparison to healthy controls and to explore the relationship, if any, of anxiety and depression with various subtypes of IBS.
MATERIALS AND METHODS
The study was carried out at the Department of Gastroenterology, School of Digestive and Liver Diseases, IPGMER and SSKM Hospital, Kolkata. Proper approval was obtained from the Institutional Ethics Committee of IPGMER. Fifty consecutive patients of IBS (diagnosed as per Rome III criteria) between 18 and 65 years of age were enrolled for the study following their informed consent. Patients with other preexisting GI disorders, patients with GI surgery, abnormal upper and lower GI endoscopy, patients of chronic medical illness, namely, chronic kidney disease and diabetes mellitus, and those taking drugs producing GI symptoms or affecting GI motility were excluded from the study. Fifty age- and sex-matched healthy controls not having IBS and other chronic medical illness or taking drugs producing GI symptoms and affecting GI motility were recruited from among the staffs of SSKM Hospital. The patients of IBS were further classified as per Rome III criteria[11] into IBS-C, diarrhea predominant IBS (IBS-D), IBS with mix of 2 symptoms (IBS-M), and IBS unsubtype, with neither constipation nor diarrhea. The patients of IBS were categorized into mild, moderate, and severe according to the Irritable Bowel Syndrome Severity Scoring Scale.[12] Thereafter, the patients were assessed for the presence of anxiety and depression using Hamilton Rating Scale for Anxiety (HAMA)[13] and Hamilton Rating Scale for Depression (HAMD),[14] respectively.
Statistical analysis
Descriptive statistics were used for sociodemographic and clinical variables. For detecting group difference between variables, independent samples t-test and Pearson's Chi-square test were used for continuous and categorical variables, respectively. To determine the relationship between HAMA scores and IBS severity scores, simple regression analysis was carried out. SPSS software (version 10.0, IBM) was used for analysis of data. A confidence level of 95%, i.e., P < 0.05 (two tailed) was considered statistically significant.
RESULTS
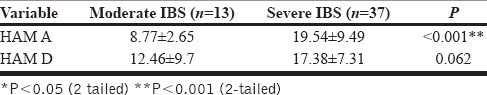
The mean age of the case group was 37.48 (± 10.90) years while that of the control group was 37.50 (± 10.72) years. There were 37 (74%) males and 13 (26%) females in each of the case and the control groups. In terms of severity scores, 13 patients were found to have moderate IBS and 37 had severe IBS. Among IBS subtypes, 11 patients had IBS-C and 39 patients had IBS-D. Table 1 shows the difference between cases and controls in terms of HAMA and HAMD scores. The patient group scored higher than controls (P < 0.001) in both HAMA and HAMD scores. Table 2 shows the difference between cases of moderate and severe IBS in terms of anxiety and depression. The HAMA scores were significantly higher (P < 0.001) in the severe IBS group. Simple regression analysis carried out with IBS severity scores as dependent variable and HAMA scores as predictor variable revealed that HAMA scores predicted 25.6% (R2 = 0.256) of variance in IBS severity scores. However, there was no significant difference between the two groups in terms of HAMD scores. There was no significant difference between IBS-C and IBS-D groups in terms of anxiety (HAMA) and depression (HAMD) scores. The prevalence of syndromal anxiety and depression was calculated in patients with IBS as well as controls using HAMA (>18) and HAMD (>7) cutoff scores. Among patients with IBS, the prevalence of anxiety was 44% and that of depression was 84%. In healthy controls, the prevalence of anxiety was 8% and that of depression was 6%.
Table 1.
Difference between IBS cases and healthy controls in terms of HAM A and HAM D scores
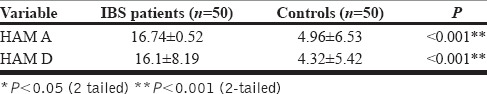
Table 2.
The difference between cases of moderate and severe IBS in terms of anxiety and depression
DISCUSSION
We assessed fifty consecutive patients of IBS for the presence of anxiety and depression and compared them with healthy controls. We used HAMA and HAMD scores for the assessment of anxiety and depression, respectively. Both these tools are considered to be one of the most standardized and validated tools in psychiatry for research purposes. Some of the previous studies examining psychiatric morbidity in IBS have used the Hospital Anxiety and Depression Scale (HADS). The HADS has been criticized as an inadequate tool when separate measures of anxiety and depression are required. Similar criticisms also apply to scales such as Symptom Checklist and Patient Health Questionnaire, which have been used in other studies. Beck's Depression Inventory and Beck's Anxiety Inventory used in another study is a well-validated instrument, but being a subjective assessment, leaves room for overreporting of psychiatric symptoms. The patients of IBS with multiple somatic preoccupations are more prone to overreport anxiety and depressive symptoms. HAMD and HAMA, being clinician rated, offer advantage in this aspect as a trained clinician objectively rates the symptoms and the confounding effects of overreporting are minimized.
Sociodemographic features
The mean age of the IBS case group was 37.48 ± (10.90) years, which is in accordance with the study by Ghoshal et al.[15] where the mean age of presentation was 39.4 years. In our study, there were 37 males (74%) and 13 females (26%). This was in accordance with other Indian studies where male preponderance is seen. The multicentric study by Ghoshal et al. showed that 68% of the IBS patients were males. Male preponderance has been observed in other Indian studies where it ranges from 66%[16] to 87%.[17] This male predominance may be due to differing patterns of health-care-seeking behavior between males and females in our country. This appears more so because findings from Indian and Asian studies seem to stand in contrast to Western studies which have consistently shown women to be at greater risk for IBS.[18] Further investigations are required, especially community-based studies, to determine the exact cause of this gender difference in IBS across continents.
In our study, 37 patients had severe IBS and 13 patients had moderate IBS. None had mild IBS. It may be because mild cases seek medical care less often or present more commonly to a primary care setup.
Prevalence of anxiety and depression
The prevalence of anxiety in the patients with IBS (as determined by HAMA cutoff scores) in our study was 44%. Kabra and Nadkarni found the prevalence of anxiety disorder to be 37.1% in the patients with IBS.[19] Similarly, Modabbernia et al.[20] in a study of patients with IBS in Iran found the prevalence of anxiety symptoms in 35.5% of patients. Hence, our study results regarding the prevalence in anxiety in IBS patients are in keeping with the available literature.
The severity of comorbid anxiety was measured using HAMA. The mean HAMA score of the IBS cases was 16.74 (± 9.52) and that of the controls was 4.96 (± 6.53). HAMA scores were significantly higher (P < 0.001) in patients with IBS in comparison to normal controls. This finding is in agreement with several Indian as well as Western studies. Makharia et al.[2] in a study comparing 184 patients with IBS with 198 normal controls found significantly higher levels of panic and other anxiety syndrome in patients with IBS. Similar findings have also been reported from India by Kabra and Nadkarni.[19] Koloski et al.[22] and Locke et al.[23] have reported similar findings from Western population.
The prevalence of depression in patients with IBS was 84% in our study. The result was in accordance with the study of Tosic-Golubovic et al.[24] where the prevalence of depression in patients with IBS was 83.33%. The mean HAMD score of patients with IBS was 16.1 (± 8.19) and that of the controls was 4.32 (± 5.42). This difference was statistically significant (P < 0.001). van der Veek et al.[25] and Sugaya et al.[7] have also reported higher levels of anxiety and depression in patients with IBS in comparison to healthy controls.
Among the etiological models of IBS, there is support for the hypothesis that dysfunction in brain-gut axis plays an important role in the presentation of the condition.[26,27] This hypothesis of IBS has two models. According to the bottom-up model, abdominal symptoms secondarily influence anxiety and depression. As per the top-down model, the psychological factors such as stress, anxiety, and depression themselves influence physiological factors such as motor functions, sensory threshold, and stress reactivity of the gut through vagal and sympathetic afferents. Our findings of elevated levels of anxiety and depression in patients with IBS lend further support to the inseparable role of psychological factors in this disorder. Thus, looking for comorbid anxiety and depression in patients with IBS will not only helps in understanding this disease better but also contributes in terms of better treatment outcome.
Anxiety and depression and severity of irritable bowel syndrome
The mean HAMA score of the moderate IBS cases was 8.77 (± 2.65) while that of the severe IBS cases was 19.54 (± 9.49) with a statistically significant (P < 0.001) difference between the two groups. Simple regression analysis revealed that HAMA scores predicted 25.6% (R2 = 0.256) of variance in IBS severity scores. Thus, in our study sample, anxiety scores accounted for as much as one fourth the increase in IBS severity which is a fairly large variance. Unlike most previous studies,[21,22] we were able to demonstrate a dose–response relationship between anxiety and IBS in our study sample, which may have a prominent implication in the clinical management of these cases. Drossman also showed that anxiety score increases as the severity of IBS increases.[28] They also concluded that psychological factors such as anxiety appear to play important roles as moderators of symptom severity, symptom persistence, decisions to seek treatment, and response to treatment. van Tilburg et al.[29] explored which psychological factors had the highest impact on severity of IBS and concluded that anxiety had an indirect effect on amplification of IBS symptoms through psychological mechanisms of catastrophizing, as well as somatization. Anxiety, in turn, was predicted by neuroticism and stressful life events. Hence, anxiety symptoms should be specifically assessed and treated in IBS.
Anxiety and depression and subtypes of irritable bowel syndrome
There was no significant difference between IBS-C and IBS-D groups in terms of anxiety (HAMA) and depression (HAMD) scores. Fond et al.[30] in their meta-analysis examined eight studies, which had specifically examined the relationship among anxiety, depression, and IBS subtypes. They concluded that both IBS-C and IBS-D subtypes had higher levels of anxiety and depression in comparison to healthy controls.
LIMITATIONS AND CONCLUSION
In spite of methodological improvements over previous studies, our study had few limitations. Small sample size and hospital-based samples representing more severe cases limit the generalizability of our findings. Cross-sectional nature of our study could prove an association between anxiety, depression, and IBS, but community-based longitudinal designs would be important to probe causality.
IBS accounts for a huge proportion of referrals to gastroenterology clinics, and the cost burden to the patients with IBS and the society is substantial. The high prevalence of psychiatric comorbidities such as anxiety and depression in IBS samples in our study provides evidence in favor of proper screening for these disorders in GI clinics. Recognition and treatment for these comorbidities can improve the quality of life as well as overall outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Choung RS, Locke GR., 3rd Epidemiology of IBS. Gastroenterol Clin North Am. 2011;40:1–10. doi: 10.1016/j.gtc.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Makharia GK, Verma AK, Amarchand R, Goswami A, Singh P, Agnihotri A, et al. Prevalence of irritable bowel syndrome: A community based study from Northern India. J Neurogastroenterol Motil. 2011;17:82–7. doi: 10.5056/jnm.2011.17.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kapoor KK, Nigam P, Rastogi CK, Kumar A, Gupta AK. Clinical profile of irritable bowel syndrome. Indian J Gastroenterol. 1985;4:15–6. [PubMed] [Google Scholar]
- 4.Porcelli P. Psychological abnormalities in patients with irritable bowel syndrome. Indian J Gastroenterol. 2004;23:63–9. [PubMed] [Google Scholar]
- 5.Cho HS, Park JM, Lim CH, Cho YK, Lee IS, Kim SW, et al. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver. 2011;5:29–36. doi: 10.5009/gnl.2011.5.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Savas LS, White DL, Wieman M, Daci K, Fitzgerald S, Laday Smith S, et al. Irritable bowel syndrome and dyspepsia among women veterans: Prevalence and association with psychological distress. Aliment Pharmacol Ther. 2009;29:115–25. doi: 10.1111/j.1365-2036.2008.03847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sugaya N, Nomura S, Shimada H. Relationship between cognitive factors and anxiety in individuals with irritable bowel syndrome. Int J Behav Med. 2012;19:308–15. doi: 10.1007/s12529-011-9195-0. [DOI] [PubMed] [Google Scholar]
- 8.Alander T, Heimer G, Svärdsudd K, Agréus L. Abuse in women and men with and without functional gastrointestinal disorders. Dig Dis Sci. 2008;53:1856–64. doi: 10.1007/s10620-007-0101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berman S, Suyenobu B, Naliboff BD, Bueller J, Stains J, Wong H, et al. Evidence for alterations in central noradrenergic signaling in irritable bowel syndrome. Neuroimage. 2012;63:1854–63. doi: 10.1016/j.neuroimage.2012.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muscatello MR, Bruno A, Pandolfo G, Micò U, Stilo S, Scaffidi M, et al. Depression, anxiety and anger in subtypes of irritable bowel syndrome patients. J Clin Psychol Med Settings. 2010;17:64–70. doi: 10.1007/s10880-009-9182-7. [DOI] [PubMed] [Google Scholar]
- 11.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–91. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 12.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: A simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11:395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- 13.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghoshal UC, Abraham P, Bhatt C, Choudhuri G, Bhatia SJ, Shenoy KT, et al. Epidemiological and clinical profile of irritable bowel syndrome in India: Report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2008;27:22–8. [PubMed] [Google Scholar]
- 16.Pimparkar BD. Irritable colon syndrome. J Indian Med Assoc. 1970;54:95–103. [PubMed] [Google Scholar]
- 17.Arun P, Vyas JN, Rai RR, Kanwal K, Sushil CS. Psychological and sociodemographic correlates of the irritable bowel syndrome. Indian J Psychiatry. 1993;35:193–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Gwee KA, Bak YT, Ghoshal UC, Gonlachanvit S, Lee OY, Fock KM, et al. Asian consensus on irritable bowel syndrome. J Gastroenterol Hepatol. 2010;25:1189–205. doi: 10.1111/j.1440-1746.2010.06353.x. [DOI] [PubMed] [Google Scholar]
- 19.Kabra N, Nadkarni A. Prevalence of depression and anxiety in irritable bowel syndrome: A clinic based study from India. Indian J Psychiatry. 2013;55:77–80. doi: 10.4103/0019-5545.105520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Modabbernia MJ, Mansour-Ghanaei F, Imani A, Mirsafa-Moghaddam SA, Sedigh-Rahimabadi M, Yousefi-Mashhour M, et al. Anxiety-depressive disorders among irritable bowel syndrome patients in Guilan, Iran. BMC Res Notes. 2012;5:112. doi: 10.1186/1756-0500-5-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh P, Agnihotri A, Pathak MK, Shirazi A, Tiwari RP, Sreenivas V, et al. Psychiatric, somatic and other functional gastrointestinal disorders in patients with irritable bowel syndrome at a tertiary care center. J Neurogastroenterol Motil. 2012;18:324–31. doi: 10.5056/jnm.2012.18.3.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koloski NA, Talley NJ, Boyce PM. Epidemiology and health care seeking in the functional GI disorders: A population-based study. Am J Gastroenterol. 2002;97:2290–9. doi: 10.1111/j.1572-0241.2002.05783.x. [DOI] [PubMed] [Google Scholar]
- 23.Locke GR, 3rd, Weaver AL, Melton LJ, 3rd, Talley NJ. Psychosocial factors are linked to functional gastrointestinal disorders: A population based nested case-control study. Am J Gastroenterol. 2004;99:350–7. doi: 10.1111/j.1572-0241.2004.04043.x. [DOI] [PubMed] [Google Scholar]
- 24.Tosic-Golubovic S, Miljkovic S, Nagorni A, Lazarevic D, Nikolic G. Irritable bowel syndrome, anxiety, depression and personality characteristics. Psychiatr Danub. 2010;22:418–24. [PubMed] [Google Scholar]
- 25.van der Veek PP, Van Rood YR, Masclee AA. Symptom severity but not psychopathology predicts visceral hypersensitivity in irritable bowel syndrome. Clin Gastroenterol Hepatol. 2008;6:321–8. doi: 10.1016/j.cgh.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Bercik P, Collins SM, Verdu EF. Microbes and the gut-brain axis. Neurogastroenterol Motil. 2012;24:405–13. doi: 10.1111/j.1365-2982.2012.01906.x. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy PJ, Clarke G, Quigley EM, Groeger JA, Dinan TG, Cryan JF. Gut memories: Towards a cognitive neurobiology of irritable bowel syndrome. Neurosci Biobehav Rev. 2012;36:310–40. doi: 10.1016/j.neubiorev.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Drossman DA. Do psychosocial factors define symptom severity and patient status in irritable bowel syndrome? Am J Med. 1999;107:41S–50S. doi: 10.1016/s0002-9343(99)00081-9. [DOI] [PubMed] [Google Scholar]
- 29.van Tilburg MA, Palsson OS, Whitehead WE. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. J Psychosom Res. 2013;74:486–92. doi: 10.1016/j.jpsychores.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fond G, Loundou A, Hamdani N, Boukouaci W, Dargel A, Oliveira J, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): A systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264:651–60. doi: 10.1007/s00406-014-0502-z. [DOI] [PubMed] [Google Scholar]


