Abstract
Cognitive deficits in patients with schizophrenia have been documented consistently. They are known to contribute to functional impairment in patients. Cognitive remediation has been found to be beneficial in symptoms reduction and functional recovery. CH was a 26/F, completed her graduation, currently pursuing a management course through correspondence, unmarried, currently living with her parents, from Bengaluru, right-handed, Middle socio economic status (MSES). A diagnosis of paranoid schizophrenia was referred for cognitive assessment and rehabilitation. Patient's cognitive assessment showed impairment in all the cognitive domains. She was given home-based and neurofeedback training along with family intervention. Significant improvement was seen in patients overall functioning.
Keywords: Cognitive assessment, cognitive retraining, neurofeedback training
INTRODUCTION
Cognitive deficits in patients with schizophrenia have been documented consistently. They are known to contribute to functional impairment in patients.[1,2] Deficits in neurocognition have long since been understood as a core feature in schizophrenia, and not a manifestation of iatrogenic effects, chronicity, or social drifting. Meta-analytic studies have found impairments in all domains of cognitive functioning – intelligence quotient, memory, language, executive function, and attention. Cognitive remediation has been found to be beneficial in symptoms reduction and functional recovery. The use of electroencephalograph - neurofeedback training in improving cognitive functions in schizophrenia has been scarcely recorded in literature. Since in the Indian context most of the patients live with their families and family contexts can influence recovery in patients.
Design
Pre–post-interventional single case study design was adopted.
CASE REPORT
CH was a 26/F, completed her graduation, currently pursuing a management course through correspondence, unmarried, currently living with her parents, from Bengaluru, right-handed, MSES. A diagnosis of paranoid schizophrenia was made by the adult psychiatry unit and referred for neuropsychological assessment and rehabilitation to the neuropsychology unit.
CH had a 13-year history of schizophrenia, with an episodic course. The episodes had been characterized by hallucinations, and negative symptoms of apathy, social withdrawal, and blunted affect. Her social functioning was also impaired, and characterized by poor interpersonal relationships, difficulty in communication, poor social skills. There was a history of specific learning difficulty, family history of schizophrenia and schizoid personality disorder in first-degree relatives, schizoid personality in multiple second- and third-degree relatives on the paternal side. Temperamentally, the patient had been a difficult child. CH was receiving a stable dosage of antipsychotic medication.
CH presented to the neuropsychology unit with complaints of poor concentration, inability to study and recall learnt material, poor interpersonal relationship with mother. At the time of presentation, CH had no positive symptoms, but negative symptoms of blunted affect, poor abstraction, emotional withdrawal, and social withdrawal were present.
Neuropsychological assessment pre–post-neuropsychological rehabilitation was carried out.
Tools
Patient's cognitive functions were assessed pre- and post-intervention using the National Institute of Mental Health and Neuro Science (NIMHANS) neuropsychology battery[3]
Patient's social functioning: assessed through an interview with patient and her primary caregiver (mother) and observations of the therapist.
Intervention
Cognitive retraining
CH was given a home-based cognitive retraining program developed by Hegde.[4] Domain-wise retraining was done as per a predetermined schedule over a period of 10 weeks. CH visited the hospital once a week; on other days, she performed the retraining tasks at home for approximately 1 h daily.
The neurocognitive functions for which retraining was provided were: attention, mental speed, response inhibition, information processing, working memory, nonverbal fluency, verbal fluency, sustained attention and set shifting, visuoconstructive ability, visuospatial reasoning, planning, abstraction, and immediate visual memory.
Electroencephalograph neurofeedback training (EEG NFT)
EEG NFT is noninvasive brain wave training, targeted at specific brain waves that have been shown to improve cognitive functions in many clinical conditions. Twenty sessions of alpha/theta protocol with O1, O2 scalp locations training on alternate days for a duration of 40 min was given to the patient.
Family intervention
The family intervention was guided by the family intervention manual developed at NIMHANS.[5] Sessions were held with CH and her mother to address the interpersonal problems occurring between them. This was done by working on communication style of the mother, her perfectionism, helping her to develop realistic expectations from the patient, encouraging her to reinforce the CH's adaptive behaviors. Need for direct, clear, and mutually respectful communication was discussed with CH and her mother. Time during the weekly sessions was also given to the mother to address issues of caregiver burden.
Social functioning
A pre- and post-intervention comparison of patient's social functioning revealed significant improvement.
Mother reported that CH had improved in her communication style. Interactions between them became more pleasant. Patient's motivation had improved significantly, as indicated by her increased participation in household activities, interest in grooming herself, and going for hobby classes in the course of the interventions. The patient showed more empathy for mother, which she did not show earlier. She was noted to be getting less annoyed and irritable. Mother felt that patient could relate to her better now, compared to the past. Patient's emotional reactivity improved. She was laughing and smiling more in social interactions. The patient reported that her studies were gradually improving. Therapist's observations were that patient's expressive speech improved, conversational ability was better, affect was increased in range.
Cognitive functions
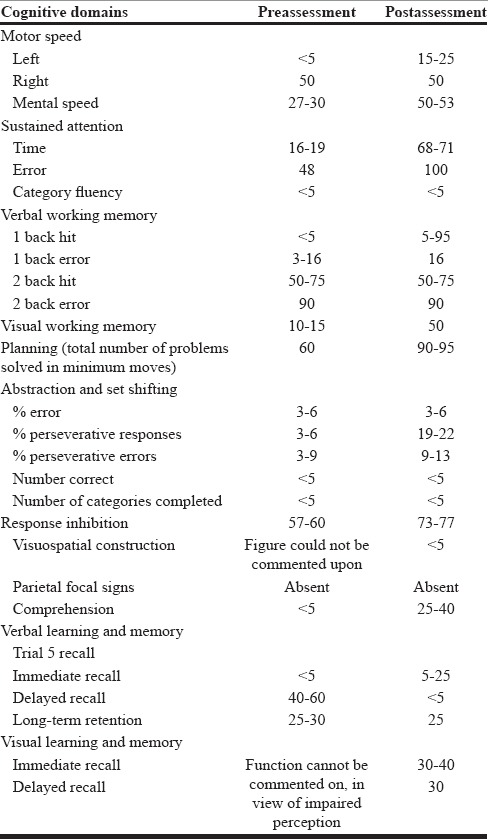
A pre- and post-intervention comparison of performance on the neuropsychology battery revealed improvement in most neurocognitive domains. Details are given in the [Table 1] below. All figures indicate percentiles. Percentiles below 15 indicate deficit; 15th percentile and above indicate adequacy in neurocognitive functioning.
Table 1.
Pre-Post Cognitive Functions (NIMHANS Neuropsychology Battery Rao et al. 2004)
DISCUSSION
The integrated cognitive remediation and psychosocial intervention programs were found to be useful in improving social functioning in a patient with schizophrenia. Postintervention deficits remained in category fluency, abstraction, and set shifting. Cognitive retraining augments the process of social and occupational recovery by improving neural plasticity, thereby facilitating patient's ability to learn and carry out social and occupational activities. In addition, improved interpersonal relationship between the patient and the family member and improved cognitive functioning reduces criticality toward the patient. This may increase the motivation of the patient. The study also highlights the role of addressing concerns of caregivers of patients with schizophrenia with regard to handling difficult behaviors of patients and caregiver burden.
CONCLUSION
Cognitive retraining has proven to be useful in patients with schizophrenia. Cognitive retraining improves cognitive functions. It augments social and occupational functioning. When it is used in conjunction with family intervention, improvement in an interpersonal relationship is seen. Patient subjectively reported significant improvement (80%) in attention, concentration, and patience. The mother reported 60% improvement in patient's ability to concentrate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–30. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 2.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–36. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 3.Rao SL, Subbukrishna DK, Gopukuar K. NIMHANS Neuropsychology Battery – 2004. NIMHANS Publication No. 60. Bangalore: NIMHANS; 2004. [Google Scholar]
- 4.Hegde S. Addition of Cognitive Retraining to Improve Global Functioning in Schizophrenia: A Randomised Controlled Study. Unpublished PhD Thesis Submitted to NIMHANS (Deemed University) 2008 [Google Scholar]
- 5.Varghese M, Shah A, Udayakumar GS, Murali T, Isabel MP. Family intervention and support in schizophrenia: A manual on family intervention for the mental health professional. Bangalore: NIMHANS; 2004. [Google Scholar]


