Introduction
The goal of total knee arthroplasty (TKA) is to provide the patient with a well-functioning, pain-free knee that will last for many years. To improve implant survival, the goal is to position the prosthesis in a way that restores proper biomechanical alignment, and advances in technology have enabled arthroplasty surgeons to produce accurate results on a more consistent basis. One of these advances is the use of computer-assisted orthopaedic surgery (CAOS) to assist in proper component alignment and produce accurate restoration of the biomechanical axis consistently.1–17 Functional scores and revision-free survival are at least equivalent to conventional arthroplasty.17–26
Traditional cutting guides for TKA rely on intramedullary femoral instruments, and either intramedullary or extramedullary tibial instruments, to obtain proper axial alignment. In cases where retained hardware is present, or in patients with knee osteoarthritis associated with pre-existing femoral or tibial extra-articular deformity, CAOS has proved to be an exceptionally useful, effective, and appealing option.27–37 A portable, accelerometer-based navigation device (OrthAlign, OrthAlign Inc., Aliso Viejo, CA) for TKA has demonstrated promising results with regard to the alignment accuracy of large-console CAOS systems.10–14
We present three patients who underwent TKA with retained femoral hardware. Two patients had intramedullary femoral fixation and one patient had an interference screw from a previous anterior cruciate ligament (ACL) reconstruction that would interfere with the use of a conventional intramedullary alignment guide. A novel, portable, accelerometer-based navigation (OrthAlign® precision alignment system, OrthAlign Inc., Aliso Viejo, CA) guide enabled performance of TKA without the need for surgical removal of hardware.
Case Reports
Case #1
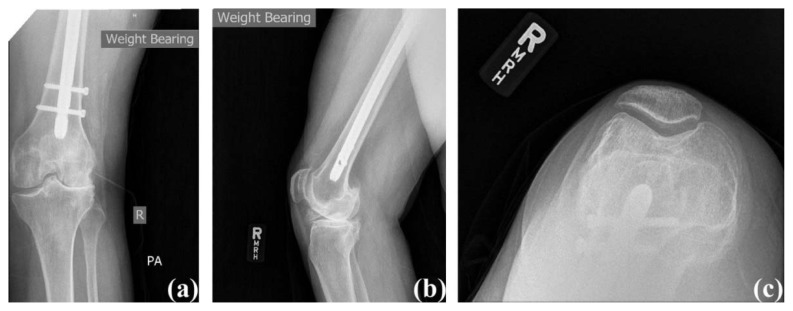
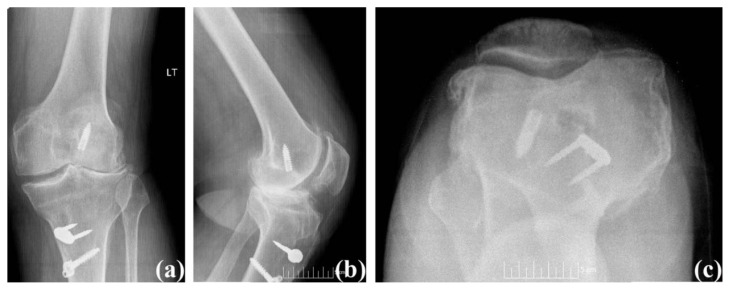
A 52-year-old female (Body Mass Index (BMI): 35.1 kg/m2) presented with a chief complaint of right knee pain (Knee Society Score: 57 and functional Knee Society Score: 50). She had a remote history of right intertrochanteric hip fracture treated surgically with a long antegrade cephalomedullary fixation nail. Her fracture proceeded to union, and she was able to bear full weight on the affected extremity. Since her previous surgery, however, she developed anterior and lateral right knee pain accompanied by crepitation. Rest, ice, heat, nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen were used to control her pain but were not successful. Physical examination of her right knee showed correctable valgus deformity and tenderness to palpation both anteriorly and laterally. Her active range of motion was from 0° to 110° of flexion, and she had a mild effusion with crepitus throughout a range of motion. Radiographs showed patellofemoral and lateral compartment joint space narrowing, subchondral sclerosis, and osteophyte formation (Figure 1). The presence of a long antegrade cephalomedullary nail with two distal interlocking screws also was noted.
Figure 1.
Case #1 pre-operative radiographs: (a) anterior posterior view, (b) lateral view, and (c) sunrise view.
Given the presence of the long antegrade cephalomedullary fixation nail, a decision was made to use the OrthAlign® precision alignment system to assist in positioning the bone cuts to obviate the need to extract the femoral hardware prior to TKA. During surgery, a standard midline incision was used with a medial parapatellar arthrotomy. Surgery proceeded as usual with the addition of the use of the OrthAlign® precision alignment system to determine the femoral and tibial cuts. The Movation™ system (DJO, LLC, Vista, CA), a posterior stabilized knee system, with femoral size 4, tibia base plate size 2, patella size 32, and an 11 mm posterior, stabilized polyethylene insert was used. Palacios bone cement with vancomycin also was used. Surgical course was without complication. Total tourniquet time was 41 minutes at 300 mmHg.
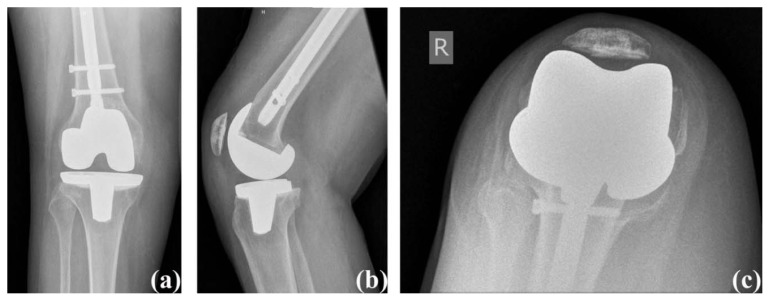
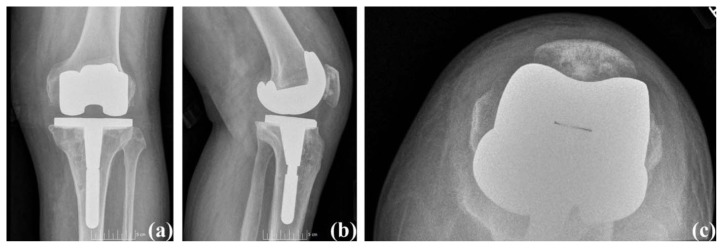
Her post-operative course was without complication. She was mobilized and ambulated with physical therapy. She was discharged home on post-operative day two with a prescription for outpatient physical therapy. At six weeks post-operatively, her incision had healed without any complications, her passive range of motion was 0° – 125° and was pain free (Knee Society Score: 100 and functional Knee Society Score: 85). Her knee was stable on exam and well-aligned, radiographically (Figure 2). She was walking unlimited distances with a cane, and she was using stairs in a reciprocal manner. Her next follow-up visit was scheduled for six months after surgery.
Figure 2.
Case #1 post-operative radiographs: (a) anterior posterior view, (b) lateral view, and (c) sunrise view.
Case #2
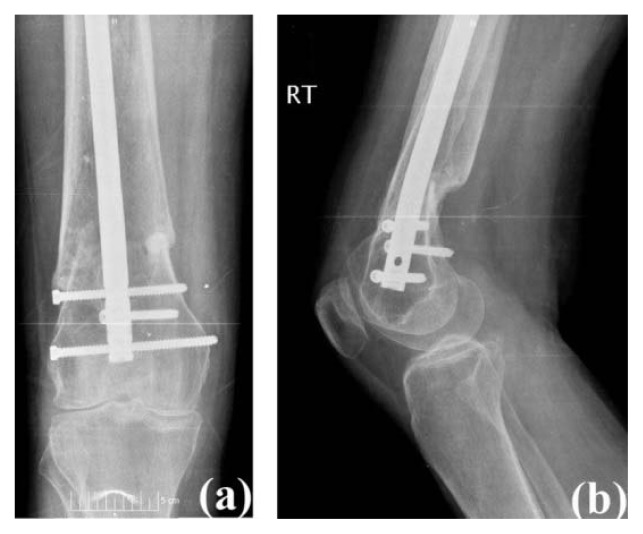
A 62-year-old female (BMI: 20.8 kg/m2) presented with a chief complaint of right knee pain (Knee Society Score: 52 and functional Knee Society Score: −10). She was a poly-trauma victim, suffering a boating accident ten months prior. She sustained numerous fractures including the spine, pelvis, femur, ankle, and clavicle which required open reduction and internal fixation. Her right femur was treated with a retrograde femoral nail with three distal interlocking screws. Despite the treatment, her right knee pain progressively had been worsening, and was associated with crepitus throughout her range of motion. The use of stairs, as well as prolonged standing and walking, exacerbated her pain. Her pain had not been relieved with conservative treatment measures, or corticosteroid injections. She also noted some discomfort over the two lateral-to-medial distal interlocking screws and requested that these be removed during surgery. Physical examinations revealed a correctable varus deformity of the right knee and active range of motion was from 10° to 105°, accompanied by crepitation. A moderate effusion also was noted along with tenderness along the medial joint line. Radiographs showed a healed fracture of the distal femur at the metaphyseal-diaphyseal junction, and a retrograde femoral nail is visualized with two proximal and three distal interlocking screws (Figure 3).
Figure 3.
Case #2 pre-operative radiographs: (a) anterior posterior view and (b) lateral view.
The presence of the retrograde femoral nail precluded the use of a conventional intramedullary alignment guide. Therefore, navigation-assisted TKA was performed. The two symptomatic distal interlocking screws were removed percutaneously. The Donjoy© surgical foundation cruciate retaining (CR) knee system with femoral size 6, tibia base plate size 4, patella size 32, and an 11 mm standard CR polyethylene insert was used. Surgical course was without complication. Total tourniquet time was 48 minutes at 300 mmHg.
The patient was discharged to skilled nursing on post-operative day two for continued physical therapy for approximately two weeks after surgery. She was dismissed home with a prescription for outpatient physical therapy. At six weeks post-operatively, her active range of motion was from 0° to 125° and pain free (Knee Society Score: 100 and functional Knee Society Score: 90). Radiographs showed well-aligned components and restored mechanical axis (Figure 4). She was walking unlimited distances without any assistive device and using stairs in a reciprocal manner with a rail. Her follow-up visit was scheduled for six months after surgery.
Figure 4.
Case #2 post-operative radiographs: (a) anterior posterior view, (b) lateral view, and (c) sunrise view.
Case #3
A 60-year-old male (BMI: 31.0 kg/m2) presented with a chief complaint of left knee pain. The patient sustained an ACL rupture while playing sports 20 years prior and subsequently underwent an ACL reconstruction. He presented with anterior and lateral left knee pain that was dull, aching, and throbbing, and it progressively had been worsening (Knee Society Score: 56 and functional Knee Society Score: 50). His pain had not been relieved with conservative treatment measures, or corticosteroid injections. Physical examination revealed a 5° valgus deformity with range of motion from 5° to 120° of flexion accompanied by crepitation on lateral and patellofemoral compartment, as well as tenderness to palpation. He was limited to ambulating two to five blocks at a time, and the use of stairs as well as prolonged standing and walking exacerbated the pain. Radiographs showed loss of lateral and patellofemoral compartment joint space with significant sclerosis, osteophyte formation, and retained screws in both the femur and tibia as well as a staple in the tibia from previous ACL reconstruction (Figure 5).
Figure 5.
Case #3 pre-operative radiograph: (a) anterior posterior view, (b) lateral view, and (c) sunrise view.
During surgery, it was determined that the tibial screw and staple would need to be removed for placement of the tibial component, and removal of the screw and staple were incorporated as part of the patient’s standard midline incision and medial parapatellar arthrotomy. Given the presence of the femoral interference screw, the navigation-assisted system was used to assist in making accurate bony cuts, orient the implants, assess the soft tissue balancing, and to obviate the need for the screw removal prior to TKA. A posterior stabilized implant was employed, and after making the box cut on the femoral side, the interference screw was protruding about 1 cm into the femoral box; therefore, it was removed. The Movation™ system (DJO, LLC, Vista, CA), a posterior stabilized system with femoral size 8, tibia base plate size 8, patella size 35, and a 9 mm posterior stabilized polyethylene insert and 14 mm tibial modular stem were used. The remainder of the surgical course was without complication. Total tourniquet time was 63 minutes at 300 mmHg.
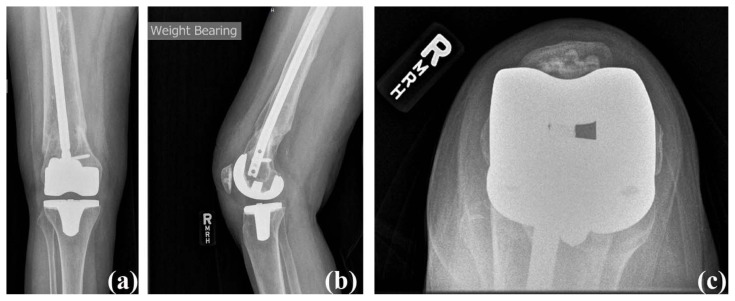
At six weeks post-operatively, his knee range of motion was from 0° to 130° of flexion and pain free (Knee Society Score: 100 and functional Knee Society Score: 90). Radiographs showed well-aligned components and restored mechanical axis (Figure 6). He was walking unlimited distances without any assistive device, and he was using stairs in a reciprocal manner with a rail. His follow-up visit was scheduled for six months after surgery.
Figure 6.
Case #3 Post-Operative Radiographs. (a) Anterior posterior view, (b) Lateral view, and (c) Sunrise view.
Discussion
CAOS can be an effective tool to align TKA component and produce accurate restoration of the biomechanical axis consistently for cases when traditional instrumentation is not possible or appropriate due to posttraumatic femoral deformity, retained femoral hardware, a history of osteomyelitis, or severe cardiopulmonary disease.27–37 In this report, the rationale for the use of navigation-assisted systems in these three cases was appropriate because they allowed establishment of the biomechanical axis and did not require hardware removal. The use of navigation-assisted system had no adverse impact on the patient’s total time in the operating room or tourniquet time. The post-operative course was not adversely affected, and all three patients’ pain and function were improved at six-week follow-up.
Based on these results, navigation-assisted systems present physicians with an effective option for performing TKA in patients with pre-existing hardware. It obviated the need for a prior surgery to remove the retained implant, saving the patient the risk and subsequent morbidity of a second surgery and conceivably improving patient rehabilitation and outcomes. Furthermore, it also reduced the cost to the patient and the health care system through decreased number of surgeries and total operating room time. Although long-term follow-up was not available, the postoperative course was uneventful. Further research using randomized, prospective studies would be beneficial to compare outcomes in single-stage TKA using navigation-assisted versus two-stage surgery with hardware removal.
In summary, navigation-assisted TKAs with retained femoral hardware were successful and safe. The advantages of the navigated-assisted TKA for normal cases remain a matter of debate, however, navigation-assisted TKA was an excellent alternative for hardware retaining cases.
Acknowledgement
The authors wish to thank Dr. George Lucas for his assistance, revision and critical comments on the paper.
Footnotes
Conflict of Interest Statement
This study uses the OrthAlign® precision alignment system from OrthAlign Inc. (Aliso Viejo, CA). However, OrthAlign Inc. had no role in the collection, analysis and interpretation of data, writing of the manuscript, or decision to submit the manuscript for publication. This study did not receive any payments or other personal benefits or a commitment or agreements that were related in any way to the subject of the current research project.
References
- 1.Molli RG, Anderson KC, Buehler KC, Markel DC. Computer-assisted navigation software advancements improve the accuracy of total knee arthroplasty. J Arthroplasty. 2011;26(3):432–438. doi: 10.1016/j.arth.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Blakeney WG, Khan RJ, Wall SJ. Computer-assisted techniques versus conventional guides for component alignment in total knee arthroplasty: A randomized controlled trial. J Bone Joint Surg Am. 2011;93(15):1377–1384. doi: 10.2106/JBJS.I.01321. [DOI] [PubMed] [Google Scholar]
- 3.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Anderson KC, Buehler KC, Markel DC. Computer assisted navigation in total knee arthroplasty: Comparison with conventional methods. J Arthroplasty. 2005;20(7 Suppl 3):132–138. doi: 10.1016/j.arth.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Confalonieri N, Manzotti A, Pullen C, Ragone V. Computer-assisted technique versus intramedullary and extramedullary alignment systems in total knee replacement: A radiological comparison. Acta Orthop Belg. 2005;71(6):703–709. [PubMed] [Google Scholar]
- 6.Belvedere C, Ensini A, Leardini A, Bianchi L, Catani F, Giannini S. Alignment of resection planes in total knee replacement obtained with the conventional technique, as assessed by a modern computer-based navigation system. Int J Med Robot. 2007;3(2):117–124. doi: 10.1002/rcs.131. [DOI] [PubMed] [Google Scholar]
- 7.Manzotti A, Pullen C, Confalonieri N. Computer-assisted alignment system for tibial component placement in total knee replacement: A radiological study. Chir Organi Mov. 2008;91(1):7–11. doi: 10.1007/s12306-007-0002-7. [DOI] [PubMed] [Google Scholar]
- 8.Pang CH, Chan WL, Yen CH, et al. Comparison of total knee arthroplasty using computer-assisted navigation versus conventional guiding systems: A prospective study. J Orthop Surg (Hong Kong) 2009;17(2):170–173. doi: 10.1177/230949900901700209. [DOI] [PubMed] [Google Scholar]
- 9.Cheng T, Zhao S, Peng X, Zhang X. Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1307–1322. doi: 10.1007/s00167-011-1588-8. [DOI] [PubMed] [Google Scholar]
- 10.Nam D, Weeks KD, Reinhardt KR, Nawabi DH, Cross MB, Mayman DJ. Accelerometer-based, portable navigation vs imageless, large-console computer-assisted navigation in total knee arthroplasty: A comparison of radiographic results. J Arthroplasty. 2013;28(2):255–261. doi: 10.1016/j.arth.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 11.Nam D, Jerabek SA, Haughom B, Cross MB, Reinhardt KR, Mayman DJ. Radiographic analysis of a hand-held surgical navigation system for tibial resection in total knee arthroplasty. J Arthroplasty. 2011;26(8):1527–1533. doi: 10.1016/j.arth.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Nam D, Nawabi DH, Cross MB, Heyse TJ, Mayman DJ. Accelerometer-based computer navigation for performing the distal femoral resection in total knee arthroplasty. J Arthroplasty. 2012;27(9):1717–1722. doi: 10.1016/j.arth.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Nam D, Cross M, Deshmane P, Jerabek S, Kang M, Mayman DJ. Radiographic results of an accelerometer-based, handheld surgical navigation system for the tibial resection in total knee arthroplasty. Orthopedics. 2011;34(10):e615–621. doi: 10.3928/01477447-20110826-12. [DOI] [PubMed] [Google Scholar]
- 14.Nam D, Cody EA, Nguyen JT, Figgie MP, Mayman DJ. Extramedullary guides versus portable, accelerometer-based navigation for tibial alignment in total knee arthroplasty: A randomized, controlled trial: Winner of the 2013 HAP PAUL award. J Arthroplasty. 2014;29(2):288–294. doi: 10.1016/j.arth.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK. Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplasty. 2012;27(6):1177–1182. doi: 10.1016/j.arth.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 16.Huang TW, Lee CY, Lin SJ, et al. Comparison of computer-navigated and conventional total knee arthroplasty in patients with Ranawat type-II valgus deformity: Medium-term clinical and radiological results. BMC Musculoskelet Disord. 2014;15:390. doi: 10.1186/1471-2474-15-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moskal JT, Capps SG, Mann JW, Scanelli JA. Navigated versus conventional total knee arthroplasty. J Knee Surg. 2014;27(3):235–248. doi: 10.1055/s-0033-1360659. [DOI] [PubMed] [Google Scholar]
- 18.Roberts TD, Clatworthy MG, Frampton CM, Young SW. Does computer assisted navigation improve functional outcomes and implant survivability after total knee arthroplasty? J Arthroplasty. 2015;30(9 Suppl):59–63. doi: 10.1016/j.arth.2014.12.036. [DOI] [PubMed] [Google Scholar]
- 19.de Steiger RN, Liu YL, Graves SE. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am. 2015;97(8):635–642. doi: 10.2106/JBJS.M.01496. [DOI] [PubMed] [Google Scholar]
- 20.Schnurr C, Güdden I, Eysel P, König DP. Influence of computer navigation on TKA revision rates. Int Orthop. 2012;36(11):2255–2260. doi: 10.1007/s00264-012-1606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim YH, Park JW, Kim JS. Computer-navigated versus conventional total knee arthroplasty a prospective randomized trial. J Bone Joint Surg Am. 2012;94(22):2017–2024. doi: 10.2106/JBJS.L.00142. [DOI] [PubMed] [Google Scholar]
- 22.Rebal BA, Babatunde OM, Lee JH, Geller JA, Patrick DA, Jr, Macaulay W. Imageless computer navigation in total knee arthroplasty provides superior short term functional outcomes: A meta-analysis. J Arthroplasty. 2014;29(5):938–944. doi: 10.1016/j.arth.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Lützner J, Günther KP, Kirschner S. Functional outcome after computer-assisted versus conventional total knee arthroplasty: A randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1339–1344. doi: 10.1007/s00167-010-1153-x. [DOI] [PubMed] [Google Scholar]
- 24.Tolk JJ, Koot HW, Janssen RP. Computer navigated versus conventional total knee arthroplasty. J Knee Surg. 2012;25(4):347–352. doi: 10.1055/s-0031-1299670. [DOI] [PubMed] [Google Scholar]
- 25.Blakeney WG, Khan RJ, Palmer JL. Functional outcomes following total knee arthroplasty: A randomised trial comparing computer-assisted surgery with conventional techniques. Knee. 2014;21(2):364–368. doi: 10.1016/j.knee.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 26.Yaffe M, Chan P, Goyal N, Luo M, Cayo M, Stulberg SD. Computer-assisted versus manual TKA: No difference in clinical or functional outcomes at 5-year follow-up. Orthopedics. 2013;36(5):e627–632. doi: 10.3928/01477447-20130426-26. [DOI] [PubMed] [Google Scholar]
- 27.Hernandez-Vaquero D, Suarez-Vazquez A, Iglesias-Fernandez S. Computer-assisted navigation in total knee arthroplasty without femoral hardware removal. Acta Chir Orthop Traumatol Cech. 2012;79(4):331–324. [PubMed] [Google Scholar]
- 28.Tigani D, Masetti G, Sabbioni G, Ben Ayad R, Filanti M, Fosco M. Computer-assisted surgery as indication of choice: Total knee arthroplasty in case of retained hardware or extra-articular deformity. Int Orthop. 2012;36(7):1379–1385. doi: 10.1007/s00264-011-1476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamada D, Egawa H, Goto T, et al. Navigation-assisted total knee arthroplasty for osteoarthritis with extra-articular femoral deformity and/or retained hardware. Case Rep Orthop. 2013;2013:174384. doi: 10.1155/2013/174384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Catani F, Digennaro V, Ensini A, Leardini A, Giannini S. Navigation-assisted total knee arthroplasty in knees with osteoarthritis due to extra-articular deformity. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):546–551. doi: 10.1007/s00167-011-1602-1. [DOI] [PubMed] [Google Scholar]
- 31.Kuo CC, Bosque J, Meehan JP, Jamali AA. Computer-assisted navigation of total knee arthroplasty for osteoarthritis in a patient with severe posttraumatic femoral deformity. J Arthroplasty. 2011;26(6):976.e17–20. doi: 10.1016/j.arth.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 32.Lin SY, Chen CH, Huang PJ, Fu YC, Huang HT. Computer-navigated minimally invasive total knee arthroplasty for patients with retained implants in the femur. Kaohsiung J Med Sci. 2014;30(8):415–421. doi: 10.1016/j.kjms.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 33.Manzotti A, Chemello C, Pullen C, Cerveri P, Confalonieri N. Computer-assisted total knee arthroplasty after prior femoral fracture without hardware removal. Orthopedics. 2012;35(10 Suppl):34–39. doi: 10.3928/01477447-20120919-55. [DOI] [PubMed] [Google Scholar]
- 34.Shao J, Zhang W, Jiang Y, et al. Computer-navigated TKA for the treatment of osteoarthritis associated with extra-articular femoral deformity. Orthopedics. 2012;35(6):e794–799. doi: 10.3928/01477447-20120525-15. [DOI] [PubMed] [Google Scholar]
- 35.Mullaji A, Shetty GM. Computer-assisted total knee arthroplasty for arthritis with extra-articular deformity. J Arthroplasty. 2009;24(8):1164–1169.e1. doi: 10.1016/j.arth.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 36.Klein GR, Austin MS, Smith EB, Hozack WJ. Total knee arthroplasty using computer-assisted navigation in patients with deformities of the femur and tibia. J Arthroplasty. 2006;21(2):284–288. doi: 10.1016/j.arth.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 37.Fehring TK, Mason JB, Moskal J, Pollock DC, Mann J, Williams VJ. When computer-assisted knee replacement is the best alternative. Clin Orthop Relat Res. 2006;452:132–136. doi: 10.1097/01.blo.0000229363.50361.25. [DOI] [PubMed] [Google Scholar]