Abstract
Purpose
Recent national trends show decelerating declines in heart disease mortality, especially among younger adults. National trends may mask variation by geography and age. We examined recent county-level trends in heart disease mortality by age group.
Methods
Using a Bayesian statistical model and National Vital Statistics Systems data, we estimated overall rates and percent change in heart disease mortality from 2010 through 2015 for four age groups (35–44, 45–54, 55–64, and 65–74 years) in 3098 US counties.
Results
Nationally, heart disease mortality declined in every age group except ages 55–64 years. County-level trends by age group showed geographically widespread increases, with 52.3%, 58.5%, 69.1%, and 42.0% of counties experiencing increases with median percent changes of 0.6%, 2.2%, 4.6%, and −1.5% for ages 35–44, 45–54, 55–64, and 65–74 years, respectively. Increases were more likely in counties with initially high heart disease mortality and outside large metropolitan areas.
Conclusions
Recent national trends have masked local increases in heart disease mortality. These increases, especially among adults younger than age 65 years, represent challenges to communities across the country. Reversing these trends may require intensification of primary and secondary prevention—focusing policies, strategies, and interventions on younger populations, especially those living in less urban counties.
Keywords: Heart diseases, Geography, Mortality decline, Mortality rates, Age groups
Introduction
Over the past 40 years, heart disease mortality in the United States has declined sharply across race, gender, and age groups [1,2], with similarly strong declines occurring at the county level [3,4]. Recent national trends, however, indicate a slowing and even slight increase in heart disease mortality [5–7]. These slowing declines appear to be the most prominent among young adults [2,6], a group that has also recently experienced increased all-cause and stroke mortality [8–10].
Prior studies of age-specific declines in heart disease mortality in the United States have focused on national trends, potentially masking changes in local age-specific patterns. Local trends, which have historically been strong but varied [3,4], can provide important insights into potential drivers of population shifts in heart disease mortality and inform the development of tailored interventions. Therefore, using a period of marked leveling of national declines (2010–2015) [5], we examined recent county-level heart disease mortality trends by age group.
Methods
We obtained annual counts of county-level heart disease deaths during 2010–2015 from the National Vital Statistics System. Deaths with underlying causes of “diseases of the heart” were identified with the International Classification of Diseases, 10th revision (ICD-10) (codes I00–I09, I11, I13, I20–I51), including: rheumatic heart disease, hypertensive heart disease, ischemic heart disease, and pulmonary heart disease. The study population included residents of the 3098 counties in the continuous US, ages 35–74 years, stratified by age group (35–44, 45–54, 55–64, and 65–74 years). We chose this age range to reflect premature, largely avoidable, deaths due to heart disease [11]. All counties were included. We used US Census intercensal estimates for annual county-level population counts [12].
We estimated the rates of heart disease mortality using a Bayesian multivariate space-time conditional autoregressive model. Details of this model have been previously described [13]. Briefly, this model is based on the popular Besag-York-Mollié conditional autoregressive model for spatially referenced count data [14]. It incorporates correlation across space, time, and age group. By iteratively estimating parameters and borrowing strength from spatially, temporally, and age-adjacent groups, these models generate precise, reliable rates even in the presence of small case counts and small populations [3,13]. We fit this model with a Markov chain Monte Carlo (MCMC) algorithm using user-developed code in the R programming language.
We estimated national and county-level heart disease mortality rates for all ages (ages 35–74 years combined) and each age group as the medians of the posterior distributions defined by the MCMC iterations. National values for rates and percent change were calculated using the sums of county-specific deaths and populations, and are therefore skewed toward high population counties. To describe the distribution of rates and percent change across counties, we report median county-level values, which are unweighted by county populations. National and county-specific overall rates for ages 35–74 years combined were age-standardized to the 2000 US standard population.
We estimated relative percent change in national and county-level rates from 2010 through 2015 using Poisson regression, rather than using differences in rates between 2010 and 2015. Using rates generated by each MCMC iteration, separate regression models were run for each county using rates for all 6 years for the given county. Relative percent change was calculated as 100 (e5β−1), where β is the county-specific (or national) median coefficient for the year variable from the MCMC iterations, and five represents number of between-year intervals in the study period.
To further explore geographic and spatial patterns, we mapped relative percent change in mortality rates and 2015 mortality rates by county. Moreover, we compared percent change across quintiles of county-level heart disease mortality in 2010 and across urban/rural status using the National Center for Health Statistics’ 2013 urban-rural classification scheme [15].
Results
Nationally, from 2010 to 2015, age-standardized heart disease mortality for ages 35–74 years declined slightly with a percent change of −1.6% (133.0 to 130.9 per 100,000 in 2010 and 2015, respectively) (Table 1). Nationally, rates slightly declined among adults at ages 35–44, 45–54, and 65–74 years, and increased among adults at ages 55–64 years.
Table 1.
National and county-level heart disease mortality rates and percent change over time, by age group, United States, 2010–2015
| Summary statistic | Ages 35–44 years | Ages 45–54 years | Ages 55–64 years | Ages 65–74 years | Ages 35–74 years* |
|---|---|---|---|---|---|
| National | |||||
| 2010 rate (per 100,000) (95% credible interval) | 27.0 (26.6–27.5) | 84.8 (84.0–85.7) | 191.0 (189.6–192.3) | 415.6 (413.2–417.9) | 133.0 (132.3–133.6) |
| 2015 rate (per 100,000) (95% credible interval) | 27.1 (26.7–27.5) | 82.7 (81.7–83.4) | 194.6 (193.4–195.8) | 400.7 (397.7–402.6) | 130.9 (130.2–131.5) |
| Percent change‡ (95% credible interval) | −0.8 (−2.5 to 0.8) | −1.7 (−0.5 to 2.8) | 2.0 (0.4–3.7) | −3.8 (−6.3 to −1.2) | −1.6 (−3.3 to 0.0) |
| County-level† | |||||
| 2010 rate (per 100,000) (interquartile range) | 28.9 (21.9–40.7) | 90.5 (69.0–125.6) | 201.0 (158.5–262.1) | 438.2 (359.5–530.2) | 140.4 (113.3–180.0) |
| 2015 rate (per 100,000) (interquartile range) | 29.3 (21.8–41.7) | 92.2 (69.4–127.7) | 208.9 (162.0–278.2) | 431.5 (347.8–530.3) | 142.8 (112.1–185.3) |
| Percent change‡ (interquartile range) | 0.6 (−7.4 to 9.1) | 2.2 (−3.9 to 8.2) | 4.6 (−1.5 to 11.4) | −1.5 (−6.6 to 4.0) | 1.0 (−4.1 to 6.3) |
Age standardized to the 2000 US population.
Median county-level rates and percent change are determined from the age-group–specific distribution of county-level rates and percent change. They differ from the national rates and percent change because they are not population weighted.
Percent change was calculated using Poisson regression across all years.
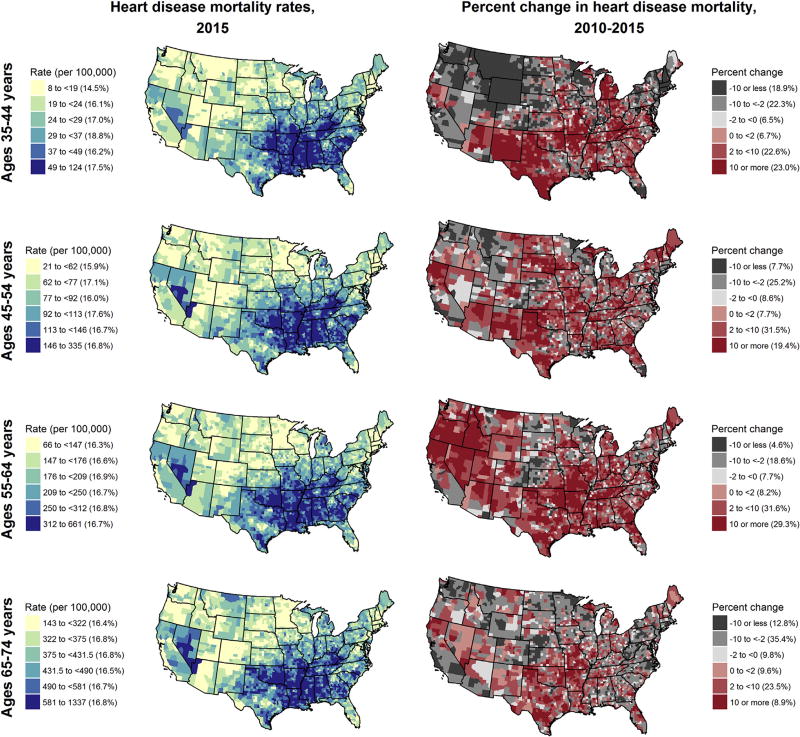
In contrast to the national trends, at the county-level, from 2010 through 2015, the majority of counties experienced increases in heart disease mortality rates: 52.3%, 58.5%, and 69.1% of all counties among ages 35–44, 45–54, and 55–64 years, respectively (Table 2). Even in the oldest age group (65–74 years), 42.0% of the counties experienced increases. The magnitudes of the increases varied by age group, with roughly 1 in 5 counties in the 3 youngest age groups experiencing an increase of at least 10% (23.0%, 19.4%, and 29.3% of all counties among ages 35–44, 45–54, and 55–64 years, respectively; Fig. 1).
Table 2.
Percent of counties experiencing increasing heart disease mortality, by age group, United States, 2010–2015
| County classification | Ages 35–44 years | Ages 45–54 years | Ages 55–64 years | Ages 65–74 years | Ages 35–74 years* |
|---|---|---|---|---|---|
| Overall | 52.3% | 58.5% | 69.1% | 42.0% | 54.5 |
| Quintile of 2010 rates | |||||
| Lowest rates (first quintile) | 42.9 | 58.2 | 64.5 | 37.9 | 46.1 |
| Second quintile | 45.2 | 60.7 | 60.4 | 36.5 | 48.1 |
| Third quintile | 53.1 | 59.4 | 64.0 | 43.5 | 53.9 |
| Fourth quintile | 57.8 | 56.9 | 76.6 | 45.6 | 62.2 |
| Highest rates (Fifth quintile) | 62.4 | 57.3 | 80.0 | 46.5 | 62.3 |
| 2013 NCHS urban/rural classification | |||||
| Large central metro (most urban) | 40.6 | 34.4 | 50.0 | 20.3 | 31.3 |
| Large fringe metro | 53.6 | 47.3 | 66.8 | 32.1 | 46.4 |
| Medium metro | 55.8 | 61.8 | 71.3 | 42.8 | 56.1 |
| Small metro | 53.6 | 60.7 | 72.2 | 47.5 | 59.0 |
| Nonmetropolitan | 52.0 | 62.4 | 68.5 | 43.7 | 56.2 |
| Noncore (most rural) | 48.2 | 52.4 | 69.3 | 38.9 | 51.3 |
Age standardized to the 2000 US population.
Fig. 1.
County-level heart disease mortality rates* and percent change† by age group, United States, 2010–2015. *Heart disease death rates for 2015 are categorized by sextiles based on the distribution of county rates for each age group. †Percent change in heart disease death rates are categorized using a common classification across age groups. The percent of counties within each category is shown in parentheses in the legend.
With the exception of ages 45–54 years, increasing rates were most prevalent among counties with the highest rates in 2010 (62.4%, 80.0%, and 46.5% of counties in the top quintile of 2010 heart disease mortality for ages 35–44, 55–64, and 65–74 years, respectively, compared with 42.9%, 69.1%, and 42.0% of counties in the bottom quintile) (Table 2). For ages 35–74 years combined, 62.3% of counties in the top quintile of rates in 2010 experienced increases, compared to 46.1% of counties in the bottom quintile of 2010 rates.
All age groups exhibited similar spatial patterns of county-level heart disease mortality rates in 2015, with the highest rates concentrated in a band stretching from Georgia through Oklahoma and extending through Appalachia (Fig. 1). Spatial patterns of increasing heart disease mortality were generally dispersed throughout the United States and not confined to counties with the highest rates. These patterns varied somewhat across age groups. However, increasing heart disease mortality rates varied markedly by urban-rural status (Table 2). Across all age groups, increasing rates were least prevalent in large central metro counties (40.6%, 34.4%, 50.0%, and 20.3% for ages 35–44, 55–64, and 65–74 years, respectively). Increasing rates were most prevalent in counties outside of large metropolitan areas, where, for all age groups except ages 65–74 years, a majority of counties experienced increasing heart disease mortality.
Discussion
This study of county-level trends in heart disease mortality from 2010 to 2015 reveals geographically dispersed, local increases across age groups. These trends, which have been masked in prior studies using national data and wider age groups [2,6], vary in magnitude across counties and age groups. However, given the strong, consistent declines that have occurred since the 1970s, any leveling or increase in heart disease mortality is noteworthy [4,5]. Our findings suggest that the warnings issued about the potential implications of stagnating heart disease mortality among young adults during the latter part of the last century appear to have come to fruition [16], with over 50% of counties experiencing increases in heart disease mortality from 2010 through 2015 among adults aged 35–64 years. These county-level increases in heart disease mortality occurred within the context of increases in the prevalence of obesity and diabetes over the past 2 decades [17,18], and recent increases in national all-cause and stroke mortality, including increases in similar age groups [8–10]. The observed widespread increases in heart disease mortality among this working-age population are concerning, as these largely avoidable deaths are often attributable to a lack of preventive health care or of timely and effective medical care and to insufficient access to or adoption of heart-healthy behaviors [11].
Given the widespread nature of these increases, three sets of counties are particularly noteworthy. First, for each age group, a large percentage of counties with already high heart disease mortality experienced increases from 2010 through 2015. Should these trends continue, the magnitude of geographic disparity among counties will increase. Second, increases in heart disease mortality were more prevalent outside the large metropolitan areas. Specifically, increases were focused in medium and small metropolitan areas and in rural counties, which could lead to a widening of the urban-rural disparity that began in the mid-2000s [19]. Finally, many counties well outside the belt of high-burden Southern counties [4] experienced increased heart disease mortality, raising questions about the nature and pervasiveness of conditions responsible for increasing heart disease mortality. Are the conditions contributing to increased heart disease mortality similar across regions and across age groups? What can we learn from those resilient counties in which heart disease death rates continued to decline for the various age groups? Given the paucity of county-level risk factor data by age group, answers to these questions are challenging, requiring further study, and the use of novel study designs and data sources.
The common experience of increasing heart disease mortality for many counties throughout the country suggests that reversing these trends will require addressing both primary and secondary prevention of heart disease mortality at the individual, community, state, and national levels. Previous studies have concluded that prevention and treatment are both responsible for past declines [20]. Primary prevention of heart disease includes health-promoting activities that can occur both within and outside of the traditional health care system. The latter may represent an key opportunity for reaching younger, working-age individuals, who may underutilize effective preventive health care [7,21]. A focus of primary prevention on younger adults also represents an opportunity to reduce the cumulative negative effects of heart disease risk factors [22,23]. Similarly, focusing primary prevention efforts outside of large urban counties may be important as populations in these counties often have lower prevalence of healthy behaviors [24].
For secondary prevention of both heart disease events and risk factors, communities and the health care and public health systems may require a renewed focus on the diagnosis and effective treatment of heart disease risk factors, including tobacco use, diabetes, obesity, hypertension, and hyperlipidemia, especially among younger age groups. Enhancing secondary prevention will require younger adults to engage with the health care system, preparing both for the increased health care needs of an aging population. These same efforts, when focused outside of large urban centers, will need to overcome lower access to care in these communities [25,26].
The observed disparities suggest that any proposed solutions to reverse these trends should strive for equity across both geography and age. This may include implementing broader policies and strategies to support heart-healthy lifestyles, such as healthy institutional food procurement, comprehensive tobacco control programs, healthy community designs, and access to and use of effective health care services.
A key strength of this study is its application of a fully Bayesian spatiotemporal model to national surveillance data. By borrowing statistical strength across adjacent counties and years, this model estimates rates that are more precise than other statistical methods, even in counties with small populations and numbers of deaths [3], thereby permitting the inclusion of all counties. In addition, this analysis used national vital statistics data that include all recorded deaths.
A limitation of this study is that these data are based on non-validated death certificates. However, their use for surveillance at the aggregate level is valid [27]. Local variation in reporting heart disease as the underlying cause of death represents a potential source of bias, but using the broad ICD category (diseases of the heart) rather than subgroups or specific diagnoses reduces the potential for this misclassification [27,28].
Conclusions
After over 40 years of declines at the national and county levels, the observed increases in heart disease mortality at the local level and by age group represent a challenge to individuals, communities, and the entire country. Enhanced prevention and treatment efforts tailored to the needs of communities are vital to prevent heart disease mortality, including an enhanced focus for younger, working-age adults, and for less urban areas.
Acknowledgments
The US Centers for Disease Control and Prevention supported this study. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Kramer MR, Valderrama AL, Casper ML. Decomposing black-white disparities in heart disease mortality in the United States, 1973–2010: an age-period-cohort analysis. Am J Epidemiol. 2014;182:302–12. doi: 10.1093/aje/kwv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilmot KA, O’Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: Evidence for stagnation in young adults, especially women. Circulation. 2015;132:997–1002. doi: 10.1161/CIRCULATIONAHA.115.015293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vaughan AS, Kramer MR, Waller LA, Schieb LJ, Greer S, Casper M. Comparing methods of measuring geographic patterns in temporal trends: an application to county-level heart disease mortality in the United States, 1973 to 2010. Ann Epidemiol. 2015;25:329–35. doi: 10.1016/j.annepidem.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casper M, Kramer MR, Quick H, Schieb LJ, Vaughan AS, Greer S. Changes in the Geographic Patterns of Heart Disease Mortality in the United States 1973 to 2010. Circulation. 2016;133:1171–80. doi: 10.1161/CIRCULATIONAHA.115.018663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ma J, Ward EM, Siegel RL, Jemal A. Temporal Trends in Mortality in the United States, 1969–2013. JAMA. 2015;314:1731–9. doi: 10.1001/jama.2015.12319. [DOI] [PubMed] [Google Scholar]
- 6.Sidney S, Quesenberry CP, Jr, Jaffe MG, Sorel M, Nguyen-huynh MN, Kushi LH, et al. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 2016;94612:E1–6. doi: 10.1001/jamacardio.2016.1326. [DOI] [PubMed] [Google Scholar]
- 7.Benjamin E, Blaha M, Chiuve S, Cushman M, Das S, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet. 2017;389:1043–54. doi: 10.1016/S0140-6736(17)30187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112:201518393. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Q, Tong X, Schieb L, Vaughan A, Gillespie C, Wiltz JL, et al. Vital signs: Recent trends in stroke death rates - United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;66:1–7. doi: 10.15585/mmwr.mm6635e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schieb LJ, Greer SA, Ritchey MD, George MG, Casper ML. Vital signs: avoidable deaths from heart disease, stroke, and hypertensive disease - United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2013;62:721–7. [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. US Census populations with bridged race categories. [Accessed January 10, 2017];2016 http://www.cdc.gov/nchs/nvss/bridged_race.htm.
- 13.Quick H, Waller LA, Casper M. A multivariate space-time model for analysing county level heart disease death rates by race and sex. J R Stat Soc Ser C Appl Stat. 2017 https://doi.org/10.1111/rssc.12215. [Epub ahead of print]
- 14.Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Ann Inst Stat Math. 1991;43:1–20. [Google Scholar]
- 15.Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. Vital Heal Stat. 2014;2:1–81. [PubMed] [Google Scholar]
- 16.Lloyd-Jones DM. Slowing progress in cardiovascular mortality rates: you reap what you sow. JAMA Cardiol. 2016;1:29–30. doi: 10.1001/jamacardio.2016.1348. [DOI] [PubMed] [Google Scholar]
- 17.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 18.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314:1021. doi: 10.1001/jama.2015.10029. [DOI] [PubMed] [Google Scholar]
- 19.Kulshreshtha A, Goyal A, Dabhadkar K, Veledar E, Vaccarino V. Urban-rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep. 2014;129:19–29. doi: 10.1177/003335491412900105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 21.Maimaris W, Paty J, Perel P, Legido-Quigley H, Balabanova D, Nieuwlaat R, et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001490. https://doi.org/10.1371/journal.pmed.1001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ritchey MD, Wall HK, Gillespie C, George MG, Jamal A. Million hearts: prevalence of leading cardiovascular disease risk factors - United States, 2005–2012. MMWR Morb Mortal Wkly Rep. 2014;63:462–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PWF, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–8. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 24.Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, et al. Health-related behaviors by urban-rural county classification - United States. MMWR Surveill Summ. 2013;2017:1–8. doi: 10.15585/mmwr.ss6605a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caldwell JT, Ford CL, Wallace SP, Wang MC, Takahashi LM. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health. 2016;106:1463–9. doi: 10.2105/AJPH.2016.303212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGrail MR, Wingrove PM, Petterson SM, Bazemore AW. Mobility of US rural primary care physicians during 2000–2014. Ann Fam Med. 2017;15:322–8. doi: 10.1370/afm.2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coady SA, Sorlie PD, Cooper LS, Folsom AR, Rosamond WD, Conwill DE. Validation of death certificate diagnosis for coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. J Clin Epidemiol. 2001;54:40–50. doi: 10.1016/s0895-4356(00)00272-9. [DOI] [PubMed] [Google Scholar]
- 28.Ives DG, Samuel P, Psaty BM, Kuller LH. Agreement between nosologist and cardiovascular health study review of deaths: Implications of coding differences. J Am Geriatr Soc. 2009;57:133–9. doi: 10.1111/j.1532-5415.2008.02056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]