Abstract
Background: Vasovagal responses associated with acupuncture therapy are relatively uncommon adverse events, occurring in ∼0.02%–7% of treatments. The complex neurocardiovascular reflexes involved in vasovagal responses can induce a range of symptoms such as dizziness, nausea, sweating, bradycardia, hypotension, and, in some cases, syncope or convulsions. Although patients typically recover quickly with proper support, these events may be of concern and anxiety-producing for both patient and provider. Providers need to be well-versed in methods for prevention and treatment of acupuncture-associated vasovagal responses to promote safe practice environments, patient satisfaction and comfort, and cost-effectiveness.
Objectives: To examine the biomedical and Traditional Chinese Medicine mechanisms of vasovagal responses, propose updated terminology, and outline steps for prevention and treatment.
Methods: During an 18-month period, 281 community-style acupuncture treatments were performed on family members of admitted patients and hospital staff members at the University of Minnesota Masonic Children's Hospital. Five (1.8%) treatments resulted in documented acupuncture-associated vasovagal response (AAVR) symptoms.
Results: All 5 patients recovered from their AAVR symptoms after treatment interventions. After recovery, 3 patients reported reductions in their main complaint symptoms; main complaint symptom outcomes were not recorded for the other 2 patients.
Conclusions: As integrative practices become more prevalent in academic institutions and primary care environments, clear communication about, as well as prevention treatment, documentation and reporting of acupuncture-associated adverse events will become increasingly valuable. The authors recommend that clinicians in integrative practice clinical environments consider developing formal AAVR response plans as well as training students, supervising and attending providers, and ancillary staff members to ensure rapid, prepared handling and documentation of AAVR incidents.
Keywords: : vasovagal syncope, vasovagal shock, needle shock, needle sickness, adverse effects, acupuncture therapy
Introduction
Vasovagal reflex responses associated with acupuncture therapy are relatively uncommon adverse events, occurring in ∼0.02%–7% of treatments.1–3 A wide range of symptoms can manifest, including presyncopal symptoms of dizziness, nausea, sweating, pale skin, bradycardia, and, in more severe cases, syncope or convulsions.1–4 Although patients typically recover without lasting effects, the experience may be of concern and anxiety-producing for both patients and providers.
A plethora of terminology is used when referring to vasovagal responses associated with acupuncture treatment. Search terms commonly encountered include needle sickness, needle shock, needle fainting, fainting, reflex fainting, vasovagal response, vasovagal syncope (VVS), vasovagal shock, vasovagal attack, vasomotor reflex, and vasodepressor reflex.1,4–7 This range of terminology poses challenges. Researching this subject in published literature becomes a practice in creative and diligent search queries, as there is no widely accepted single term. There is also the problem of biomedical inaccuracy. For example, the terms syncope and shock refer to different physiologic states; and yet, these terms are often utilized interchangeably when referring to vasovagal responses associated with acupuncture treatment.
Additionally, using words such as needle sickness, needle shock, and needle fainting pose risks for potential negative associations, increased anxiety, and possibly, an increased incidence of adverse reactions. Research has shown that the framing of information in disclosures of potential adverse events associated with medical interventions can affect both the incidence of these adverse events and clinical outcomes.8 This phenomenon, known as the nocebo effect, can modulate the effect of a treatment negatively.8 Pairing pathologic physiologic states (such as sickness), or inaccurate terms (such as shock), with the word needle risks perpetuating worry and fear about the safety of acupuncture and the potential of pain or adverse reactions associated with treatment.
Providers of acupuncture are often faced with supporting patients through fear, needle-phobia, blood/injury phobia, and memories of painful experiences with needles in medical settings. It is estimated that 10% of individuals in medical settings experience fear of needles, resulting in distress and avoidance.9,10 Approximately 3% of the general population experiences pronounced needle-phobia, and blood/injury phobia is also present in ∼3%–4%.10,11 It is estimated that 50% of individuals with needle phobia experience VVS when exposed to needles.9 For patients with blood/injury phobia, seeing blood, sustaining injury, or receiving an invasive medical procedure can result in a phobic response; published literature indicates 80% of these phobic responses include vasovagal presyncope or VVS.11 The language and framing used by providers is an important component of building trust, reducing anxiety, improving outcomes, and possibly, reducing incidence of VVS and other adverse reactions associated with acupuncture treatment, while simultaneously providing sufficient and accurate information in the consent process.8 This is especially important when working with patients who experience pronounced fears or phobias.
As complementary and alternative medicine therapies, such as acupuncture, become more integrated in primary care environments, it is important that providers have an in-depth understanding of, and clear terminology for, communicating about possible adverse events associated with treatment. The current authors propose a new term: acupuncture-associated vasovagal response (AAVR). AAVR is inclusive of the broad range of possible symptoms that can occur in association with the vasovagal reflex. This acronym is used throughout the rest of this article. Additionally, a thorough understanding of the AAVR mechanism, at-risk patient populations, and AAVR prevention and treatment guidelines is imperative; prevention and treatment recommendations are discussed.
Biomedical Mechanism of AAVR
AAVR represents one possible manifestation of VVS, the most prevalent cause of transient loss of consciousness in outpatient clinical settings.5,12 Typically, VVS events are benign, isolated, and spontaneous, and are associated with emotional or orthostatic stressors.5,12 In most individuals, VVS is not caused by complicating cardiovascular, neurologic, genetic, or other pathologies, and, typically, medical intervention is not required or utilized.5,12 An individual might only experience one instance of VVS in his or her life, or might have recurring episodes.12
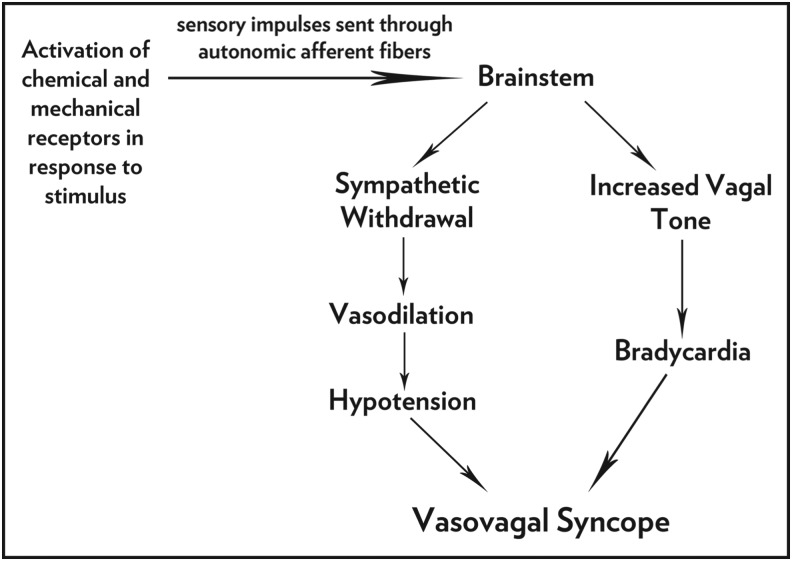
The mechanism of VVS is not completely understood and is highly complex, being characterized by hypotension and bradycardia resulting from a transient withdrawal of sympathetic tone and an increase in vagal tone (Fig. 1).12 Evidence suggests that episodes of VVS result from activation of complex neurocardiovascular reflexes, initiated through stimulation of unidentified peripheral chemical and/or mechanical receptors.5 These receptors relay sensory impulses through autonomic afferent fibers to the cardiovascular control center in the medulla.5 Through the action of central modulatory mechanisms that are still somewhat poorly understood, a sudden vasodilation and a dramatic hypotensive response results, mediated by the efferent autonomic fibers to the vessels and heart.5 As a result, there is a peripheral loss of arterial tone, resulting in bradycardia, or in some instances, prolonged asystolic events or heart blocks.5 Together, bradycardia and hypotension reduce blood flow to the brain quickly, resulting in a loss of consciousness.
FIG. 1.
Vasovagal syncope.
Research has shown that the unidentified neural pathways involved in VVS are likely present in all humans, with individual differences in susceptibility.12 Head-up tilt testing (HUT) is an effective means of assessing individual susceptibility to VVS.12 HUT trials have shown that people in half of the general population will experience spontaneous VVS at some point in their lives, while 40% of the other half will experience VVS only when triggered by pronounced stress or fear.12 A 2001 study examined possible autonomic predisposition to VVS in individuals who experience syncope only when exposed to blood or injury stimuli.11 The study subjects had greater susceptibility to a VVS response in HUT testing, even without the presence of blood or injury stimulus.11 This indicates that these individuals have an autonomic reflex predisposition to VVS and that syncope responses during blood or injury stimulus occur as a result of this underlying dysfunction.11 It is estimated that the autonomic reflex involved with VVS is present in 70% of the general population.12
Orthostatic stress from HUT is just one of the many possible stressors that may trigger the reflex activity involved with VVS.5,12 In most cases of isolated VVS, there will be an identifiable clinical trigger (anxiety, nervousness, fright, pain, sight of blood, some other disturbance, etc.), followed by the onset of presyncope, a set of prodromes or “preliminary warning symptoms” characteristic of sympathetic overactivation.1,5,12 In the case of AAVR, onset of prodromal symptoms is most commonly reported while needles are being inserted or during needle retention, however, published literature shows cases of AAVR onset occurring up to 12 hours post-treatment.4,6,13
Due to the complexity of the neurocardiovascular reflexes involved, a patient can experience a wide range of signs and symptoms. These could include bradycardia, fatigue, lightheadedness, tunnel vision, blurred vision, nausea, vomiting, a feeling of warmth, cold perspiration, yawning, shaking, or general weakness.1,4 Objectively, the provider may note that the patient's complexion becomes pale, the pupils dilate, the pulse is slow and/or weak, and the blood pressure is low.1,4 Without intervention, or in more pronounced cases, a patient might temporarily lose consciousness.1,4 It is also possible, though rarely, that a patient could experience convulsions. Published literature shows 3 case reports of patients experiencing convulsive syncope associated with acupuncture treatment, characterized by a transient loss of consciousness with tonic–clonic movements, batting of the eyelids, and upward rolling of the eyes.2,3 With intervention, the effects of AAVR typically pass quickly, and in most cases, the patient recovers with no lasting effects.4,6,13
In association with acupuncture treatment, it is possible that a patient can experience VVS suddenly and without the typical clinical triggers or prodromes of an AAVR.5,12 While it is possible these individuals could be experiencing benign episodes of syncope, these patients should be examined further and referred as necessary to rule out any complicating and potentially life-threatening causes, such as cardiac or neurologic conditions, dysautonomic disturbances, or treatment-induced adverse events or injuries.1,4–6,12 This is an especially important consideration for elderly patients, who are more at risk for vasovagal events associated with disease pathology.12
Risk of AAVR is increased in cases when patients are nervous or fearful, poorly rested, fatigued, dehydrated, hungry or have not eaten recently, have a weak constitution, or are receiving acupuncture for the first time.4,13 Additionally, strong stimulation from vigorous needling techniques, electrostimulation, or a large needle count, especially with acupuncture-naive patients, can confer additional risks.1,4,13 Patient position during treatment also plays a role. Because acupuncture treatment causes vasodilation and subsequently reduced blood pressure, treating patients in a supine or prone position can help prevent AAVR.4,14
Traditional Chinese Medicine Perspective
Terminology
Several Chinese terms can be used to describe symptoms associated with vasovagal phenomena. The term yūn zhēn (晕针), translated literally as “dizzy needle,” is defined by Wiseman and Feng as “needle sickness” and is characterized by symptoms representative of AAVR.15,16 Two articles in the published literature utilize the Chinese term yun cheng to refer to syncope during acupuncture treatment.3,17 Unfortunately, neither of these articles include Chinese characters, and the term yun cheng is not included in Wiseman and Feng's A Practical Dictionary of Chinese Medicine.15 A similar-sounding term, yùn chǎng (晕场), is defined as “fainting from stress,” but is not specific to acupuncture treatment.18
In a broader sense, the terms yūn dǎo (晕倒) and yūn jué (晕厥) can both be used to describe fainting and/or loss of consciousness.15,19,20 There are subtle differences between the direct translation of these two terms. Dǎo is translated as “inverted” or “counterflow,” whereas jué is translated as “reversal.”15,16 Wiseman and Feng state that the term jué refers to a state of disruption in the flow of Qi and Blood and a decline in the outward spread of Yang Qi.15 In Traditional Chinese Medicine (TCM) diagnostics, reversal patterns (jué zhèng) are identified as conditions that are marked by sudden fainting, loss of consciousness, and/or reversal cold of the limbs.15 Wiseman and Feng note that “counterflow” and “reversal” are closely related, yet differ in that the word “counterflow” is used to describe disruption of the Qi dynamic of Zang Fu, such as the Lung, Liver, or Stomach, and is not used in terminology for the loss of consciousness.15 Jué is also used in the term jué yin, or “reversal” Yin, the meridian classification for the LR and PC. It is in jué yin that the Yin is in its final stage before reverting toward Yang, suggesting the transformation from Internal to External and from Lower to Upper.21
TCM Mechanism of AAVR
TCM physiology and etiology can offer several perspectives on the mechanism of AAVR and the associated symptoms. Wiseman and Feng note nine distinct reversal patterns that are marked by loss of consciousness, eight of which were discussed in the Nei Jing.15 In individuals with excess Liver Yang or dietary irregularities, experiencing acute pain or mental stress can disturb the Qi dynamic and cause it to move in a counterflow direction, influencing the movement of Blood and/or Phlegm toward the orifices of the Heart and resulting in the clouding of the Shen.15 Reversal patterns are also known to occur in cases of insufficient Qi and Blood, such as in individuals with weak Yuan Qi, damage to the bodily substances after prolonged illness or stress, or a loss of blood.15
The circulation of fluid and substances in and around the Zang Fu is regulated in large part through the Triple Energizer (TE) which is more specifically responsible for circulation of Rong (Ying) Qi, or nourishing Qi. Additionally, the TE controls both the Blood and the blood vessels, influencing the activity of these tissues.22 The internal meridian trajectory of the TE moves from ST 12 to CV 17, where it then spreads into the chest and wraps around the Pericardium, spreading through the diaphragm, circulating through the chest, and then moving to the San Jiao. Externally, there is a connection to the PC meridian through TE 5, and PC is considered to be the Yin–Yang couple of the TE. Although the Triple Energizer meridian does not have a corresponding physical organ, the role of the channel is to be the ambassador for the body's Yuan Qi. In this capacity, the TE controls the circulation of Jin Ye, or body fluids including movement between the organs and meridians of the Spleen, Kidney, Stomach, Large Intestine, Small Intestine, and Urinary Bladder. Because of these functions, it is said that TE has an overall connecting function, bringing together all of the organs within the body.22
The analogous physiologic explanation of AAVR invoking the interrelationship of the autonomic nervous system (ANS), with its effects on heart rate and vasodilation/vasoconstriction of the blood vessels supplying the organs is evident. As we know from lower-body, negative pressure studies during vasovagal responses, renal vascular resistance does not change but regional vascular responses in the splanchnic beds of other organs shows vasoconstriction—an activity easily ascribed to the TE.23,24
Methods
Treatment Format and Environment
In partnership with Northwestern Health Sciences University (NWHSU), student interns perform acupuncture treatments on family members of admitted pediatric patients and hospital staff at the University of Minnesota Masonic Children's Hospital (UMMCH).
Treatments are conducted in a community-style format in a family lounge located in the hospital. During these community-style acupuncture sessions, patients are seated in a common space in comfortable, padded chairs or couches, with the patients' feet elevated on footstools. Patients are fully clothed during treatments. Student interns perform patient intakes to gather relevant information on each patient's condition in order to make an appropriate differential diagnosis and develop a treatment strategy. The acupoints most often selected for treatment are distal to the knees and elbows, as well as on the neck, head, and ears. The details of patient encounters are maintained in secured patient charts. These paper charts are updated when patients are interviewed, diagnoses are made, protocols are noted, and treatments are performed.
During an 18-month period, (from May 6, 2015, to October 12, 2016, 281 community-style acupuncture treatments were performed on family members of admitted patients and on hospital staff. All patients gave informed consent. A retrospective chart review was approved through the institutional review board (IRB) process at the University of Minnesota (IRB #1611E99783). Criteria for inclusion in the current analysis were documented onset of AAVR symptoms during needling or needle retention that resulted in treatment alteration or termination, and/or additional intervention; based on this criteria, no cases were excluded. The NWHSU clinical supervisor was interviewed for details in cases for which written documentation did not reveal specifics.
AAVR Case Studies
Results of the retrospective chart review revealed that five treatments resulted in documented AAVR symptoms (Table 1).
Table 1.
Case History Patients with AAVR Symptoms
| Age/gender | Main complaint symptoms | New to acupuncture treatment | Punctured sites | Patient position | Time of AAVR onset | AAVRs | Outcome |
|---|---|---|---|---|---|---|---|
| 46/F | Shoulder and neck pain and tension | Yes | Bilateral GB 20, GB 21, LI 4, ST 36, SP 6, LR 8, KI 3 & LR 3 | Sitting | After inserting last needle | Sweat, pale complexion, dizziness | Patient recovered, symptoms reduced |
| 53/F | Lumbago, acute back sprain | Yes | Bilateral auricular BFA protocol (Cingulate Gyrus, Thalamus, Omega 2, Point Zero & Shen Men) & UB 62 | Sitting | While inserting needles | Sweat, pale complexion, dizziness | Patient recovered, symptoms reduced |
| 38/M | Stress, acid reflux, digestive irregularity | Unknown | EX-HN 3 (YinTang), bilateral LI 4, ST 36, ST 44 & LR 3 | Sitting | After inserting last needle | Dizziness | Patient recovered, no symptom outcome measure recorded |
| 32/F | Headache, upper-back tension, shoulder pain | Yes | Bilateral GB 20, LI 4, ST 36 & LR 3 | Sitting | During needle retention | Dizziness | Patient recovered, no symptom outcome measure recorded |
| 52/F | Headache, shoulder tension | Unknown | Bilateral auricular Shen Men & Spleen; GB 20, GB 21, GB 8, LI 4, ST 36 & LR 3 | Sitting | After inserting last needle | Nausea, “glossy” feeling | Patient recovered, symptoms reduced |
AAVR, acupuncture-associated vasovagal response; F, female; M, male; BFA, Battlefield Acupuncture.
Shoulder and Neck Tension with Pain
The patient was a 46-year-old female experiencing chronic shoulder and neck tension and soreness, with occasional pain referred to the arms. She rated these symptoms at moderate severity prior to treatment. In the past, she had pursued physical therapy, chiropractic, and massage to help manage her symptoms. She stated that the condition was improved with exercise and worse with bad posture. In addition to musculoskeletal pain, this patient reported stress and anxiety for 4 years, accompanied by difficulty in falling asleep and staying asleep, waking 5 times nightly to urinate. She had a poor appetite and an irregular meal schedule. It was noted that the patient was fasting prior to treatment.
This patient had no prior experience with acupoint therapy. For treatment, the provider selected bilateral acupoints GB 20, GB 21, LI 4, ST 36, SP 6, LR 8, KI 3, and LR 3. During needle retention, she became pale and dizzy, and broke out in a full body sweat (oral communication, July 19, 2017, B.J. Gosse). The acupuncture needles were removed immediately and the patient was given time to recover (oral communication, July 19, 2017, B.J. Gosse). After recovery, tu'ina was performed on the patient's neck and shoulders. Post-treatment, she ranked her shoulder and neck tension symptoms as mild. She was advised to eat before her next treatment.
Despite experiencing AAVR symptoms during her first treatment, this patient continued to return for 6 additional treatments without additional AAVR or other adverse events.
Pain from Back Strain
The patient was a 53-year-old female who was seeking relief for constant low-back pain associated with a recent strain, neck tension, and headache. Her low-back pain was constant, severe with movement, and moderate while sitting. She had experienced similar low-back pain two to three times over the last 5 years. Her headaches occurred one to two times weekly, with associated neck and shoulder tension. There was a recent flare in her neck tension and increased stress. She had a history of poor sleep, with difficulty in both sleep onset and staying asleep.
This patient had no prior experience with acupoint therapy. The session started with bilateral insertion of acupuncture needles following the auricular Battlefield Acupuncture protocol (Cingulate Gyrus, Thalamus, Omega 2, Point Zero, Shen Men), followed by UB 62. Within a few minutes, she became sweaty, her complexion became pale, and she felt dizzy. The needles were removed immediately upon onset of the symptoms, and patient was placed supine to recover. She reported afterward that she was able to move more easily and experienced less pain and tension in her back.
Stress and Digestive Concerns
The patient was a 38-year-old male, who had been experiencing increased stress levels and acid reflux for 6 months. He reported his stress levels and acid reflux as moderate. Additionally, he had been experiencing an irregular sleep schedule, waking in the night to care for his hospitalized child and sometimes feeling tired upon waking in the morning.
It was not known if this patient had prior experience with acupoint therapy. During treatment, needles were inserted at acupoints EX-HN3 (YinTang), and bilateral LI 4, ST 36, ST 44, and LR 3. After insertion of the last needle, the patient became dizzy (oral communication, July 19, 2017, B.J. Gosse). The needles were removed immediately; as they were being removed, the patient lost consciousness and became verbally unresponsive for ∼60 seconds (oral communication, July 19, 2017, B.J. Gosse). His feet were elevated, and acupressure was performed on GV 26 (oral communication, July 19, 2017, B.J. Gosse). The patient began speaking, was given water to drink, and, after a few minutes, was walked back to his child's hospital room. After recovery, he appeared optimistic, stating “that was an experience” and that he was ready for a nap.
Headache and Back Tension
The patient was a 33-year-old female, who was experiencing tension headaches with shoulder and back pain, tension, and stiffness for 1 week. She reported her symptoms as mild at the time of treatment and said that the symptoms were reduced with massage and nonsteroidal anti-inflammatory drug medications. Although she did not have sleeping problems when at home, she reported that, while staying overnight in the hospital with her family member, she was not getting much sleep and had low energy.
This patient had no previous experience with acupoint therapy. The provider selected bilateral acupoints ST 36, LI 4, GB 20, and LR 3 for treatment. The patient reported experiencing dizziness during treatment, and the needles were removed early to allow her time to recover. Duration of needle dwelling prior to onset of dizziness was not recorded in this patient's chart notes. After recovery, tu'ina was performed on her neck and shoulders.
Headache and Shoulder Tension
The patient was a 52-year-old female, who had been experiencing a mild but persistent frontal headache for 2 days with severe, constant, bilateral shoulder tension for a “few days.” She had a history of chronic migraines for 40 years, 2–3 times per month, typically manifesting as right-sided pain starting in the occipital region that could last for 2 days each time. Recently, she had been experiencing increased stress and irregular disrupted sleep. This patient had a history of Bell's palsy on the right side in 1976, with recurring right eye watering associated with fatigue.
This patient's prior experience with acupoint therapy was unknown. The treatment included auricular acupoints Shen Men and Spleen, and bilateral body acupoints LR 3, ST 36, LI 4, GB 21, GB 20, and GB 8. After insertion of GB 8, the patient reported experiencing nausea and a “glossy” feeling. The provider removed GB 8 after 1 minute. Auricular needles were removed 5 minutes later. The “glossy” and nauseous feeling decreased, and treatment continued. After the needles were removed, tu'ina massage was performed on the patient's neck and shoulders. After treatment, the patient reported that both her headache, and shoulder pain and tension, had been reduced, that the remaining pain was mild, and that she was able to turn her head more easily.
Discussion
As noted previously, paper charts are maintained. Given that this is an educational clinic experience for advanced student interns from NWHSU, charts were updated manually and were used by different interns throughout the course of this study's 18-month timeline. The chart review demonstrated the importance of maintaining detailed charting of historical details, symptoms, treatment, and outcome measures for every patient, especially in cases when adverse events occurred. The 5 featured case studies demonstrate the variability of AAVR onset and symptom presentation. Three of the patients were new to receiving acupuncture treatment; prior experience for 2 of the patients was unknown. Increased stress levels, irregular sleep, and disrupted lifestyle patterns precipitated by hospitalization of a family member were common symptoms of all of these patients. Three of them reported common symptoms of headaches, and neck, shoulder, and back tension. Despite experiencing AAVR, 3 patients reported reduction of their main complaint symptoms after treatment. Two cases did not have outcome measures of the main complaint recorded.
The fact that 3 patients had documented reduction of symptoms, despite AAVR, raises interesting questions about the potential positive outcomes that could result from what is typically considered an adverse event. Greenwood discusses this question at length, suggesting that AAVR may be a signal of a transformative experience in-progress.1 By cautiously allowing AAVR to proceed and self-resolve, rather than “pathologizing” the phenomena and immediately terminating treatment, Greenwood asserts that a provider might facilitate a large, transformational energy shift for a patient experiencing AAVR.1 Highlighting that an intention of acupuncture treatment is to promote the unrestricted, smooth flow of Qi, he notes that the dramatic symptoms associated with AAVR indicate that Qi is moving, albeit strongly. Terminating treatment in light of AAVR may freeze “an energy shift in process,” potentially deterring the patient from moving past “entrenched blocks” and reconnecting with original energy.1 Rather than being unsuitable for acupuncture treatment, Greenwood suggests that affected patients may be particularly sensitive and responsive to it.1
Greenwood acknowledges that the decision to halt treatment is safer and that the decision to allow the treatment to proceed without intervention must be made with consideration of the situation and context.1 However, his observations about the nature and movement of Qi associated with AAVR and the potential for transformative effects are thought-provoking. The difficulty is that a provider must allow the situation to progress in order to see if something positive would result, a choice that could pose potential risks to both patients and providers.
While some patient groups present with clearly increased susceptibility to AAVR, the potential to feel vulnerable, uncomfortable, or anxious in a new situation, whether that be an external environment or an internal psychoemotional experience, is a commonality of the human experience. The body, and the experience of living in it, is ever changing—under specific circumstances, any patient, at any time, could be “that patient.” Precautions should be taken throughout the treatment process to ensure the safety and comfort of all patients. The provider must pay close attention to the subjective experience and objective observations of the patient, and respond appropriately.
AAVR Prevention and Treatment
In the process of bringing acupuncture to an academic medical center, the authors recognize the importance of quality improvement, quality assurance, training, and documentation measures. To that end, we have developed recommendations for prevention and treatment of AAVR. These are discussed in the next two sections.
Prevention
Prevention of adverse events encourages a safe-practice environment, patient satisfaction and comfort, and cost-effectiveness.
The acronym PEACHES can be helpful for remembering areas of consideration to prevent AAVR:
• Position
• Experience
• Anxiety
• Constitution
• Hydration, feeding, and sleep
• Environment
• Symptom recognition.
Position
During treatment, a patient should be as comfortable as possible in a supine, prone, or seated position. For seated treatments, a zero-gravity–style chair is an excellent choice. Zero-gravity chairs allow a patient to be reclined with legs extended and can be adjusted to patient and provider preference. If zero-gravity chairs are not an option, choose a chair with sturdy arms and that allow enable the patient's legs to be elevated and extended on a footstool.
Experience
The prior experiences of both the patient and the provider should be taken into consideration prior to treatment.
Patient intake should include assessment of previous experience with acupuncture and bodywork, the presence of needle-fear or anxiety about medical interventions, and past history of vasovagal reflex responses. Additionally, the provider should invite discussion of any fears or concerns the patient may have regarding acupuncture treatment and offer clear, encouraging explanations of treatment procedures. Possible symptoms of AAVR should be discussed with the patient, and the patient should be empowered to share with the provider any sensations experienced during the treatment.
Treatment should be structured based on information gathered during patient assessment. As appropriate, one should consider conservation of needles, gentle needling techniques and insertions, and thinner needle gauges for patients who have increased risks of possible AAVR. Needle-free treatment approaches, such as acupressure, shonishin, laser, tuning fork, and tu'ina are well-tolerated and effective. These interventions are particularly well-suited for sensitive, vulnerable, and needle-phobic patients.
Clinicians should take time to develop a knowledge base regarding AAVR prevention and treatment. Students of acupuncture in clinical internship training programs should receive education and consult their supervisors and mentors for guidance. The current authors recommend taking time to develop training for all providers in a practice environment, as well as developing AAVR response plans.
Anxiety
Clinicians should consider teaching anxiety-reduction strategies and stress-management tools as part of a treatment, especially with acupuncture-naive, needle-phobic, and anxious patients. For example, guiding the patient in simple breathwork exercises and using needling techniques aligned with the patient's breath can be helpful. This approach could not only help reduce stress associated with receiving treatment but also provide tools that patients can use as part of a larger self-care strategy for stress management.
As a provider, it is also vital to consider one's own level of calm, confidence, and centeredness prior to interaction with each patient. Providers are often exposed to unexpected challenging situations in clinical environments that may trigger anxiety, self-doubt, frustration, or compassion fatigue. To manage one's own stress and reduce the risk of poor communication with patients and colleagues, one should consider exploring ways to build resiliency through stress management and self-compassion techniques, seeking out additional training to be confident in clinical knowledge, and consulting with other providers when necessary.
Constitution
Significant emotional and mental stress, lifestyle irregularity, overwork, and insufficient sleep will tax the body's Qi, Blood, Yin, and Yang. The impact this has on a patient, and the intensity of the resulting symptoms, will vary from individual to individual, depending on each patient's unique constitution. When planning treatment, it is important to take into account both each patient's constitutional root pattern diagnosis and more acute branch-type pattern diagnoses.
Hydration and Feeding, and Sleep
A provider should inquire regarding the hydration, feeding, and sleep patterns of a patient. When did the patient last eat or drink, and what is this patient's diet and meal schedule? What is the sleep pattern? Is the patient sleep-deprived, overworked, or fatigued? Is this a new pattern or an established pattern in his or her lifestyle?
Environment
Managing the treatment environment is an area of opportunity for promoting calmness and comfort through various sensory stimuli. To the extent that a provider is able, one can explore options for individualization as part of the patient's treatment. Some options include:
• Dimmable or low level lighting
• Noise-level management
• Music or sound healing
• Ventilation and air circulation
• Temperature control
• Room dividers/screens/curtains for patient privacy
• Aromatherapy
• General flow and energetics of the treatment space.
Symptom (Recognition)
A provider should be well-versed on the varied symptoms of AAVR. One should check with the patient regularly during treatment to ensure that his or her condition is stable, especially with acupuncture-naive or sensitive individuals.
Treatment
With proper support, most individuals will recover from an AAVR within 5 minutes.4 Published literature discusses many approaches for treating AAVR symptoms in patients. The acronym RIPCORD can be helpful for remembering appropriate interventions to address AAVR, as follows:
• Recognize
• Initiate
• Position
• Communicate
• Order treatments
• Reassess
• Document.
Recognize
One needs to recognize the risk-factors and early signs of AAVR to interrupt escalation of symptoms and prevent a more-serious situation.
Initiate
One should do the following: Complete a full, but brief, assessment of the patient's condition and what is immediately required. Assess the A, B, Cs (Airway, Breathing, Circulation). Know the location of the automated external defibrillator and how to use the equipment if necessary. Initiate the AAVR or emergency response plan that the clinical environment has in place.
Position
If a patient is showing symptoms of an AAVR, the provider should remove all needles from the patient immediately.4 If possible, one should lie the patient supine and elevate the patient's feet to increase flow of blood toward the brain and heart.4 Care should be taken to ensure the patient is positioned safely and will not fall. Ensure the patient has access to fresh air, opening a window if possible and loosening any tight or restrictive clothing.4 One should offer room temperature or warm water for the patient to drink.1,4
Communicate
It is important to monitor the patient closely and maintain affirming verbal communication.1,4 If other providers are in the treatment area, one should communicate with them as necessary to help support the patient's health and safety, obtain what is needed to manage the incident, and ensure the well-being of any bystanders. Witnessing an AAVR incident can be a trigger for bystanders to experience anxiety, fear, panic, or possibly vasovagal responses of their own, so maintaining a calm environment is key.
Order Treatments
A quick response can help promote patient recovery. Depending on the severity of symptoms, there are several ways to support a patient after needles have been removed and they are positioned safely.
Acupoint therapy
Published literature shows a variety of suggested acupoints for emergency treatment of AAVR (Table 2). 1,4,25,26 Acupoint GV 26 is commonly suggested.1,4,25 Tonification of ST 36 to address AAVR symptoms associated with needle placement in the upper body, or tonification of LI 4 to address AAVR symptoms associated with needle placement in the lower body, are also recommended. Acupoints KI 1, GV 25, PC 6, PC 7, PC 8, and PC 9 are also frequently cited as options for treatment.1,21,25,27 These points can be stimulated with a needle, a needle-insertion tube, or a fingernail.
Table 2.
Emergency Treatment Methods for AAVR in the Published Literature
| Stimulation method | Acupoints & references |
|---|---|
| Needle, or apply pressure with a needle insertion tube or fingernail | • GV 261,4,25 • GV 2525 • ST 36, precipitating needles in upper body1,25 • LI 4, precipitating needles in lower body1 • KI 127 • PC 625 • PC 721 • PC 821 • PC 921,25 • EX-HN 3 (YinTang) + CV 2426 |
| Moxibustion | • GV 2025 • CV 625 • CV 425 |
Acupoints EX-HN 3 (YinTang) and CV 24 can also be useful for supporting recovery. A 2015 case report explored the emergency first-aid use of acupoints EX-HN 3 and CV 24 on a 45-year-old female patient experiencing cardiac arrhythmia and neurocardiogenic syncope after walking for 20 minutes.26 While waiting for mobile intensive care unit to arrive, 0.25 mm × 0.15 mm needles were inserted perpendicular to the meridian at acupoints EX-HN 3 and CV 24 and stimulated continuously for 1 minute.26 Needles were retained for ∼20 minutes, with additional needle stimulations every 5 minutes, and then removed.26 During needle retention, vital signs were monitored and the patient's condition normalized.26 Although the featured patient did not experience onset of syncope in association with acupuncture treatment and EX-HN 3 and CV 24 are not included in the other sources referenced in this section, this case report indicates that these points could be useful for promoting ANS function and homeostasis in cases of neurocardiogenic syncope.26
Auricular acupoints are not typically referenced as options for emergency AAVR treatment in the published literature. Auriculotherapy's pronounced effect on the nervous system and vagal regulation, however, makes this modality an easily accessible option for emergency AAVR treatment that warrants further exploration and research.28 The auricle is supplied by cranial and spinal nerves; notably, the auricular branch of the vagus nerve—the only peripheral branch of the vagus nerve—innervates the concha and the region around the auditory meatus.28
Oleson discusses at length the neurophysiologic, embryologic, and microsystem theories of auriculotherapy, linking the autonomic vagus nerve to a chain of acupoints on the concha wall of the auricle.29 Additionally, several primary Master Points, including Point Zero, Sympathetic Autonomic, Thalamus, and Shen Men act directly on the ANS to reduce disequilibrium and promote homeostasis.29 Oleson asserts that primary Master Points support the action of other auricular points; thus, using a Master Point in combination with select anatomical or functional auricular reflex points would enable an elegant and tailored treatment approach, depending on the patient's presenting AAVR symptoms and underlying constitution.29 Auricular regions and acupoints may be stimulated by various methods, such as traditional acupuncture or intradermal needles, press needles, an ear probe, laser, acupoint stimulator, an insertion tube, adhesive pellets, or fingernail pressure. Intradermal needles, press needles, and adhesive pellets that are retained in place, provide the opportunity to produce an ongoing therapeutic effect hours-to-days after the onset of AAVR symptoms and initial emergency treatment.
When clinical environment policies permit, the use of moxibustion can also be helpful in AAVR recovery. Moxibustion is the practice of burning mugwort leaf, or ài yè (艾叶), on or over the skin's surface to produce a warming, moving effect. Various species of mugwort are used medicinally throughout the world; traditionally, the Asian species Artemisia argyi has been used in China.30 Published literature suggests the use of moxibustion on acupoints GV 20, CV 6, or CV 4 in cases of AAVR.25 Due to the fact that many patients will have significant hair at the location GV 20, moxibustion at this point might not be appropriate.
In the event of AAVR, a provider should assess the patient's presenting symptoms, clinical history, and constitution, as well as clinical function of the recommended acupoints, and choose the most appropriate acupoint(s) and methods of stimulation for emergency treatment.
Flower essences
A provider may consider administering Bach Rescue Remedy® to the patient experiencing AAVR symptoms. Rescue Remedy is a 5 × (Homeopathic Pharmacopoeia of the United States) dilution of flower essences from impatiens (Impatiens gladulifera), Star of Bethlehem (Orithogalum umbellatum), cherry plum (Prunus cerasifera), rock rose (Helianthemum), and clematis (Clematis vitalba).31 Rescue Remedy is indicated for use in stressful situations or in times of crisis.31 This should not be primary therapy, but may be added during recovery time at provider discretion.
Additional emergency medical interventions
If the patient's condition deteriorates or consciousness is not regained after 5 minutes, one should call 911, or. if working in a hospital environment, call the appropriate code.4 Basic life support procedures should be utilized as necessary while waiting for additional emergency support.
Reassess
After each treatment intervention, it is important to reassess the patient to ensure up-to-date information is acquired for accurate decision-making. Additionally, one should reassess the scene to ensure that witnesses have been attended to and are safe and comfortable.
Document
After the event, detailed documentation of the event should be made in the patient's chart and in any adverse events reporting logs specific to the provider's clinical environment. The incident should be reviewed with the patient's care team as appropriate, and opportunities for improvement in response and prevention should be examined as necessary.
Conclusions
This article summarizes the prevailing Western and TCM explanations for AAVR, presents case studies demonstrating a range of symptom severity, and proposes novel descriptive terminology. As integrative practices become more prevalent in academic institutions and primary-care environments, clear communication about—and prevention, treatment, documentation, and reporting of—acupuncture-associated adverse events will become increasingly valuable. The recommendations for uniform terminology and educational tools for prevention and treatment of AAVR in this article contribute to the existing published literature and add to the base of evidence-informed practice. If utilized, these recommendations could support site quality-improvement and quality-assurance efforts, improved patient outcomes and experiences, and accurate reporting of AAVR incidents in charting and in the literature. Accurate reporting will support the ability to study prevention and interventions to reduce and treat AAVR appropriately in the future. The current authors recommend that clinicians in integrative practice clinical environments consider developing AAVR response plans, and training students, supervising and attending providers, and ancillary staff members to ensure rapid, prepared handling and documentation of AAVR incidents.
Acknowledgments
The authors would like to thank Jamie Walski, BA, CCRP, Clinical Research and Cancer Survivorship Programs manager, University of Minnesota, and Jill Larsen, DAOM, DiplOM, LAc, for their support during this project. Gratitude is also extended to the patients and families, the dedicated staff at the UMMCH, and students at NWHSU, who exemplify an integrative and transdisciplinary approach to health care every day. Dr. Christensen is the recipient of the Pediatric Integrative Health Fellowship, sponsored jointly by the University of Minnesota's medical school department of pediatrics and NWHSU.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Greenwood MT. Needle shock: Adverse effect or transformational signal. Medical Acupuncture. 2004;15(3):27–32 [Google Scholar]
- 2.Cole M, Shen J, Hommer D. Convulsive syncope associated with acupuncture. Am J Med Sci. 2002;324(5):288–289 [DOI] [PubMed] [Google Scholar]
- 3.Kung Y-Y, Chen F-P, Hwang S-J, Hsieh J-C, Lin Y-Y. Convulsive syncope: An unusual complication of acupuncture treatment in older patients. J Altern Complement Med. 2005;11(3):535–537 [DOI] [PubMed] [Google Scholar]
- 4.Zhu HZ. Running a Safe and Successful Acupuncture Clinic. New York, NY: Elsevier Churchhill Livingstone; 2006 [Google Scholar]
- 5.Gatzoulis KA, Toutouzas PK. Neurocardiogenic syncope. Drugs. 2012;61(10):1415–1423 [DOI] [PubMed] [Google Scholar]
- 6.Wu J, Hu Y, Zhu Y, Yin P, Litscher G, Xu S. Systematic review of adverse effects: A further step towards modernization of acupuncture in China. Evid Based Complement Alternat Med. 2015;2015:432467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Birch S, Alraek T, Norheim AJ. Acupuncture adverse events in China: A glimpse of historical and contextual aspects. J Altern Complement Med. 2013;19(10):845–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colloca L, Finniss D. Nocebo effects, patient–clinician communication, and therapeutic outcomes. JAMA. 2012;307(6):567–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alboni P, Furlan R, eds. Vasovagal Syncope. New York, NY: Switzerland Springer International Publishing; 2015 [Google Scholar]
- 10.Hamilton JG. Needle phobia: A neglected diagnosis. J Fam Pract. 1995;41(2):169–175 [PubMed] [Google Scholar]
- 11.Accurso V, Winnicki M, Shamsuzzaman AS, Wenzel A, Johnson AK, Somers VK. Predisposition to vasovagal syncope in subjects with blood/injury phobia. Circulation. 2001;104(8):903–907 [DOI] [PubMed] [Google Scholar]
- 12.Alboni P, Brignole M, Degli Uberti EC. Is vasovagal syncope a disease? Europace. 2007;9(2):83–87 [DOI] [PubMed] [Google Scholar]
- 13.He W, Zhao X, Li Y, Xi Q, Guo Y. Adverse events following acupuncture: a systematic review of the Chinese literature for the years 1956–2010. J Altern Complement Med. 2012;18(10):892–901 [DOI] [PubMed] [Google Scholar]
- 14.Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9(1):72–83 [PubMed] [Google Scholar]
- 15.Wiseman N, Feng Y. A Practical Dictionary of Chinese Medicine. Brookline, MA: Paradigm Publications; 1998 [Google Scholar]
- 16.Yuan Z, Liangbi W, Yongchang R, Manser MH, eds. Pocket Oxford Chinese Dictionary: English–Chinese, Chinese-English, 3rd ed. New York, NY: Oxford University Press; 2004 [Google Scholar]
- 17.Chen FP, Hwang SJ, Lee HP, Yang HY, Chung C. Clinical study of syncope during acupuncture treatment. Acupunct Electrother Res. 1990;15(2):107–119 [DOI] [PubMed] [Google Scholar]
- 18.yùn chǎng, Definition, Mandarin Chinese Pinyin English Dictionary: Yabla Chinese. Online document at: https://chinese.yabla.com/chinese-english-pinyin-dictionary.php?define=%E6%99%95%E5%9C%BA Accessed June19, 2017
- 19.yūn dǎo, Definition, Mandarin Chinese Pinyin English Dictionary: Yabla Chinese. Online document at: https://chinese.yabla.com/chinese-english-pinyin-dictionary.php?define=yun+dao Accessed June19, 2017
- 20.yūn jué, Definition, Mandarin Chinese Pinyin English Dictionary: Yabla Chinese. Online document at: https://chinese.yabla.com/chinese-english-pinyin-dictionary.php?define=y%C5%ABn+ju%C3%A9 Accessed June19, 2017
- 21.Pirog JE. The Practical Application of Meridian Style Acupuncture. Berkeley, CA: Pacific View Press; 1996 [Google Scholar]
- 22.Hopwood V. The San Jiao/Triple Energizer meridian. J Acupunct Assoc Chartered Physiother. 2014. Spring;41–49 [Google Scholar]
- 23.van Lieshout JJ, Wieling W, Karemaker JM, Eckberg DL. The vasovagal response. Clin Sci (Lond). 1991;81(5):575–586 [DOI] [PubMed] [Google Scholar]
- 24.Hirsch AT, Levenson DJ, Cutler SS, Dzau VJ, Creager MA. Regional vascular responses to prolonged lower body negative pressure in normal subjects. Am J Physiol. 1989;257(1[pt2]):H219–H25 [DOI] [PubMed] [Google Scholar]
- 25.Xinnong C. Chinese Acupuncture and Moxibustion, 3rd ed. Beijing: Foreign Languages Press; 2009 [Google Scholar]
- 26.Fabrin S, Soares N, Pezarezi Yoshimura D, et al. Effects of acupuncture at the Yintang and the Chengjiang acupoints on cardiac arrhythmias and neurocardiogenic syncope in emergency first aid. J Acupunct Meridian Stud. 2016;9(1):26–30 [DOI] [PubMed] [Google Scholar]
- 27.Patel JK. Clinical Acupuncture. New Delhi, India: Health Harmony; 1981, 1996 [Google Scholar]
- 28.He W, Wang X, Shi H, et al. Auricular acupuncture and vagal regulation. Evid Based Complement Alternat Med. 2012;2012:786839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture. 2nd ed. Mesa, AZ: Health Care Alternatives, Inc.; 1996 [Google Scholar]
- 30.Adams JD, Garcia C, Garg G. Mugwort (Artemisia vulgaris, Artemisia douglasiana, Artemisia argyi) in the treatment of menopause, premenstrual syndrome, dysmenorrhea and attention deficit hyperactivity disorder. Chin Med. 2012;03(3):116–123 [Google Scholar]
- 31.Thaler K, Kaminski A, Chapman A, Langley T, Gartlehner G. Bach Flower Remedies for psychological problems and pain: a systematic review. BMC Complement Altern Med. 2009;26;9:16. [DOI] [PMC free article] [PubMed] [Google Scholar]