Abstract
Purpose
We sought to measure inpatient healthcare utilization among U.S. Veteran Affairs beneficiaries surviving sepsis hospitalization, and to examine how post-sepsis utilization varies by select patient characteristics.
Materials and Methods
Retrospective cohort study of 26,561 Veterans who survived sepsis hospitalization in 2009. Using difference-in-differences analysis, we compared changes in healthcare utilization in one year before and one year after sepsis hospitalization by Veteran age, illness severity, and recent nursing facility use.
Results
Median days in a healthcare facility increased from 5 to 10. Veterans with recent nursing facility use spent a median 65 days (or 86% of days alive) in a healthcare facility in the year after sepsis. Older age, greater illness severity, and recent nursing home use were each associated with spending more days, and a greater proportion of days alive, in a healthcare facility during the year after sepsis. However, none of these characteristics was associated with a greater rise in utilization after sepsis.
Conclusions
Veterans surviving sepsis experience high rates of post-sepsis mortality and significant increases in healthcare facility use. Recent nursing facility use is strongly predictive of greater post-sepsis healthcare utilization.
INTRODUCTION
Over the past decade, there has been a steady rise in number of hospitalizations with a recognized diagnosis of sepsis, and a concurrent decline in the rate of in-hospital sepsis mortality1–4. As a result, there is an emerging population of sepsis survivors4, the majority of whom experience new functional disability and/or cognitive impairment4,5. In the U.S.-nationwide Veterans Affairs (VA) health system, over 35,000 Veterans are hospitalized with sepsis each year, and approximately 80% survive to hospital discharge2,6. Similar to Medicare beneficiaries, Veterans have a high rate of hospital readmission following sepsis6. However, little is known about the overall burden of healthcare utilization in Veterans surviving sepsis, and how this utilization differs by patient subtypes. Thus, we sought to measure all days spent in a hospital or nursing facility among Veterans surviving a sepsis hospitalization, to compare post-sepsis utilization to Veterans’ own pre-sepsis resource use, and examine how post-sepsis utilization varies by patient characteristics, such as age, illness severity, and recent nursing home use.
METHODS
Cohort of Sepsis Hospitalizations
We identified all sepsis hospitalizations at any of 114 VA hospitals in 2009. We used the method of Angus et al.7, which requires either concurrent International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) codes for infection and acute organ dysfunction or explicit coding for severe sepsis or septic shock. This method has similar specificity, but greater sensitivity than other claims-based identification methods8, and performs comparably within the VA to non-federal hospitals6. We excluded hospitalizations with inpatient mortality and hospitalizations in which the patient transferred from a non-VA hospital to the VA. For patients with multiple sepsis hospitalizations during 2009, we included just the first hospitalization.
Healthcare Use
Our outcome of interest was days spent in a healthcare facility—the composite of short-term acute care hospitalizations, long-term acute care hospitalizations, skilled nursing facility (SNF), and custodial nursing care. To measure healthcare facility use before and after sepsis hospitalization, we used four data sources: (1) VA Inpatient Evaluation Center files on VA hospitalizations, (2) VA Inpatient Evaluation Center files on VA nursing homes, (3) “fee-based” care files for VA-funded care provided outside of the VA, and (4) MedPAR files for dual VA and Medicare beneficiaries. Collectively, these files capture all inpatient healthcare provided or paid for by the VA, as well as all non-VA care paid for by Medicare.
Inspired by the methods of Intrator, et al.9, we determined each patient’s daily location based on dates of service in the four data sources, and assumed that patients were at home for any day that they were known to be alive and not admitted to a healthcare facility based on the above files. By determining each patient’s daily location for the one year before and one year after sepsis hospitalization, we ensured that healthcare use was never “double-counted”. For example, if a skilled nursing facility bed were “held” while a patient was briefly hospitalized, the days with over-lapping SNF and hospitals stays would be counted just once in the tally of healthcare facility days. For the instances where patients use multiple types of healthcare facilities, we classified the patient’s location using the following hierarchy: dead, hospital, nursing facility, home, similar to Intrator, et al.
After determining the daily location of each patient during the one year before and one year after sepsis hospitalization, we calculated the total number of days spent separately at home, in a hospital, and in nursing facilities. We also calculated the total number of days spent in any healthcare facility (hospital or nursing facility), and also the proportion of days alive spent in a healthcare facility.
Illness Severity
We calculated illness severity (predicted 30-day mortality) using a composite score similar to APACHE IV2,10. We constructed the score using variables that make up the VA ICU severity score, a validated risk-adjustment measure10 that includes age, admission diagnosis category, 29 comorbid conditions11,12, and 11 laboratory values drawn in the first 24 hours of hospitalization: sodium, blood urea nitrogen, glomerular filtration rate, glucose, albumin, bilirubin, WBC count, hematocrit, pH, PaCO2, and PaO2. To allow for a flexible nonlinear structure in the severity of illness score, we used a logistic multivariate adaptive regression spline (MARS)13, a nonparametric spline-and-knot-based form of regression that models the functional forms of covariates, as well as the nonlinearities and higher-level interactions thereof, for an outcome of 30-day mortality2.
Statistical Analysis
We present patient and hospitalization characteristics as numbers (percentages), means (SDs), or medians (interquartile ranges [IQR]) as appropriate. To compare Veterans’ own healthcare use before and after sepsis, we used the Wilcoxon signed-rank test. This non-parametric test accounts for the skewed distribution of the outcomes and the paired nature of the data. To compare healthcare utilization in the year after sepsis among non-patients sub-groups, we used the non-parametric Wilcoxon rank sum test.
We performed three difference-in-difference analyses14 to compare changes in healthcare use between patients of differing: (1) age: older (≥ 65 years) versus younger (≤ 64 years); (2) illness severity: predicted mortality above versus below median predicted 30-day mortality (as described below); and (3) pre-sepsis nursing facility use: none versus any in the 30 days preceding hospitalization.
We then built a multivariable model predicting the percentage of days alive in the year after sepsis hospitalization that are spent in a healthcare facility. Because the dependent variable (percentage of days in a healthcare facility) falls between 0 and 1, we used a generalized linear model with a logit link and the binomial family15. Model calibration was assessed by comparing the predicted versus actual percentage of days alive spent in a healthcare facility, by decile of predicted percentage. Using this model, we present post-sepsis utilization for select patient scenarios. Specifically, we calculated the predicted percentages of days alive spent in a nursing facility for patients with median illness severity and median hospital length of stay, but varying ages (50, 65, and 80 years) and varying nursing home use (none, the week prior, and the 6 months prior to sepsis hospitalization).
This research was approved by the Ann Arbor VA Institutional Review Board. We conducted all analyses using Stata MP Software, version 14.1 (StataCorp, College Station, TC) and SAS 9.4.
RESULTS
Patient and Hospital Characteristics
We identified 26,561 Veterans who survived a first sepsis hospitalization at any of 114 VA hospitals in 2009 (Table 1). Patients were older (median 69 years), predominantly male (96.8%), with a moderate burden of co-morbid disease (median Elixhauser Comorbidity Index 6). Hospital length of stay was a median of 7 days (IQR 4–13 days). 36.2% of patients were admitted to an ICU, and 12.7% were mechanically ventilated. Median predicted risk of 30-day mortality was 10.6%. Patient and hospitalization characteristics by subgroup are presented in Supplemental Table 1.
Table 1.
Characteristics and Outcomes of Sepsis Hospitalizations with Live Discharge
| Patient and Hospitalization Characteristics | Sepsis Hospitalizations (N=26,561) |
|---|---|
| Age, median (IQR) | 69 (61, 80) |
| Race, N (%) | |
| African American | 4,900 (18.5%) |
| Caucasian | 19,135 (72.0%) |
| Other | 366 (1.4%) |
| Unknown | 2,160 (8.1) |
| Male, N (%) | 25,710 (96.8%) |
| Elixhauser Comorbidity Index, median (IQR) | 6 (3, 11) |
| Length of Stay, median (IQR) | 7 (4, 13) |
| Admitted to an Intensive Care Unit, N (%) | 9,626 (36.2%) |
| Used mechanical ventilation, N (%) | 3,372 (12.7%) |
| Outcomes | |
| 30-Day Readmission, N (%) | 7,251 (27.3%) |
| 90-Day Readmission, N (%) | 11,504 (43.3%) |
| 30-Day Mortality, N (%) | 2,329 (8.8%) |
| 90-Day Mortality, N (%) | 4,368 (16.5%) |
| 1-Year Mortality, N (%) | 8,289 (31.2%) |
Healthcare Use and Mortality in the Year after Sepsis
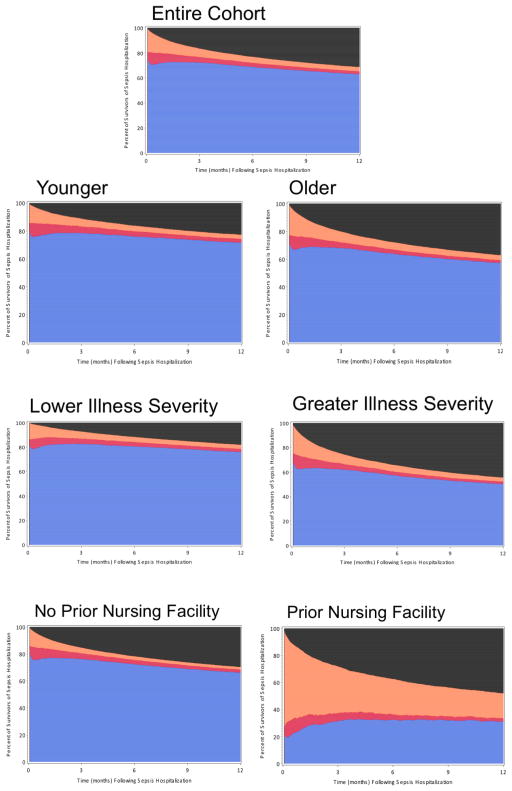
Of the 26,561 Veterans surviving sepsis, 2,373 (8.9%) had been admitted to a nursing facility in the prior 30 days, and 5,144 (19.4%) were discharged to a nursing facility. In the year after sepsis hospitalization, the median patient spent 0 days (IQR 0, 12) in a nursing facility and 10 days (IQR 0, 37) in any healthcare facility, or 3.8% of days alive (IQR 0.0%, 20.9%) (Table 2, Figure 1). 2,329 (8.8%) died within 30 days, and 8,289 (31.2%) died within 1 year of discharge from sepsis hospitalization.
Table 2.
One-year outcomes in survivors of sepsis
| Cohort | Days at Home, Median (IQR) | Days in Healthcare Facility, Median (IQR) | % of days alive in Healthcare Facility, Median (IQR) | 1-Year Mortality N (%) |
|---|---|---|---|---|
| All Patients, N=26,561 | 336 (115, 362) | 10 (0, 37) | 3.8% (0.0%, 20.9%) | 8,289 (31.2%) |
| Age ≥ 65 years, N=15,924 | 320 (64, 320) | 11 (0, 39) | 4.6% (0.0%, 26.1%) | 5,893 (37.0%) |
| Age < 65 years, N=10,637 | 349 (228, 365) | 9 (0, 34) | 3.0% (0.0%, 15.3%) | 2,396 (22.5%) |
| Higher Illness Severity, N=13,280 | 268 (30, 357) | 12 (0, 42) | 6.6% (0.0, 33.7%) | 5,901 (44.4%) |
| Lower Illness Severity, N=13,281 | 353 (278, 365) | 8 (0, 32) | 2.5% (0.0%, 12.6%) | 2,388 (18.0%) |
| Recent Nursing Facility Use, N=2,373 | 9 (0, 262) | 65 (17, 215) | 86.5% (16.4%, 100%) | 1,138 (48.0%) |
| No Recent Nursing Facility Use, N=24,188 | 343 (168, 363) | 8 (0, 31) | 3.0% (0.0%, 15.3%) | 7,151 (29.6%) |
Recent nursing facility use = any nursing facility use in the 30 days prior to sepsis hospitalization; Community dwelling = no nursing facility use in the 30 days prior to sepsis hospitalization.
Abbreviations: IQR=interquartile range; MV=mechanically ventilated; NF=nursing facility
Figure 1.
Healthcare Facility Use and Mortality in the Year Before and After Sepsis Hospitalization, Overall and by Subgroups
This figure shows the daily location of 26,591 sepsis survivors in the year after sepsis hospitalization. The index sepsis hospitalization is not included; the year after begins the day after hospital discharge. Patients are depicted as being at home (blue), admitted to a hospital (red), admitted to an LTAC or nursing facility (orange), or dead (black).
Inpatient facility use was markedly higher in the patients with recent nursing facility use. These patients spent a median 65 days (IQR 17, 215) admitted to an inpatient healthcare facility in the year after sepsis—which represented 86.5% (IQR 16.4%, 100.0%) of all days alive. Patients with ≥3 weeks of nursing facility use in the prior 30 days (N=1,343) spent a median 111 days (100% of all days alive) in a healthcare facility in the year after sepsis (Supplemental Table 2).
Patients with older age and greater illness severity spent more days and a greater percent of days alive in inpatient facilities in the year after sepsis (Table 2), compared to younger and less severely ill Veterans, respectively, p<0.001 for each comparison. Meanwhile, patients with prior nursing facility use spent substantially more days in healthcare facilities after sepsis: median 65 days (IQR 17, 215) versus 8 (0, 31) in patients without recent nursing facility use; p<0.001; and median 86.5% of days alive (IQR 16.4%, 100%) versus 3.0% (0.0%, 15.3%) in patients without recent nursing facility use.
Changes in Healthcare Use Before and After Sepsis
Overall, patients used more inpatient healthcare resources in the year after sepsis compared to the year prior (Supplemental Table 3, Figure 1). Median hospital days increased from 4 to 6 days (p<0.001), while median healthcare facility days increased from 5 to 10 days (p<0.001), and median percent of days alive in a healthcare facility increased from 1.4% to 3.8% (p<0.001).
Changes in Healthcare Use by Age, Illness Severity, and Recent Nursing Facility Use
Changes in healthcare utilization before and after sepsis hospitalization by sub-group are presented in Supplemental Tables 4–6. The rise in inpatient facility days after sepsis hospitalization was similar between older (age ≥65 years) and younger (age <65 years) patients (difference-in-differences for days in a healthcare facility 0.9 days [95% CI: −1.4, 3.2], p=0.43); and also similar between patients with higher versus lower severity of acute illness (difference-in-differences for days in an healthcare facility −1.5 [95% CI: −3.8, 0.7], p=0.18) (Table 3). However, because older sepsis survivors experienced greater mortality in the year after sepsis (37.8% versus 22.2%, p<0.001), they had a greater rise in the proportion of days alive admitted to a healthcare facility (difference-in-differences 5.7% [95% CI: 4.8%, 6.6%], p<0.001) and steeper decline in days spent at home (difference-in-differences −40.3 days [95% CI: −44.0, −36.5], p<0.001). Likewise, because Veterans who survived a more severe sepsis hospitalization had greater mortality in the year after sepsis (44.4% versus 18.0%, p<0.001), they also experienced a greater rise in the proportion of days alive admitted to a healthcare facility (difference-in-differences 5.1% [95% CI: 4.2%, 5.9%], p<0.001) and a steeper decline in days spent at home in the year after sepsis (difference-indifferences −37.8 days [95% CI: −41.5, −34.1], p<0.001).
Table 3.
Difference-in-Differences Analyses Comparing Changes in Healthcare Use in Older vs Younger Patients, Higher versus Lower Illness Severity, and Nursing Home Use versus Not
| Older Age | Illness Severity | Nursing Home Use | ||||
|---|---|---|---|---|---|---|
| DID Estimate (95% CI) | P | DID Estimate (95% CI) | p | DID Estimate (95% CI) | p | |
| Days at Home | −40.3 (−43.9, − 36.5) | <0.001 | −37.8 (−41.5, − 34.1) | <0.001 | −12.9 (−18.8, − 6.9) | <0.001 |
| Days in Healthcare Facility | 0.9 (−1.4, 3.2) | 0.43 | −1.5 (−3.8, 0.7) | 0.18 | −40.8 (−44.1, − 37.5) | <0.001 |
| Days in a Hospital | −0.5 (−1.3, 0.2) | 0.16 | −2.8 (−3.5, − 2.1) | <0.001 | −12.6 (−13.9, − 11.3) | <0.001 |
| Days in a Nursing Facility | 1.4 (−0.6, 3.5) | 0.17 | 1.3 (−0.7, 3.3) | 0.21 | −28.2 (−31.2, − 25.2) | <0.001 |
| Proportion of days alive in a healthcare facility | 0.06 (0.05, 0.07) | <0.001 | 0.05 (0.04, 0.06) | <0.001 | 0.09 (0.08, 0.1) | <0.001 |
Veterans who resided in a nursing facility prior to sepsis experienced a much higher rate of 1-year mortality: 48.0% versus 29.6% (p<0.001) in patients without recent nursing facility use (Figure 2). Due to this high rate of mortality post-hospitalization and high healthcare use prior to sepsis, these Veterans spent fewer days in healthcare facilities in the year after sepsis, compared to the year prior: median 92 days (IQR 42, 287) in the year prior versus 65 (IQR 17,215) in the year after sepsis hospitalization.
Percentage of Days Alive Spent in a Healthcare Facility
In a multivariable model, age, illness severity, length of hospitalization, and prior nursing facility use were each significantly associated with the percentage of days alive spent in a healthcare facility in the year after sepsis (Supplemental Table 7, Supplemental Figure 1). We present the predicted percentages of days alive spent in a healthcare facility for a variety of clinical scenarios in Table 4. These can vary dramatically. For example, for a 50-year-old Veteran surviving sepsis hospitalization, with median illness severity, median hospital length of stay, and no recent nursing facility use, the predicted percentage of days spent in a healthcare facility in the year after sepsis was 8%. This jumps dramatically to 25% for a 50-year-old Veteran who spent the prior week in a nursing facility, and to 58% for a 50-year-old Veteran who spent the prior 6 months in a nursing facility. By contrast, the predicted percentage increases just slightly with age (to 9% for a 65-year-old Veteran, with no recent nursing facility use, and 11% for an otherwise similar 80-year-old Veteran), and only trivially with greater severity of illness.
Table 4.
Predicted Proportion of Days Alive after Sepsis Hospitalization Spent in a Healthcare Facility
| Scenario* | Age | Nursing Facility Use | Predicted Risk of 30-Day Mortality | Predicted Percentage of Days After Sepsis In a Healthcare Facility, 95% CI |
|---|---|---|---|---|
| 1 | 50 | None | Median (10.7%) | 7.6% (7.2%, 7.9%) |
| 2 | 50 | Prior Week | Median (10.7%) | 24.8% (22.9%, 26.7%) |
| 3 | 50 | Prior 6 months | Median (10.7%) | 58.1% (55.5%, 60.7%) |
| 4 | 65 | None | Median (10.7%) | 9.1% (8.8%, 9.4%) |
| 5 | 65 | Prior Week | Median (10.7%) | 28.8% (26.8%, 30.7%) |
| 6 | 65 | Prior 6 months | Median (10.7%) | 63.0% (60.6%, 65.3%) |
| 7 | 65 | None | 5th percentile (3.1%) | 9.1% (8.8%, 9.4%) |
| 8 | 65 | Prior Week | 5th percentile (3.1%) | 28.7% (26.8%, 30.7%) |
| 9 | 65 | Prior 6 months | 5th percentile (3.1%) | 62.9% (60.6%, 65.3%) |
| 10 | 65 | None | 95th percentile (41.4%) | 9.2% (8.9%, 9.5%) |
| 11 | 65 | Prior Week | 95th percentile (41.4%) | 28.9% (27.0%, 30.9%) |
| 12 | 65 | Prior 6 months | 95th percentile (41.4%) | 63.1% (60.8%, 65.4%) |
| 13 | 80 | None | Median (10.7%) | 10.9% (10.5%, 11.4%) |
| 14 | 80 | Prior Week | Median (10.7%) | 33.1% (31.0%, 35.3%) |
| 15 | 80 | Prior 6 months | Median (10.7%) | 67.6% (65.3%, 69.9%) |
For each scenario patients had a median hospital length of stay (7 days).
DISCUSSION
In this study of a national cohort of Veterans, we found that sepsis survivors use substantial inpatient healthcare resources in the year after sepsis. The median patient spent 10 days (3.8% of all days alive) admitted to a healthcare facility. Older age, greater illness severity, and quite powerfully, recent nursing facility use were each associated with spending more days, and a greater proportion of days alive, in a healthcare facility during the year after sepsis. Patients with any recent nursing facility use spent a median 65 days (and over 80% of all days alive) in a healthcare facility in the year after sepsis, while those with at least 3 weeks of recent nursing facility use spent a median of 111 days (100% of all days alive) in a healthcare facility.
For the overall cohort, the median number of days in a healthcare facility doubled from 5 in the year prior to sepsis, to 10 in the year after sepsis—suggesting that the healthcare utilization in the year after sepsis is not merely a reflection of sepsis survivors’ age, co-morbidity burden, or propensity to use healthcare, but is also a reflection of new disability5 and heightened risk for medical deterioration after sepsis, such as recurrent infections16–18, acute renal failure17, aspiration17,19, and cardiovascular events20,21.
The number of healthcare facility days increased after sepsis for all sub-groups, except for patients with recent nursing facility use (who spent a median 92 days in a healthcare facility in the year prior to sepsis). However, the proportion of days alive spent in a healthcare facility increased two- to three-fold in all subgroups.
Our findings are consistent with prior studies showing similar median increases in health care utilization after sepsis hospitalization in Medicare22 and Kaiser Permanente beneficiaries23, as well as with prior studies showing high risk for death in the year after surviving sepsis hospitalization24,25. This study extends prior work, however, by understanding how post-sepsis healthcare utilization differs by patient characteristics, and by providing post-sepsis healthcare utilization estimates for common patient scenarios. These scenarios highlight the importance of prior nursing home use in patients’ post-sepsis experience. Prior nursing facility use is associated with several-fold increases in the predicted percentage of days alive spent in a healthcare facility, compared to a three percentage point increase per 15 years of age and trivial increases across the range of illness severity.
While it is not surprising that nursing home patients surviving sepsis hospitalization have high rates of subsequent healthcare utilization and mortality, we believe that these estimates may be helpful to counseling patients and families who are interested not just in the likelihood of long-term survival, but also in quality of their remaining days. While the median Veteran surviving sepsis hospitalization spent just under 4% of their days alive in the subsequent year admitted to a healthcare facility, the median Veteran with recent nursing facility use spent over 2 months and over 80% of their days alive in the subsequent year admitted to a healthcare facility. Patients with recent nursing home use have already made the decision that residing in nursing facility provides acceptable quality of life (at least for the short term). However, sepsis hospitalization—which frequently results in additional functional limitations5—signifies that care-taking needs are unlikely to be temporary, and thus may be an ideal time to reassess goals of care.
Our study should be interpreted in the context of several limitations. First, sepsis was ascertained by ICD-9-CM coding for infection and acute organ dysfunction. This method has greater sensitivity and similar specificity to other claims-based methods for identifying sepsis8, and performs similarly in the VA6. However, there is the possibility for misclassification in both directions. Second, days spent at home were defined by an absence of claims data indicating that the Veteran was admitted to a healthcare facility. While we examined claims for all care provided by the VA, paid for by the VA, or paid for by Medicare for the duration of the study, we did not have information on private insurance claims, Medicaid claims, or self-paid healthcare use. However, we believe that our data sources captured the vast majority of healthcare use for the study population. Third, our study examined sepsis survivors alone. It is possible that these findings are not unique to patients surviving sepsis hospitalization, but rather, are common to survivors of all types of acute medical illness requiring hospitalization.
CONCLUSION
In this national cohort of Veterans surviving sepsis hospitalization, we found that post-sepsis healthcare use was markedly elevated relative to patients own utilization in the year prior to sepsis. The median percentage number of day in a healthcare facility 5 in the year prior to sepsis, to 10 in the year after sepsis. Older age, greater illness severity, and in particular, recent nursing facility use were each associated with spending more days and a greater proportion of days alive in a healthcare facility after sepsis. Veterans with recent nursing facility use spent a median 65 days and >80% of days alive in a healthcare facility during the year after sepsis.
Supplementary Material
Highlights.
The median patient spent 3.8% of their post-sepsis year in a healthcare facility
Recent nursing facility use was strongly predictive of post-sepsis healthcare use
Those with recent nursing facility use spent little time at home post-sepsis
Acknowledgments
Funding: This work was supported by grants K08 GM115859 [HCP] from the National Institutes of Health and VA HSR&D 11-109[TJI] from the Department of Veterans Affairs. The funders had no role in the study design, data collection, data analysis, interpretation of the data, writing of the manuscript, or decision to submit the article for publication.
We appreciate the expert programming of Kyle Kepreos, MA, Wyndy Wiitala, PhD, and Jennifer Davis, MS at the VA Center for Clinical Management Research.
Footnotes
Author Contributions: BV and HCP designed the study and analyzed the data. KD and HCP drafted the manuscript. KD, BV, TJI, and HCP interpreted the data and edited the manuscript critically for intellectual content.
Declaration of Interests: The authors have no potential financial conflicts of interest to report.
Disclaimer: This work does not necessarily represent the view of the U.S. Government or Department of Veterans Affairs.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Crit Care Med. 2014;42:625–31. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prescott HC, Kepreos KM, Wiitala WL, Iwashyna TJ. Temporal Changes in the Influence of Hospitals and Regional Healthcare Networks on Severe Sepsis Mortality. Crit Care Med. 2015;43:1368–74. doi: 10.1097/CCM.0000000000000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014;311:1308–16. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 4.Iwashyna TJ, Cooke CR, Wunsch H, Kahn JM. Population burden of long-term survivorship after severe sepsis in older Americans. J Am Geriatr Soc. 2012;60:1070–7. doi: 10.1111/j.1532-5415.2012.03989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prescott HC. Variation in Postsepsis Readmission Patterns: A Cohort Study of Veterans Affairs Beneficiaries. Ann Am Thorac Soc. 2017;14:230–237. doi: 10.1513/AnnalsATS.201605-398OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Angus DC, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Iwashyna TJ, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Med Care. 2014;52:e39–43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents’ long-term care histories(*) Health Serv Res. 2011;46:120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Render ML, et al. Veterans Affairs intensive care unit risk adjustment model: validation, updating, recalibration. Crit Care Med. 2008;36:1031–42. doi: 10.1097/CCM.0b013e318169f290. [DOI] [PubMed] [Google Scholar]
- 11.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 13.Friedman J, Hastie T, Tibshirani R SpringerLink (Online service) The Elements of Statistical Learning Data Mining, Inference, and Prediction. 2009. [Google Scholar]
- 14.Abadie A. Semiparametric Difference-in-Difference Estimators. Review of Economic Studies. 2005;72:1–19. [Google Scholar]
- 15.Baum CF. Modeling Proportions. Stata J. 2008:299–303. [Google Scholar]
- 16.Wang T, et al. Subsequent infections in survivors of sepsis: epidemiology and outcomes. J Intensive Care Med. 2014;29:87–95. doi: 10.1177/0885066612467162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prescott HC, Langa KM, Iwashyna TJ. Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA. 2015;313:1055–1057. doi: 10.1001/jama.2015.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun A, et al. Association between Index Hospitalization and Hospital Readmission in Sepsis Survivors. Crit Care Med. 2015 doi: 10.1097/CCM.0000000000001464. [DOI] [PubMed] [Google Scholar]
- 19.Zielske J, Bohne S, Brunkhorst FM, Axer H, Guntinas-Lichius O. Acute and long-term dysphagia in critically ill patients with severe sepsis: results of a prospective controlled observational study. Eur Arch Otorhinolaryngol. 2014 doi: 10.1007/s00405-014-3148-6. [DOI] [PubMed] [Google Scholar]
- 20.Corrales-Medina VF, et al. Association Between Hospitalization for Pneumonia and Subsequent Risk of Cardiovascular Disease. JAMA. 2015;313:264–264. doi: 10.1001/jama.2014.18229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ou SM, et al. Long-Term Mortality and Major Adverse Cardiovascular Events in Sepsis Survivors. A Nationwide Population-based Study. Am J Respir Crit Care Med. 2016;194:209–217. doi: 10.1164/rccm.201510-2023OC. [DOI] [PubMed] [Google Scholar]
- 22.Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;190:62–69. doi: 10.1164/rccm.201403-0471OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu V, et al. Hospital readmission and healthcare utilization following sepsis in community settings. J Hosp Med. 2014;9:502–507. doi: 10.1002/jhm.2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quartin AA, Schein RM, Kett DH, Peduzzi PN. Magnitude and duration of the effect of sepsis on survival. Department of Veterans Affairs Systemic Sepsis Cooperative Studies Group. JAMA. 1997;277:1058–1063. [PubMed] [Google Scholar]
- 25.Prescott HC, Osterholzer JJ, Langa KM, Angus DC, Iwashyna TJ. Late mortality after sepsis: propensity matched cohort study. BMJ. 2016;353:i2375–i2375. doi: 10.1136/bmj.i2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.