Abstract
Background: Peripheral neuropathy (PN) is defined as damage to the peripheral nervous system caused by a primary lesion or dysfunction. Multiple recent trials have suggested that acupuncture is beneficial for treating neuropathic pain. One challenge in acupuncture research is the lack of standardization of point selection, number of needles used, needle-retention time, needling depth, amount of needle manipulation, and use of moxibustion and electroacupuncture (EA).
Objectives: This article presents a standardized acupuncture protocol for the treatment of PN that incorporates structural acupuncture principles based on proximity to peripheral nerves and on traditional approaches to the treatment of neuropathic pain.
Materials and Methods: Ten consecutive patients diagnosed with large- or small-fiber neuropathy of various etiologies were treated with a standardized protocol, based on anatomical correlations of peripheral nerves and acupuncture points. Manual acupuncture was applied to left LR 4, LU 5; bilateral LI 11, KI 27, ST 36, GB 34, SP 6, SP 9, LI 4, TE 5, and BaFeng (except for the space between the first and second digits of the toes; LR 3 was used for that space). EA was applied to bilateral KI 3–1 and bilateral ST 41–LR 3. Patients underwent at least six acupuncture sessions, although the total number of sessions varied. Outcomes were measured using a visual analogue scale (VAS) and clinical signs and symptoms.
Results: All 10 patients indicated improvement on the VAS and in clinical presentation.
Conclusions: This standardized protocol appears to be effective for the treatment of neuropathy of various causes, including large- and small-fiber involvement. Further studies with larger sample sizes and randomized comparisons against sham acupuncture and other acupuncture regimens will be helpful to determine if this protocol could be established as a guideline for approaching peripheral neuropathy.
Keywords: : electroacupuncture, neurologic disorders, pain management, neuropathic pain, manual acupuncture
Introduction
Peripheral neuropathy (PN) is broadly defined as damage to the peripheral nervous system caused by a primary lesion or dysfunction.1 Polyneuropathy involves multiple nerves and mononeuropathy involves a single nerve. The most common causes of polyneuropathy are diabetes, thyroid disorders, vitamin B12 deficiency, alcohol abuse, chemotherapy, HIV infection, and hereditary factors.1–3 In spite of exhaustive workups, no cause is identified in one-third of PN cases, and they are considered to be idiopathic.3,4
Studies starting in the 2000s have showed acupuncture to be effective in the treatment of diabetic PN5–9 and human immunodeficiency virus–related PN.9–12 Acupuncture has been shown in multiple trials to reduce neuropathic pain5–9,11–16 and to improve nerve-conduction–study parameters5,8,13,16 significantly more than control treatments.
One challenge of acupuncture research is the lack of standardization of point selection, number of needles used, needle-retention time, needling depth, amount of needle manipulation, and use of moxibustion and electroacupuncture (EA). Treatment regimens vary widely, and there is no clear concept of an appropriate dose of acupuncture and how much treatment is needed for a given medical condition.
This article presents a standardized acupuncture protocol for the treatment of PN, which incorporates structural acupuncture principles based on proximity to peripheral nerves and traditional approaches to the treatment of neuropathic pain.
Materials and Methods
Patients
This was a retroactive chart review of patients treated for PN of various etiologies at the Neurology Wellness Clinic at Oregon Health and Science University, in Portland, OR, during the period of January 2014–August 2016. All patients treated during this time period, who underwent a minimum of 6 acupuncture sessions, were included. All patients had neuropathic pain, and numbness or paresthesias in the arms and legs, in a typical stocking-and-glove pattern, in addition to other neuropathic symptoms. This case series was exempt from institutional review board submission, as data were presented without any subject identifiers and the series represented a chart review intended for educational purposes.
Acupuncture Protocol
Acupuncture was performed by the present author (a trained medical acupuncturist), using sterile single-use MAC acupuncture needles (0.22 × 25 mm; TianJin Haing Lim Sou Won Medical Equipment Co, Ltd., South Korea). Manual acupuncture was administered for 25 minutes. EA was performed using an Electrostimulator 6c.Pro (Pantheon Research, Venice, CA). EA frequency was set to 100-Hz continuous stimulation. Stimulus intensity was increased every 5–7 minutes as needed, titrated to a patient-perceived intensity of 5–6/10. EA was administered for 25 minutes.
All patients were treated with the following acupuncture protocol:
Manual acupuncture: Left LR 4, LU 5; bilateral LI 11, KI 27, ST 36, GB 34, SP 6, SP 9, LI 4, TE 5, and BaFeng (except for the space between the first and second digits of the toes; LR 3 was used).
Electroacupuncture: Bilateral KI 3–1; bilateral ST 41–LR 3 (Figs. 1–4). Needles were connected to the EA machine leads as follows:
• Lead 1: KI 3 (red/anode clip)–KI 1 (black/cathode clip)–right foot
• Lead 2: ST 41 (red clip)–LR 3 (black clip)–right foot
• Lead 3: KI 3 (red clip)–KI 1 (black clip)–left foot
• Lead 4: ST 41 (red clip)–LR 3 (black clip)–left foot.
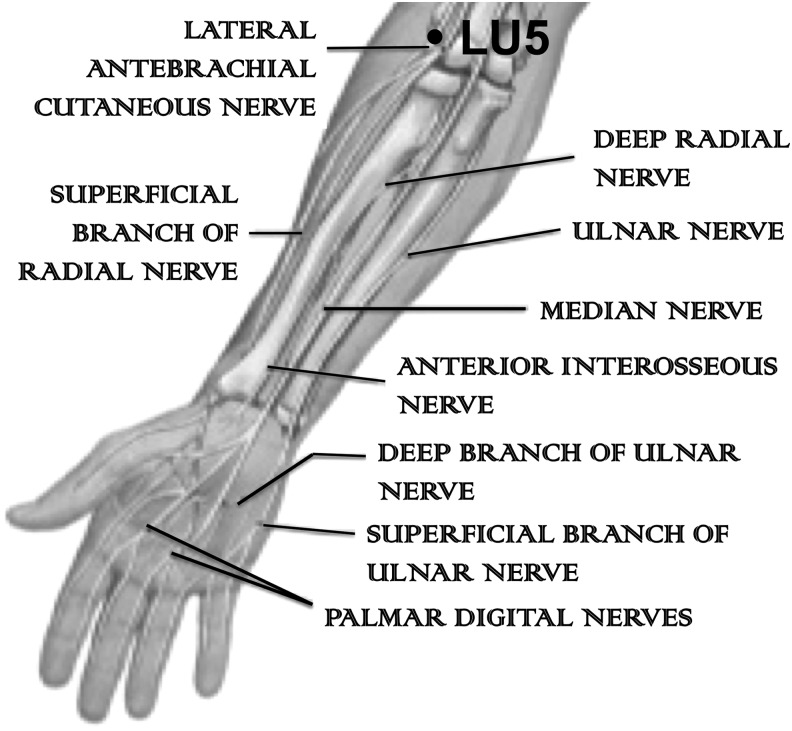
FIG. 1.
Anterior arm.
FIG. 2.
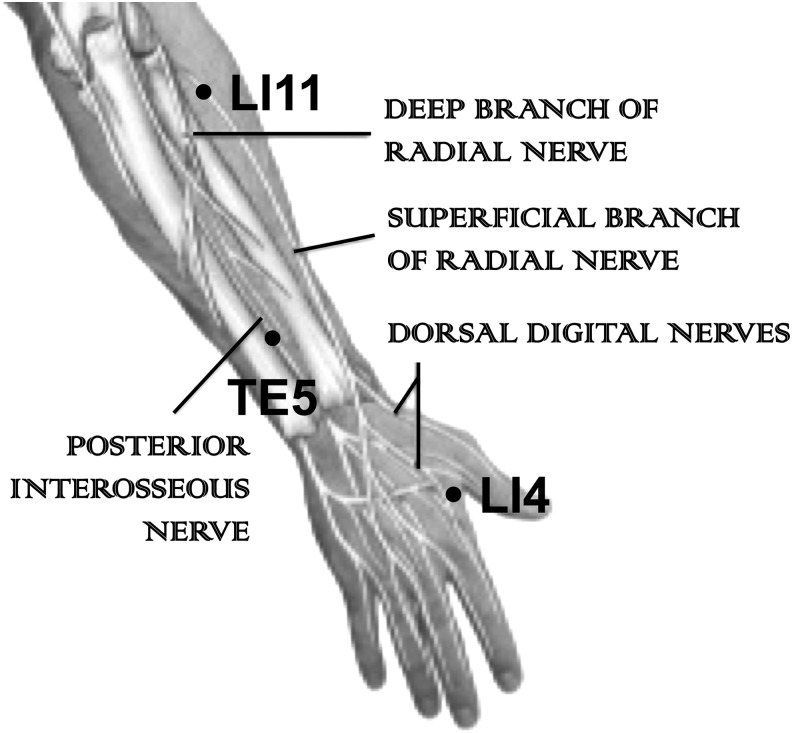
Posterior arm.
FIG. 3.
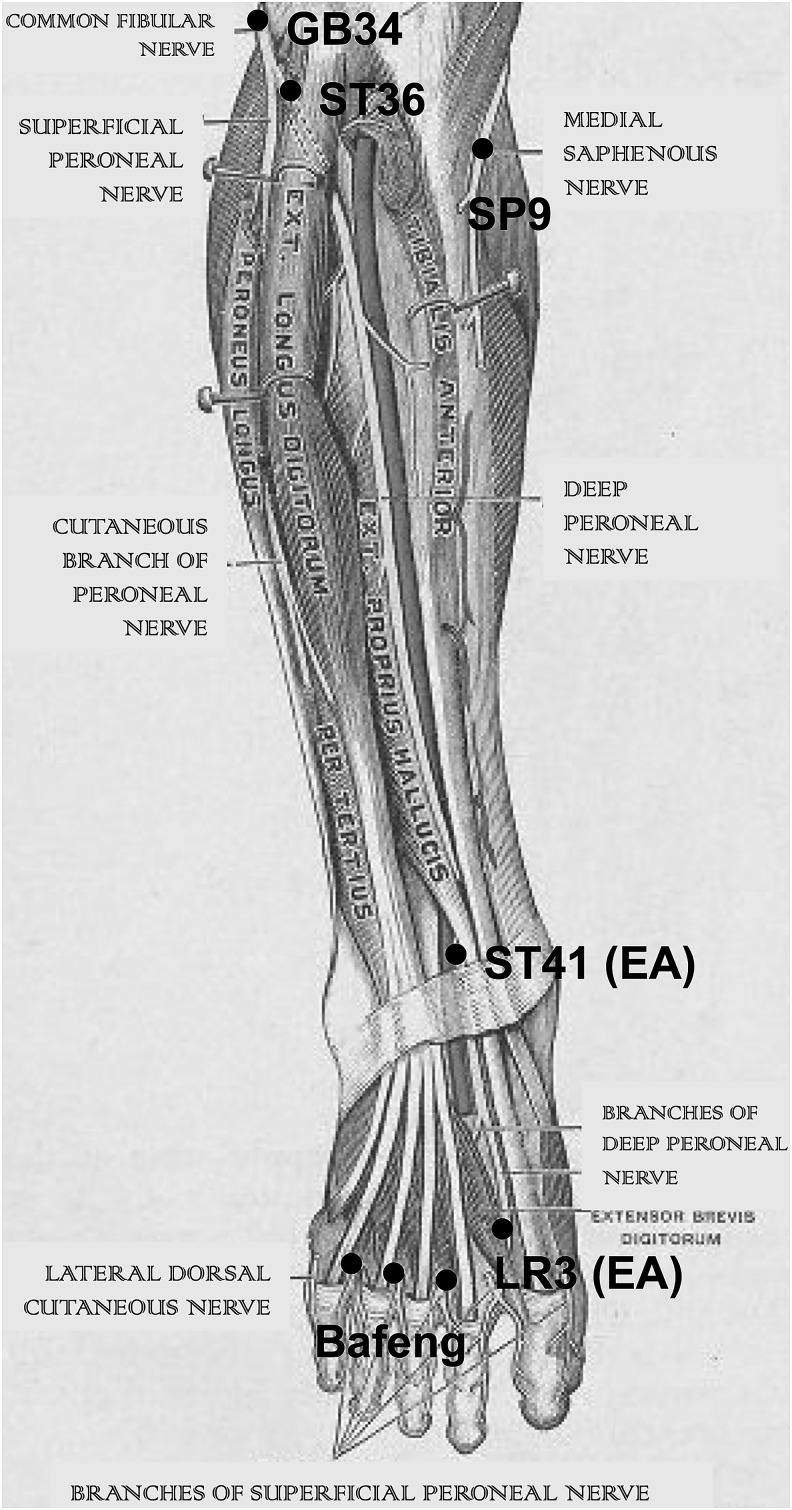
Anterior leg.
FIG. 4.
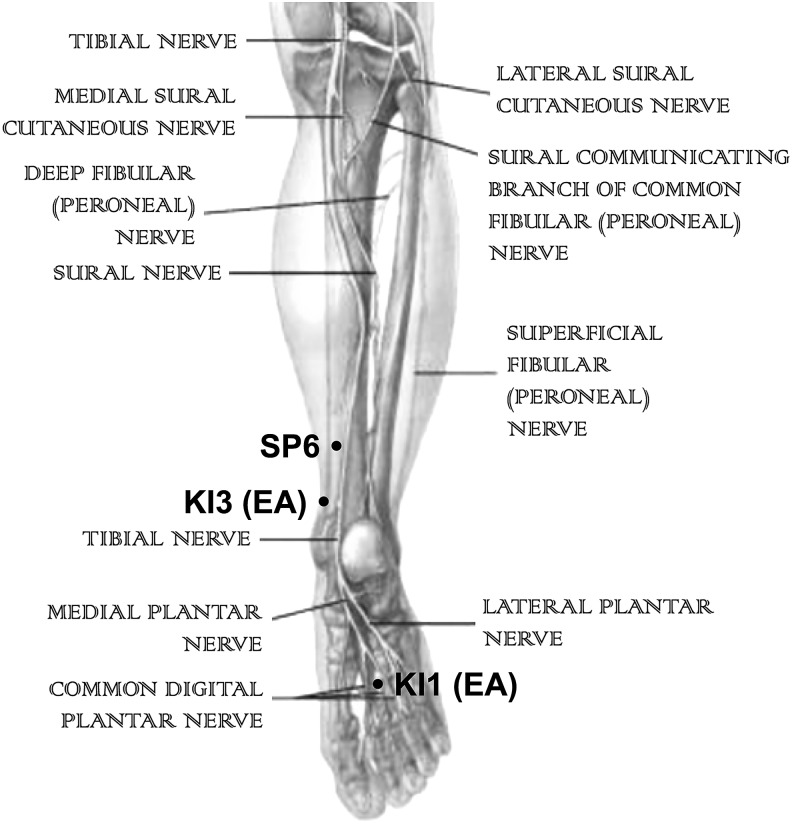
Posterior leg.
Assessment Methods
Patients were assessed at the beginning of each acupuncture appointment with a visual analogue scale (VAS), for indicating pain, and open-ended questions about symptoms and deficits.
Cases
Patient 1—a 24-Year-Old Woman with Idiopathic Small-Fiber Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of anxiety, depression, asthma, and gastroesophageal reflux disease. At age 15, she had developed symptoms consisting of increased skin sensitivity, imbalance, and spells of diffuse weakness, as well as experiencing “creepy-crawly” feelings over the shoulders, down the arms, in the thoracic paraspinal areas, in the left hip, down both legs, and in the feet. These symptoms were most bothersome at night, interfering with sleep. She described her baseline discomfort as 3–4/10 on the VAS, with a peak intensity up to 7–8/10. Her neurologic examination revealed normal bulk and tone; full-power strength throughout; sensation intact to light touch, proprioception, pinprick, and vibration, with normal 2+ reflexes throughout; absent Babinski responses; a normal gait; and normal cerebellar examination results.
Diagnostic workup
The patient underwent an extensive workup, consisting of a normal 2-hour glucose tolerance test; tests for antinuclear antibodies (ANAs), anticytoplasmic antibodies (ANCAs, proteinase-3, myeloperoxidase); a paraneoplastic panel; tests for Sjögren's syndrome antibodies (Sjögren's syndrome [SS]70A, SSB), topoisomerase I (scleroderma [SCL]-70), smooth-muscle, histidyl-tRNA synthetase (Jo-1), centromere, and ribonucleoprotein (RNP) antibodies; a celiac-disease panel; a Lyme disease panel; and tests for copper levels, creatine kinase (CK), methylmalonic acid (MMA), vitamins (B1, B6, B12, E), and angiotensin-converting enzyme. She had mildly reduced serum immunoglobulins A and G, as well as a mildly elevated rheumatoid factor—all of which were considered noncontributory. Urine heavy-metal levels were normal. This patient also underwent a nerve conduction study (NCS) in 2006 of the left arm and left leg and an NCS/electromyography (EMG) of the right leg in 2010, both of which were negative for large-fiber neuropathy. Autonomic testing revealed abnormal quantitative sudomotor autonomic reflex testing results, but no other evidence of dysautonomia. An abdominal fat pad biopsy was negative for amyloid and magnetic resonance imaging (MRI) of the brain and cervical, thoracic, and lumbar spine were unremarkable (Table 1).
Table 1.
Diagnostic Information
| Pt. # | Age | Sex | Diagnosis | Symptom duration | Diagnostic workup | EMG findings | Failed treatments |
|---|---|---|---|---|---|---|---|
| 1 | 24 | F | Idiopathic small-fiber neuropathy | 9 years | Serologic testing Urine heavy metals Abdominal fat pad biopsy MRI of brain & of cervical, thoracic & lumbar spine |
(1) NCS of left arm & leg Unremarkable (2) NCS/EMG of right leg Unremarkable |
Gabapentin: 2400 mg daily Methylprednisolone: 1 g 1–2-day course, 1–4 times per year, × 7 years Nortriptyline: 30 mg nightly Citalopram: 20 mg daily Hydrocodone/acetaminophen: 5–500 prn |
| 2 | 43 | M | Idiopathic small-fiber neuropathy | 20 years | Serologic testing |
(1) NCS of left arm & leg Normal, with mildly prolonged peak latency of sural nerve, attributed to cold temperature (2) NCS/EMG of left arm & leg Normal sural latency; no evidence of large-fiber neuropathy |
Gabapentin: 300 mg daily Tramadol: 50 mg every 6 hours prn Vitamin E: Daily |
| 3 | 45 | M | Idiopathic small-fiber neuropathy | 10 months | Serologic testing CSF testing MRI of brain, & of cervical, thoracic & lumbar spine |
(1) NCS/EMG of right arm & leg No evidence of large-fiber neuropathy |
Gabapentin: 2700 mg daily, Amitriptyline: 75 mg at bedtime |
| 4 | 52 | F | Length-dependent axonal sensorimotor neuropathy & limited autonomic neuropathy | 4 years | Serologic testing Autonomic testing |
(1) NCS/EMG of left arm & leg Mild, axonal, length-dependent sensorimotor peripheral neuropathy |
Alpha-lipoic acid: Twice daily Vitamin E: Daily |
| 5 | 56 | M | Idiopathic small-fiber neuropathy | 6.5 years | Serologic testing MRI of cervical spine |
(1) NCS/EMG of right arm Negative for neuropathy or radiculopathy |
Gabapentin: 1800 mg daily Hydrocodone/acetaminophen: 5/300 mg daily prn Duloxetine: 60 mg daily Amitriptyline: 25 mg at bedtime |
| 6 | 57 | F | Idiopathic small-fiber neuropathy | 2 years | Serologic testing |
(1) NCS/EMG of left arm & leg No evidence of large-fiber neuropathy |
Alpha-lipoic acid: Twice daily Vitamin E: Daily |
| 7 | 58 | M | Length-dependent axonal sensorimotor neuropathy & idiopathic small-fiber neuropathy | 1 year & 9 months | Serologic testing Skin biopsy Autonomic testing, QST MRI of cervical & lumbar spine |
(1) NCS/EMG of left arm & leg Length-dependent sensorimotor axonal neuropathy |
Gabapentin: 2700 mg daily Alpha-lipoic acid: Twice daily Vitamin E: Daily |
| 8 | 64 | M | Anti-MAG neuropathy | 6 years | Serologic testing CSF testing |
(1) NCS/EMG of right arm & leg Very severe sensory predominant sensorimotor polyneuropathy |
IVIG: (4-day course) for 3 months Plasmapheresis: × 3 over 3 months Rituximab: 3 courses Gabapentin: 3600 mg daily Pregabalin: 600 mg daily Duloxetine: 60 mg daily Tramadol: 50 mg q6h as needed |
| 9 | 67 | M | Idiopathic small-fiber neuropathy | 7 years | Serologic testing Skin biopsy |
(1) NCS/EMG of left arm & leg Mild bilateral carpal tunnel syndrome; no evidence of large-fiber neuropathy |
Gabapentin: 2700 mg daily Alpha-lipoic acid: Twice daily, Coenzyme Q10 and vitamin E: daily Gluten-free & lactose-free diet: Ongoing |
| 10 | 69 | M | Length-dependent axonal sensorimotor neuropathy | 3 years | Serologic testing Autonomic testing |
(1) EMG × 2 Length-dependent, sensorimotor, axonal peripheral neuropathy |
Gabapentin: 1800 mg daily Oxycodone: 5 prn as needed at bedtime |
Pt., patient; EMG, electromyography; F, female; M, male; MRI, magnetic resonance imaging; NCS, nerve conduction study; prn, pro re nata (as needed); CSF, cerebrospinal fluid, QST, quantitation sensory testing; MAG, myelin-associated glycoprotein; IVIG, intravenous immunoglobulin.
Past treatments
The patient had been prescribed up to 2400 mg of gabapentin daily without effect, and she underwent 1-or 2-day courses of 1 g of intravenous (IV) methylprednisolone 1–4 times a year. This regimen was effective for symptom reduction over the first 3–4 years; however, over time, she required 2-day courses with increased frequency, as the benefits diminished. At the onset of acupuncture therapy, this patient was taking 30 mg of nortriptyline nightly, 20 mg of citalopram daily (for depression), and 5–500 mg of hydrocodone/acetaminophen 2–3 times daily as needed.
Acupuncture course
The patient underwent 14 sessions over a 17-week period as an initial treatment course, followed by maintenance treatment, consisting of 9 sessions over a 34-week period (once every 3–4 weeks on average) and 3 additional sessions, which were 2 months apart. Following this, she was discharged from the clinic. The standard neuropathy protocol was administered each time, in addition to EA to ST 41–GB 34 and back treatment, consisting of manual acupuncture and EA, which were administered in more than 50% of the sessions. See Table 2 for details.
Table 2.
Treatments
| Pt. # | Age | Sex | Diagnosis | Tx course | Sessions/week | Maintenance course | Baseline VAS pre-Tx | Peak VAS pre-Tx | VAS post-Tx | Summary of other points used |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 24 | F | Idiopathic small-fiber neuropathy | 14 sessions over 17 weeks | 0.82 | 12 sessions over 13 months | 3–4/10 | 7–8/10 | 0/10 | EA to ST 41–GB 34 Back treatment: EA to bilateral GB 21–SI 14, SI 12–9, BL 32–38, BL 27, 28, 37, Huato T-1–T-4 & Huato L-5–GB 30 MA to right GB 20, GV 12,14, bilateral GB 21, Huato C5-7, T2-3, T10-11 |
| 2 | 43 | M | Idiopathic small-fiber neuropathy | 10 sessions over 11 weeks | 0.91 | ___ | 3/10 | 7/10 | 1/10 | 3 of the 10 visits with different acupuncturist for low-back pain |
| 3 | 45 | M | Idiopathic small-fiber neuropathy | 12 sessions over 18 weeks | 0.67 | ___ | 8/10 | 9–10/10 | 4/10 |
Back treatment: MA to right GB 20, GV 7, 8 & 1; & bilateral GB 21, LI 11,15 & BL 40–58–60 |
| 4 | 52 | F | Length-dependent axonal sensorimotor neuropathy | 12 sessions over 19 weeks | 0.63 | Ongoing | 2–3/10 | 6–7/10 | 1/10 | EA to bilateral PC 3–6 |
| 5 | 56 | M | Idiopathic small-fiber neuropathy | 10 sessions over 13 weeks | 0.77 | ___ | 5/10 | 9/10 | 2–3/10 | MA to bilateral Baxie & left shoulder Ah Shi points |
| 6 | 57 | F | Idiopathic small-fiber neuropathy | 6 sessions over 9 weeks | 0.67 | ___ | 2/10 | 4/10 | 1/10 | EA to bilateral Bafeng |
| 7 | 58 | M | Length-dependent axonal sensorimotor neuropathy & idiopathic small-fiber neuropathy | 16 sessions over 24 weeks | 0.67 | 8 sessions over 10.5 months | 1–2/10 | 6–7/10 | 0/10 | EA to bilateral SP 5–9, KI 6–SP 9, KI 1–ST 36 & ST 36–41 Back treatment: MA to right GB 20, GB 21, LI 14, LU 1, GV 12 & GV 14 |
| 8 | 64 | M | Anti-MAG neuropathy | 25 sessions over 37 weeks | 0.68 | ___ | 7–8/10 | 10/10 | 4–6/10 | EA to bilateral ST 41–GB 34 Back treatment: MA to GV 12; GV 14; & bilateral LI 14, LI 5, BL 40–58–60, BL 52, GB 25, ST 10 & right GB 20 |
| 9 | 67 | M | Idiopathic small-fiber neuropathy | 12 sessions over 17 weeks | 0.70 | 6 sessions over 3.5 months | 3–4/10 | 6–7/10 | 0–1/10 | EA to bilateral ST 41–ST 36 |
| 10 | 69 | M | Length-dependent axonal sensorimotor neuropathy | 24 sessions over 40 weeks | 0.60 | ___ | 5–6/10 | 8/10 | 1–3/10 | EA to bilateral Baxie points, ST 41–GB 34 & ST 41–36 Back treatment: MA to right GB 20, Huato C-5–7, T-2–3, GV 12, GV 14, BL 40–58–60 & bilateral GB 21 & trapezius dry needling/trigger pointing |
Tx, treatment; VAS, visual analogue scale; EA, electroacupuncture; MA, manual acupuncture; M, male; F, female; MAG, myelin-associated glycoprotein.
Clinical course
The patient experienced a gradual reduction in severity of paresthesias over the initial 17-week treatment course. She stopped taking 5–500 mg of hydrocodone/acetaminophen after 3 sessions and the nortriptyline after 6 sessions. During the maintenance treatment phase, she only experienced occasional “crawly” sensations; and burning in the feet, upper back, shoulders, and posterior thighs. Those only occurred for 6–7 weeks and responded well to a single maintenance session. Eventually, all symptoms resolved, and she was discharged from the clinic. She described her pain level on the VAS as 0/10.
Patient 2—a 43-Year-Old Man with Idiopathic Small-Fiber Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of hypertension, hyperlipidemia, and degenerative disc disease with low-back pain. He presented to the present author's clinic with painful leg paresthesias. He had first noticed numbness and tingling in the toes ∼20 years prior. The symptoms had progressed to burning paresthesias and ascended to the left distal thigh and below the right knee 5 years prior. In addition, 1.5 years prior his symptoms had worsened significantly and, on presentation, he felt as if his feet were in ice water or were burning. Other complaints included weakened handgrips, bilateral paresthesias in digits 1 and 2, sometimes in the forearms, and leg jerks that were worse at night. The patient described his baseline neuropathic pain intensity as 3/10, with a peak pain of 7/10. His neurologic examination was remarkable for vibratory loss at the great toes and decreased pinprick below the mid-shins bilaterally. Otherwise, he had normal bulk and tone, strength, full-power throughout, normal 2+ reflexes throughout, absent Babinski responses, and normal gait and cerebellar examination results.
Diagnostic workup
The patient underwent a serologic workup, which revealed unremarkable thyroid function, hemoglobin A1c (HgA1c), C-reactive protein, and magnesium test results. He also underwent an NCS of the left arm and leg in 1/2015, which produced normal results, except for a mildly prolonged peak latency of the sural nerve, which was attributed to the cold temperature in the environment. Repeat NCS/EMG in 6/2016 for worsening symptoms, again of the left arm and leg, were negative for large-fiber neuropathy, with normal sural latency (Table 1).
Past treatments
The patient was taking 100 mg of gabapentin three times daily, 50 mg of tramadol every 6 hours as needed for pain, and vitamin E daily.
Acupuncture course
He underwent 10 acupuncture sessions over 11 weeks, of which 7 were focused on neuropathy treatment and involved the standardized protocol without deviations. Three sessions were administered by a different acupuncturist and were focused on low-back pain. No maintenance treatments were performed due to loss of insurance coverage (Table 2).
Clinical course
Neuropathic pain was much reduced, was not bothersome, with transient and mostly painless paresthesias, which he rated as 1/10 on the VAS. He stopped tramadol and gabapentin. He reported improved sensation in the feet and reductions of the muscle spasms in his legs, especially at bedtime.
Patient 3—a 45-Year-Old Man with Idiopathic Small-Fiber Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of irritable bowel syndrome, post-traumatic stress disorder (PTSD), migraine, hypertension, and hyperlipidemia. He presented to the Wellness clinic for 10 months of progressive, painful, burning paresthesias in the feet and hands, which he rated as 8/10 on the VAS at baseline, up to 9–10/10 at times. Other complaints included feeling like his limbs were falling asleep, plantar and dorsiflexion weakness, and diffuse muscle spasms. His motor examination revealed normal bulk and tone, no abnormal movements, full-strength 5/5 throughout, except for left finger opposition weakness 4/5. There was reduced sensation to light touch and pinprick in the hands and below the mid-calves in a stocking-and-glove distribution. Proprioception and vibration were intact. Reflexes were 1+ throughout, Babinski reflexes were absent, and coordination and gait were intact.
Diagnostic workup
Serologic testing revealed normal results on HgA1c, vitamin B12 levels, serum protein electrophoresis (SPEP), ANA, SSA, SSB, SCL-70, smooth muscle, Jo-1, centromere, RNP and anti-ganglioside GM1 antibodies, and a celiac disease panel; he also tested negative for HIV. MRI of the brain and entire spine was unremarkable. Cerebrospinal fluid analysis revealed mildly elevated protein at 64 mg/dL (normal <60), otherwise there were unremarkable basic studies. NCS/EMG in 1/2015 of the right arm and leg was without evidence of peripheral neuropathy, radiculopathy, or myopathy (Table 1).
Past treatments
He was taking 900 mg of gabapentin three times daily and 75 mg of amitriptyline at bedtime.
Acupuncture course
The patient underwent 12 acupuncture sessions over 18 weeks. The neuropathy protocol was used each time, with additional back treatment in about 1/3 of the sessions (Table 2). Maintenance treatment was not administered because only 12 treatments were covered by insurance.
Clinical course
After 12 sessions, he reported a baseline pain level reduction to 4/10 on the VAS and he lowered his gabapentin dose to 400 mg three times daily.
Patient 4—a 52-Year-Old Woman with Length-Dependent Axonal Sensorimotor Neuropathy and Limited Autonomic Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of early menopause, constrictive pericarditis attributed to mononucleosis, saphenous vein stripping in 2002, hypothyroidism, and sick sinus syndrome. She had presented to the Wellness clinic for 4 years with progressive numbness in the feet with painful hyperesthesias in the soles. Other symptoms included touch-induced, electric “zapping” sensations in the calves, thighs, hips, and lower back. Over the last 6 months, she had begun to experience occasional hand numbness and tingling. Her baseline neuropathic pain level was 2–3/10 on the VAS, with exacerbations reaching 6–7/10. Her examination revealed normal bulk, tone, and motor strength. There was decreased sensation to light touch in the hands and toes bilaterally, decreased pinprick in the toes, hyperesthesia in the feet, and decreased vibration in the left great toe. Proprioception was intact; so were coordination and gait. Reflexes were brisk throughout, and Babinski responses were absent.
Diagnostic workup
Serologic testing revealed normal results on tests for HgA1c, vitamin B12, SPEP, MMA, SSA, SSB, SCL-70, smooth muscle, Jo-1, centromere, RNP antibodies, thyroperoxidase, and thyroglobulin antibodies; on a celiac-disease panel; negative for HIV; a serum paraneoplastic panel; and an auto-immune dysautonomia panel. A thyroid panel in 1/2016 was notable for low thyroid-stimulating hormone (TSH), prompting her primary care provider to adjust the patient's thyroid medication. Subsequent TSH and free T4 in 2/2016 were within normal limits. Vitamin B6 levels were elevated at 273.2 nmol/L (nL <125), in the absence of supplemental use. EMG of the left arm and leg in 2/2016 revealed a mild, axonal, length-dependent peripheral neuropathy. Autonomic function testing results in 2/2016 were consistent with limited autonomic neuropathy (Table 1).
Past treatments
The patient was reluctant to take any neuropathic pain medication. She had been only treated with daily vitamin E and twice-daily alpha-lipoic acid.
Acupuncture course
Acupuncture consisted of 12 sessions over a 19-week period. The only deviation was administration of high-frequency EA to the Pericardium Meridian (Table 2).
Clinical course
Pain in the feet resolved, with only occasional painful paresthesias, which she rated as 1/10. She was able to walk barefoot for the first time in years and felt some reduction in the numbness of her hands and feet.
Patient 5—a 56-Year-Old-Man with Idiopathic Small-Fiber Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of PTSD, depression, fibromyalgia, frozen shoulder on the right, left shoulder pain, headaches, gluten intolerance, hypothyroidism, current smoking, past alcohol abuse (quit 10 years prior), hypertension, and hyperlipidemia. He had presented to the Wellness Clinic for 6.5 years with progressive bilateral hand and foot pain, which was most acute in the sole pads, toes, and ankles. For him, walking felt like stepping on hot sand/hot asphalt or like feeling multiple paper cuts to the feet. He also had a right arm tremor since 2008, which had been diagnosed as neuropathic. The patient rated his baseline pain level as 5/10 on the VAS, with levels reaching 9/10 during exacerbations. He had normal bulk, tone, and motor strength. There was an essential tremor in both hands, which greater in the right hand. There was decreased sensation to light touch in the hands and feet bilaterally and a decreased response to a pinprick in the right lateral arm, but hyperesthesia to pinpricks in the fingertips. Vibration and proprioception were intact. Reflexes were 1+ throughout and Babinski responses were absent. Coordination and gait were intact, but there was an intention tremor when performing the finger–nose–finger test.
Diagnostic workup
Serologic testing revealed normal vitamin B12 and TSH levels with elevated free T4; slightly elevated HgA1c at 5.8 (normal is under 5.7); normal SSA, SSB, SCL-70, smooth muscle, Jo-1, centromere, RNP antibodies; negative celiac panel results, normal SPEP. EMG of the right arm in 2008 was negative for neuropathy or radiculopathy. MRI of the cervical spine showed multilevel degenerative changes with right C-6 nerve impingement and right C-7 rootlet compression; also, a 5-mm cyst at C-7 was present on the left side (Table 1).
Past treatments
The patient was taking 5 mg of hydrocodone/300 mg acetaminophen daily, 600 mg of gabapentin three times daily, 60 mg of duloxetine daily, and 25 mg of amitriptyline at bedtime.
Acupuncture course
Acupuncture consisted of 10 sessions over a 13-week period, after which the patient ran out of acupuncture coverage. The neuropathy protocol was used each time. In addition, the patient received manual acupuncture to bilateral Baxie and left shoulder Ah Shi points (Table 2).
Clinical course
Following treatment, the burning paresthesias in his feet was reduced greatly, with an intensity change from severe to mild, which he rated as 2–3/10 on the VAS. His left shoulder pain was reduced as well. The patient also reported having more energy and being more active, which, for him, meant being able to work more on his garden.
Patient 6—a 57-Year-Old Woman with Idiopathic Small-Fiber Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of benign paroxysmal positional vertigo and malignant melanoma of the thumb, requiring partial amputation. She had presented with 2 years of progressively worsening numbness and paresthesias in the toes and in the balls of her feet, which were worse at night. At baseline, she rated her pain as 2/10 on the VAS, with occasional flareups to 4/10 on the VAS. Her examination revealed normal bulk and tone and strength full power throughout. There was loss of light touch in the toes and loss of vibratory sense in the great toes bilaterally. Pinprick and proprioception were intact. Reflexes were 2+ and symmetric throughout. The remainder of her examination was unremarkable.
Diagnostic workup
Serologic testing revealed normal vitamin B6 and B12 levels; an HgA1c of 5.8, consistent with prediabetes, which normalized to 5.6 on repeat; normal thyroid study results and SPEP. EMG of the left arm and leg in July of 2015 was unremarkable and ruled out large-fiber neuropathy (Table 1).
Past treatments
The patient took 500 mg of alpha-lipoic acid twice daily and 400 international units (IU) daily of vitamin E, and obtained some relief.
Acupuncture course
Acupuncture consisted of 6 sessions over 9 weeks. The neuropathy protocol was used each time. In addition the patient received EA to bilateral BaFeng points, instead of KI 3–KI 1, because she could not tolerate KI 1 needling (Table 2).
Clinical course
She reported improved sensation in the toes and diminished paresthesias. She rated her neuropathic pain as 1/10 on the VAS.
Patient 7—a 58-Year-Old-Man with Length-Dependent Sensorimotor Axonal Neuropathy and Small-Fiber Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of hyperlipidemia. He was assessed for a 1-year-and-9-month history of progressive, painful paresthesias in the feet that were worse with walking and running. Other complaints included cramps in the calves and thighs that were worse with activity and at night. He rated his neuropathic pain as 1–2/10 on the VAS at baseline, with exacerbation up to 6/10. His examination revealed normal bulk and tone and full-power strength throughout. There was loss of light touch below the left shin and below the right ankle, in a stocking pattern; decrease of pinprick sensation in the distal left foot with hyperesthesia in the toes in the left and right; and decrease of vibration sensation in the great toes bilaterally. Proprioception was intact. Gait and coordination were unremarkable. Reflexes were 1+ throughout with “downgoing” toes, with the exception of an absent left Achilles reflex.
Diagnostic workup
Serologic workup included normal vitamin B12, TSH, erythrocyte sedimentation rate (ESR), serum glucose, SPEP levels; normal ANA titers, anti–neutrophil cytoplasmic antibodies; and normal celiac-disease panel results. EMG of the left arm and leg in February 2013 revealed length-dependent sensorimotor axonal neuropathy. MRI of the cervical and lumbar spine showed disc bulges and mild degenerative changes. The patient underwent autonomic testing, which produced abnormal results due to neurogenic orthostatic hypotension and borderline reduction in the sweat response only in the proximal leg. Quantitative sensory testing revealed an increased cooling threshold in the hand. This prompted a skin biopsy, which was diagnostic for small-fiber neuropathy due to significantly reduced epidermal nerve fiber density in the ankle, but not in the thigh (Table 1).
Past treatments
The patient took 1800 mg of gabapentin daily, 600 mg of alpha-lipoic acid twice daily, and 400 IU of vitamin E daily.
Acupuncture course
Acupuncture consisted of 24 sessions over a period of 1.5 years. The patient underwent 10 weekly sessions, followed by 4 biweekly sessions, 2 sessions 3 weeks apart, 4 monthly sessions, 3 sessions 6 weeks apart, and a final session 3½ months later. The neuropathy protocol was followed during each session. During 25% of sessions, the patient received additional treatments, which included: EA to SP 5 and 9 bilaterally; KI 6–SP 9 bilaterally; KI 1–ST 36 bilaterally; ST 41–ST 36 bilaterally; back treatment to GV 14 and GV 12, using 3 needles each, with manipulation to right GB 20, right GB 21, right LI 15, right LU 1 (Table 2).
Clinical course
After 3 sessions, the patient reported reduced pain and ability to stand longer. He started lifting weights and walking more. After 7 sessions, he was back to jogging and his pain continued to be reduced. He started tapering off gabapentin. His pain resolved completely after 10 sessions, with only residual numbness. By the end of treatment, the patient was taking only daily vitamin E, remained pain-free, and experienced minimal numbness in the feet. His cramping was much reduced as well.
Patient 8—a 64-Year-Old-Man with Anti-Myelin-Associated Glycoprotein Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of hypertension and obesity. He presented with 6 years of progressively worsening foot and calf numbness and painful paresthesias in the feet, up to the thighs and in the fingertips; weakness noted on getting up from seated position; and tremor in both arms. Over the past year he had experienced balance difficulty and was on disability from his job as a mechanic. His symptoms interfered with sleep, both due to inability to fall asleep and to waking up at night. He rated his pain as 7–8/10 on the VAS at baseline, with frequent exacerbations causing 10/10 pain.
His examination revealed normal bulk and tone, weakness consisting of decreased rapid finger taps bilaterally that was worse on the right. There was coarse action tremor in both hands, which was worse on the left (dominant). There was a significant decrease in light touch and pinprick in a stocking distribution to the upper thigh and proximal arms bilaterally. Vibration was impaired in the legs bilaterally, with only minimal vibration at the knees and elbows bilaterally. There was proprioceptive loss in the toes, ankles, and distal metacarpophalangeal joints bilaterally. Reflexes were absent throughout. Coordination showed impaired heel-to-shin test result, in proportion to his proprioceptive loss. His gait was wide-based and antalgic, with an inability to tandem and toe-walk.
Diagnostic workup
Serologic testing was diagnostic with an anti-MAG antibody titer of 12,800 (nL <600) and an anti-sulfoglucuronyl paragloboside antibody titer of 409,600 (nL <3200). SPEP testing revealed early monoclonal protein immunoglobulin M lambda. Other laboratory tests included normal vitamin B12, TSH, MMA levels; normal Lyme titers; normal ANA titers; and normal ESR, and CK. CSF chemistry, including total protein and blood count, was normal. Recent EMG revealed very severe sensory predominant sensorimotor polyneuropathy.
Past treatments
The patient had received one course of IVIG over 2 days, followed by monthly courses of IVIG (four daily treatments), with temporary stabilization of his symptoms on treatment days but no sustained benefit. He had severe post-treatment headaches. In addition, he underwent 3 monthly plasmapheresis treatments between October and December of 2009. In March 2010, he underwent a course of rituximab, with marked improvement and ability to return to work for over a year. A second course of rituximab in April 2012 was beneficial but not to the extent of the initial infusion, and symptomatic improvement lasted a few months. A third course of rituximab in July 2013 was ineffective. The patient had taken gabapentin up to a 3600-mg daily dose, which was changed to pregabalin 200 mg three times daily, due to ineffectiveness. He also took 60 mg of duloxetine daily and 50 mg of tramadol every 6 hours as needed.
Acupuncture course
Acupuncture consisted of 25 at least weekly sessions over 37 weeks. Interruptions in treatment were caused lapses in insurance coverage. He underwent the neuropathy regimen, with occasional additions of EA to ST 41–GB 34. He also received back treatments ∼20% of the time, involving GV 12 and GV 14; bilateral LI 15 and LI 4; right GB 20; bilateral BL 60, BL 58, and BL 40; bilateral ST 10; bilateral BL 52; and bilateral GB 25.
Clinical course
Acupuncture brought the most relief, with the exception of the first course of rituximab, which the patient thought was comparable. He rated his pain level following 25 sessions at an improved baseline of 4–6/10. He was able to sleep through the night, and his wife noticed that he was less irritable. He also reported walking better, with improved balance and improved movements and sensation in his toes. Unfortunately, treatments had to be discontinued due to loss of acupuncture benefits.
Patient 9—a 67-Year-Old-Man with Idiopathic Small-Fiber Neuropathy
Brief medical history and neurologic examination
The patient had a medical history of alcohol abuse (quit 3 years prior) and atrial fibrillation. He was assessed for 7 years of progressive burning paresthesias in both feet. Initially, he had noticed difficulty in walking on the beach; his feet felt numb and like he still had socks on. Over time, this had progressed to constant painful paresthesias that was worst over the balls of the feet. At baseline, he rated the paresthesia pain as 3–4/10 on the VAS, with exacerbations up to 7/10 at night. He could not walk on a cold floor without shoes, due to pain. His symptoms were limiting; he was an avid golfer and had needed to use a cart when playing, due to difficulty with walking. Other symptoms included painful cramping in the left calf, which woke him up from sleep. He denied any neck or back pain. He was on a self-imposed gluten-free and lactose-free diet, although admitted to cheating at times.
On neurologic examination, it was noted that he had normal bulk and tone, full strength throughout, and a slight postural tremor in both hands that was worse on the left. Sensation was intact to light touch, proprioception, and vibration, with reduced pinprick along the medial left thigh and medial left sole. Reflexes were normal 2+ throughout, with absent Babinski responses. Cerebellar examination results and gait were unremarkable.
Diagnostic workup
Serologic workup revealed normal levels of vitamin B12, TSH, and HgA1c; SPEP, complete blood count and blood chemistry, and liver function tests all produced normal results; his lupus titers, SSA, SSB, SCL-70, smooth muscle, Jo-1, centromere and RNP antibodies, and MMA were all normal.
A recent EMG revealed only bilateral mild–moderate carpal tunnel syndrome, without evidence of large-fiber neuropathy. An autonomic study was unremarkable, without evidence of small-fiber neuropathy; however there was a positive skin biopsy of the right ankle, which showed significant reduction in epidermal nerve-fiber density and was diagnostic for small-fiber neuropathy. Past alcohol abuse was the presumptive etiology (Table 1).
Past treatments
The patient was taking up to a 2700-mg daily dose of gabapentin, but could not tolerate this due to oversedation and reduced it to 900 mg daily. He was also taking 300 mg of alpha-lipoic acid twice daily, and vitamin E and coenzyme Q10 supplementation daily.
Acupuncture course
The patient underwent 12 acupuncture sessions over 17 weeks, followed by a 6-month break and a maintenance course of 6 sessions over 3.5 months. The standardized protocol was applied each time with the additional treatment of EA to ST 41–ST 36 bilaterally, during several sessions.
Clinical course
At the completion of the maintenance course, the patient reported minimal pain, at worst 1/10 on the VAS, with only occasional numbness in the feet. He was more active and was pleased that he was able to walk through a game of golf and wear golf shoes. His foot cramping resolved (Table 2).
Patient 10—a 69-Year-Old-Man with Axonal Length-Dependent Sensorimotor Neuropathy
Brief medical history and neurologic examination
The patient had a history of Wolff–Parkinson–White syndrome, psoriatic arthritis, hypertension, and knee-replacement surgery. He presented with 3 years of progressive burning paresthesias in the feet up to the shins and, more recently, similar sensations in the fingertips. These occurred following his knee- replacement surgery and became increasingly more painful, becoming worse in the evening. At times, he woke up at night due to severe pain. He rated the pain at baseline as 5–6/10 on the VAS, with exacerbations up to 8/10. He had difficulties with balance.
His neurologic examination showed that he had normal bulk and tone, no tremors, and full power, except for bilateral toe flexion 4+/5 and extension 4+/5. Light touch was decreased in the palms and from the midshin down bilaterally. Pinprick was reduced in the feet to about midshin, with hyperesthesia in the fingertips. Vibration was decreased in the toes bilaterally. Proprioception was intact bilaterally. Reflexes were absent at the biceps, brachioradialis, and Achilles bilaterally. Patellar reflexes were 1+ bilaterally, with “downgoing” toes. Coordination was normal and gait was antalgic, but steady.
Diagnostic workup
The patient underwent a diagnostic workup, consisting of a positive ANA titer at 1:320, with a homogenous pattern; an ESR of 21 (normal <15); normal antibody titers to SSA, SSB, SCL-70, smooth muscle, Jo-1, centromere, RNP, and anti-dole-stranded DNA; normal levels of complement C3 and C4; normal SPEP; normal copper and vitamin E and B6 levels; and normal HgA1c.
EMG in 2013 and 2014 revealed a length-dependent, sensorimotor, axonal peripheral neuropathy, which was worse in 2014. There was no evidence of autonomic neuropathy on autonomic testing (Table 1).
Past treatments
The patient was taking 1800 mg of gabapentin daily and 5 mg of oxycodone at bedtime, 1–2 times per week, on average. The patient had seen 2 prior acupuncturists—1 for 3 visits and another acupuncturist for 8 weeks.
Acupuncture course
The patient underwent 24 visits over 40 weeks. The standardized protocol was applied, with the addition of EA to bilateral Baxie points, EA to bilateral ST 41–GB 34, and bilateral ST 41–36. The patient also received back treatments involving bilateral GB 21; right GB 20; Huato Jiaji of C5-7, T2-3, GV 14, and GV 12; bilateral BL 58–40–60; and bilateral dry needling and trigger-pointing of the trapezius. These deviations occurred in about one-third of the treatments. The patient's pain was reduced to 1–3/10 on the VAS. His hand paresthesias resolved, and he reported improved sensation, minimal paresthesias in the feet, and improved balance. He stopped taking oxycodone (Table 2).
Discussion
The Case for Standardization
Acupuncture is practiced in a variety of ways and in various settings, using diverse styles such as traditional acupuncture, 5-Element theory, structural, microsystems, etc. Traditional acupuncture practice typically aims for individualized point selection, based on pathologic presentation assessed through history, pulse and tongue diagnostics, palpation, and other forms of physical examination. While this approach certainly has its merits and is a well-established way of practice, it is difficult to translate into Western practice paradigms. This individualization is even more problematic in the field of acupuncture research, when one considers standardized interventions and dose–response. To-date, there is no clear concept of an appropriate dose of acupuncture and how much treatment is needed for a given medical condition.17 The relationship between number of needles and acupuncture effect is also unclear and is probably not linear. Common standardization problems with acupuncture research and practice include varied point selection, number of needles used, needle-retention time, needling depth, amount of needle manipulation, and adjunct use of moxibustion and EA.
Peripheral neuropathy, particularly when it involves the large nerve fibers, is ideally suited for a localized structural needling approach. Needles placed in close proximity to a nerve stimulate the nerve fibers directly, via an electric current or a physical stimulus from manual acupuncture. While this approach is reductionist, it is practical and could be used easily by physician–acupuncturists who largely rely on Western physiologic paradigms for diagnosis. Structural acupuncture practitioners could also use this protocol, because their training emphasizes anatomical correlations. There are even greater benefits to having a protocol in research because this allows for standardized acupuncture doses and precise comparisons against sham acupuncture or against other acupuncture styles.
A Closer Look at Point Selection
The structural theory or acupuncture dates back to Dr. Cheng Dan'an, who is widely considered as the father of modern acupuncture. In his 1932 book Chinese Acupuncture and Moxibustion Therapeutics,18 he redefined acupuncture points and meridians, moving them away from blood vessels and closer to peripheral nerves. He postulated that acupuncture's mechanism of action is mediated via the peripheral nerves. Since the 1980s, acupuncture practitioners and anatomists have attempted to correlate the location of acupuncture points to peripheral nerves, spinal segments, and spinal plexuses.19–25 This neuroanatomical theory of acupuncture suggests that acupuncture's effect is mediated via afferent input through the peripheral nervous system, eliciting a reflex at the level of the spinal cord via the sympathetic plexuses and via efferent to the visceral organs and skeletal muscle.26,27
The neurophysiologic testing to support these theories is lacking so far and further study on the local, direct effects of acupuncture on the peripheral nervous system is needed. There is a consensus, however, that the nervous system is vital for processing the effects of acupuncture.
The present neuropathy treatment protocol is based on selecting acupuncture points that are closely associated with large peripheral nerves. Interestingly, in many cases these points are traditionally used for the treatment of paralysis, fatigue, peripheral neuropathy, and other neurologic conditions (Table 3).28 In this protocol, LR 4, LU 5, LI 11, and KI 27 were chosen for traditional reasons—left LR 4 and LU 5 are Oketsu points and LI 11 is an immune point according to Kiito Matsumoto–style acupuncture. KI 27 is traditionally used to close the Kidney channel (Figs. 1 and 2). The remainder of the points were chosen for their proximity to peripheral nerves. EA was applied to points in close association with large nerves in the ankle and foot—ST 41–LR 3, deep peroneal nerve; and KI 1–3, posterior tibial/medial plantar nerves (Figs. 3 and 4). KI 1 and BaFeng, in addition to being closely associated with nerves, are very commonly used in traditional-style neuropathy treatments.
Table 3.
Overview of Selected Acupuncture Points
| Acupuncture point | Traditional functions | Traditional indicationsa | Anatomical correlations (nerves) |
|---|---|---|---|
| LI 4 | Disperses Wind, relieves Exterior conditions, suppresses pain & clears the channels | Common cold, headache, diseases of the sensory organs, facial paralysis, hemiplegia, global weakness, chronic fatigue & pain in general | Radial |
| LU 5 | Oketsu/drains the Heat in the Lungs & suppresses rebellious Qi | Coughing, asthma, pneumonia, bronchitis, pleurisy, spitting blood, swelling & pain in the throat, swelling & pain in the elbow & arm | Lateral antebrachial cutaneous (musculocutaneous) |
| LI 11 | Eliminates Wind and Exterior conditions, cools Heat & alleviates Dampness & regulates the Blood | Arthritis pain in the upper limb, paralysis, hemiplegia, hypertension, high fever, measles, anemia, allergies, goiter & skin diseases | Radial |
| TE 5 | Relieves Exterior and Hot conditions & facilitates circulation of Stagnant Qi in the channels | Common cold, high fever, pneumonia, parotitis, deafness, tinnitus, migraine headache, enuresis, stiff neck, hemiplegia, paralysis & pain in the joints of the upper limb | Posterior interosseous (radial) |
| GB 34 | Tonifies Liver and Gallbladder, relaxes muscles, helps with smoothness of movement & removes Dampness & Heat | Muscle cramps, musculoskeletal pain, rigidity, weakness, hemiplegia, sciatica, acute hepatitis & acute cholecystitis | Common peroneal |
| ST 36 | Orders the Spleen and Stomach, regulates the Qi & Blood & strengthens weak & Deficient conditions | Acute and chronic gastritis, enteritis, acute pancreatitis, indigestion, hemiplegia, shock, anemia, hypertension, allergies, jaundice, seizures, asthma, enuresis, diseases of the reproductive system, chronic fatigue & global weakness | Deep peroneal |
| ST 41 | Clears away Stomach fire & resolves Phlegm | Headache, nephritis, enteritis, seizures, diseases of the ankle & surrounding soft tissues & drop foot | Deep peroneal |
| LR 3 | Pacifies the Liver, clears Heat, regulates the lower Jiao & opens the channels | Headache, vertigo, hypertension, insomnia, hepatitis, mastitis, irregular menstruation, thrombocytopenia & soreness of the joints of the extremities. | Deep peroneal |
| LR 4 | Oketsu/removes Heat from the Liver & Gallbladder, regulates the lower Jiao, spreads the Liver Qi & clears the channels | Hepatitis, retention of urine, nocturnal emissions, genital pain, hernia pain, lower abdominal pain & diseases of the ankle and the surrounding soft tissues | Deep peroneal |
| BaFeng (EX-LE 10) | Enhances collateral circulation and regulates Blood flow | Headache, toothache, stomach pain, irregular menses, inflammation of the dorsum of the foot & toes, foot numbness, neuropathic pain & foot & leg weakness | Superficial peroneal |
| SP 9 | Transforms Damp Stagnation & benefits the lower Jiao | Abdominal distention, ascites, urinary retention, incontinence, urinary-tract infection, irregular menses, impotence, enteritis & knee pain | Medial saphenous (femoral) |
| SP 6 | Strengthens the Spleen & transforms Dampness, spreads the Liver Qi & benefits the Kidneys | Incontinence, reproductive problems, abdominal pain and distention, diarrhea, hemiplegia, chronic fatigue & generalized weakness | Posterior tibial |
| KI 3 | Relieves Heat by controlling Yin, strengthens Kidney-Yang, regulates the Uterus & strengthens the waist & knee | Nephritis, cystitis, irregular menses, spermatorrhea, enuresis, toothache, chronic laryngitis, stomatitis, tinnitus, pulmonary emphysema, cough, asthma, chronic fatigue, global weakness, sciatica, paralysis of the lower limbs, painful heel, vomiting & constipation. | Posterior tibial |
| KI 1 | Strengthens all senses, stops adverse flow of Stomach Qi to stop vomiting, clears Heart-Fire, replenishes Yang & prevents collapse | Shock, heat exhaustion, insomnia, stroke, cerebral hemorrhage, hypertension, seizures, psychosis, mental illness, vertex headache, lower-limb paralysis, lower-limb spasms & low back pain | Medial plantar (posterior tibial) |
Bold indicates neurologic conditions.
Study Limitations
This was a limited case series aimed to introduce a standardized acupuncture protocol for peripheral neuropathy of various causes. As such, it has not withstood the test of a randomized controlled trial against sham acupuncture or other acupuncture regimens. While the mechanism of action is likely direct effect on the peripheral nerves, exerted by the acupuncture needles, it is unclear why this works equally well in the case of large- and small-fiber neuropathy. One likely explanation is that small-fiber neuropathic pain is also mediated through larger peripheral nerves, and eventually modulated through the central nervous system. This case series ignores central mechanisms of pain mediation and possible placebo and expectancy effects. It is well-established that positive expectancy increases acupuncture's therapeutic potential.29,30
As this protocol uses both manual acupuncture and EA, it is impossible to isolate and characterize their individual therapeutic effects. It is unclear if applying EA to different points would have similar therapeutic value. There is an emerging body of evidence to suggest that manual acupuncture and EA might not be interchangeable and that their effects and mechanisms of action might be different.31
While the present author tried to use a standardized intervention as much as possible, she also applied additional treatments when there was neuropathic pain elsewhere—which were deviations from the protocol. In those cases, points were selected using the same strategy of local, direct nerve effects. The 10 patients also received various amounts of acupuncture, and there were no post-treatment follow-ups.
Given that this work is based on clinical observations, the VAS was the only used outcome measure. In a randomized controlled trial, additional outcome measures should be used, such as quality-of-life measures, peripheral neuropathy scales, and nerve-conduction studies as an objective measure of nerve function. In spite of all these limitations, there was satisfactory improvement in each of these consecutive cases, which warrants further exploration into this proposed treatment protocol.
Conclusions
This review of 10 cases of neuropathy was designed to introduce a standardized acupuncture protocol, based on anatomical correlations between nerves and acupuncture points. Further studies with larger sample sizes and randomized comparisons against sham acupuncture and other acupuncture regimens will be helpful to determine if this protocol could be established as a guideline for approaching peripheral neuropathy.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Amato AA, Russell JA. Neuromuscular Disorders. New York: McGraw-Hill Medical; 2008 [Google Scholar]
- 2.Herskovitz S, Scelsa SN, Schaumburg HH. Peripheral Neuropathies in Clinical Practice. New York: Oxford University Press; 2010 [Google Scholar]
- 3.Gordon Smith A, Robinson Singleton J. Idiopathic neuropathy, prediabetes and the metabolic syndrome. J Neurol Sci. 2006;242(1–2):9–14 [DOI] [PubMed] [Google Scholar]
- 4.Martyn CN, Hughes RA. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1997;62(4):310–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu J, Cui Z. Clinical study of diabetic peripheral neuropathy treated by acupuncture. Int J Clin Acupunct. 2001;12(4):315–318 [Google Scholar]
- 6.Zhang C, Ma YX, Yan Y. Clinical effects of acupuncture for diabetic peripheral neuropathy. J Tradit Chin Med. 2010;30(1):13–14 [DOI] [PubMed] [Google Scholar]
- 7.Zheng HT, Li YF, Yuan SX. Observations on 52 patients with diabetic peripheral neuropathy treated by needling combined with drug. J Acu Tuina Sci. 2004;2(6):24–26 [Google Scholar]
- 8.Zuo L, Zhang L. Study on the effect of acupuncture plus methylcobalamin in treating diabetic peripheral neuropathy. J Acu Tuina Sci. 2010;8(4):249–252 [Google Scholar]
- 9.Dimitrova A, Murchison C, Oken B. Acupuncture for the treatment of peripheral neuropathy: A systematic review and meta-analysis. J Altern Complement Med. 2017;23(3):164–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shiflett SC, Schwartz GE. Effects of acupuncture in reducing attrition and mortality in HIV-infected men with peripheral neuropathy. Explore (N Y). 2011;7(3):148–154 [DOI] [PubMed] [Google Scholar]
- 11.Shlay JC, Chaloner K, Max MB, et al. Acupuncture and amitriptyline for pain due to HIV-related peripheral neuropathy: A randomized controlled trial. Terry Beirn Community Programs for Clinical Research on AIDS. JAMA. 1998;280(18):1590–1595 [DOI] [PubMed] [Google Scholar]
- 12.Anastasi JK, Capili B, McMahon DJ, Scully C. Acu/moxa for distal sensory peripheral neuropathy in HIV: A randomized control pilot study. J Assoc Nurses AIDS Care. 2013;24(3):268–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khosrawi S, Moghtaderi A, Haghighat S. Acupuncture in treatment of carpal tunnel syndrome: A randomized controlled trial study. J Res Med Sci. 2012;17(1):1–7 [PMC free article] [PubMed] [Google Scholar]
- 14.Kumnerddee W, Kaewtong A. Efficacy of acupuncture versus night splinting for carpal tunnel syndrome: A randomized clinical trial. J Med Assoc Thai. 2010;93(12):1463–1469 [PubMed] [Google Scholar]
- 15.Yao E, Gerritz PK, Henricson E, et al. Randomized controlled trial comparing acupuncture with placebo acupuncture for the treatment of carpal tunnel syndrome. PM R. 2012;4(5):367–373 [DOI] [PubMed] [Google Scholar]
- 16.Yang CP, Hsieh CL, Wang NH, et al. Acupuncture in patients with carpal tunnel syndrome: A randomized controlled trial. Clin J Pain. 2009;25(4):327–333 [DOI] [PubMed] [Google Scholar]
- 17.White A, Cummings M, Barlas P, et al. Defining an adequate dose of acupuncture using a neurophysiological approach—a narrative review of the literature. Acupunct Med. 2008;26(2):111–120 [DOI] [PubMed] [Google Scholar]
- 18.Dan'an C. Chinese Acupuncture and Moxibustion Therapeutics [in Chinese]. Shanghai: Quanqingtang Shuju; 1932 [Google Scholar]
- 19.Dung HC. Acupuncture points of the cranial nerves. Am J Chin Med. 1984;12(1–4):80–92 [DOI] [PubMed] [Google Scholar]
- 20.Dung HC. Acupuncture points of the cervical plexus. Am J Chin Med. 1984;12(1–4):94–105 [DOI] [PubMed] [Google Scholar]
- 21.Dung HC. Acupuncture points of the brachial plexus. Am J Chin Med. 1985;13(1–4):49–64 [DOI] [PubMed] [Google Scholar]
- 22.Dung HC. Acupuncture points of the lumbar plexus. Am J Chin Med. 1985;13(1–4):133–143 [DOI] [PubMed] [Google Scholar]
- 23.Dung HC. Acupuncture points of the sacral plexus. Am J Chin Med. 1985;13(1–4):145–156 [DOI] [PubMed] [Google Scholar]
- 24.Dung HC. Acupuncture points of the typical spinal nerves. Am J Chin Med. 1985;13(1–4):39–47 [DOI] [PubMed] [Google Scholar]
- 25.Bossy J. Morphological data concerning the acupuncture points and channel network. Acupunct Electrother Res. 1984;9(2):79–106 [DOI] [PubMed] [Google Scholar]
- 26.Cheng KJ. Neuroanatomical basis of acupuncture treatment for some common illnesses. Acupunct Med. 2009;27(2):61–64 [DOI] [PubMed] [Google Scholar]
- 27.Cheng KJ. Neuroanatomical characteristics of acupuncture points: Relationship between their anatomical locations and traditional clinical indications. Acupunct Med. 2011;29(4):289–294 [DOI] [PubMed] [Google Scholar]
- 28.Bensky D, O'Connor J, trans. & eds. Acupuncture: A Comprehensive Text. Shanghai College of Traditional Medicine. Seattle, WA: Eastland Press; 1996 [Google Scholar]
- 29.Prady SL, Burch J, Vanderbloemen L, et al. Measuring expectations of benefit from treatment in acupuncture trials: A systematic review. Complement Ther Med. 2015;23(2):185–199 [DOI] [PubMed] [Google Scholar]
- 30.Kong JT, Kaptchuk TJ, Polich G, et al. An fMRI study on the interaction and dissociation between expectation of pain relief and acupuncture treatment. Neuroimage. 2009;47(3):1066–1076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Langevin HM, Schnyer R, MacPherson H, et al. Manual and electrical needle stimulation in acupuncture research: Pitfalls and challenges of heterogeneity. J Altern Complement Med. 2015;21(3):113–128 [DOI] [PMC free article] [PubMed] [Google Scholar]