Abstract
This exploratory longitudinal study examined behavioral outcomes and parenting stress among families with children adopted from foster care, taking into account environmental and biological risk factors. Child internalizing and externalizing problems and parenting stress were assessed in 82 adopted children and their families at 2 months post-placement, 12 months post-placement, and then yearly until 5 years post-placement. A history of abuse/neglect predicted significantly higher externalizing and internalizing problems at a borderline level of statistical significance. In the initial stages after placement, externalizing problems were significantly higher among children who were 4 years or older at placement versus those who were younger than 4, although differences were no longer significant 5 years post-placement. Statistical trends in parenting stress reflected reduced stress in the first 12 months followed by a plateau for parents who adopted older children and greater stress for parents who adopted younger children. Familiar limitations for observational cohort data apply. Nonetheless, the availability of longitudinal follow-up on a sizable sample of children adopted from foster care adds insight to the psychological dynamics for adoptive families and suggests that families of children adopted from the foster care system may have unique needs for ongoing support around behavioral issues.
Keywords: externalizing, behavior(s), internalizing, strain, caregiver(s), at-risk populations, welfare, child
The number of children adopted from the foster care system has increased dramatically in recent years. In 2013, more than 50,000 children were adopted from the foster care system (U.S. Department of Health and Human Services: Administration for Children and Families, 2014). Yet, we know relatively little about the long-term emotional and behavioral trajectories of these children or about the parenting experiences of their adoptive parents. The present study examines the trajectories of emotional and behavioral problems and parenting stress over the first 5 years of adoptive placement among children adopted from foster care, while examining the role of children’s pre-placement risk factors and family demographic characteristics.
Although children who are adopted fare better in many domains than those who remain in foster care (e.g., Berlin, Vinnerljung, & Hjern, 2011; Brand & Brinich, 1999), adoptees are at higher risk for emotional and behavioral problems than their nonadopted peers. A meta-analysis examining more than 25,000 adoptees across different countries concluded that adoptees have more internalizing and externalizing symptoms than nonadopted children, with domestic adoptees experiencing more difficulties than international adoptees (Juffer & van Ijzendoorn, 2005). Adopted children are also overrepresented in clinical settings (Juffer & van Ijzendoorn, 2005; Miller et al., 2000; Warren, 1992; Wierzbicki, 1993).
Particular attention has been paid to externalizing problems (symptoms consistent with oppositional and conduct problems). Domestic and international adoptees (adopted before age 2) exhibit more symptoms of externalizing disorders in adolescence than their nonadopted peers (Keyes, Sharma, Elkins, Iacono, & McGue, 2008). A study of adopted youth in the United States 8 years after adoptive placement found that 30% of the sample exhibited symptoms consistent with oppositional defiant disorder, attention deficit/hyperactivity disorder, or both (Simmel, Brooks, Barth, & Hinshaw, 2001). In one of the few studies that has followed domestic adoptive families over time, both disruptive behavioral problems and internalizing symptoms were observed to be higher for children adopted from foster care than those not adopted from foster care, 8 years post-adoption (Simmel, Barth, & Brooks, 2007). Both groups of adoptees experienced symptom levels that were higher than would be expected compared with the general population (Simmel et al., 2007). The higher rates of emotional and behavioral difficulties can affect children’s long-term psychological and functional outcomes. In addition, the severity of emotional and behavioral issues among children has been associated with higher level of caregiver strain and parenting stress (Brannan & Heflinger, 2006; Brannan, Heflinger, & Bickman, 1997; Vaughan, Feinn, Bernard, Brereton, & Kaufman, 2013).
Although parents’ reports of the impact of adopted children on the family have typically been positive (Berry & Barth, 1989; Glidden, 1991; Groze, 1996; Nelson, 1985), stress associated with adopting children from foster care may affect family outcomes. In a study of 41 adoptive families, Glidden and Pursley (1989) found that 88% of respondents reported some type of negative impact, including negative personality changes among children already in the family, more arguments between spouses, negative reactions from extended family members, financial difficulties, and trouble coping with their children’s problem behaviors. Another study of families adopting older children (ages 3–15 at the time of adoption) from foster care found that 25% of parents reported that the experience was worse than they had expected (Berry & Barth, 1989).
Relatively few studies have taken a longitudinal perspective on parenting stress after adoption (e.g., Barth & Brooks, 1997; Berry & Barth, 1989; Glidden, 1991; Groze, 1996; Nelson, 1985). In a 3-year longitudinal study, mothers not only reported higher levels of personal reward 3 years after adoption than at baseline but also reported higher levels of family disharmony (Glidden & Pursley, 1989). Another study of families adopting from foster care reported that the impact of the adoption became more negative over a 1-year time span for 21% of families (Groze, 1996). Parenting stress and satisfaction with adoption have been found to relate chiefly to children’s emotional and behavioral difficulties (McGlone, Santos, Kazama, Fong, & Mueller, 2002; Nalavany, Glidden, & Ryan, 2009). We examine the trajectories of internalizing behaviors, externalizing behaviors, and parenting stress over time.
Pre-Placement Risk Factors
Inter-related risk factors for psychological and behavioral problems are common to this population. Older children adopted from public agencies often experience risk factors that cluster together, such as prenatal substance exposure, premature birth, low birth weight, a history of abuse and/or neglect, and multiple placements (Rushton & Dance, 2006). These factors are likely to place children at higher risk for subsequent emotional problems (Bimmel, Juffer, van Ijzendoorn, & Bakermans-Kranenburg, 2003; Grotevant, Manfred, van Dulmen, & Dunbar, 2006).
For adopted youth, older age at placement in an adoptive home is a strong predictor of higher risk for psychological and school problems (Berry & Barth, 1989; Keyes et al., 2008; Sharma, McGue, & Benson, 1996b). More specifically, Sharma, McGue, and Benson (1996b) found that compared with controls and infant adoptees, adolescents who were adopted over the age of two often exhibited emotional and behavioral difficulties, with those placed in adoptive homes over the age of 4 being the most troubled. Children who are adopted when they are older are more likely to have experienced prior abuse and/or neglect, strong predictors of behavioral and emotional problems (Dance, Rushton, & Quinton, 2002; Garland et al., 2001; McMillen et al., 2005; Simmel, 2007). Older children are also more likely to have experienced multiple placements, which are associated with poor adjustment into the adoptive placement (Berry & Barth, 1989), increased internalizing and externalizing problems (Newton, Litrownik, & Landsverk, 2000; Rosenthal & Groze, 1994), and greater mental health service utilization (Rubin et al., 2004).
Few longitudinal studies of youth adopted from public care have specifically examined pre-placement risk factors as they relate to behavior problems. Studies in the United Kingdom have found that older age at placement, a history of emotional abuse, and high levels of behavior problems predicted poor placement progress and disruptions at a 6-year follow-up (Dance et al., 2002, Rushton & Dance, 2006). In one of the few U.S.-based studies, Simmel (2007) reported that prenatal substance exposure, abuse and/or neglect, older age at adoption, multiple placements, and lower parental readiness for adoption predicted continued externalizing symptoms over time. The current study provides an update to the literature with this study sample recruited 10 years after the previous longitudinal studies (e.g., Crea, Barth, Guo, & Brooks, 2008; Simmel, 2007; Simmel et al., 2007). This study sample reflects populations adopted from foster care after the legislation designed to encourage greater rates of adoption from foster care had been enacted (thereby increasing adoption rates of older children; Hansen, 2007).
Conflicting findings regarding the long-term impact of prenatal substance exposure on children’s developmental outcomes exist in the literature (Barth & Miller, 2000; LaGasse, Seifer, & Lester, 1999; Messinger et al., 2004), but prenatal exposure to cocaine and other substances may affect long-term behavioral outcomes (Bada et al., 2007; Crea et al., 2008). Moreover, exposure to substances such as nicotine is associated with low birth weight and prematurity (Kramer, 1987; Olsen et al., 1995). Studies of school-aged children born extremely prematurely have found associations with a number of negative outcomes, including internalizing and externalizing problems (Reijneveld et al., 2006).
Post-Placement Risk Factors
The adoptive placement itself, such as adoptive parents’ educational attainment, may affect outcomes for adoptive children. Although family socioeconomic status is positively related to child outcomes in nonadoptive families, both national and international studies have found that higher socioeconomic status is negatively related to children’s psychological outcomes in adoptive families (Berry & Barth, 1989; Erich & Leung, 1998; Rosenthal & Groze, 1990; Rosenthal, Schmidt, & Conner, 1988; Tieman, van der Ende, & Verhulst, 2005; Verhulst, Althaus, & Versluis-den Bieman, 1990a, 1990b). To date, we have little understanding of the ways in which being adopted into a home of higher socioeconomic status and higher educational achievement than that of the birth family may affect children’s behavioral trajectories and the adoptive parents’ parenting stress over time.
Transracial adoption has long been a subject of debate among professionals, legislators, and researchers but is largely unexplored in longitudinal analyses. Legislation prohibiting race as a factor in adoptive placement exists (e.g., The Multiethnic Placement Act [MEPA] of 1994), as well as legislation governing the adoption of children of Native American descent (Indian Child Welfare Act of 1978), in which the tribe must be notified of any impending adoption, and efforts should be made to place the child with the tribe or another Native American tribe. A review of the available literature examining the psychosocial adjustment and well-being of transracially adopted children has not found any significant negative repercussions of placement with adoptive parents of a different race (Feigelman, 2000; Frasch & Brooks, 2003). Pre-placement problems and delays in permanent placement accounted for a greater proportion of adoptees’ difficulties related to self-esteem and development of racial/ethnic identity than did issues related to their transracial placement (Silverman, 1993). In this study, we examine whether transracial adoption affects child and parent outcomes.
Study Questions
The current study sought to examine the trajectory of parents’ and children’s long-term adjustment in the years following children’s placement in their adoptive homes. Specifically, we examined behavioral syndromes and the trajectories of broadband internalizing and externalizing behavior problems in a sample of children adopted from foster care during the first 5 years of their adoptive placement, as well as trajectories of parents’ stress. We focused on how these trajectories varied with key environmental and biological risk factors (e.g., history of abuse/neglect, multiple placements, older age at adoption) and family factors (e.g., parental educational attainment, transracial adoption).
Method
Participants
Participants were recruited from the University of California, Los Angeles (UCLA) TIES (Training, Intervention, Education, and Services) for Families program (formerly called TIES for Adoption), which aims to facilitate successful adoption of high-risk children transitioning from foster care to adoptive placement. The families taking part in this program between 1996 and 2001 were asked to participate in this longitudinal study (N = 82 children; n = 69 families).
The Department of Adoptions of the Los Angeles County Department of Child and Family Services (DCFS) requires potential adoptive parents to attend a series of educational seminars prior to being assigned a child. The TIES program offered three additional educational meetings aimed at understanding parenting strategies for dealing with children with the aforementioned risk factors. For those attending the three meetings, additional comprehensive services were offered to eligible families, including multidisciplinary pre-placement consultation, parent and child counseling services, support groups, and medical, educational, and psychiatric consultation. The research study was mentioned at the third session of the additional educational meetings, and families who subsequently had children placed with them and requested services from TIES for Families were asked if they would like to participate in the follow-up study. Participants were subsequently tracked for a period of at least 5 years.
Characteristics of the sample are presented in Table 1. The primary adoptive parents were predominantly female, with an average age of 41. The majority (68.8%) of the adoptive parents were White and nearly two thirds had attended college. About 40% of the children were placed in transracial adoptions (minority children with White parents). Children were, on average, 4.3 years old at placement, with a range from shortly after birth to 8 years old. There were roughly even numbers of girls and boys, and the majority (82.9%) of children in the sample were ethnic minorities.
Table 1.
Child and Primary Adoptive Parent Descriptive Statistics.
| Child | Primary adoptive parent | |
|---|---|---|
|
|
|
|
| n = 82 | n = 69 | |
|
|
|
|
| n or M (SD) | n or M (SD) | |
| Age at placement (years) (n = 63 for parent) | 3.9 (2.2) Range: 0–8.1 |
41.1 (5.6) Range: 30–56 |
| Gender (n = 80 children; 68 parents) | ||
| Female | 38 (46.3%) | 52 (76.5%) |
| Ethnicity (n = 80 children; 68 parent) | ||
| White | 14 (17.1%) | 44 (64.7%) |
| Latino | 33 (40.2%) | 6 (8.8%) |
| African American | 21 (25.6%) | 13 (19.1%) |
| Biracial or Other | 14 (17.1%) | 5 (7.4%) |
| Number of previous placements (n = 79) | 3.2 (2.4) Range: 0–15 |
|
| Parent’s education (n = 68) | ||
| Less than college | 24 (35.3%) | |
| College | 21 (30.9%) | |
| More than college | 23 (33.8%) | |
| Parent’s marital status (n = 68) | ||
| Single | 21 (30.9%) | |
| Married | 35 (51.5%) | |
| Domestic partner | 9 (13.2%) | |
| Divorced | 3 (4.4%) | |
| Risk factors | ||
| Environmental | ||
| History of abuse/neglect (n = 80) | 35 (43.8%) | |
| Age older than 4 | 40 (48.8%) | |
| Lived with biological mother (n = 80) | 41 (51.3%) | |
| >3 placements (n = 79) | 30 (38.0%) | |
| Biological | ||
| Prenatal exposure (n = 65) | 59 (90.2%) | |
| Premature (n = 64) | 24 (37.5%) | |
| Low birth weight (n = 63) | 24 (38.1%) | |
| Transracial adoption | 42 (51.5%) | |
| Parenting stress score | 104.3 (24.6) | |
Note. For variables with missing values, sample sizes are given in the first column.
Procedures
The DCFS granted permission to review the child’s records. Approximately 2 months after placement (Baseline), parents filled out questionnaires and came with their child(ren) to UCLA for in-person interviews and testing. They returned approximately 1 year after adoptive placement (Year 1) and each year thereafter, for a total of 5 years (Years 2–5). When the child lived with two adoptive parents, the one spending the most time with the child was designated as the primary parent. Both parents completed questionnaires in English at home in advance of the in-person interview; data for the primary caregiver (as identified by the parents) were used in the study. All “risk factor” variables were assessed at baseline. “Behavior” and “parenting stress” variables were assessed at baseline and at each subsequent time point. All research procedures were reviewed and approved by the Institutional Review Board of UCLA.
Measures
Demographic characteristics
Age, gender, and ethnicity were recorded for children. For the primary adoptive parent, demographic characteristics included age, gender, ethnicity, marital status, and education level.
Risk factors
We examined a number of biological and environmental risk factors. Information about risk factors was gathered from birth records, court reports, and DCFS records. All variables were coded dichotomously.
Biological risk
Biological risk factors of prenatal substance exposure, prematurity, and birth complications were each recorded for their presence or absence whenever the information was available. Missing data on some biological risk factors were most often due to lack of availability of birth records. Prematurity was defined as 35 weeks or less gestation. Birth complications included drug withdrawal symptoms at birth, as well as other complications of prematurity (i.e., respiratory distress, need for resuscitation at birth, and low birth weight). Low birth weight referred to weight less than 2,500 g (about 5 lbs).
Environmental risk
Environmental risk factors included history of abuse or neglect, age older than 4 at placement, whether the child ever lived with the birth mother, and more than three prior foster placements. Placement at age 4 or older was used to signal adoption at relatively older age. The State of California used this age cutoff to denote “special needs” adoptions. In addition, the decision to use more than three placements as a risk marker was based on the distribution of prior placements in the sample.
Associated factors
Additional factors included transracial adoption status and the education level of the adoptive parents. The adoption was considered transracial if the child’s ethnicity matched neither parent. Generally, in these cases, a child of color was placed with White adoptive parents. Higher parental education was examined with an indicator for whether or not the primary adoptive parent had any college education. Education was used in lieu of income because income data were determined to be more unreliable and were at times lowered due to parents who reduced or stopped working due to the adoption.
Child behavior problems
Behavioral outcomes were obtained using the Child Behavior Checklist (CBCL) for ages 1.5 to 5 (Achenbach & Rescorla, 2001) and the CBCL for ages 4 to 18 (Achenbach, 1991). These versions of the widely used CBCL are designed to assess areas of competency and difficulty for preschool- and school-aged children and have been routinely used in both treatment outcome studies and longitudinal studies of child behavioral problems (e.g., Lochman et al., 2010; Milan, Pinderhughes, & The Conduct Problems Prevention Research Group, 2006). The pre-school scale includes 99 items, and the school-age version has 118 items that describe common childhood problems; the scales have strong psychometric properties in diverse populations (Achenbach & Rescorla, 2001). The current study examined the internalizing and externalizing broadband scales and the corresponding empirically derived syndrome subscales. For school-age children, these include Aggression, Delinquent Behavior, Anxiety, Depression, and Somatic Problems. For younger children, these include Aggression, Attention Problems, Anxiety, Depression, Somatic Problems, and Emotional Reactivity. Participants were asked to rate the degree to which each item applies to their child now or within the past 2 months, with each item scored as 0 = not true, 1 = somewhat or sometimes true, and 2 = very often or often true. CBCL scoring yields a total problem score, composite externalizing and internalizing scores, and seven subscale scores.
Parenting stress
Parenting stress was measured at each time point using the parenting stress index (PSI; Abidin, 1983). This 126-item questionnaire measures stress involving a parent–child dyad. Parents are asked to rate each item on a 5-point Likert-type scale from strongly agree to strongly disagree (range from 1 to 5). The PSI generates raw scores as well as norm-referenced summaries on two major source domains of stressors (the child domain and the parent domain). We analyzed outcomes from the child domain, which is comprised of 47 questions that map into six subscales: Adaptability, Acceptability, Demandingness, Mood, Distractibility/Hyperactivity, and Reinforcement. Scores above 116 for the child domain are considered “high.” The test–retest reliability of the PSI has been established in multiple studies with estimates ranging from r = .55 to .82 (Abidin & Lloyd, 1985; Burke, 1978), and the inter-item reliability for the PSI has been estimated at .89 (Abidin & Lloyd, 1985).
Results
Sample Characteristics
The children had a variety of characteristics pointing to elevated risk for adverse outcomes. With respect to biological risk factors, 38% of the sample was born prematurely, and 38% percent had low birth weight. Approximately 44% of the sample had experienced documented abuse or neglect, either in their birth homes or in foster care, and 48.8% were placed in their adoptive home at or after age 4. The prior number of placements ranged from one to 15, with 41.8% having more than three prior placements. About half of the sample had been discharged to their birth mother and, therefore, had lived (at least briefly) in an environment with a variety of risk factors, including drug abuse. Almost 90% of the sample had documented prenatal substance exposure; given the ubiquity of this risk factor, we did not include prenatal substance exposure in our primary analysis of outcomes over time.
Behavioral Syndromes and Parental Stress Over Time
Table 2 shows the percentages of children with CBCL scores in the clinical, borderline, and non-clinical range at each time point for the broadband internalizing and externalizing indices as well as the corresponding empirically derived syndrome scales as described in the “Method” section (i.e., Aggression, Delinquent Behavior, Attention Problems, Withdrawn, Depressed, Somatic, and Emotional Reactivity). Although the percentages of children in the borderline and clinical ranges for externalizing and internalizing problems and across the empirically derived syndrome scales fluctuated over time, at least 20%, and often 30% or more, of the children were in either the clinical or borderline range for externalizing problems at any time point. Smaller, but still substantial percentages of children were in the clinical or borderline range for internalizing problems. With respect to the specific behavioral syndromes, children showed higher average scores on each of the component subscales for externalizing behavior (e.g., Aggression, Delinquent Behavior) than on each of the scales making up the internalizing component (e.g., Withdrawn, Depressed, Somatic). The range of children in either the borderline or clinical range for externalizing syndromes ranged from approximately 20% to 31% for aggressive behavior, 21% to 37% for delinquent behavior, and 21% and 42% for attentional problems. For internalizing syndromes, the proportion ranged from approximately 3% to 15% for withdrawn/depression, 7% to 15% for anxious/depressed, and 0% to 8% for somatic problems.
Table 2.
Percentage in Borderline and Clinical Range on CBCL and PSI.
| Time 1 (n = 64) % | Time 2 (n = 54) % | Time 3 (n = 52) % | Time 4 (n = 40) % | Time 5 (n = 36) % | Time 6 (n = 39) % | |
|---|---|---|---|---|---|---|
| CBCL broadband scales | ||||||
| Externalizing | ||||||
| Non-clinical | 68.8 | 70.4 | 69.2 | 77.5 | 69.4 | 71.8 |
| Borderline | 9.4 | 11.1 | 25.0 | 7.5 | 5.6 | 10.3 |
| Clinical | 21.9 | 18.5 | 5.8 | 15.0 | 25.0 | 17.9 |
| Internalizing | ||||||
| Non-clinical | 82.8 | 86.5 | 88.5 | 90.0 | 91.7 | 84.6 |
| Borderline | 10.9 | 1.9 | 3.8 | 7.5 | 2.8 | 5.1 |
| Clinical | 6.2 | 11.5 | 7.7 | 2.5 | 5.6 | 10.3 |
| CBCL empirically derived syndrome scales | ||||||
| Aggressive behavior | ||||||
| Non-clinical | 68.7 | 71.7 | 71.1 | 80.0 | 72.2 | 74.4 |
| Borderline | 14.1 | 5.7 | 17.3 | 10.0 | 5.6 | 12.8 |
| Clinical | 17.2 | 22.6 | 11.5 | 10.0 | 22.2 | 12.8 |
| Delinquent behaviora | (n = 37) | (n = 42) | (n = 35) | (n = 39) | ||
| Non-clinical | 73.0 | 64.3 | 74.3 | 79.5 | 72.2 | 74.4 |
| Borderline | 10.8 | 16.7 | 11.4 | 2.6 | 11.1 | 10.3 |
| Clinical | 16.2 | 19.0 | 14.3 | 17.9 | 16.7 | 15.3 |
| Attention problems | ||||||
| Non-clinical | 73.4 | 79.2 | 76.9 | 70.0 | 58.3 | 71.8 |
| Borderline | 12.5 | 13.2 | 15.4 | 12.5 | 19.4 | 15.4 |
| Clinical | 14.1 | 7.6 | 7.7 | 17.5 | 22.3 | 12.8 |
| Withdrawn/depressed | ||||||
| Non-clinical | 84.4 | 88.7 | 94.2 | 95.0 | 97.2 | 84.6 |
| Borderline | 4.7 | 1.9 | 3.8 | 2.5 | 2.8 | 7.7 |
| Clinical | 10.9 | 9.4 | 1.9 | 2.5 | 0 | 7.7 |
| Anxious/depressed | ||||||
| Non-clinical | 87.5 | 84.9 | 92.3 | 90.0 | 86.1 | 87.2 |
| Borderline | 10.9 | 7.5 | 1.9 | 7.5 | 8.3 | 10.3 |
| Clinical | 1.6 | 7.6 | 5.8 | 2.5 | 5.5 | 2.5 |
| Somatic problems | ||||||
| Non-clinical | 96.9 | 92.4 | 94.2 | 100.0 | 94.4 | 89.7 |
| Borderline | 3.1 | 3.8 | 3.8 | 0 | 2.8 | 2.6 |
| Clinical | 0 | 3.8 | 2 | 0 | 2.8 | 7.7 |
| Emotional reactivityb | (n = 27) | (n = 11) | (n = 17) | (n = 1) | ||
| Non-clinical | 77.8 | 90.9 | 88.2 | 0 | — | — |
| Borderline | 14.8 | 9.1 | 0 | 100.0 | — | — |
| Clinical | 7.4 | 0 | 11.7 | 0 | — | — |
| PSI | ||||||
| Non-elevated | 59.4 | 71.2 | 76 | 81.1 | 76.5 | 67.5 |
| Elevated | 40.6 | 29.8 | 24 | 18.9 | 23.5 | 32.5 |
Note. Clinical = score of 70 and above, Borderline = score between 65 and 69, Non-clinical = 64 and below. CBCL = Child Behavior Checklist; PSI = parenting stress index.
Subscale only available for families completing the school-age version of the CBCL.
Subscale only available for families completing the preschool version of the CBCL.
At baseline, the average parenting stress score was 104.3, below the cutoff score (116) traditionally used to indicate clinically concerning levels of stress (Abidin, 1983). Roughly 40% of the parents, however, had a score that exceeded 116 at baseline. Substantial percentages of parents were found to be in this elevated range of parenting stress at each wave. Fifty-two percent of parents were found to remain consistently below the clinical range, 18% remained consistently above the clinical cutoff, and 30% moved in and out of the clinical range across time. See the online supplementary table for means and standard deviations for each key outcome measure.
Inter-Relationships of Risk Factors
We examined associations among candidate predictor variables using chi-square analyses and found a number of associations in the expected directions for the environmental and biological risk factors. Being older than age 4 at the time of adoption was associated with having a history of abuse or neglect, having more than three previous placements, and having lived with the biological mother (each p < .05). Similarly, low birth weight and prematurity were strongly associated with one another (p < .01). There were negative associations between the environmental and biological risk factors such that the presence of environmental risk factors (older age at adoption, three or more previous placements, history of abuse) was associated with less likelihood of prematurity and low birth weight (each p < .05). Parent education level and transracial adoption status were not strongly related to other risk factors.
Risk Factors, Behavioral Problems, and Parenting Stress Over Time
Data analysis strategy
To evaluate the relationship between the covariates of interest and the three outcome measures (i.e., CBCL internalizing score, CBCL externalizing score, parenting stress), we fit a linear mixed model (separately) for each outcome. All three models included a change point, that is, a change in the trajectory of the outcome, at 12 months post-placement (discussed in more detail below). Each mixed model included a random subject-specific intercept and time slope.
Nearly every baseline covariate in this model had at least some missing data, with the number of missing values ranging from two (2.4%) to 18 (22%). Table 3 shows participant attrition over time. Of note, the number of participants increased from Time 4 to Time 5 due to increased success in tracking and engaging participants in the study. To address missing data, we performed multiple imputation for missing values (Rubin, 1987) using the predictive mean-matching method developed by Little (1988), implemented with five cells for predictive means. This process was repeated 30 times, giving us 30 versions of imputed data. Multiple imputations were performed using the R package mice under the default settings, with the exception of the number of imputations (default is five; van Buuren & Groothuis-Oudshoorn, 2011). In addition, we conducted additional analysis to explore the sensitivity of our results to missing data. Missing-data sensitivity analysis is discussed after the primary study findings.
Table 3.
Study Attrition Over Time.
| Time 1 | Time 2 | Time 3 | Time 4 | Time 5 | Time 6 | Total | |
|---|---|---|---|---|---|---|---|
| Parenting stress by time | |||||||
| Observed | 69 | 57 | 50 | 37 | 34 | 40 | 287 |
| Missing | 13 | 25 | 32 | 45 | 48 | 42 | 205 |
| Total | 82 | 82 | 82 | 82 | 82 | 82 | 492 |
| CBCL internalizing and externalizing scales by time | |||||||
| Observed | 64 | 54 | 52 | 40 | 36 | 39 | 287 |
| Missing | 18 | 28 | 30 | 42 | 46 | 43 | 205 |
| Total | 82 | 82 | 82 | 82 | 82 | 82 | 492 |
Note. CBCL = Child Behavior Checklist.
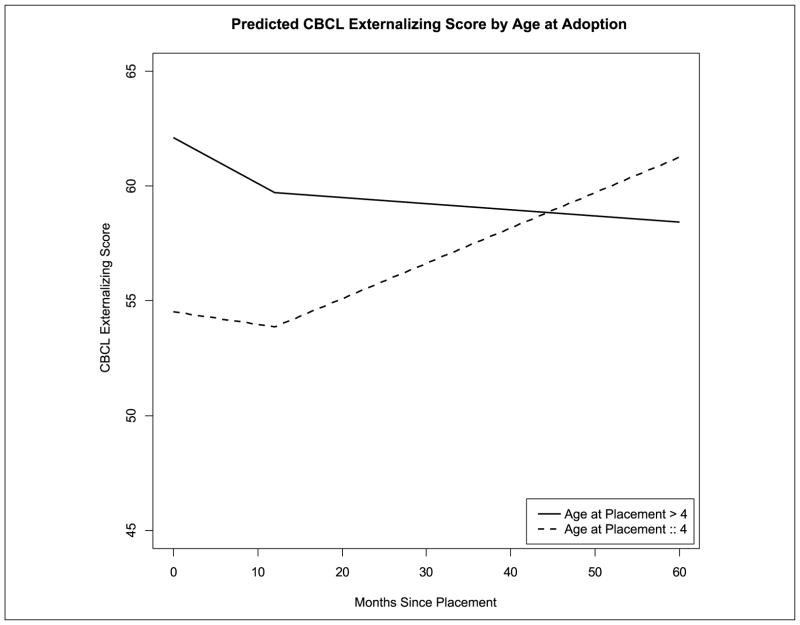
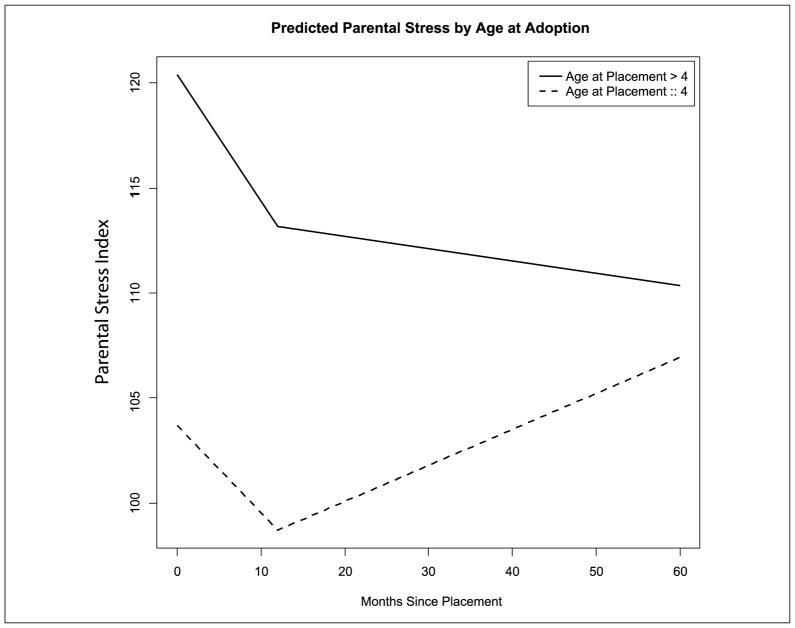
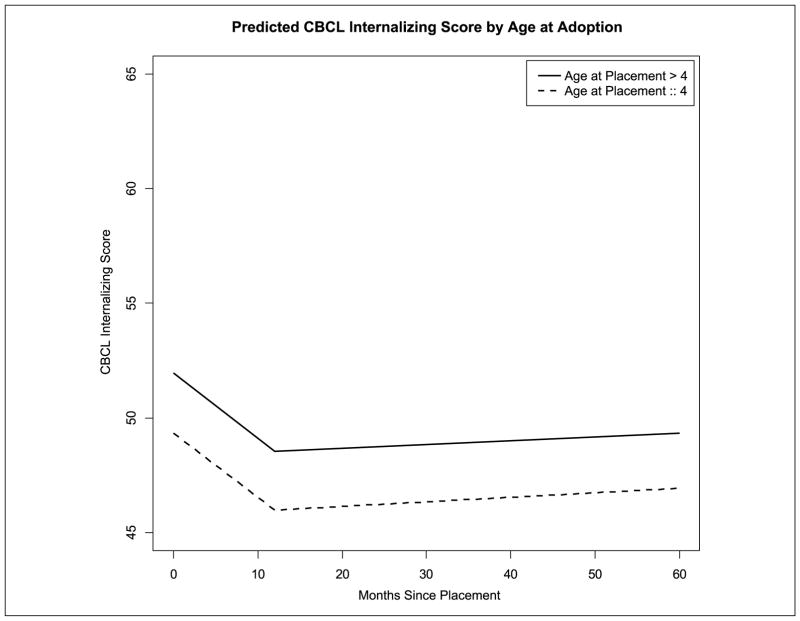
For each of the three outcomes, we fit a model that included time (in months) and indicators of a history of abuse, transracial adoption, age older than 4 years at placement, and primary parent’s education (less than college, college, more than college). Other baseline risk factors were also considered but were ultimately not included after they were found not to have substantial conditional associations with any of the three outcomes. Moreover, with only 82 subjects, parsimony was a consideration in model selection. The model also allowed the slope describing the change in outcomes over time to change at 1 year post-placement and included an interaction between time and age older than 4 years at placement, thus, differentiating between average trajectories for children placed by age 4 and children placed at an older age. Given that actual visit times were measured for each participant, we chose to treat time as a continuous variable. By including continuous time and a time slope change at 12 months post-placement, we posited that the outcome trajectories over time are piecewise linear with a “bend” at 12 months post-placement. See Figures 1 to 3 for an illustration of these trajectories. Statistical analyses were performed using R version 3.0.1. To account for the role of other variables, covariate values are fixed at reference levels.
Figure 1.
Predicted CBCL externalizing score by age at adoption.
Note. CBCL = Child Behavior Checklist.
Figure 3.
Predicted parental stress by age at adoption.
Regression results
Table 4 summarizes the results of the three linear mixed models. For externalizing behaviors, the trajectory over time depended on age at placement: For children less than 4 years old at placement, externalizing behavior scores tended to be higher over time, whereas for children more than 4 years old at placement, externalizing score appeared to decline over the first 12 months post-placement and then level off. Regardless of the child’s age at placement, internalizing behaviors showed a similar pattern of appearing to decline over the first 12 months post-placement and then leveling off. For parenting stress, the trends were less pronounced, reaching borderline levels of statistical significance. To the extent that the findings reflect an actual signal, the trajectories also seemed to depend on both time and age at placement, with parents of children who were more than 4 years old at placement having noticeably higher average scores at baseline and leveling off or slight declines as of 12 months post-placement. Parents of children who were less than 4 years old at placement showed declining scores over the first 12 months followed by greater levels over time. As an illustration, these trajectories are visually depicted in Figures 1 to 3.
Table 4.
Longitudinal Mixed-Effect Model Results for Behavioral Problems and Parenting Stress.
| Estimate | SE | p | |
|---|---|---|---|
| Externalizing behavior | |||
| Intercept | 54.520 | 2.689 | <.001 |
| Months (first 12) | −0.055 | 0.116 | .635 |
| Months (after 12) | 0.123 | 0.039 | .002 |
| Transracial adoption (yes = 1) | −4.270 | 2.263 | .061 |
| Age > 4 at placement (yes = 1) | 7.591 | 2.634 | .004 |
| Months × Age > 4 interaction | −0.144 | 0.052 | .006 |
| History of abuse (yes = 1) | 5.938 | 2.497 | .018 |
| Primary parent college | −2.645 | 2.842 | .353 |
| Primary parent > college | −1.080 | 2.590 | .677 |
| Internalizing problems | |||
| Intercept | 49.344 | 2.740 | <.001 |
| Months (first 12) | −0.281 | 0.137 | .041 |
| Months (after 12) | 0.016 | 0.046 | .725 |
| Transracial adoption (yes = 1) | −0.235 | 2.125 | .912 |
| Age > 4 at placement (yes = 1) | 2.606 | 2.716 | .339 |
| Months × Age > 4 interaction | −0.003 | 0.062 | .960 |
| History of abuse (yes = 1) | 4.357 | 2.356 | .066 |
| Primary parent college | 1.219 | 2.675 | .649 |
| Primary parent > college | 3.073 | 2.433 | .208 |
| Parenting stress | |||
| Intercept | 103.712 | 5.912 | <.001 |
| Months (first 12) | −0.417 | 0.243 | .088 |
| Months (after 12) | 0.137 | 0.079 | .083 |
| Transracial adoption (yes = 1) | −7.825 | 4.841 | .108 |
| Age > 4 at placement (yes = 1) | 16.693 | 6.144 | .007 |
| Months × Age > 4 interaction | −0.185 | 0.106 | .084 |
| History of abuse (yes = 1) | 7.460 | 5.369 | .166 |
| Primary parent college | −3.565 | 6.027 | .555 |
| Primary parent > college | −3.412 | 5.569 | .541 |
Note. Sample sizes for each outcome at each time point can be found in Table 3.
Average CBCL externalizing and internalizing scores for children with a history of abuse/neglect were estimated to be roughly 5.9 and 4.4 points higher, respectively, than those for individuals without such a history, holding all other variables constant. This difference was found to be significant for externalizing behavior and borderline significant for internalizing behavior (p = .018 and p = .066, respectively). A history of abuse/neglect was also positively associated with an increase in the average parenting stress score, but this association was not found to be significant (p = .166). Primary parent’s education level and transracial adoption status were not found to be significantly associated with parenting stress, externalizing behaviors, or internalizing behaviors, though transracial adoption status was found to have a borderline significant, negative association with externalizing behaviors (p = .061).
The maximum-likelihood estimates of the standard deviations of repeated measures were 5.58 for CBCL externalizing, 6.61 for CBCL internalizing, and 12.18 for parental stress. Drawing on the maximum-likelihood estimates of the variances and covariances for the random intercept and slope parameters, the ratios of between-individual to within-individual variance at baseline were estimated to be 2.75 for CBCL externalizing, 1.97 for CBCL internalizing, and 3.42 for parental stress, and the corresponding ratios at 60 months were estimated to be 3.48 for CBCL externalizing, 1.97 for CBCL internalizing, and 2.28 for parental stress. Such variance ratios are consistent with substantial intra-class correlation among repeated measures. It is also worth noting that all three regression models were re-significance results that were qualitatively similar to those presented above.
Analysis for sensitivity to missing data
Although we did not find any significant differences in baseline characteristics between dropouts (those with missing Time 6 values) and completers, we did explore the sensitivity of our results to nonignorable longitudinal dropout. As a general strategy, we drew on perspectives from the recent National Research Council report on handling missing data in clinical trials (Little et al., 2012; National Research Council, 2010). Specifically, we conducted “tipping point analyses,” using imputations under an ignorable missing-data model and perturbed some or all of the values in ways consistent with a particular nonignorable missing-data assumption. For example, one could assume that imputations for individuals at one level of a binary baseline classification (e.g., age greater than 4 at adoption) are consistent with patterns seen in cases with fully observed outcomes but that there is systematic bias in imputations for individuals at the other level of the binary baseline classification (i.e., age at most 4 at adoption) with imputed values being too high or too low by a given percentage, which we might label q. Considering different possible values of q, it is then possible to summarize findings by describing the “tipping point” of how large q would have to be to overturn an otherwise statistically significant finding. By exploring a range of possible departures from the assumptions used to produce our reported findings, we characterize the robustness (or lack thereof) of statistically significant findings to conceivable differences between individuals with available measurements and individuals who drop out of the study.
Exploring the sensitivity of the significant interaction effect (signaling dependence of CBCL externalizing score trajectories on age at placement) to the possibility of a non-ignorable dropout mechanism, we found that the time slope under a missing-at-random model for individuals who dropped out of the study and were at most 4 years of age at placement had to be decreased by .195 to overturn the significant effect of the interaction between time and the indicator of age being greater than 4 at placement. This represents a 355% decrease in the time slope for the first 12 months and a 159% decrease in the slope thereafter for these individuals, suggesting a fair degree of robustness for there being a genuine interaction effect with trajectories in CBCL externalizing scores depending on age at placement.
We also performed a tipping-point analysis to see whether nonignorable dropout could explain away the significant effect of a history of abuse on the externalizing score seen when fitting a missing at random (MAR) model to the observed data, finding that the magnitude of the coefficient reflecting the nonignorable effect needed to be slightly more than 9 times larger than the fixed effect of abuse observed in our original model (i.e., 5.94), which we interpret as meaning that the fixed effect of abuse is highly robust to the prospect of nonignorable dropout.
Discussion
Behavioral outcomes among children adopted from foster care are crucially important but have not been well studied. The current study sample gives us unique insight into trajectories of behavioral outcomes in a group of children whose profiles reflect considerably more adversity than have been seen in other studies of post-adoption behavioral adjustment. Overall, our findings suggest a tendency for internalizing and externalizing problems to decline after the transition to an adoptive home. However, outcomes fluctuate over time, and many children adopted from foster care continue to have problems in the clinical or borderline-clinical range, particularly externalizing behaviors.
Our findings regarding externalizing behaviors are consistent with the domestic and international literature showing that adopted children have high levels of problem behaviors (Juffer & van Ijzendoorn, 2005; Keyes et al., 2008; Simmel, 2007) and that increased externalizing problems are associated with early environmental risk factors (e.g., Bimmel et al., 2003; Simmel, 2007). Specifically, we found that externalizing problems were higher among children who were older than 4 years of age at the time of placement.
We also found an Age at Placement × Time interaction, suggesting that externalizing behavior trajectories may vary with a child’s age at placement. Specifically, the observed patterns suggest that though children who are older than 4 at the time of placement start out with higher levels of externalizing problems, they show improvement at a similar rate to children adopted at a younger age for the first year in an adoptive home and subsequently level off over time. In contrast, children younger than 4 at the time of placement appear to have an increase in behavior problems after the first year post-placement and reach a level similar to the older group by 5 years post-placement.
One possible reason for this finding may be that after a certain amount of time in an adoptive home, children adopted at a younger age feel comfortable enough to test limits. Our own exploratory analyses suggest that the trend in behavior problems was not related to child age at the time of the study (i.e., during the transition to adolescence) or the age at which they were placed. Nonetheless, this pattern of findings, along with the overall elevation in the number of children showing clinical and borderline-clinical levels of behavior problems, highlight the importance of supportive services for families who are adopting children from the foster care system. Although the majority of children were in the average range, consistently 20% or more of children had significant problems related to attention, aggression, and delinquent behavior. Future studies should explore the potential value of adoption-specific treatment strategies that take into account the children’s past history.
With regard to internalizing behaviors, levels declined in the first year post-placement and consistently leveled off in the subsequent years of the study. This suggests that although externalizing problems continue to be a significant challenge in adoptive families, internalizing problems, such as depression and anxiety, are greatly reduced after the first year and tend to remain at lower levels afterward. Some children, however, continued to exhibit internalizing problems in the clinical or borderline-clinical ranges, most commonly along the anxiety and depression spectrums. Both internalizing and externalizing problems were pronounced among children with histories of abuse/neglect. After permanent placement in a stable and ostensibly more nurturing home environment, children’s behavior appears to improve.
Our findings for parenting stress followed a similar pattern to those for behavior problems, particularly externalizing problems. Again, we found evidence of a Time × Age Greater Than 4 at Placement interaction, though in this case, it was only borderline significant. It appears that parents experienced an initial reduction of stress in the first year post-adoption, followed by a plateau in stress levels for parents who adopted older children and an increase in stress for parents who adopted younger children. This difference in trajectories was not as dramatic as that associated with externalizing behaviors, and overall, the levels of parenting stress were lower for parents of children adopted at younger ages. Given the well-documented association between parenting stress and behavior problems (Berry & Barth, 1989; McGlone et al., 2002), it seems likely that the impact of pre-placement risk factors on parenting stress is mediated by the association between those risk factors and child behavior problems (Berry & Barth, 1989; Dance et al., 2002; Sharma, McGue, & Benson, 1996a, 1996b; Simmel, 2007). Future research with larger samples should explore the interplay of child and parent characteristics, behavior problems, and caregiving strategies and their relationship to child and parent outcomes.
These findings with regard to parental stress are generally in keeping with previous work showing that most parents report that the impact of the adoption on the family remains the same, or becomes more positive, over time (Groze, 1996). Based on the present analyses, it is unclear whether the decrease in parenting stress is a natural part of a family’s adjustment to adoptive placement or a response to services obtained following placement. Future research examining service use among these families would be informative in elucidating the factors contributing to decreases in parenting stress over time.
Consistent with other studies (Simmel et al., 2007), none of the biological risk factors were related to behavioral or parenting stress outcomes, suggesting the particular importance of environmental risk factors in the expression of behavior problems. We were unable to draw conclusions about the relationship between prenatal substance exposure and behavioral or parenting stress outcomes because 90% of the sample experienced prenatal substance exposure. Even with the possible protective effects of adoption for behavior problems, the longer-term general elevations in externalizing behavior could reflect effects of prenatal substance exposure.
There are important limitations to the current study. Although sizable for a study of children adopted from foster care, the sample size was not large in absolute terms, which limited the power available to detect significant relationships. Fitting outcome models separately facilitates interpretation but could be viewed as introducing multiple-testing concerns. We did not incorporate any formal statistical adjustments for multiple comparisons due to the exploratory nature of our investigation; rather, we view findings of statistical significance as provisional and subject to validation in future research. Regarding measurement, our baseline measures were not obtained until after the children were placed in their adoptive homes. In addition, the sample was drawn from a supportive program for adoptive families; this population may differ from other families adopting from foster care. For example, parents in our sample had access to premier adoption support services and could have availed themselves of supportive educational and mental health services for their children. In addition, the lack of a control group precludes comparisons with parents who did not take part in TIES with the trajectories of children adopted internationally, or with the trajectories of children adopted domestically through private agencies. However, in the context of the existing literature and normative samples of children, the study yielded a number of findings that are consistent with other research (e.g., Dance et al., 2002; Simmel, 2007) while offering additional texture, given the profile of our study sample and insights flowing from the follow-up assessments available to us.
Additional limitations are related to missing data. Some baseline characteristics were not available from certain families, and attrition has the potential to introduce biases. The random-effect analysis framework implicitly assumes that missing outcomes are missing at random (e.g., Rubin, 1987), which is not known with certainty, and which could influence the interpretation to some extent. A variety of scenarios related to participant dropout are conceivable, with potential implications for study findings. For example, it is possible that parents who adopted younger children were more likely to drop out of the program if their children were doing well, which could be translated into an illusory increase over time in parental stress and externalizing scores. Alternately, it is possible that changes in externalizing scores are more apparent and have a greater impact on willingness to stay in the study than do changes in internalizing scores, which also could affect the interpretation of study findings.
The current study is among the few to examine the long-term outcomes of children adopted from the foster care system at an older age. These children experienced multiple environmental and biological risk factors, which placed them at heightened risk for externalizing and internalizing behavior problems later in life. Following the trajectories of these children over time, it appears that children’s behavior problems and parents’ stress improved and stabilized. However, behavior problems did persist over time, highlighting the importance of developing targeted interventions and support services for children adopted from foster care and their adoptive parents.
Development of a program that combines evidence-based cognitive–behavioral child psychotherapy techniques with current thinking about attachment, trauma, and loss would be especially useful. Specific behavioral problems such as food hoarding, lying, and stealing experienced by children adopted older from foster care can be frequently adaptive when living in their previous unpredictable abusive or neglectful situations. Understanding such behaviors through the lens of children’s past experience and developing interventions that take this understanding into account would be very helpful in reducing problem behaviors. Such services and programs should also give at least as much attention to the adoptive parents who will hopefully serve as positive nurturing change agents as work directly with the child. Parents adopting older children from foster care may benefit from both support from a therapist as well as the help they may receive from support groups of parents similarly adopting from foster care.
Supplementary Material
Figure 2.
Predicted CBCL internalizing score by age at adoption.
Note. CBCL = Child Behavior Checklist.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Writing of this manuscript was supported by the following grants from the National Institute of Mental Health: K01MH083694 (Nadeem) and P30MH082760 (Belin, Miranda). Additional support was received from the National Institutes of Health (NIH)/National Center for Advancing Translational Science UCLA Clinical and Translational Science Institute (CTSI) Award UL1TR000124 (Belin).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abidin RR. Parenting stress index manual. Charlottesville, VA: Pediatric Psychology Press; 1983. [Google Scholar]
- Abidin RR, Lloyd B. Revision of the Parenting Stress Index. Journal of Pediatric Psychology. 1985;10:169–177. doi: 10.1093/jpepsy/10.2.169. [DOI] [PubMed] [Google Scholar]
- Achenbach TM. Manual for the CBCL 4–18. Burlington: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA preschool forms and profiles. Burlington: Department of Psychiatry, University of Vermont; 2001. [Google Scholar]
- Bada HS, Das A, Bauer CR, Shankaran S, Lester B, LaGasse L, … Higgins R. Impact of prenatal cocaine exposure on child behavior problems through school age. Pediatrics. 2007;119:e348–e359. doi: 10.1542/peds.2006-1404. [DOI] [PubMed] [Google Scholar]
- Barth RP, Brooks D. A longitudinal study of family structure and size and adoption outcomes. Adoption Quarterly. 1997;1(1):29–56. [Google Scholar]
- Barth RP, Miller JM. Building effective post-adoption services: What is the empirical foundation? Family Relations. 2000;49:447–455. [Google Scholar]
- Berlin M, Vinnerljung B, Hjern A. School performance in primary school and psychosocial problems in young adulthood among care leavers from long term foster care. Children and Youth Services Review. 2011;33:2489–2497. [Google Scholar]
- Berry M, Barth RP. Behavior problems of children adopted when older. Children and Youth Services Review. 1989;11:221–238. [Google Scholar]
- Bimmel N, Juffer F, van Ijzendoorn MH, Bakermans-Kranenburg MJ. Problem behavior of internationally adopted adolescents: A review and meta-analysis. Harvard Review of Psychiatry. 2003;11:64–77. doi: 10.1080/10673220303955. [DOI] [PubMed] [Google Scholar]
- Brand AE, Brinich PM. Behavior problems and mental health contacts in adopted, foster, and nonadopted children. Journal of Child Psychology and Psychiatry. 1999;40:1221–1229. [PubMed] [Google Scholar]
- Brannan AM, Heflinger CA. Caregiver, child, family, and service system contributors to caregiver strain in two child mental health service systems. The Journal of Behavioral Health Services & Research. 2006;33:408–422. doi: 10.1007/s11414-006-9035-1. [DOI] [PubMed] [Google Scholar]
- Brannan AM, Heflinger CA, Bickman L. The Caregiver Strain Questionnaire: Measuring the impact on the family of living with a child with serious emotional disturbance. Journal of Emotional and Behavioral Disorders. 1997;5:212–222. [Google Scholar]
- Burke WT. Unpublished doctoral dissertation. Institutes of Child Psychology, University of Virginia; Charlottesville: 1978. The development of a technique for assessing the stresses experienced by parents of young children. [Google Scholar]
- Crea TM, Barth RP, Guo S, Brooks D. Behavioral outcomes for substance-exposed adopted children: Fourteen years postadoption. American Journal of Orthopsychiatry. 2008;78:11–19. doi: 10.1037/0002-9432.78.1.11. [DOI] [PubMed] [Google Scholar]
- Dance C, Rushton A, Quinton D. Emotional abuse in early childhood: Relationships with progress in subsequent family placement. Journal of Child Psychology and Psychiatry. 2002;43:395–407. doi: 10.1111/1469-7610.00030. [DOI] [PubMed] [Google Scholar]
- Erich S, Leung P. Factors contributing to family functioning of adoptive children with special needs: A long term outcome analysis. Children and Youth Services Review. 1998;20:135–150. [Google Scholar]
- Feigelman W. Adjustments of transracially and inracially adopted young adults. Child and Adolescent Social Work Journal. 2000;17:165–183. [Google Scholar]
- Frasch KM, Brooks D. Normative development in transracial adoptive families: An integration of the literature and implications for the construction of a theoretical framework. Families in Society. 2003;84:201–212. [Google Scholar]
- Garland AF, Hough RL, McCabe KM, Yeh M, Wood PA, Aarons GA. Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:409–418. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- Glidden LM. Adopted children with developmental disabilities: Post-placement family functioning. Children and Youth Services Review. 1991;13:363–377. [Google Scholar]
- Glidden LM, Pursley JT. Longitudinal comparisons of families who have adopted children with mental retardation. American Journal on Mental Retardation. 1989;94:272–277. [PubMed] [Google Scholar]
- Grotevant HD, Manfred H, van Dulmen M, Dunbar N. Antisocial behavior of adoptees and nonadoptees: Prediction from early history and adolescent relationships. Journal of Research on Adolescence. 2006;16:105–131. [Google Scholar]
- Groze V. A 1 and 2 year follow-up study of adoptive families and special needs children. Children and Youth Services Review. 1996;18:57–82. [Google Scholar]
- Hansen ME. Using subsidies to promote the adoption of children from foster care. Journal of Family and Economic Issues. 2007;28:377–393. doi: 10.1007/s10834-007-9067-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juffer F, van Ijzendoorn MH. Behavior problems and mental health referrals of international adoptees: A meta-analysis. Journal of the American Medical Association. 2005;293:2501–2515. doi: 10.1001/jama.293.20.2501. [DOI] [PubMed] [Google Scholar]
- Keyes MA, Sharma A, Elkins IJ, Iacono WG, McGue M. The mental health of US adolescents adopted in infancy. Archives of Pediatric Adolescent Medicine. 2008;162:419–425. doi: 10.1001/archpedi.162.5.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MS. Determinants of low birth weight: Methodological assessment and meta-analysis. Bulletin of the World Health Organization. 1987;65:663–737. [PMC free article] [PubMed] [Google Scholar]
- LaGasse LL, Seifer R, Lester BM. Interpreting research on prenatal substance exposure in the context of multiple confounding factors. Clinical in Perinatology. 1999;26:39–54. [PubMed] [Google Scholar]
- Little RJ, D’Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, … Stern H. The prevention and treatment of missing data in clinical trials. New England Journal of Medicine. 2012;367:1355–1360. doi: 10.1056/NEJMsr1203730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJ. Missing-data adjustments in large surveys. Journal of Business & Economic Statistics. 1988;6:287–301. [Google Scholar]
- Lochman JE, Bierman KL, Coie JD, Dodge KA, Greenberg MT, McMahon RJ, Pinderhughes EE. The difficulty of maintaining positive intervention effects: A look at disruptive behavior, deviant peer relations, and social skills during the middle school years. The Journal of Early Adolescence. 2010;30:593–624. doi: 10.1177/0272431609340513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlone K, Santos L, Kazama L, Fong R, Mueller C. Psychological stress in adoptive parents of special needs children. Child Welfare. 2002;81(2):151–171. [PubMed] [Google Scholar]
- McMillen JC, Zima BT, Scott LD, Auslander WF, Munson MR, Ollie MT, Spitznagel EL. Prevalence of psychiatric disorders among older youths in the foster care system. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:88–95. doi: 10.1097/01.chi.0000145806.24274.d2. [DOI] [PubMed] [Google Scholar]
- Messinger DS, Bauer CR, Das A, Seifer R, Lester BM, Lagasse LL, … Poole WK. The maternal lifestyle study: Cognitive, motor, and behavioral outcomes of cocaine-exposed and opiate-exposed infants through three years of age. Pediatrics. 2004;113:1677–1685. doi: 10.1542/peds.113.6.1677. [DOI] [PubMed] [Google Scholar]
- Milan S, Pinderhughes EE The Conduct Problems Prevention Research Group. Family instability and child maladjustment trajectories during elementary school. Journal of Abnormal Child Psychology. 2006;34:40–53. doi: 10.1007/s10802-005-9007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BC, Fan X, Grotevant HD, Christensen M, Coyl D, van Dulmen M. Adopted adolescents’ overrepresentation in mental health counseling: Adoptees’ problems or parents’ lower threshold for referral? Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1504–1511. doi: 10.1097/00004583-200012000-00011. [DOI] [PubMed] [Google Scholar]
- Nalavany B, Glidden L, Ryan S. Parental satisfaction in the adoption of children with learning disorders: The role of behavior problems. Family Relations. 2009;58:621–633. [Google Scholar]
- National Research Council. The prevention and treatment of missing data in clinical trials (Panel on Handling Missing Data in Clinical Trials, Committee on National Statistics, Division of Behavioral and Social Sciences and Education) Washington, DC: The National Academies Press; 2010. [Google Scholar]
- Nelson KA. On the frontier of adoption: A study of special-needs adoptive families. New York, NY: Child Welfare League of America; 1985. [Google Scholar]
- Newton R, Litrownik AJ, Landsverk JA. Children and youth in foster care: Disentangling the relationship between problem behaviors and number of placements. Child Abuse & Neglect. 2000;24:1363–1374. doi: 10.1016/s0145-2134(00)00189-7. [DOI] [PubMed] [Google Scholar]
- Olsen P, Laara E, Rantakallio P, Jarvelin MR, Sarpola A, Hartikainen AL. Epidemiology of preterm delivery in two birth cohorts with an interval of 20 years. American Journal of Epidemiology. 1995;142:1184–1193. doi: 10.1093/oxfordjournals.aje.a117577. [DOI] [PubMed] [Google Scholar]
- Reijneveld S, de Kleine M, van Baar A, Kollee L, Verhaak C, Verhulst F, Verloove Vanhorick SP. Behavioural and emotional problems in very preterm and very low birthweight infants at age 5 years. Archives of Disease in Childhood Fetal & Neonatal Edition. 2006;91:423–428. doi: 10.1136/adc.2006.093674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal JA, Groze V. Special-needs adoption: A study of intact families. The Social Service Review. 1990;64:475–505. [Google Scholar]
- Rosenthal JA, Groze VK. A longitudinal study of special-needs adoptive families. Child Welfare. 1994;73:689–706. [PubMed] [Google Scholar]
- Rosenthal JA, Schmidt D, Conner J. Predictors of special needs adoption disruption: An exploratory study. Children and Youth Services Review. 1988;10:101–117. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley; 1987. [Google Scholar]
- Rubin DM, Alessandrini EA, Feudtner C, Mandell DS, Localio AR, Hadley T. Placement stability and mental health costs for children in foster care. Pediatrics. 2004;113:1336–1341. doi: 10.1542/peds.113.5.1336. [DOI] [PubMed] [Google Scholar]
- Rushton A, Dance C. The adoption of children from public care: A prospective study of outcome in adolescence. Journal of American Academy of Child & Adolescent Psychiatry. 2006;45:877–883. doi: 10.1097/01.chi.0000220850.86768.e8. [DOI] [PubMed] [Google Scholar]
- Sharma A, McGue M, Benson P. The emotional and behavioral adjustment of United States adopted adolescents: Part I. An overview. Children and Youth Services Review. 1996a;18:83–100. [Google Scholar]
- Sharma A, McGue M, Benson P. The emotional and behavioral adjustment of United States adopted adolescents: Part II. Age at adoption. Children and Youth Services Review. 1996b;18:101–114. [Google Scholar]
- Silverman AR. Outcomes of transracial adoption. The Future of Children. 1993;3(1):104–118. [Google Scholar]
- Simmel C. Risk and protective factors contributing to the longitudinal psychosocial well-being of adopted foster children. Journal of Emotional and Behavioral Disorders. 2007;15:237–249. [Google Scholar]
- Simmel C, Barth RP, Brooks D. Adoptive foster youths’ psychosocial functioning: A longitudinal perspective. Child & Family Social Work. 2007;12:336–348. [Google Scholar]
- Simmel C, Brooks D, Barth RP, Hinshaw SP. Externalizing symptomatology among adoptive youth: Prevalence and preadoption risk factors. Journal of Abnormal Child Psychology. 2001;29(1):57–69. doi: 10.1023/a:1005251513130. [DOI] [PubMed] [Google Scholar]
- Tieman W, van der Ende J, Verhulst FC. Psychiatric disorders in young adult intercountry adoptees: An epidemiological study. American Journal of Psychiatry. 2005;162:592–598. doi: 10.1176/appi.ajp.162.3.592. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services: Administration for Children and Families. Trends in foster care and adoption: FFY 2002-FFY2013. 2014 Retrieved from http://www.acf.hhs.gov/sites/default/files/cb/trends_fostercare_adoption2013.pdf.
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software. 2011;45(3):1–67. [Google Scholar]
- Vaughan EL, Feinn R, Bernard S, Brereton M, Kaufman JS. Relationships between child emotional and behavioral symptoms and caregiver strain and parenting stress. Journal of Family Issues. 2013;34:534–556. doi: 10.1177/0192513X12440949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhulst FC, Althaus M, Versluis-den Bieman HJ. Problem behavior in international adoptees: I. An epidemiological study. Journal of the American Academy of Child & Adolescent Psychiatry. 1990a;29:94–103. doi: 10.1097/00004583-199001000-00015. [DOI] [PubMed] [Google Scholar]
- Verhulst FC, Althaus M, Versluis-den Bieman HJ. Problem behavior in international adoptees: II. Age at placement. Journal of the American Academy of Child & Adolescent Psychiatry. 1990b;29:104–111. doi: 10.1097/00004583-199001000-00016. [DOI] [PubMed] [Google Scholar]
- Warren S. Lower threshold for referral for psychiatric treatment for adopted adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:512–517. doi: 10.1097/00004583-199205000-00019. [DOI] [PubMed] [Google Scholar]
- Wierzbicki M. Psychological adjustment of adoptees: A meta-analysis. Journal of Clinical Child Psychology. 1993;22:447–454. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.