Abstract
Background:
Recently, modifications of Aβ1-42 levels in CSF and plasma associated with improvement in memory and language functions have been observed in patients with mild-moderate Alzheimer’s disease (AD) treated with plasma exchange (PE) with albumin replacement.
Objective:
To detect structural and functional brain changes in PE-treated AD patients as part of a Phase II clinical trial.
Methods:
Patients received between 3 and 18 PE with albumin (Albutein® 5%, Grifols) or sham-PE (controls) for 21 weeks (divided in one intensive and two maintenance periods) followed by 6-month follow-up. Brain perfusion assessed by SPECT scans using an automated software (NeuroGam®) and brain structural changes assessed by MRI were performed at weeks 0 (baseline), 21, and 44 (with additional SPECT at weeks 9 and 33). Statistical parametric mapping (voxel-based analysis, SPM) and Z-scores calculations were applied to investigate changes to baseline.
Results:
42 patients were recruited (39 evaluable; 37 analyzed: 18 PE-treated; 19 controls). There was a trend toward decreasing hippocampi and total intracranial volume for both patient groups during the study (p < 0.05). After six months, PE-treated patients had less cerebral perfusion loss than controls in frontal, temporal, and parietal areas, and perfusion stabilization in Brodmann area BA38-R during the PE-treatment period (p < 0.05). SPM analysis showed stabilization or absence of progression of perfusion loss in PE-treated patients until week 21, not observed in controls.
Conclusions:
Mild-moderate AD patients showed decreased brain volume and impairment of brain perfusion as expected for the progression of the disease. PE-treatment with albumin replacement favored the stabilization of perfusion.
Keywords: Albumin, Alzheimer’s disease, magnetic resonance imaging, plasma exchange, single-photon emission computed tomography
INTRODUCTION
Alzheimer’s disease (AD), as a neurodegenerative process, is expressed by cognitive deterioration manifested in the form of memory loss, language alterations, visual-spatial deficits, impaired recognition capacity, and attention loss, among the most relevant neuropsychological aspects. Non-cognitive symptoms or neuropsychiatric alterations often accompany AD, with depression and behavioral disorders being the most prevalent manifestations in the early stages of the disease [1].
At present, it is only possible to evaluate progression of the disease on the basis of clinical data, cognitive function scales, and imaging and biochemical marker (i.e., surrogate markers). The diagnostic utility of different neuroimaging techniques is being explored. Computed axial tomography (CAT) is useful for detecting some causes of dementia, although it is unable to precisely distinguish between early AD and normal aging [2]. In a similar way, single-photon emission computed tomography (SPECT) might prove useful for establishing a differential diagnosis in dementia [3, 4]. Lastly, magnetic resonance imaging (MRI) offers superior anatomical discrimination, and generates a more precise image of the affected brain areas [5]. Other technologies and ways of evaluating the images obtained are also being investigated.
Current treatment of AD is not curative but symptomatic [6, 7]. The accumulation of amyloid-β peptide (Aβ) in the extracellular spaces of the AD brain and in the walls of the cerebral blood vessels constitutes one of the most important targets for the development of new therapies. However, pivotal clinical trials that pharmacologically targeted Aβ to improve AD function have so far failed [8–10], thus questioning the validity of continuing such studies [11]. Interestingly, the “sink hypothesis” for peripheral Aβ clearance to induce concomitant changes in brain Aβ levels is being explored as a therapeutic strategy for AD treatment.
Matsuoka et al. reported that peripheral sequestering of plasma Aβ results in a reduction of Aβ in both the cerebrospinal fluid (CSF) and in the brain tissues [12]. Taking this approach a step further, a novel strategy that uses plasmapheresis with plasma exchange (PE) for the treatment of AD is being developed on the basis that the vast majority of Aβ circulating in blood (around 90%) is bound to albumin in a 1:1 ratio [13]. Thus, PE removes patient’s plasma that would contain albumin-bound Aβ, to be replaced by new Aβ-free therapeutic albumin [14] to maintain normal volemia and osmotic balance [15]. Such a process of plasma Aβ sequestration may induce/accelerate the efflux of Aβ from CNS to compensate for the drop of peripheral Aβ, thus redressing the CNS/plasma equilibrium [16].
This neuroimaging study is part of a multicenter, randomized, patient- and rater-blind, controlled Phase II trial (ClinicalTrials.gov Identifier: NCT00742417; EudraCT Number: 2007-000414-36) aimed to evaluate the efficacy and safety of PE with 5% albumin in AD patients [17]. The clinical results of the trial showed that PE was able not only to mobilize Aβ1-42 in CSF and plasma, but was also associated with an improvement in memory and language function, in comparison to a control group of AD patients undergoing a simulated (sham) PE, who experienced the cognitive decline expected in AD [17]. In this part of the trial, we assessed whether changes in the neuroimaging analyses paralleled the previous findings of Aβ mobilization and cognition improvement observed in PE-treatedpatients.
MATERIAL AND METHODS
Objectives
This study was aimed to detect structural and functional brain modifications in PE-treated AD patients in comparison to untreated patients (controls). The first objective was to evaluate the changes in volume of the hippocampus, posterior cingulate cortex, and other associated areas based on neuroimaging studies with MRI. The second objective was to determine possible variations in brain hypoperfusion based on SPECT imaging.
Patients
Patients were recruited from 4 different centers, 2 in Spain and 2 in USA. To be eligible for participation in the trial, the patients had to meet the following requirements: males or females between 55–85 years of age, diagnosed of probable AD (NINCDS-ADRDA criterion, and a MMSE score between≥18 and≤26); undergoing stable treatment with acetylcholinesterase inhibitors for the previous three months; and absence of cerebrovascular disease as assessed by CAT or MRI obtained in the 12 months prior to recruitment.
Patients meeting any of the following criteria could not participate in the trial: Any contraindication or difficulty with receiving PE (e.g., difficult venous access, behavioral disorders, a history of frequent adverse reactions to blood products; hypersensitivity to albumin or allergies to any of the components of human albumin 5%); abnormal coagulation or laboratory parameters (e.g., hypocalcemia Ca++ <8.7 mg/dL; thrombocytopenia <100,000/μL; fibrinogen <1.5 g/L; prothrombin time [Quick] p < 60% versus control; angiotensin-converting enzyme inhibitors or beta-blocker treatment and bradycardia <60/min; plasma creatinine >2 mg/dL; alanine aminotransferase >2.5×upper limit of normal; bilirubin >2 mg/dL); uncontrolled high blood pressure and/or heart disease; participation in other clinical trials or the use of any other investigational drug in the three months prior to the start of the study; fewer than six years of education; and any condition that complicated adherence to the study protocol.
The patient and a close relative or legal representative signed the informed consent form to participate in the trial.
Study design
Two weeks from the first visit (recruitment) patients were allocated for screening and randomization (1:1 ratio to either the control group or the PE-treatment group). After these two weeks, the treatment period began which consisted of undergoing up to 18 PE (removal of approximately one plasma volume with simultaneous substitution by a similar volume of 5% human albumin) in 3 periods of 6 PE each, according to the following schedule: 1) Intensive treatment period: 3 weeks with two PE per week; 2) Maintenance treatment period I: 6 weeks with one weekly PE; 3) Maintenance treatment period II: 12 weeks with one PE every two weeks; and 4) Follow-up period without treatment of 6 months. All patients subjected to at least three PE sessions during the intensive treatment period were considered for analysis.
The control group was subjected to sham treatment (simulated PE without invasive procedures) [17]. These patients undertook the same visits schedule as the patients in the PE-treatment group.
The therapeutic albumin product for PE was Human Albumin Grifols® / Albutein® 5% (Grifols, Barcelona, Spain). The volume of each PE was calculated from body weight, height and hematocrit (approximately 35–45 mL/kg, corresponding to a volume of 2500–3000 mL). The doses and infusion rates of Albutein® 5% administered to the treatment group were based on the previous study [17, 18].
MRI was carried out at baseline (week 0), after the PE-treatment period (week 21) and after the follow-up period (week 44). A margin of±7 days was allowed in each time point. SPECT was carried out at baseline (week 0), after the Maintenance Period I (week 9) after the Maintenance Period II (week 21) and during and after the follow-up period (weeks 33 and 44).
MRI determinations
MRI study was carried out to determine possible structural changes in volume of the hippocampus, posterior cingulate region, and total intracranial volume (TIV). MRI was performed with a 1.5 Tesla magnet (GE Healthcare, Chicago IL, USA) with a real-time acquisition system (real-time functional MRI [fMRI]). LX 9.1 M4 software was used. The gradient amplitude was 40 mT/m, with a slew rate of 150 T/m/s. The MRI scans were examined by a clinical neuroradiologist who was blind to the study group and the clinical records of the patient. The neuroradiologist in turn issued a report and was held responsible for communicating any imaging anomalies to the investigating team. Once all the study MRI scans had been obtained, they were analyzed using comprehensive visual rating scale (CVRS) standards. The 3D-SPGR, imaged were: 1) reconstructed in the axial plane, aligning with a standard reference image (MNI T1 matrix); 2) tracing of the hippocampus and the posterior cingulate gyrus using standard software; and 3) analysis of the volume of the hippocampus and of the posterior cingulate region [19]. The images were processed using voxel based morphometry, in statistical parametric mapping (SPM) to determine local concentration of gray matter volumes on a voxel-by-voxel basis [20].
SPECT determinations
The SPECT study was carried out according to the usual protocol of each center to determine possible variations in brain hypoperfusion. A gamma camera with two detectors with low-energy, high-resolution collimators and parallel orifices was used. The tracer (740-1000 MBq of 99mTc-ECD) was administered intravenously with physiological saline in a quiet room, with the patient in the waking state and with the eyes open, but with minimal visual or acoustic stimuli. After waiting 20 minutes to two hours, 64 images were acquired (one every 3°) with a 128*128 acquisition matrix and an acquisition time of 25–30 seconds per image. The total number of counts was≥8 million. The pixel size was 2.9 mm, with a rotation radius of 15 cm (noncircular). Reconstruction was carried out by filtered retroprojection (Butterworth) or on an iterative OSEM basis. The images were stored in DICOM format.
Five SPECT studies per patient were made and compared with a similar number of controls. A qualitative evaluation was performed by an experienced specialist who was blind to the group and the clinical records of the patient. Individual quantification was carried out on a semiautomatic basis in cortical volumes of interest (VOI), using SPM8. The study groups and the patients with themselves (baseline versus final) were compared.
Data analysis
Volumetry
The hippocampus was segmented manually by a trained operator who was blind to the study group and the clinical records of the patient. Volume of the posterior cingulum was measured by morphometry based on T1-weighted MR images of gray matter. TIV was measured by morphometry and taken as the sum of the volumes of gray matter, white matter, and CSF (obtained from the segmented baseline MRI images).
Longitudinal analysis of change between the value of baseline volume (week 0) and the volume at week 21 (treatment period) and week 44 (end of follow-up), for the treatment group and the control group, was carried out by an analysis of covariance (ANCOVA). The analysis provided adjusted (least-squares) mean and 95% confidence intervals as output and the change from baseline value at the last available measurement as dependent variable, treatment group as a factor, and the baseline value as a covariate. The volumes were examined with a mixed model for repeated measures between-group differences in values at week 21 and week 44. The dependent variable in each analysis was the change from baseline. Fixed effects were treatment, visit, and treatment-by-visit interaction.
Brain perfusion
Cerebral metabolism was assessed as the degree of brain perfusion following three approaches: Individual Analysis with NeuroGam® software (Segami Corporation, Columbia MD, USA), Individual Analysis with VOI, and Global Analysis (patterns) with SPM8. A normal database was created with 22 healthy subjects (AD-asymptomatic) of age and sex ratio similar to those of the study patients to be used as reference (reference group) to ascertain the normal distributions of the brain taking into account variations of normality and possible differences due to sex or age of subjects.
For Individual Analysis with NeuroGam®, the first step was to create the normal database using the reference group and Talairach space normalization along with the age range, tracer and characteristics of the person processed. Thereafter, patient images were normalized to determine the Z-scores (a minimum of two standard deviations [SD] with respect to mean were considered) for each patient compared to the normal database images with the same characteristics (tracer, age range, correction, etc.). In this way, the study of each patient was evaluated individually. Following that, the rendered image was also obtained, with the percentages representing the percent of change between the two studies. Its primary use is for individual visual monitoring of the evolution of the disease. Using these data, a visual inspection was made of the rendered images and a table was constructed to show the initial condition (baseline) for each group of patients (rounded to 5% multiples) by lobe involved and number of lobes involved.
For Individual Analysis with VOI, the scans were spatially normalized to compare one with each other and be able to use the standardized and digitalized cerebral atlases. For this purpose, the reconstructed images were re-oriented without correction for attenuation and normalized using SPM. Thereafter, the areas or regions that are known to be involved in Alzheimer’s disease were selected according to reference studies [21–23]. With that purpose, the arithmetic mean (calculated in counts per pixel [cpp]) for both hemispheres was obtained for each of the following Brodmann areas: BA 7, BA 9, BA 10, BA 21, BA 22, BA 23-24, BA 37, BA 38, BA 39, BA 40, and BA 46. Longitudinal statistical analysis was carried out by ANCOVA as done in MRI. In this case, the analysis of change was performed between the value of baseline images (week 0) and the value of images at weeks 9, 21, 33, and 44.
For Global Analysis (patterns) with SPM, the images already normalized spatially in the VOI analysis were also reduced and normalized in intensity. A general design matrix was created using a full factorial test with two factors: 1) Time, with 5 levels (weeks 0, 9, 21, 33, and 44); and 2) Group, with 3 levels (reference group, control group and treatment group). The degree of disease in each of the groups was observed compared to the normal reference group at each week. For this analysis, appropriate contrasts were selected for comparisons and uncorrected p = 0.001 and a κ= 100 voxels were used.
RESULTS
Patients characteristics
Forty-two patients with mild to moderate AD were randomized (21 to the PE treatment group and 21 to the control group with sham PE treatment). Thirty-nine patients provided baseline and longitudinal data (evaluable population), 19 in the PE treatment group (15 women; median age: 65.0, years [Q1,Q3:60.0–76.0]; MMSE score: 22.6±2.7 SD) and 20 in the control group (15 women; median age 65.5 years [Q1,Q3:58.0–78.0]; MMSE score: 20.9±3.1 SD). The characteristics of the two study groups were comparable. Median exposure to treatment of the 39 evaluable patients was 155 days (range: 1–166). Two patients did not undergo at least three PE sessions during the intensive treatment period and were therefore not included in the analyzed population (37 patients: 18 in the PE treatment group and 19 in the control group). In the 22 healthy subjects of the reference group (MMSE score >27), there were 15 women and median age was 63.5 years (Q1,Q3:51.5–67.5).
Analysis of structural changes by MRI
There was a statistically significant decrease in volume over visits in both study groups for both left and right hippocampi and TIV (p < 0.05), but not for the posterior cingulum. Final results of brain volumetry are shown in Table 1. However, no differences were found in the relationship between treatment groups and visits (treatment-by-visit effect) for any of the periods analyzed.
Table 1.
Brain volumetry measurements (cm3) performed at week 0 (baseline), 21 (end of treatment) and 44 (end of follow-up) in plasma exchange [PE]-treated patients (n = 18) and controls (n = 19) (mean±SD; *p < 0.05 in week 21 versus week 0 and week 44 versus week 21 comparisons)
| Volume (cm3) | ||||
| Brain area | Patient group | Baseline | End of treatment | End of follow-up |
| Left Hippocampus | PE-treated | 1.90±0.41 | 1.76±0.45* | 1.64±0.43* |
| Control | 1.91±0.48 | 1.85±0.4* | 1.76±0.39* | |
| Right Hippocampus | PE-treated | 2.04±0.41 | 1.98±0.41* | 1.88±0.35* |
| Control | 2.14±0.38 | 2.07±0.32* | 1.96±0.34* | |
| Posterior Cingulate | PE-treated | 10.60±1.34 | 10.22±1.58 | 10.60±1.48 |
| Control | 10.38±0.80 | 10.39±0.80 | 10.23±1.06 | |
| Total Intracranial volume | PE-treated | 1034±100 | 990±83* | 985±86* |
| Control | 1064±130 | 1043±120 | 1027±148* | |
Individual analysis of cerebral perfusion with NeuroGam®
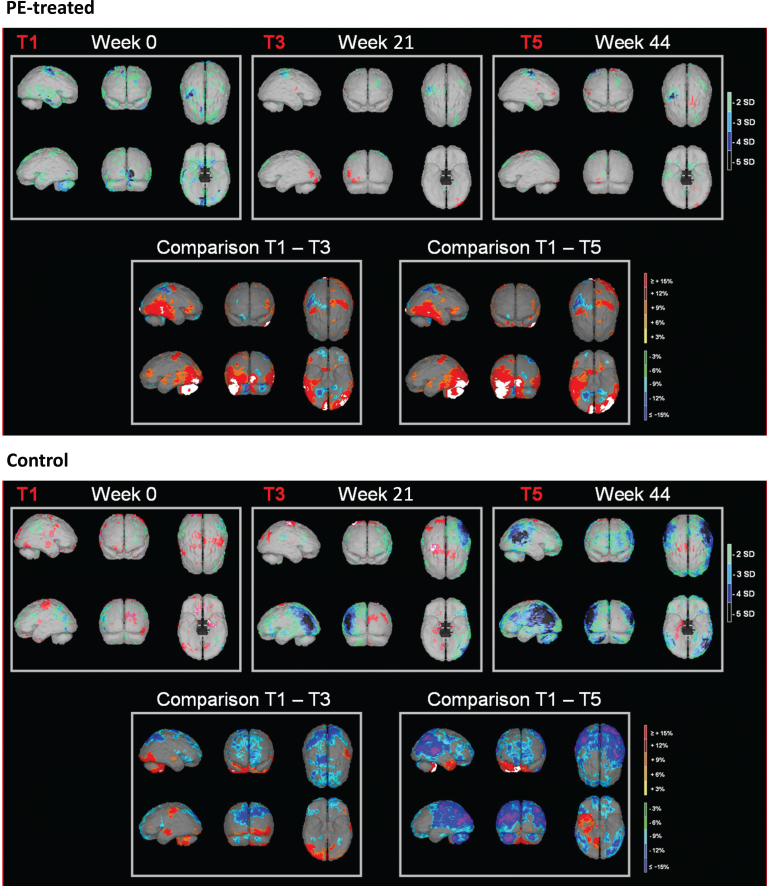
Representative images of NeuroGam® analysis in a control patient and a PE-treated patient are shown in Fig. 1. Visual inspection of the rendered images to set the initial condition (baseline) showed that the control group included more patients with alterations in all lobes (parietal, temporal, and frontal) and more patients with at least one lobe affected (80% versus 65% of patients, respectively) than the PE-treated group. Details are shown in Table 2.
Fig.1.
Representative images of NeuroGam® analysis of brain perfusion in a plasma exchange [PE]-treated patient (upper panel) and an untreated control patient (lower panel). Color scale in images at week 0 (baseline, T1), 21 (end of treatment, T3), and 44 (end of follow-up, T5) indicates Z-score (number of standard deviations [SD] with respect to mean). Color scale in the images of T1–T3 and T1–T5 comparisons indicates the difference (increase or decrease) in percentage.
Table 2.
Percentages of patients showing lobe perfusion alterations (in type and number of lobes) at baseline and their evolution up to the end of the study (n = 18 for plasma exchange [PE]-treated; n = 19 for untreated controls)
| Patients (%) with affected lobes at baseline | Perfusion evolution from baseline to end of the study | ||||||
| Patients (%) with impairment | Patients (%) with improvement | ||||||
| PE-treated | Control | PE-treated | Control | PE-treated | Control | ||
| Affected lobe | Parietal | 35 | 60 | 30 | 15 | 25 | 20 |
| Temporal | 45 | 65 | 20 | 45 | 25 | 10 | |
| Frontal | 30 | 35 | 30 | 50 | 5 | 5 | |
| Number of affected lobes | 0 | 35 | 20 | 40 | 30 | 75 | 75 |
| 1 | 30 | 25 | 40 | 40 | 0 | 15 | |
| 2 | 25 | 30 | 20 | 20 | 20 | 10 | |
| 3 | 10 | 25 | 0 | 10 | 5 | 0 | |
Regarding the evolution of affected lobes from baseline (week 0) compared to the end of the study (week 44), despite some variability it could be observed that the percentage of patients showing lobe perfusion impairment was globally higher in the control group (particularly in frontal and temporal lobes). Conversely, there were more PE-treated patients globally showing lobe perfusion improvement (particularly in parietal and temporal lobes) (see Table 2).
Regarding the evolution of the number of lobes affected, the PE-treatment group had more patients showing 2 to 3 lobes with perfusion improvement whereas the control group had more patients showing 2 to 3 lobes with perfusion impairment (Table 2).
Individual analysis of cerebral perfusion with volumes of interest (VOI)
Baseline perfusion values (in cpp) in controls ranged from 42.7±5.3 in BA 38-L to 63.0±9.8 in BA 7-L, while in PE-treated patients values in the same areas ranged from 43.5±5.9 to 62.4±7.4. At week 21 (end of treatment) and week 44 (end of follow-up), values in BA 38-L in controls were 40.3±3.7 and 43.2±5.4, respectively, while in PE-treated patients the respective values were 43.2±4.4 and 44.3±4.1. In BA 7-L, values in controls at weeks 21 and 44 were 61.5±6.3 and 60.3±6.7, respectively, while in PE-treated patients the respective values were 61.8±7.1 and 60.8±7.2.
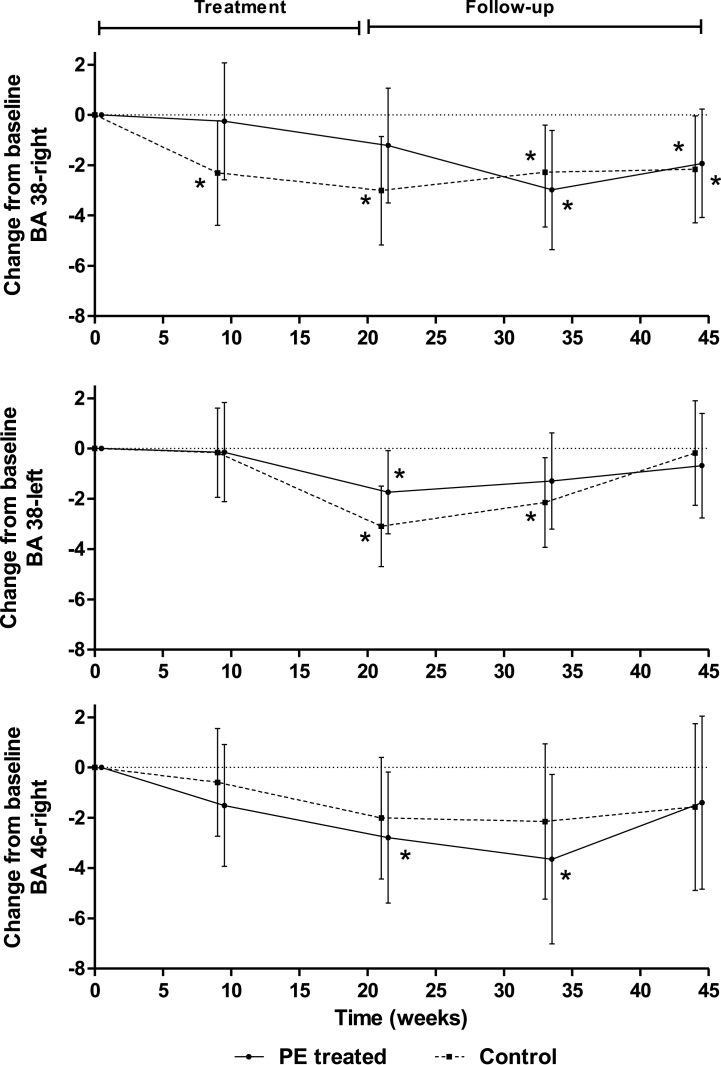
Repeated measures analysis found out that the change from baseline values were not significant for most of the Brodmann areas studied, except for BA 38-R, BA 38-L and BA 46-R. As shown in Fig. 2, a significant visit effect was detected in BA 38-L and BA 46-R (p = 0.0061 and p = 0.0219, respectively), associated with a change of perfusion over time regardless of treatment. Moreover, a significant treatment-by-visit effect (p = 0.0143) was detected in BA 38-R, where the control group showed a significant worsening of perfusion at all time points. By contrast, the PE-treatment group showed a stable perfusion until week 21 (treatment period), as well as a not so marked worsening during the follow up (Fig. 2).
Fig.2.
Repeated measures analysis of SPECT images of the Brodmann areas BA 38 right, BA 38 left, and BA 46 right. Change from values of cerebral perfusion (least square mean±95% CI) at baseline (week 0) to week 21 (end of treatment), week 33 and week 44 (follow-up) in plasma exchange [PE]-treated (n = 18) and untreated control patients (n = 19) is shown. *p < 0.05 versus baseline for individual time points (treatment-by-visit effect in BA 38-R, visit effect in BA 38-L and BA 46-R).
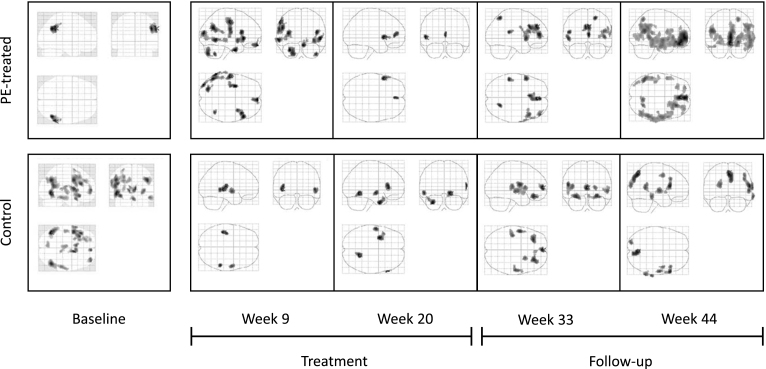
Global analysis of cerebral perfusion with statistical parametric mapping
In this analysis, the control group showed a greater degree of perfusion impairment at baseline in the temporal-parietal regions bilaterally, in contrast to the PE-treated group which showed only unilateral parietal involvement. Representative images are shown in Fig. 3.
Fig.3.
Representative images of SPM analysis of cerebral perfusion loss in plasma exchange [PE]-treated patients (upper panels) and untreated control patients (lower panels). Baseline images (left panels) show the degree of perfusion impairment compared to the normal reference group. Images of perfusion impairment with respect to baseline are shown to end of treatment (week 21), and end of follow-up (week 44).
Longitudinally, the control group showed progressive decrease of perfusion in the temporal and parietal regions and extending toward the frontal region throughout the study. By contrast, the PE-treatment group showed marked stabilization or absence of progression of perfusion decrease until week 21 of the study, coinciding with the period of most intense treatment. Thereafter, decrease of perfusion resumed, extending from the temporal lobes to the frontal lobe (Fig. 3).
DISCUSSION
This neuroimaging study was a part of the Phase II multicenter, randomized, controlled clinical trial in which mild to moderate AD patients were treated with PE with 5% human albumin replacement in comparison to a placebo control group [17]. Clinical results of the Phase II study showed that PE-treatment mobilized Aβ in both CSF and plasma, which was associated with patient improvement in memory and language functions as assessed by cognitive tests [17]. Preliminary neuroimaging data resulting from the pilot study of PE with 5% human albumin replacement [18, 21] detected differences in blood flow in the hippocampus and Brodmann areas between the PE-treated and the untreated control groups. The results of the present study, associated with the Phase II clinical trial, confirmed that PE-treated AD patients did not experience the progressive brain hypoperfusion that was observed in control patients, although such changes did not correlate with brain volumetry.
MRI is a useful diagnostic tool in diagnosing AD [5, 24]. Brain structural changes assessments of our study indicated a progressive decrease in TIV that was similar in both PE-treated and control patient groups. Lower volume in both hippocampi accounted for this change but not for posterior cingulate area. Damage of hippocampus is observed at the time of early AD clinical symptoms [25] and even before AD symptoms appear [26, 27], while hippocampal volume change is considered a marker for AD progression [24].
In contrast to MRI, differential results between patient groups were observed in SPECT cerebral perfusion assessments. In fact, poor correlation between SPECT and MRI measures is not unexpected [28]. The role of hypoperfusion is critical for the understanding of the pathogenesis of AD [29–31]. In our SPECT study, changes in brain perfusion were analyzed under several approaches, individually with NeuroGam® software and through VOI, as well as globally (patterns) with SPM, using a reference group of healthy subjects to set the degree of perfusion impairment at baseline in both patient groups.
Individual Analysis with NeuroGam® suggested an imbalance between the patient groups at baseline. Control group showed greater bilateral parietal and temporal region involvement compared to the treatment group, which showed only unilateral parietal involvement. Although NeuroGam® software can yield false positives when analyzing the temporal lobe [32], Global Analysis with SPM corroborated the results of the Individual Analysis, since the control group had greater severity of damage than the treatment group at baseline, particularly in the parietal and temporal regions.
Nevertheless, dissimilar baseline values should not affect the longitudinal assessments, in which baseline results were compared to the time points related to treatment and follow-up. A higher degree of CNS dysfunction at baseline in the controls would mean a lower margin for worsening. Both the NeuroGam® and SPM analysis showed some beneficial effect of PE treatment in the form of less brain perfusion loss. Results were more variable with NeuroGam®, which could be ascribed to the small sample size. However, that did not preclude the observation that PE-treated patients globally showed a better lobe perfusion than controls at the end of the study. In SPM analysis, the untreated group evolved with progressive hypoperfusion in both the temporal and parietal regions, extending toward the frontal region. In contrast, in the PE-treated group hypoperfusion did not progress through week 21 of the study, more markedly during the first 9 weeks, coinciding with the period of most intense treatment. Thereafter, perfusion decline resumed.
Individual analysis with VOI showed a cerebral perfusion impairment that was statistically significant in three Brodmann areas: BA38-R and -L, and BA46-R. BA 46 corresponds with the dorsolateral prefrontal cortex which plays a role in sustaining attention and working memory [33]. Interestingly, the analysis detected a treatment-by-visit effect in Brodmann area BA 38-R with a progressive perfusion impairment in the untreated group while the PE-treated group remained unchanged during the treatment period, BA 38 corresponds to the temporal pole and it is among the earliest affected by AD [34]. Moreover, BA38 is assumed to play significant role in language [35], which would be consistent with the clinical observations of the trial where PE induced an improvement in language functions which persisted after PE was discontinued [17]. The results of this neuroimaging approach suggest that functional perfusion of the brain but not structural changes in areas such as the hippocampi volume would be associated with the Aβ mobilization and cognitive stabilization induced by PE [31, 36]. Indeed, dissociation between cortical atrophy and perfusion parameters has beendescribed [37].
In AD, microvascular abnormalities are probably the most important [31], which suggest being a therapeutic target of interest. Moreover, our neuroimaging findings together with the clinical results of the same trial [17] would be in agreement not only with the correlation between blood perfusion of the brain and neuropsychological tests that have been previously described, particularly MMSE scores [38], but also with possible interactions between Aβ levels, cerebral blood perfusion and cognition [39]. The ongoing AMBAR (Alzheimer Management by Albumin Replacement) clinical trial (NCT01561053), of which the primary objective is to evaluate cognitive and brain functional changes in AD patients treated with PE with albumin and immunoglobulin [40], will help to shed light on these relationships.
Our study sample was 30 women and 9 men, which is statistically within the generally defined ratio of approximately two-thirds females in AD patients [41]. Apart of the relatively small sample size, possible study limitations would also include the risk of bias associated with methods entailing visual assessment of the images. In addition, not every Brodmann area related to language was analyzed, because the selection was made prior knowing the results of the cognitive tests of the clinical part of the trial. In addition, a better contrast and spatial resolution in brain perfusion could be obtained if positron emission tomography (PET) scans had been used instead of SPECT. Nevertheless, the AMBAR study performed on a larger sample will expand the brain areas analyzed, including fluorodeoxyglucose-PET procedures.
In summary, neuroimaging results of this study indicated that patients with mild to moderate AD showed the decrease of brain volume and impairment of perfusion expected for the progression of the disease. Remarkably, brain perfusion was stabilized in the patients treated with PE with albumin replacement. These findings could be related to the cognitive improvement previously shown in the PE-treated patients.
ACKNOWLEDGMENTS
This study was funded by Grifols. The following investigators are acknowledged for patient recruitment and participation in the clinical study: Fernando Anaya (Nephrology Service, Hospital General Universitario Gregorio Marañón, Madrid, Spain), Pilar Ortiz (Banc de Sang i Teixits, Barcelona, Spain), Javier Olazarán (Neurology Service, Hospital General Universitario Gregorio Marañón, Madrid, Spain), Joshua R. Shua-Haim (Alzheimer’s Research Corporation, Mid Atlantic Geriatric Association, Manchester, NJ, USA), Thomas O. Obisesan (Department of Internal Medicine, Howard University, Washington DC, USA), Joan Ramon Grifols (Banc de Sang i Teixits, Barcelona, Spain), Isidre Ferrer (Institut de Neuropatologia, Hospital Universitario Bellvitge, Barcelona, Spain), and Oscar L. Lopez (Departments of Neurology and Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, USA). James T. Becker (Department of Psychiatry, Neurology and Psychology. University of Pittsburgh, Pittsburgh PA, USA) read and commented on an earlier draft of the manuscript. Jordi Bozzo PhD, CMPP (Grifols) is acknowledged for medical writing and editorial assistance in the preparation of the manuscript.
Authors’ disclosures available online (http://j-alz.com/manuscript-disclosures/17-0693r2).
REFERENCES
- [1]. Feldman HH, Jacova C, Robillard A, Garcia A, Chow T, Borrie M, Schipper HM, Blair M, Kertesz A, Chertkow H (2008) Diagnosis and treatment of dementia: 2. Diagnosis. CMAJ 178, 825–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Naugle RI, Cullum CM, Bigler ED, Massman PJ (1985) Neuropsychological and computerized axial tomography volume characteristics of empirically derived dementia subgroups. J Nerv Ment Dis 173, 596–604. [DOI] [PubMed] [Google Scholar]
- [3]. Sakurai T, Kawashima S, Satake S, Miura H, Tokuda H, Toba K (2014) Differential subtypes of diabetic older adults diagnosed with Alzheimer’s disease. Geriatr Gerontol Int 14(Suppl 2), 62–70. [DOI] [PubMed] [Google Scholar]
- [4]. Song IU, Chung YA, Chung SW, Jeong J (2014) Early diagnosis of Alzheimer’s disease and Parkinson’s disease associated with dementia using cerebral perfusion SPECT. Dement Geriatr Cogn Disord 37, 276–285. [DOI] [PubMed] [Google Scholar]
- [5]. Boelaarts L, Scheltens P, de Jonghe J (2016) Does MRI increase the diagnostic confidence of physicians in an outpatient memory clinic. Dement Geriatr Cogn Dis Extra 6, 242–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Hogan DB, Bailey P, Black S, Carswell A, Chertkow H, Clarke B, Cohen C, Fisk JD, Forbes D, Man-Son-Hing M, Lanctot K, Morgan D, Thorpe L (2008) Diagnosis and treatment of dementia: 5. Nonpharmacologic and pharmacologic therapy for mild to moderate dementia. CMAJ 179, 1019–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Hogan DB, Bailey P, Black S, Carswell A, Chertkow H, Clarke B, Cohen C, Fisk JD, Forbes D, Man-Son-Hing M, Lanctot K, Morgan D, Thorpe L (2008) Diagnosis and treatment of dementia: 4. Approach to management of mild to moderate dementia. CMAJ 179, 787–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Brody M, Liu E, Di J, Lu M, Margolin RA, Werth JL, Booth K, Shadman A, Brashear HR, Novak G (2016) A phase II, randomized, double-blind, placebo-controlled study of safety, pharmacokinetics, and biomarker results of subcutaneous bapineuzumab in patients with mild to moderate Alzheimer’s disease. J Alzheimers Dis 54, 1509–1519. [DOI] [PubMed] [Google Scholar]
- [9]. Cummings JL, Morstorf T, Zhong K (2014) Alzheimer’s disease drug-development pipeline: Few candidates, frequent failures. Alzheimers Res Ther 6, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Vandenberghe R, Rinne JO, Boada M, Katayama S, Scheltens P, Vellas B, Tuchman M, Gass A, Fiebach JB, Hill D, Lobello K, Li D, McRae T, Lucas P, Evans I, Booth K, Luscan G, Wyman BT, Hua L, Yang L, Brashear HR, Black RS (2016) Bapineuzumab 3000 and 3001 Clinical Study Investigators, Bapineuzumab for mild to moderate Alzheimer’s disease in two global, randomized, phase 3 trials. Alzheimers Res Ther 8, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Morris GP, Clark IA, Vissel B (2014) Inconsistencies and controversies surrounding the amyloid hypothesis of Alzheimer’s disease. Acta Neuropathol Commun 2, 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Matsuoka Y, Saito M, LaFrancois J, Saito M, Gaynor K, Olm V, Wang L, Casey E, Lu Y, Shiratori C, Lemere C, Duff K (2003) Novel therapeutic approach for the treatment of Alzheimer’s disease by peripheral administration of agents with an affinity to beta-amyloid. J Neurosci 23, 29–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Kuo YM, Kokjohn TA, Kalback W, Luehrs D, Galasko DR, Chevallier N, Koo EH, Emmerling MR, Roher AE (2000) Amyloid-beta peptides interact with plasma proteins and erythrocytes: Implications for their quantitation in plasma. Biochem Biophys Res Commun 268, 750–756. [DOI] [PubMed] [Google Scholar]
- [14]. Costa M, Ortiz AM, Jorquera JI (2012) Therapeutic albumin binding to remove amyloid-beta. J Alzheimers Dis 29, 159–170. [DOI] [PubMed] [Google Scholar]
- [15]. Meca-Lallana JE, Rodriguez-Hilario H, Martinez-Vidal S, Saura-Lujan I, Carreton-Ballester A, Escribano-Soriano JB, Martin-Fernandez J, Genoves-Aleixandre A, Mateo-Bosch E, Fernandez-Barreiro A (2003) Plasmapheresis: Its use in multiple sclerosis and other demyelinating processes of the central nervous system. An observation study. Rev Neurol 37, 917–926. [PubMed] [Google Scholar]
- [16]. Huang Y, Potter R, Sigurdson W, Kasten T, Connors R, Morris JC, Benzinger T, Mintun M, Ashwood T, Ferm M, Budd SL, Bateman RJ (2012) beta-amyloid dynamics in human plasma. Arch Neurol 69, 1591–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. Boada M, Anaya F, Ortiz P, Olazaran J, Shua-Haim JR, Obisesan TO, Hernández I, Munoz J, Buendia M, Alegret M, Lafuente A, Tarraga L, Nunez L, Torres M, Grifols JR, Ferrer I, Lopez OL, Paez A (2017) Efficacy and safety of plasma exchange with 5% albuminto modify CSF and plasma Aß concentrations and cognitionoutcomes in Alzheimer’s disease patients: A multicenter,randomized, controlled clinical trial. J Alzheimers Dis 56, 129–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Boada M, Ortiz P, Anaya F, Hernandez I, Munoz J, Nunez L, Olazaran J, Roca I, Cuberas G, Tarraga L, Buendia M, Pla RP, Ferrer I, Paez A (2009) Amyloid-targeted therapeutics in Alzheimer’s disease: Use of human albumin in plasma exchange as a novel approach for Abeta mobilization. Drug News Perspect 22, 325–339. [DOI] [PubMed] [Google Scholar]
- [19]. Thompson PM, Hayashi KM, De Zubicaray GI, Janke AL, Rose SE, Semple J, Hong MS, Herman DH, Gravano D, Doddrell DM, Toga AW (2004) Mapping hippocampal and ventricular change in Alzheimer disease. Neuroimage 22, 1754–1766. [DOI] [PubMed] [Google Scholar]
- [20]. Ashburner J, Friston KJ (2000) Voxel-based morphometry–the methods. Neuroimage 11, 805–821. [DOI] [PubMed] [Google Scholar]
- [21]. Roca I, Cuberas-Borros G (2010) Neuroimaging in Alzheimer’s disease: Findings in plasmapheresis with albumin. Rev Neurol 50(Suppl 5), S19–S22. [PubMed] [Google Scholar]
- [22]. Tranfaglia C, Palumbo B, Siepi D, Sinzinger H, Parnetti L (2009) Semi-quantitative analysis of perfusion of Brodmann areas in the differential diagnosis of cognitive impairment in Alzheimer’s disease, fronto-temporal dementia and mild cognitive impairment. Hell J Nucl Med 12, 110–114. [PubMed] [Google Scholar]
- [23]. Valotassiou V, Papatriantafyllou J, Sifakis N, Tzavara C, Tsougos I, Kapsalaki E, Hadjigeorgiou G, Georgoulias P (2012) PerfusionSPECT studies with mapping of Brodmann areas indifferentiating Alzheimer’s disease from frontotemporaldegeneration syndromes. Nucl Med Commun 33, 1267–1276. [DOI] [PubMed] [Google Scholar]
- [24]. Schuff N, Woerner N, Boreta L, Kornfield T, Shaw LM, Trojanowski JQ, Thompson PM, Jack CR Jr, Weiner MW (2009) MRI of hippocampal volume loss in early Alzheimer’s disease in relation to ApoE genotype and biomarkers. Brain 132, 1067–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25]. Braak H, Braak E (1998) Evolution of neuronal changes in the course of Alzheimer’s disease. J Neural Transm Suppl 53, 127–140. [DOI] [PubMed] [Google Scholar]
- [26]. Du AT, Schuff N, Amend D, Laakso MP, Hsu YY, Jagust WJ, Yaffe K, Kramer JH, Reed B, Norman D, Chui HC, Weiner MW (2001) Magnetic resonance imaging of the entorhinal cortex and hippocampus in mild cognitive impairment and Alzheimer’s disease. J Neurol Neurosurg Psychiatry 71, 441–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Jack CR Jr, Petersen RC, Xu YC, O’Brien PC, Smith GE, Ivnik RJ, Boeve BF, Waring SC, Tangalos EG, Kokmen E (1999) Prediction of AD with MRI-based hippocampal volume in mild cognitive impairment. Neurology 52, 1397–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. El Fakhri G, Kijewski MF, Johnson KA, Syrkin G, Killiany RJ, Becker JA, Zimmerman RE, Albert MS (2003) MRI-guided SPECT perfusion measures and volumetric MRI in prodromal Alzheimer disease. Arch Neurol 60, 1066–1072. [DOI] [PubMed] [Google Scholar]
- [29]. Jagust W (2004) Molecular neuroimaging in Alzheimer’s disease. NeuroRx 1, 206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30]. Jagust W, Thisted R, Devous MD Sr, Van Heertum R, Mayberg H, Jobst K, Smith AD, Borys N (2001) SPECT perfusion imaging in the diagnosis of Alzheimer’s disease: A clinical-pathologic study. Neurology 56, 950–956. [DOI] [PubMed] [Google Scholar]
- [31]. Leeuwis AE, Benedictus MR, Kuijer JP, Binnewijzend MA, Hooghiemstra AM, Verfaillie SC, Koene T, Scheltens P, Barkhof F, Prins ND, van der Flier WM (2017) Lower cerebral blood flow is associated with impairment in multiple cognitive domains in Alzheimer’s disease. Alzheimers Dement 13, 531–540. [DOI] [PubMed] [Google Scholar]
- [32]. Wang Y, Liu Z, Liu X (2014) The application of NeuroGam software in aging brain using SPECT. J Nucl Med 55, 2639–2639. [Google Scholar]
- [33]. Petrides M, Pandya DN (1999) Dorsolateral prefrontal cortex: Comparative cytoarchitectonic analysis in the human and the macaque brain and corticocortical connection patterns. Eur J Neurosci 11, 1011–1036. [DOI] [PubMed] [Google Scholar]
- [34]. Ding SL, Van Hoesen GW, Cassell MD, Poremba A (2009) Parcellation of human temporal polar cortex: A combined analysis of multiple cytoarchitectonic, chemoarchitectonic, and pathological markers. J Comp Neurol 514, 595–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35]. Pascual B, Masdeu JC, Hollenbeck M, Makris N, Insausti R, Ding SL, Dickerson BC (2015) Large-scale brain networks of the human left temporal pole: A functional connectivity MRI study. Cereb Cortex 25, 680–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36]. Sun Y, Cao W, Ding W, Wang Y, Han X, Zhou Y, Xu Q, Zhang Y, Xu J (2016) Cerebral blood flow alterations as assessed by 3D ASL in cognitive impairment in patients with subcortical vascular cognitive impairment: A marker for disease severity. Front Aging Neurosci 8, 211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37]. Lacalle-Aurioles M, Navas-Sanchez FJ, Aleman-Gomez Y, Olazaran J, Guzman-De-Villoria JA, Cruz-Orduna I, Mateos-Perez JM, Desco M (2016) The disconnection hypothesis in Alzheimer’s disease studied through multimodal magnetic resonance imaging: Structural, perfusion, and diffusion tensor imaging. J Alzheimers Dis 50, 1051–1064. [DOI] [PubMed] [Google Scholar]
- [38]. Yoon HJ, Park KW, Jeong YJ, Kang DY (2012) Correlation between neuropsychological tests and hypoperfusion in MCI patients: Anatomical labeling using xjView and Talairach Daemon software. Ann Nucl Med 26, 656–664. [DOI] [PubMed] [Google Scholar]
- [39]. Bangen KJ, Clark AL, Edmonds EC, Evangelista ND, Werhane ML, Thomas KR, Locano LE, Tran M, Zlatar ZZ, Nation DA, Bondi MW, Delano-Wood L (2017) Cerebral blood flow and amyloid-beta interact to affect memory performance in cognitively normal older adults. Front Aging Neurosci 9, 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Boada M, Ramos-Fernández E, Guivernau B, Muñoz FJ, Costa M, Ortiz AM, Jorquera JI, Nunez L, Paez A (2016) Treatment of Alzheimer’s disease using a combined therapy of plasma exchangeand hemopheresis with albumin and intravenous immunoglobulin:Rationale and theraeutic approach to the AMBAR study (AlzheimerManagement by Albumin Replacement). Neurología 31, 473–481. [DOI] [PubMed] [Google Scholar]
- [41]. Poirier J, Gauthier S (2011) A disease of epidemic proportions In Alzheimer’s Disease: The Complete Introduction, Melgaard M, ed. Dundurn, Toronto, Canada. [Google Scholar]