Abstract
Objectives
Although many secondary effects of high levels of vanadium (V) and chromium (Cr) overlap with symptoms seen in paediatric patients with chronic kidney disease (CKD), their plasma V and Cr levels are understudied.
Design
Ancillary cross-sectional study to a prospective, longitudinal, randomised controlled trial.
Setting
Children’s Hospital of Western Ontario, London Health Sciences Centre, London, Ontario, Canada.
Participants
36 children and adolescents 4–18 years of age with CKD.
Interventions
1–6 trace element measurements per patient. Cystatin C (CysC) estimated glomerular filtration rate (eGFR) was calculated using the Filler formula. Plasma V and Cr levels were measured using high-resolution sector field inductively coupled mass spectrometry. Anthropomorphic data and blood parameters were collected from our electronic chart programme. Water Cr and V data were obtained from the Ontario Water (Stream) Quality Monitoring Network.
Primary and secondary outcome measures
Primary outcomes: plasma Cr and V. Secondary outcomes: age, season, CysC, CysC eGFR, and Cr and V levels in environmental water.
Results
The median (IQR) eGFR was 51 mL/min/1.73 m2 (35, 75). The median V level was 0.12 µg/L (0.09, 0.18), which was significantly greater than the 97.5th percentile of the reference interval of 0.088 µg/L; 32 patients had at least one set of V levels above the published reference interval. The median Cr level was 0.43 µg/L (0.36, 0.54), which was also significantly greater than the established reference interval; 34 had at least one set of Cr levels above the published reference interval. V and Cr levels were moderately correlated. Only some patients had high environmental exposure.
Conclusions
Our study suggests that paediatric patients with CKD have elevated plasma levels of V and Cr. This may be the result of both environmental exposure and a low eGFR. It may be necessary to monitor V and Cr levels in patients with an eGFR <30 mL/min/1.73 m2.
Trial registration number
NCT02126293; HC#172241.
Keywords: Paediatric nephrology, PUBLIC HEALTH, TOXICOLOGY, Chronic renal failure, Environmental Impact on Health
Strengths and limitations of this study.
This is the first study to examine vanadium (V) and chromium (Cr) in children with chronic kidney disease (CKD).
Our study has a strong cross-sectional design in combination with longitudinal data and a reasonable number of patients for a paediatric study. The instruments used to measure the trace elements are highly precise.
Our study links publicly available data measuring trace elements in drinking water with detailed descriptions of patients to differentiate environmental and CKD-related accumulation of V and Cr.
More subjects would have lead to more precise data, and our patient cohort has a bias towards milder CKD stages. We did not control for fluid or food intake.
There are no detailed studies on the age dependency of paediatric V and Cr concentrations.
Introduction
Vanadium (V, atomic number 23) and chromium (Cr, atomic number 24) are located beside each other on the periodic table and share many points of similarity. Both are predominantly excreted by the kidneys,1 2 are associated with normal human health and with the pathogenesis of several diseases (ie, essential and toxic),3–6 and occur naturally in our surrounding environment.7 8 Metallic V and Cr do not occur in nature and are instead found as compounds in different valence states.8–10 Humans can be exposed to V and Cr through the air, but the majority of contact stems from food and water.7 8 11 They are usually present in low, harmless concentrations in various foods (particularly seafood for V).1 Some nutritional supplements and vitamins also contain V, whose levels can exceed healthy levels.4 11
The principal pentavalent form of V can easily enter a cell via phosphate and sulfate ion channels, rendering this version of V very toxic.12 V also interferes with phosphate-containing enzymes3 4 and can activate several genes and participate in the inflammatory response. The highest initial concentrations of V are found in the kidneys, liver and lungs, and in the long-term it is stored in the bones and muscles.13 14 The effects of V on human health are largely dependent on the type of compound,11 dose, duration and route of exposure.3 4 11 The common hexavalent form of Cr easily enters cells through facilitated uptake, which is more efficient than the simple diffusion used to take up the trivalent form. Free radicals are created in cells when Cr(VI) is reduced to Cr(III).8 It is distributed to and accumulated by the erythrocyte and the highest concentrations of Cr are found in the kidneys and liver. The absorption fraction of ingested Cr is higher when dietary intakes are lower. The major route of elimination of absorbed Cr is through the urine, with unabsorbed Cr recovered in the faeces,2 while V is also mostly excreted through the urine, with some excretion in the faeces.15
V has many systemic effects, including gastrointestinal, respiratory, haematological, immunological and cardiovascular effects.1 7 16 17 The International Agency for Research on Cancer (IARC) has classified V pentoxide as ‘possibly carcinogenic’. Other data also suggest the potential of V to induce developmental effects in humans. It is unknown whether children are affected by V-containing compounds in the same ways as adults.11
The IARC has classified Cr as carcinogenic. Inhalation has been shown to cause lung cancer in humans, and exposure has been shown to cause tumours in the stomach, intestinal tract and lungs in animals.8 Depending on the route of exposure, trivalent and hexavalent Cr are also associated with gastrointestinal, immunological, haematological (including anaemia), reproductive, developmental and other serious effects. Hexavalent Cr is more toxic than its trivalent form, but trace element measurements rarely differentiate between the two.
The dangers V and particularly Cr pose to our health are made clear when the serious systemic effects associated with either acute or chronic exposure to either element in humans are explored in greater depth.
Acute oral exposure to V can cause mild gastrointestinal irritation, such as stomach cramps, mild diarrhoea and nausea.7 Although there are no studies examining the effect of chronic oral exposure to V on human health, chronic exposure to V through inhalation may cause neurocognitive deficits and may impair neurobehavioural abilities, symptoms that are regularly seen in paediatric patients with chronic kidney disease (CKD).18 Chronic exposure to V through inhalation has also been shown to cause immunological effects, such as significant decreases in lymphocyte stimulation and an increase in the incidence of viral and bacterial respiratory infections in children, a vulnerable population.16 Another study examining the health effects of chronically inhaling V found a significant association between V and systolic blood pressure and pulse pressure in an elderly population.17
Cr appears even more toxic; acute oral exposure has been linked to (1) death, and at lethal doses respiratory effects such as pleural effusions, pulmonary oedema, bronchitis and bronchopneumonia; (2) cardiovascular effects such as cardiopulmonary arrest, cardiac arrest, and a drop in cardiac output, heart rate and blood pressure; (3) gastrointestinal haemorrhage and necrosis, abdominal pain and vomiting; (4) haematological effects such as inhibited coagulation; (5) hepatic effects such as the development of jaundice, fatty degeneration, hepatic necrosis, and increased bilirubin, serum lactic dehydrogenase, alanine and aspartate aminotransferase, and γ-glutamyl transferase; and (6) renal effects such as renal failure characterised by proteinuria, haematuria and anuria, renal necrosis, necrosis and swelling of renal tubules, oliguria, destruction of the tubular epithelium of the kidneys, and highly elevated serum creatinine and blood urea nitrogen; and (7) metabolic acidosis.8 Two studies in particular have shown the effects of chronic oral exposure to Cr(VI). Both studies are exceptionally relevant to our study and consisted of populations who had Cr(VI)-contaminated drinking water. The first study, from an area near a ferrochromium production plant in the Liaoning Province in China, found an association between contaminated water and gastrointestinal effects such as oral ulcers, diarrhoea, abdominal pain, indigestion and an increased incidence of lung and stomach cancer.8 19 The second study, from an area of Greece with elevated Cr(VI) in the public drinking water, found significantly higher standardised mortality ratios for primary liver, lung, kidney and genitourinary cancer.8 20
Several studies show that the serum concentrations of V and Cr are higher in adult haemodialysis patients and patients with CKD; this suggests that they accumulate in the body.5 21–23 Another study confirmed this association by measuring trace elements in the hair of adult haemodialysis patients.6 Although data in paediatric patients with CKD are elusive, we hypothesised that similar to dialysis patients, we would find elevated V and Cr levels in paediatric patients with CKD who were not receiving dialysis treatments.24 We also hypothesised that levels would increase with worsening glomerular filtration rate (GFR).
Patients and methods
Study design
The study adhered to the Declaration of Helsinki. The Research Ethics Board of the University of Western Ontario approved the study as part of an intervention study on zinc supplementation in patients with CKD centred at McMaster University (NCT02126293; HC#172241; REB #104976). Patients were recruited from April 2014 to April 2016. Given that almost all patients enrolled within the first 3 months had elevated V and Cr levels, we created this ancillary cross-sectional study to specifically analyse the elevated trace elements in this population. The primary outcome of the original study was patient plasma zinc levels, while the secondary outcomes were the patient plasma trace element levels.
Study population
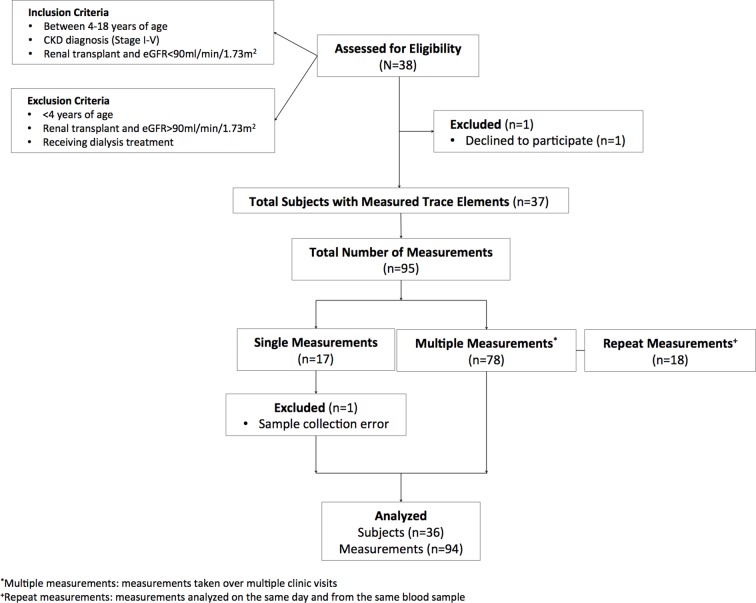
Figure 1 shows the inclusion and exclusion criteria. We performed an interim analysis on 36 study patients (16 women, 44%; average age: 11.85±4.5 years, age range: 4.42–18.98 years) with various renal pathologies and diagnosed CKD (as per the Kidney Disease - Improving Global Outcomes (KDIGO) guidelines25) using the modified Schwartz formula26 at the London Health Sciences Centre, a tertiary paediatric nephrology centre. Patients with Stage 1 (estimated glomerular filtration rate (eGFR) >90 mL/min/1.73 m2) to Stage 5 (<15 mL/min/1.73 m2) CKD were included in the study. Patients receiving dialysis treatments were excluded from the study because the dialysis water could further affect the patients’ V and Cr levels. Since this was an ancillary study, the study did not specifically select for the stage of CKD, the patient’s age or the location of the patient’s residence, which could introduce potential bias. Patients also had different numbers of repeated samples, depending on their clinic visits. Patients did not record their fluid or food intake, which could influence the results. To address potential bias due to contaminated drinking water, we matched the postal code of the patient’s home with provincial 2014 water quality data.
Figure 1.
Patient flow chart. Of the 38 subjects assessed for eligibility in the study, we included 36 in our analysis. These 36 patients had 94 trace element panel measurements. CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate.
Experimental methods
eGFR was calculated using the Filler formula,27 using the new international reference materials.28 Plasma samples were collected in BD K2-EDTA Royal Blue Vacutainer tubes (Reference #368381). V and Cr levels were measured using the high-resolution sector field inductively coupled mass spectrometry (https://ltig.lhsc.on.ca/?action=view_rec&test=Vanadium%2C_Plasma; https://ltig.lhsc.on.ca/?action=view_rec&test=Chromium%2CPlasma; last accessed 27 June 2016). The total imprecision (CV) of the V measurements was 10% at low concentration (0.100 µg/L), 4% at medium concentration (0.257 µg/L) and 8% at high concentration (0.356 µg/L). For Cr, the total imprecision (CV) was 3% (0.82 μg/L), 4% (5.40 μg/L) and 5% (43.60 μg/L), respectively. Anthropomorphic data (patient height measured by stadiometer, necessary to calculate the Schwartz eGFR), the first three digits of patients’ postal codes and creatinine and cystatin C were collected from our electronic chart programme, PowerChart (Cerner). Data were entered into an Excel spreadsheet (Excel for Mac 2011, V.14.4.4.).
Data analysis was performed using GraphPad Prism 5 for Mac OS X, V.5.0f, and HLM 7.01 (Scientific Software International, Skokie, Illinois, USA). Data were analysed for normal distribution using the D’Agostino and Pearson omnibus normality test. As most data were normally distributed, parametric methods were used for all statistical tests, with the exception of the V and Cr levels and eGFR, which were expressed as median and interquartile range (25th, 75th percentile). Spearman’s rank correlation analysis was used to analyse the correlation analysis of V levels that were not normally distributed. The Wilcoxon signed-rank test was used to compare the V and Cr levels with the 97.5th percentile as neither V nor Cr levels were normally distributed. A repeated measures analysis was conducted to determine whether the results of repeated measurements (from the same day) affected the original results.
Heat maps depicting V and Cr levels in drinking water were generated using data collected by the Government of Ontario for their Provincial (Stream) Water Quality Monitoring Network, which can be found at https://www.ontario.ca/data/provincial-stream-water-quality-monitoring-network. Only the most recent data were used (2014; https://files.ontario.ca/moe_mapping/downloads/2Water/PWQMN_by_year/pwqmn_rawdata_2014.xlsx). The station coordinate data (found at https://files.ontario.ca/moe_mapping/downloads/2Water/PWQMN1.xlsx) was used to determine the longitude and latitude of each testing station in order to generate the map. Since each station had a varying number of results, only the most recent measurement was used, unless that measurement was a negative number, in which case the second most recent measurement was used. Measurements used in the maps were taken between spring and winter of 2014. The V or Cr measurement at each station and the longitude and latitude of each station were then uploaded in two separate files to open-source mapping software created by Pete Warden, which can be found at www.openheatmap.com. Patients’ locations in Southern Ontario were mapped using the first three digits of their postal codes (data on file).
Results
Thirty-six children and adolescents with CKD and at least one set of trace element data were included in the study (figure 1, table 1). The median eGFR was 51 mL/min/1.73 m2 (35, 75). V levels were not normally distributed (D’Agostino and Pearson omnibus test p value<0.0001). The median V level was 0.12 µg/L (0.09, 0.18) and the maximum V level was 3.350 µg/L. Thirty-two patients had at least one set of V levels above the published reference interval of 0.088 µg/L (table 2) in either unit, and the results of 75 of the 94 total tests (80%) were above the interval. The V levels were significantly greater than the 97.5th percentile of the reference interval of 0.088 µg/L (Wilcoxon signed-rank test p<0.0001). There was a weak negative correlation between the V levels and the eGFR (Spearman r=−0.1209, figure 2). In patients with repeated V levels, there was no statistically significant change between the first and the last measured level (figure 3).
Table 1.
Patient demographics
| Variable | n (%) |
| Gender | |
| Male | 22 (58%) |
| Female | 16 (42%) |
| Age group (years) | |
| 4–10 | 18 (47%) |
| 11–15 | 9 (24%) |
| 16–18 | 11 (29%) |
| Primary diagnosis | |
| Hereditary | |
| Renal dysplasia | 11 (31%) |
| Metabolic disorders | 5 (14%) |
| Nephronophthisis | 2 (6%) |
| Autosomal recessive polycystic kidney disease | 2 (6%) |
| Autosomal dominant polycystic kidney disease | 1 (3%) |
| Congenital nephrotic syndrome | 1 (3%) |
| Alport syndrome | 1 (3%) |
| Acquired | |
| Reflux nephropathy | 4 (11%) |
| Haemolytic uremic syndrome | 3 (8%) |
| Glomerulonephritis/focal segmental glomerulosclerosis | 3 (8%) |
| Tubulopathy | 2 (6%) |
| Ischaemic renal Injury | 1 (3%) |
| Kidney transplant | |
| Yes | 13 (36%) |
| No | 23 (64%) |
Table 2.
Paediatric reference intervals used in our study
| Paediatric reference intervals | ||||
| μg/L | μmol/L | |||
| Lower | Upper | Lower | Upper | |
| Vanadium | 0.032 | 0.088 | 0.6 | 1.7 |
| Chromium | 0.13 | 0.31 | 2.5 | 6 |
Paediatric-specific vanadium and chromium reference intervals were not available.
Figure 2.
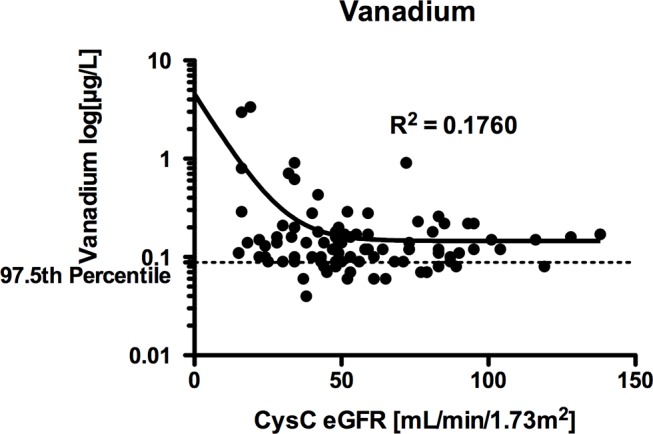
Scatter plot of vanadium levels versus estimated glomerular filtration rate (eGFR). Vanadium levels (μg/L) were not normally distributed. The non-linear regression line (one-phase exponential decay) has been included. Glomerular filtration rate was measured in mL/min/1.73 m2. The formula reads: Y=(Y0−Plateau)×exp(−K×x)+Plateau, where Y0 is the value when x is 0, plateau is Y at a large value, K is the rate constant, and the values were Y0=4.555, Plateau=0.1457 and K=0.1111 (GraphPad Prism).
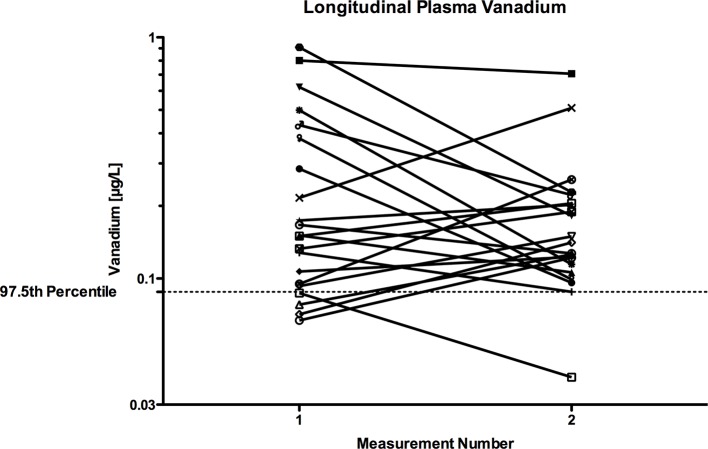
Figure 3.
Repeated measures plot of first and last vanadium level in those patients who had repeated levels. Vanadium levels (μg/L) were not normally distributed. While the median vanadium level lowered from 0.1510 to 0.1410 µg/L, and many patients demonstrated an increase of their vanadium level with repeated measures, this did not reach statistical significance (p=0.4140, Wilcoxon matched-pairs signed-rank test).
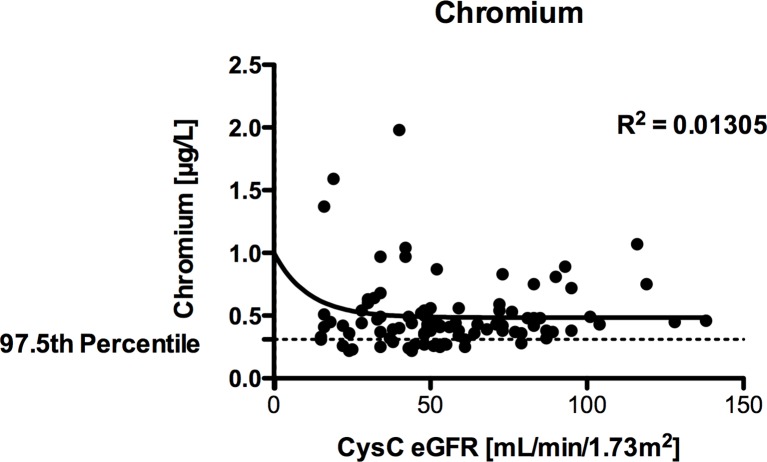
Cr levels were not normally distributed (D’Agostino and Pearson omnibus test p value<0.0001). The median Cr level was 0.43 µg/L (0.36, 0.54), which was significantly greater than the 97.5th percentile of the reference interval of 0.31 µg/L (Wilcoxon signed-rank test p<0.0001). Thirty-four patients had at least one Cr level that was above the reference interval for healthy adults (77 of 94 tests (82%)). There was a very weak non-significant positive correlation between Cr and eGFR (Spearman r=0.09111, p=0.3851, figure 4). The median level did not change from first to last measurement, and the perceived rise in the values was not statistically significant (p=0.3381, Wilcoxon matched-pairs signed-rank test, figure 5). There was a moderate but significant correlation between V and Cr levels (Spearman r=0.5973, p=<0.0001). Similar results were found with a repeated measures analysis (HLM 7.01; Scientific Software International) that accounted for all measurement points. Neither V nor Cr levels were associated with age or season.
Figure 4.
Scatter plot of chromium levels versus estimated glomerular filtration rate (eGFR). Chromium levels (μg/L) were not normally distributed. The non-linear regression line (one-phase exponential decay) has been included. Glomerular filtration rate was measured in mL/min/1.73 m2. The formula reads: Y=(Y0−Plateau)×exp(−K×x)+Plateau, where Y0 is the value when x is 0, Plateau is Y at a large value, K is the rate constant, and the values were Y0=1.641, Plateau=0.4841 and K=0.09060 (GraphPad Prism).
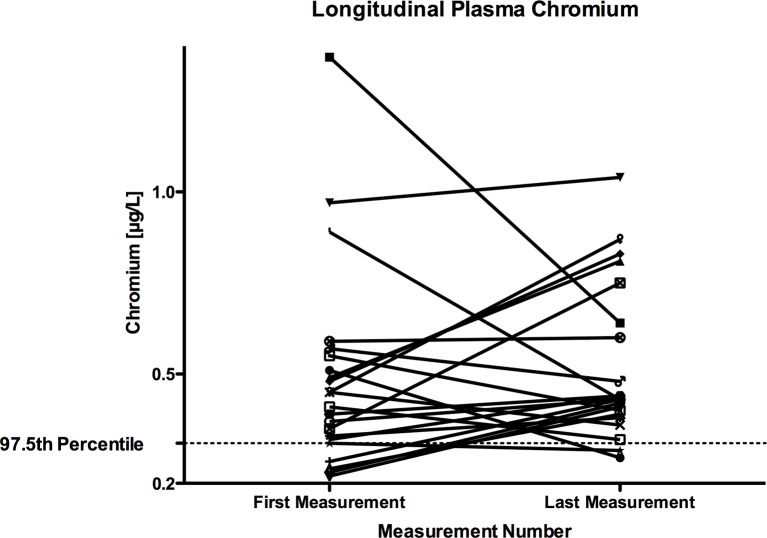
Figure 5.
Repeated measures plot of first and last chromium level in those patients who had repeated levels. Chromium levels (μg/L) were not normally distributed. The median chromium level did not change from 0.44 µg/L and the rise in the values was not statistically significant (p=0.3381, Wilcoxon matched-pairs signed-rank test).
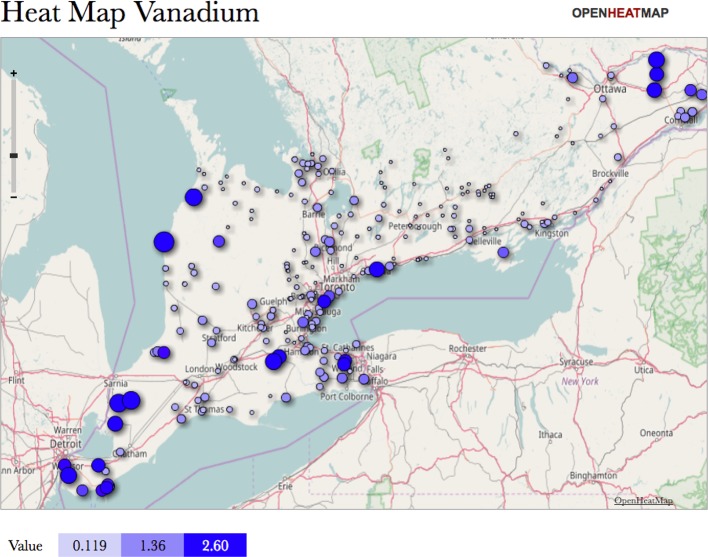
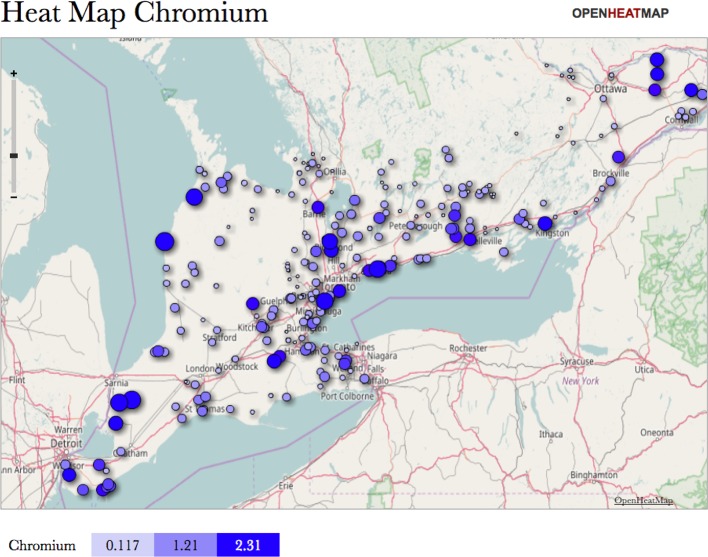
The V levels measured in water ranged from 0.00257 µg/L to 5.87 µg/L, and the measured Cr levels in water ranged from 0.0099 µg/L to 4.32 µg/L. The mapped V data show higher concentrations grouped along the Detroit and St Clair river, as well as the shores around Lake Erie and Lake Huron (figure 6). The mapped Cr levels show the same general distribution pattern but with slightly larger values overall (figure 7).
Figure 6.
Heat map showing the concentration of vanadium in 2014 in various streams around Southwestern Ontario. Map created using 2014 data from the Provincial (Stream) Water Quality Monitoring Network at https://www.ontario.ca/data/provincial-stream-water-quality-monitoring-network in open-source software found at www.openheatmap.com.
Figure 7.
Heat map showing the concentration of chromium in 2014 in various streams around Southwestern Ontario. Map created using 2014 data from the Provincial (Stream) Water Quality Monitoring Network at https://www.ontario.ca/data/provincial-stream-water-quality-monitoring-network in open-source software found at www.openheatmap.com.
Comparing the two maps with a map of the patients’ locations from the study, we found that although some groupings of patients corresponded to the areas of high V and Cr (such as Windsor, St Thomas, Hanover and Owen Sound; n=8), others were located in areas of low concentrations.
Discussion
Our study demonstrates a high prevalence of elevated V and Cr levels in paediatric patients with CKD. With V, this trend is strongest in patients with an eGFR of less than 30 mL/min/1.73 m2. In 28 of the 36 patients, V and Cr exposure in drinking water did not seem to be the major contributing factor.
Homeostasis of both trace elements depends on uptake and elimination. Uptake occurs through different types of environmental exposures, namely through the air, water, food and soil. More than 70% of Cr in the environment comes from anthropogenic sources, such as non-ferrous base metal smelters, refineries, leather tanning industries, urban storm water run-off, effluent streams from pulp and paper mills, and discharges from thermal generating stations.29 In Canada, it is largely released into the atmosphere through different means of pollution, namely industrial processes (1/3), stationary fuel consumption (1/2) and transportation (3/20).30 Ground water and other fresh water contain V (in the form of H2VO4−) at an approximate concentration of 1.17 µg/L, fats, fruits and vegetables at 1–5 µg/kg, and meat, seafood, whole grains and dairy products at 5–30 µg/kg.31 The daily intake via food is usually between 10 and 200 µg.32 Cr(III), the less toxic isoform of Cr, is also naturally found in many foods.8 Both hexavalent and trivalent Cr are found in water.29
Although previous studies have shown elevated V and Cr levels in adult dialysis patients,22 we are unaware of any published work showing high V and Cr levels in paediatric patients with CKD other than in abstract form.33 Since patients with CKD are usually polyuric and develop polydipsia, their exposure to V in drinking water is several-fold greater than the general population. Combined with the fact that V is mainly eliminated through the kidneys,1 3 this vulnerable population’s environmental exposure to toxic trace elements may pose a danger, especially if they have polyuria and polydipsia and drink contaminated water. We suspect that in addition to our patients’ low V and Cr clearance, their significantly greater exposure to V and Cr in drinking water is the reason for their high levels of both elements. Since some groupings of patients corresponded to the areas of high V and Cr and others did not, this leads us to believe that our findings are the result of both environmental factors and impaired kidney function.
There are few guidelines for maximum V concentrations in the environment, and those that exist either cover a wide range from different sources, are outdated or were determined using extremely limited and unacceptable methodologies.34 The Office of Environmental Health Hazard Assessment in California released a statement in August of 2000 in response to the Department of Health Service’s proposed level not exceeding 50 µg/L, recommending a lower level of 15 µg/L.35 Meanwhile, Environment Canada released the Federal Environmental Quality Guidelines for V in May of 2016, listing the predicted no-effect concentration for marine water at 5 µg/L and for freshwater at 120 µg/L. The Canadian federal government does not include V in their most recent Guidelines for Canadian Drinking Water Quality (2014),36 nor is it included in the water quality guidelines used by Ontario.37 Other Canadian water quality guidelines list standards ranging from 3.9 to 250 µg/L.38 39 The standard for Cr in Ontario drinking water is 50 µg/L. The Centers for Disease Control has established some minimal risk levels for humans, defined as an estimate of daily human exposure to V and Cr that is likely to be without an appreciable risk of adverse effects over a specified duration of exposure.7 These limits are as follows: oral acute (none), intermediate duration (10 µg/kg/day for V and 0.5 µg/kg/day for Cr) and chronic duration (none for V and 0.9 µg/kg/day for Cr).
The average concentration of Cr in uncontaminated surface and marine water is generally below 1.0 µg/L,30 but in Ontario these numbers can be much greater at sites most severely affected by pollution. This includes the St Marys River system with concentrations of 31 000 µg/g dry weight (dw) in Tannery Bay and concentrations exceeding 5120 µg/g (dw) in the Welland River downstream from a steel manufacturing plant compared with 10 µg/g (dw) upstream.30 Up to 1920 µg/g (dw) has been found in Detroit River sediments and 564 µg/g (dw) in Hamilton Harbour sediments.6 Elevated concentrations of twofold to fourfold above local background levels have also been reported in sediments from Lake Simcoe, the Detroit River, Lake Ontario off the Niagara River and the St Lawrence River.32 Our catchment area overlaps with several of these areas.
Twenty-eight of our patients were not from the highly polluted areas. However, some of the highest V and Cr levels were observed in patients with a low GFR, despite living in areas with low V and Cr exposure. We believe that the high water intake with CKD and the low GFR are two additional factors that result in the high prevalence of elevated V and Cr in these patients.
Clearly, the scientific evidence indicating both the safe levels and the resultant toxicity of V in our air, water and food is lacking, of poor quality and conflicting, especially considering how little, if any, of this research has been done on (1) vulnerable populations such as children and (2) children with impaired renal or hepatic function. The guidelines for Cr are slightly clearer considering its increased toxicity, but there are still little data on chronic safe levels and toxicity. Since high V and Cr levels are seen in such a large proportion of our study population, and since the environmental levels of V and Cr and the resultant health implications are mostly unknown, the question becomes: how can we limit the exposure of children with poor renal function to these potentially toxic trace elements?
Several studies have shown the potential of chelating agents such as iron in reducing V body burden and toxicity.7 The safety and efficacy of this strategy have not been established in children. Therefore, preventing high exposure may be the only feasible strategy, but using bottled water with low trace element levels may be very costly.
A strength of our study is its cross-sectional design in combination with longitudinal data and a reasonable number of patients for a paediatric pilot study. Another strength is the high precision of the instruments used to measure the trace elements. There are still several limitations. More subjects would have lead to more precise data, and our patient cohort has a bias towards milder CKD stages, which could have potentially minimised the trace element levels seen in this population. Additionally, although the reference intervals that we used were specific to our catchment area and to the equipment used to measure plasma trace elements at our site, they are based on a cohort of adults and have not been published. We did not assess whether the patients drink municipal water, well water or bottled water (with presumably lower concentrations), nor did we assess their total fluid intake. We also did not control for food intake. Certain foods such as fish, shellfish40 and grains and cereals41 may contain dangerous V concentrations. These potential confounders could have minimised the environmental impact of the high levels in this population. Finally, detailed studies on the age dependency of paediatric V and Cr concentrations are elusive. Additionally, the tubulotoxicity of Cr, in particular, may influence the progression of CKD. Although we did not examine the tubulotoxicity found in our patient cohort, there is often mixed tubular and glomerular proteinuria in patients with CKD and proximal tubular dysfunction in CKD.42 Some recent research in animal models has suggested that selenium supplementation could reverse some of the tubular damage.43 Of course, haematopoiesis is impaired in the advanced stages of CKD and nephrotoxicity should be avoided.
Despite these limitations, our data robustly demonstrate a high prevalence of elevated V and Cr levels in children with CKD. There was a trend towards higher V levels with worsening kidney function. Our data would favour monitoring V and Cr in paediatric patients with CKD, especially in areas with high exposures or in very polyuric patients.
Supplementary Material
Acknowledgments
The authors would like to thank Mrs Maria McCann and Mr Colin Bradley for their outstanding commitment to the highest level of performance with regard to measuring the trace elements on MS/MS at the Trace Element Laboratory at the London Health Sciences Centre. We would also like to thank Michael Miller, PhD, for helping our team by analysing all of the data using a repeated measures analysis.
Footnotes
Contributors: GF and VB articulated the conceptual framework for both the original RCT study and this ancillary study. GF developed the analytical approach, and GF and MK analysed the data. GF, MK and HKS drafted and edited the manuscript. VB, SHSH and LY contributed to the interpretation of data, added intellectual content during manuscript preparation and provided valuable feedback on various aspects of the manuscript. All authors read and approved the final manuscript.
Funding: This study was supported through funding from Hamilton Health Sciences in the form of a New Investigator Fund Award (NIF13312) awarded to Dr Vladimir Belostotsky.
Competing interests: None declared.
Ethics approval: Western University REB.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available on request.
References
- 1. Heinemann G, Fichtl B, Vogt W. Pharmacokinetics of vanadium in humans after intravenous administration of a vanadium containing albumin solution. Br J Clin Pharmacol 2003;55:241–5. 10.1046/j.1365-2125.2003.01711.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO. Chromium in Drinking-water Geneva. 2003. http://www.who.int/water_sanitation_health/dwq/chemicals/chromium.pdf (accessed 13 Jul 2016).
- 3. Mukherjee B, Patra B, Mahapatra S, et al. Vanadium--an element of atypical biological significance. Toxicol Lett 2004;150:135–43. 10.1016/j.toxlet.2004.01.009 [DOI] [PubMed] [Google Scholar]
- 4. Gruzewska K, Michno A, Pawelczyk T, et al. Essentiality and toxicity of vanadium supplements in health and pathology. J Physiol Pharmacol 2014;65:603–11. [PubMed] [Google Scholar]
- 5. Hosokawa S, Yamaguchi O, Yoshida O. Vanadium transfer during haemodialysis. Int Urol Nephrol 1991;23:407–9. 10.1007/BF02549614 [DOI] [PubMed] [Google Scholar]
- 6. Ochi A, Ishimura E, Tsujimoto Y, et al. Trace elements in the hair of hemodialysis patients. Biol Trace Elem Res 2011;143:825–34. 10.1007/s12011-010-8948-y [DOI] [PubMed] [Google Scholar]
- 7. Services USDoHaH. Toxicological Profile for Vanadium. United States: United States Government, 2012. http://www.atsdr.cdc.gov/ToxProfiles/tp58.pdf (accessed 11 Jul 2016). [Google Scholar]
- 8. Services USDoHaH. Toxicological Profile for Chromium. United States: United States Government, 2012. http://www.atsdr.cdc.gov/ToxProfiles/tp7.pdf (accessed 11 Jul 2016). [Google Scholar]
- 9. Lagerkvist B, Nordberg GF, Vouk VV. Handbook on the toxicology of metals. 2 Amsterdam: Elsevier Science Publishers, 1986. [Google Scholar]
- 10. Barceloux DG. Vanadium. J Toxicol Clin Toxicol 1999;37:265–78. 10.1081/CLT-100102425 [DOI] [PubMed] [Google Scholar]
- 11. Cite? T-ht. ToxGuide for Vanadium V. In: Services UDoHaH, ed 2012. [Google Scholar]
- 12. Rehder D. Biological and medicinal aspects of vanadium. Inorg Chem Commun 2003;6:604–17. 10.1016/S1387-7003(03)00050-9 [DOI] [Google Scholar]
- 13. WHO. Trace elements in human nutrition and health. Geneva: WHO, 1996. [Google Scholar]
- 14. Crebelli R, Leopardi P. Long-term risks of metal contaminants in drinking water: a critical appraisal of guideline values for arsenic and vanadium. Ann Ist Super Sanita 2012;48:354–61. 10.4415/ANN_12_04_03 [DOI] [PubMed] [Google Scholar]
- 15. Europe WHOROf. Chapter 6.12: Vanadium Chromium in Drinking-water, 2000. http://www.who.int/water_sanitation_health/dwq/chemicals/chromium.pdf (accessed 21 Jul 2016).
- 16. Lener JKJ, Kodl M, et al. Health effects of environmental exposure to vanadium. Vanadium in the environment Part 2: Health Effects. New York, NY: John Wiley & Sons, 1998:1–19. [Google Scholar]
- 17. Jacobs L, Buczynska A, Walgraeve C, et al. Acute changes in pulse pressure in relation to constituents of particulate air pollution in elderly persons. Environ Res 2012;117:60–7. 10.1016/j.envres.2012.05.003 [DOI] [PubMed] [Google Scholar]
- 18. Barth A, Schaffer AW, Konnaris C, et al. Neurobehavioral effects of vanadium. J Toxicol Environ Health A 2002;65:677–83. 10.1080/15287390252900377 [DOI] [PubMed] [Google Scholar]
- 19. Zhang JD, Li XL, Xl L. [Chromium pollution of soil and water in Jinzhou]. Zhonghua Yu Fang Yi Xue Za Zhi 1987;21:262–4. [PubMed] [Google Scholar]
- 20. Linos A, Petralias A, Christophi CA, et al. Oral ingestion of hexavalent chromium through drinking water and Cancer mortality in an industrial area of Greece--an ecological study. Environ Health 2011;10:50 10.1186/1476-069X-10-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bello-Reuss EN, Grady TP, Mazumdar DC. Serum vanadium levels in chronic renal disease. Ann Intern Med 1979;91:743 10.7326/0003-4819-91-5-743 [DOI] [PubMed] [Google Scholar]
- 22. Tonelli M, Wiebe N, Hemmelgarn B, et al. Trace elements in hemodialysis patients: a systematic review and meta-analysis. BMC Med 2009;7:25 10.1186/1741-7015-7-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shaban H, Ubaid-Ullah M, Berns JS. Measuring vitamin, mineral, and trace element levels in Dialysis patients. Semin Dial 2014;27:582–6. 10.1111/sdi.12260 [DOI] [PubMed] [Google Scholar]
- 24. Filler G, Felder S. Trace elements in dialysis. Pediatr Nephrol 2014;29:1329–35. 10.1007/s00467-013-2585-6 [DOI] [PubMed] [Google Scholar]
- 25. Kidney disease: improving global outcomes CKDMBDWG. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney Disease-Mineral and bone disorder (CKD-MBD). Kidney Int Suppl 2009;113:S1–130. [DOI] [PubMed] [Google Scholar]
- 26. Schwartz GJ, Muñoz A, Schneider MF, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol 2009;20:629–37. 10.1681/ASN.2008030287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Filler G, Lepage N. Should the Schwartz formula for estimation of GFR be replaced by cystatin C formula? Pediatr Nephrol 2003;18:981–5. 10.1007/s00467-003-1271-5 [DOI] [PubMed] [Google Scholar]
- 28. Grubb A, Blirup-Jensen S, Lindström V, et al. First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin Chem Lab Med 2010;48:1619–21. 10.1515/CCLM.2010.318 [DOI] [PubMed] [Google Scholar]
- 29. Agency EP. Chromium in Drinking Water, 2015. https://www.epa.gov/dwstandardsregulations/chromium-drinking-water (accessed 15 Jul 2016).
- 30. Canada H. Chromium and its compounds: government of Canada;. 2007 [updated 2007. (accessed 12 Oct 2016). [Google Scholar]
- 31. Rehder D. The future of/for vanadium. Dalton Trans 2013;42:11749–61. 10.1039/c3dt50457c [DOI] [PubMed] [Google Scholar]
- 32. Scior T, Guevara-García A, Bernard P, et al. Are vanadium compounds drugable? structures and effects of antidiabetic vanadium compounds: a critical review. Mini Rev Med Chem 2005;5:995–1008. 10.2174/138955705774575264 [DOI] [PubMed] [Google Scholar]
- 33. Sidhu H, Filler G, Belostotsky V, et al. High prevalence of elevated vanadium levels in CKD patients. Pediatric nephrology 2016;31:1907–8. [Google Scholar]
- 34. BHPBilliton. EKATI Diamond Mine - Site-Specific Water Quality Objective for Vanadium. 2012. http://www.mvlwb.ca/Boards/WLWB/Registry/2012/W2012L2-0001/W2012L2-0001 - Ekati - Report - SSWQO - Vanadium -_12.pdf (accessed 11 Jul 2016).
- 35. Assessment OoEHH. Proposed Notification Level for Vanadium. http://oehha.ca.gov/water/notification-level/proposed-notification-level-vanadium (accessed 11 Jul 2016).
- 36. Water F-P-TCoD. Guidelines for Canadian Drinking Water Quality. 2014. http://www.hc-sc.gc.ca/ewh-semt/alt_formats/pdf/pubs/water-eau/sum_guide-res_recom/sum_guide-res_recom_2014-10_eng.pdf (accessed 11 Jul 2016).
- 37. Canada GoC-EaCC. Water Quality Guidelines Used by Ontario. 2016. https://www.ec.gc.ca/indicateurs-indicators/default.asp?lang=en&n=93177156-1 (accessed 11 Jul 2016).
- 38. Environment OMot. Soil, Ground Water and Sediment Standards for Use under Part XV. 1 of the Environmental Protection Act Canada, 2011. https://dr6j45jk9xcmk.cloudfront.net/documents/998/3-6-3-sediment-standards-en.pdf (accessed 11 Jul 2016).
- 39. TCCoMot E. Vanadium Canada1997. http://ceqg-rcqe.ccme.ca/download/en/286 (accessed 11 Jul 2016).
- 40. Copat C, Arena G, Fiore M, et al. Heavy metals concentrations in fish and shellfish from eastern mediterranean sea: consumption advisories. Food Chem Toxicol 2013;53:33–7. 10.1016/j.fct.2012.11.038 [DOI] [PubMed] [Google Scholar]
- 41. Imtiaz M, Rizwan MS, Xiong S, et al. Vanadium, recent advancements and research prospects: a review. Environ Int 2015;80:79–88. 10.1016/j.envint.2015.03.018 [DOI] [PubMed] [Google Scholar]
- 42. Waikar SS, Sabbisetti V, Ärnlöv J, et al. Relationship of proximal tubular injury to chronic kidney disease as assessed by urinary kidney injury molecule-1 in five cohort studies. Nephrol Dial Transplant 2016;31:1460–70. 10.1093/ndt/gfw203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Soudani N, Sefi M, Ben Amara I, et al. Protective effects of Selenium (Se) on Chromium (VI) induced nephrotoxicity in adult rats. Ecotoxicol Environ Saf 2010;73:671–8. 10.1016/j.ecoenv.2009.10.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.