Short abstract
Introduction
For telemonitoring to support care coordination, a sound business model is conditional. The aim of this study is to explore the systemic and economic differences in care coordination via business-to-business and business-to-consumer models for telemonitoring patients with chronic diseases.
Methods
We performed a literature search in order to design the business-to-business and business-to-consumer telemonitoring models, and to assess the design elements and themes by applying the activity system theory, and describe the transaction costs in each model. The design elements are content, structure, and governance, while the design themes are novelty, lock-in, complementarities, and efficiency. In the transaction cost analysis, we looked into all the elements of a transaction in both models.
Results
Care coordination in the business-to-business model is designed to be organized between the places of activity, rather than the participants in the activity. The design of the business-to-business model creates a firm lock-in but for a limited time. In the business-to-consumer model, the interdependencies are to be found between the persons in the care process and not between the places of care. The differences between the models were found in both the design elements and the design themes.
Discussion
Care coordination in the business-to-business and business-to-consumer models for telemonitoring chronic diseases differs in principle in terms of design elements and design themes. Based on the theoretical models, the transaction costs could potentially be lower in the business-to-consumer model than in the business-to-business, which could be a promoting economic principle for the implementation of telemonitoring.
Keywords: Case management, chronic disease, costs, telemedicine, commerce
Introduction
Telemedicine and telemonitoring systems have profoundly changed the way in which care is provided to patients with chronic diseases. The value that different telemedicine and telemonitoring systems can deliver is closely related to a business model, which structures the provision of the care service mediated by the technological architectures. Given that chronic diseases are the main cause of disability and loss of quality of life in the 21st century—where ischemic heart disease, cerebrovascular disease, lower respiratory infections, lower back and neck pain, and chronic obstructive pulmonary disease are responsible for the biggest burden of disease globally1—it is important to properly assess how different telemedicine and telemonitoring business models impact upon healthcare provision where chronic diseases are concerned. This is even more relevant since chronic diseases are no longer seen as diseases of affluence or diseases of the elderly. They are becoming more prevalent in developing countries and among the working population2 and will be the major reason for the loss of public good in this century.3
So far health technology assessment efforts have focused on cost-effectiveness of telemedicine, overlooking the business model and stakeholder dynamic in chronic disease management. The cost analyses have not gone further than identification of utilization from the payer or societal perspective, completely ignoring the transaction costs in an implementation model. Care coordination via telemedicine is intimately tied to a business model which promotes or hinders wider implementation via interdependencies of the activity system. There is, therefore, a global need for an effective and efficient way to organize activities around the management of people who are at risk or have been diagnosed with a chronic disease.
Chronic disease management and care coordination
The current care provision is inadequate to address the challenges of an aging population.4 Chronic disease management has proposed new concepts of care coordination and integration as strategies for dealing in a more efficient and cost-effective manner with the complexity of chronic diseases and multimorbidity.5 Chronic disease management provides managerial solutions to organize and coordinate the different components involved in the care of chronic disease patients pursuing a patient-centric approach.5 To achieve these goals, and to ensure continuity of care and coordination between different healthcare services providers, an integrated care approach is needed.6 Given the diversity and complexity of the activities involved in chronic disease care provision, many different care coordination solutions have been proposed.
Schultz and McDonald7 identified 57 different definitions of care coordination, distilling them into coordination efforts aiming at organizing patient care activities between two or more participants (including the patient) in order to support and enhance the delivery of the appropriate healthcare services; and into the coordination of information exchanges among healthcare personnel, and all the other resources required to deliver the expected care services. The coordination logics underpinning the two major clusters identified by Schultz and McDonald in the analysis of key concepts of care coordination clearly differ. However, they do overlap and have unclear boundaries, and are used interchangeably8 when the design and management of new coordination mechanisms is undertaken. This is also evident in the design of telemedicine and telemonitoring systems aiming at supporting chronic care provision.
Telemonitoring, business models, and costs
Telemedicine and telemonitoring are often referred to as “solutions” for delivering high-value care to a patient with a particular condition, in a particular location. Sood et al.9 analyzed 104 peer-reviewed definitions of telemedicine, distilling them into an e-health branch of services for delivery of healthcare and education from one geographical location to another. The World Health Organization10 provides a more comprehensive definition of telemedicine as
the delivery of healthcare service, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interest of advancing the health of individuals and their communities.
Home telemonitoring, a part of telemedicine, in turn is defined as an automated transmission of patient’s health status data from a home to the respective healthcare setting.11
Telemedicine and telemonitoring can therefore offer great support for the provision of effective healthcare services, minimizing the costs of the services in many different configuration of healthcare and optimizing the use of the resources needed to provide these services. The successful implementation of telemedicine and telemonitoring is challenging since it is not easy to overcome the misfit between the patient’s needs and the care model in place, which hampers the effective deployment of these healthcare solutions in the first place. Moreover, the different value chain configurations of the business models used to support telemedicine and telemonitoring solutions affect the value generated by the chosen solution.12
A widely used definition of a business model by Chesbrough and Rosenbloom13 is “a blueprint for how a network of organizations cooperates in creating and capturing value from technological innovation.” Zott and Amit14 argued that the business model also introduces the company’s bargaining power, i.e. the ability to negotiate the price and the value it can derive from its activity.
Telemonitoring is predominantly introduced via the business-to-business (B2B) model.15 B2B is a strategy where one business makes a commercial transaction with another, e.g. a telemonitoring equipment manufacturer with a hospital. In many instances, B2B telemonitoring has not gone further than the pilot testing,16 possibly due to reimbursement strategies, implementation issues, and/or economic principles. In the B2B model, the technical and legislative costs prevent the implementation of a full-scale long-term project due to high transaction costs.17 Transaction costs are costs incurred in the selling and buying process. They are divided into search and information costs, bargaining and decision costs, and policing and enforcement costs.18 Different business models differ in terms of the transaction costs generated for the agents of exchange, and implementation is only possible when investment does not exceed the costs incurred. Hence, new business models for implementation of telemedicine and telemonitoring in the management of chronic diseases should be considered.
The alternative to the B2B model is the business-to-consumer (B2C) model. B2C is a strategy where a business makes a commercial transaction with the end customer, e.g. a telemonitoring center with a patient. The activities performed in the B2C model for telemonitoring patients with chronic diseases are different, as are the stakeholders, the structure, and the governance. The new model allows care to be administered to patients whenever and wherever they need it. It remains to be seen to what extent the B2C model has an effect on the transaction costs. A business model which leverages the supply chain of healthcare services but lowers the transaction costs in the exchange in the healthcare market has yet to be found.17
Theoretical framework
An activity system describes the set of activities that a company performs in order to capture value and is characterized by interdependencies between its suppliers and customers.14 An activity of a company can be explained as “the engagement of human, physical and/or capital resources of any party to a business model (the focal firm, end customers, vendors, etc.) to serve a specific purpose toward the fulfillment of the overall objective.”14
We employ the activity theory19 to assess the design elements and the design themes in telemonitoring patients with chronic diseases via “the NICE model.”14 The NICE model suggests that the value generated by an activity system is characterized by different design themes that consist of alternative configuration of systems’ design elements. The design elements of an activity system consist of content, structure, and governance. The design themes are novelty, lock-in, complementarities, and efficiency. These two sets of design parameters capture the purposeful, firm-centric design of the activity systems.14 The framework provides an insight by (a) giving business model design a language, concepts, and tools; (b) highlighting business model design as a key managerial/entrepreneurial task; and (c) emphasizing system-level design over partial optimization.14
The central concept of the activity system theory is interdependencies, which provide insights into processes that enable a company’s activities to evolve, even if the market in which the company is competing changes.20 The interdependencies across activities are chosen by managers in order to better position and integrate a company in the environment in which it operates. The architecture of the activity system defines the possible interactions between the suppliers, the company, and the customers and is the source of the competitive advantage in the ecosystem in which it operates. The activity system cannot easily be changed without repercussions on the interdependencies created. Such an architecture, i.e. a network, is in fact a business model.21
Complementary to the activity system theory is the transaction costs theory.22 Transaction costs theory looks into the efficiency dimension of an exchange process. The theory claims that different factors (uncertainty, bounded rationality, opportunistic behavior, and small numbers) impact upon the way in which organizations coordinate exchanges and indeed activities. These costs unfold in three different phases of an exchange: search, negotiation, and enforcement.23 The phases of the transaction unfold as activities in the activity theory.
The analysis of the impact of transaction costs on the activities underpinning telemonitoring in the B2B setting, currently predominant in telemonitoring implementation, and in the B2C, was chosen to compare the effectiveness of the two different business models.
There are several cycles of activities that add up to the transaction costs total24:
Search costs—incurred when agents spend time looking for opportunities for an exchange (in the healthcare domain the exchange of a healthcare service/product for money);
Negotiation costs—the costs associated with negotiating the terms of this exchange;
Enforcement costs—the costs associated with enforcing the agreement to exchange.
Transaction costs are seen as the costs incurred by running imperfect systems.25 The elementary unit of analysis in this theory is the exchange between at least two individuals.24 If all participants in an economic exchange were to have the same information, the transaction costs would be nonexistent. Healthcare is full of these kinds of imperfections because the knowledge is protected by the people who have it, either by means of a license to practice or a license to establish a practice.
Activity theory is potentially useful in portraying the interdependences in different telemonitoring systems. The transaction costs analysis of those interdependences might allow identification of the most efficient and effective telemonitoring configurations, and help mangers and engineers to design more efficient and effective chronic care solutions.
Study aim
The aim of this study is, first, to create the B2B and B2C care models and, second, to explore the differences in care coordination and transaction costs between these models for telemonitoring patients with chronic diseases. Our hypothesis is that, due to the different activity systems, the transaction costs in the B2C model for telemonitoring chronic diseases are lower than in the B2B model. The transaction costs are taken as a proxy for model efficiency.
Methods
We performed a literature synthesis in order to inform the B2B and B2C telemonitoring case creation, to assess the design elements and themes by applying the activity system theory, and to estimate the transactions costs in each case.
Literature search and analysis
The literature synthesis was performed via Google Scholar, where papers in English from 2000 onward were retrieved. We searched for the following terms (in various combinations): B2B, B2C, case, model, design, telemonitoring, telemedicine, telehealth. We opted for a convenience sample26 without exclusion criterion. We looked for case studies and conference papers with design elements of telemonitoring systems, in order to design our own. The input was interpreted in the B2B and B2C model for telemonitoring. As such, the literature analysis can be described as a directed content analysis approach.27 The literature was searched for and gathered by the first author, while all authors were involved in the analysis.
Cases creation
We created two telemonitoring cases for two business models—B2B and B2C—involving all the actors identified by the literature search. We also incorporated the design elements found in the literature—monitoring, modules, mediators, and actors–devices relationships. Then we applied the research design approach proposed by Griffioen.28 Griffioen used the activity system theory in the sustainable business model design for heart failure home telemonitoring opportunities in Western Europe and created a transaction mapping tool to communicate roles and transaction relations. We created a similar map, with a set of actors and a relational context looking at modules and relationships in B2B and B2C model of telemonitoring. Individuals (actors) are represented by a circle (patient, informal caregiver, care coordinator, social worker, registered nurse, physician, pharmacist, and telenurse) while institutions (stages) are represented by squares (home, hospital, pharmacy, and telemonitoring center). The relations are described in terms of voice, data, money, and drug exchange. The activity system mapping was followed by the transaction costs exploration for both models, B2B and B2C, and the discussion on the impact of the business model on the implementation possibilities of the two alternative applications.
Results
Literature review inputs
In total 22 papers were retrieved by the literature search. Seven papers were included in the analysis (three conference papers, two case studies, and two journal articles) while others were omitted as they did not contain useful design elements. The diagrams from the publications that were included were used to create the B2B and B2C telemonitoring cases.
The main finding from this limited number of sources was that companies are developing new markets through the B2C models,29 while in the B2B models they are trying to replicate and support the existing organizational structure.30 From the eICU case,31 we replicated the remote monitoring part, both in the B2B and B2C setting, while from the mobile multimedia medical system design and implementation case32 we considered four modules necessary for system to operate: information desk, patient’s portal, video outpatient service, and electronic medical information module. From the document-based service platform for telemedicine,33 we replicated the “mediator” which in our version of the B2C case is a Telemonitoring Center. From the telemedicine market case34 we considered the actors–devices relationship, and from the COPD24 case35 architectures of the business cases, i.e. the B2B and B2C case. The literature inputs to the B2B and B2C telemonitoring cases are presented in Table 1.
Table 1.
Literature inputs to the telemonitoring cases.
| Author(s) | Year | Type of study design | Study objective | Main findings |
|---|---|---|---|---|
| Herzlinger et al.31 | 2014 | Case Study | “Would the advent of global payment models and ACOs create sufficient demand for a telemedicine offering covering the care continuum, from hospitals to the home? This was the decision facing Royal Philips Electronics (Philips), the Netherlands-based producer of lighting, consumer electronics, and health care products, in 2012.” | “In the eICU model, patients in hospital ICUs were monitored using bedside devices, which transmitted patient data to a remote station from which clinicians monitored and directed care as needed. The model aimed to improve care quality by enabling early interventions and reducing adverse events, and to cut costs by allowing clinicians to care for a larger number of patients. Building on this and other offerings in its portfolio, including numerous home care devices, Philips could extend this model to create an integrated remote monitoring offering managed through a centralized clinician-staffed station.” |
| Kung et al.32 | 2006 | Qualitative Research | “This study describes in detail the system design principles and implementation considerations for mobile telemedicine systems. The system effectiveness and limitations for practical system deployment and usage are described based on the technical and managerial analysis.” | “The M3 system can also be used in a hospital’s B2B or B2C’s customer relationship management frameworks. A hospital can trace the patient’s situation online at any time, and provide information on healthcare to the patient (B2C) as well as share information and experience with other hospitals (B2B). This approach can improve the quality of the medical treatment given by a hospital and its medical professionals, and thus increase the loyalty of a patient to the hospital.” |
| Lähteenmäki et al.33 | 2008 | Conference Paper | “In this paper, we present a generic service platform, which is applicable in a wide range of telemedicine applications and in other areas involving the need for confidential information exchange.” | “The pilot hosted by the Tampere Heart Centre showed that a cardiac consultation service is useful even without full integration with the EPR. Both the Heart Centre cardiologists and the physicians of the remote units considered the benefits of the consultation service to be high. In the consultation cases, cardiology diagnostics and medication could be refined and guidance for patient logistics was provided. The physicians considered it feasible to use a commercial consultation service when available. |
| Pels et al.34 | 2011 | Case Study | “BioScience (BS) is an Argentine company, which develops and commercializes innovative diagnosis equipment since 1995. The BM is a device which sends vital signals (from a patient with a chronic disease) through the mobile phone to a recipient’s cell phone (doctor and/or relative).Three market segments, the alternative value propositions and the suggested go-to-markets for each of them are suggested.” | “BS realized that contrary to the neurological market, where it was crucial to be in a clinical network, in the telemedicine market, it was fundamental to be associated with telecommunication companies. BS needed the telcos as they had the infrastructure necessary to offer the service. Alternatively, telcos saw telemedicine as an additional high-value application they could offer. BS had already signed an alliance with Telefonica Argentina. The agreement followed the industry practice (such as ringtones) in which the 30 per cent of the profit would go to BS, and the 70 per cent remaining to Telefonica Argentina.” |
| Shevchenko30 | 2004 | Qualitative Research | “The goal of this paper is to outline important trend(s) in the advancement of this rapidly growing area of economy, i.e. the transformation of e-market, and to provide recommendations regarding feasible structure of emerging integrated industrial production/distribution chains, which could be useful for businesses. | “Like e-market place, i.e. B2C eHub, which has its conventional analogue in supermarket, the B2B eHub can be considered as web-based extension of a conventional enterprise, namely as a sort of ‘virtual’ implementation of a large corporation with specialized departments spread over the territory, e.g. city, region or country.” |
| Wac and Hausheer35 | 2011 | Conference Paper | “The goal of our COPD24 scenario is to demonstrate and validate the precise conditions to be fulfilled from a healthcare perspective, as well as derive requirements for Future Internet (PI) technologies for subsequent deployment of self-management and tele-monitoring/treatment services for COPD patients.” | “Two main alternatives can be distinguished in terms of potential business cases for the COPD24 service. The COPD patient can either have a Business-to-Consumer (B2C) relationship directly with the COPD24 application provider, or with the mobile network operator. In the former case, the COPD24 application provider takes care of establishing SLAs with all involved mobile network operators, denoted as Business-to-Business (B2B) relationships. Optionally, a user may have an additional business relationship with its (home) mobile network operator. In the latter case, the mobile network operator is the only entity in B2C relation with the patient, while the mobile network operator's B2B relationship with COPD24 application provider is transparent to the patient.” |
| Wen and Tan29 | 2003 | Conference Paper | “More specifically, hospitals and health provider organizations tend to use static websites that supply information, but have not made major investments in interactive technologies to engage patients and healthcare consumers more actively. In this paper, we survey a number of key participants in the e-health marketplace and the technologies that these players have employed to date.” | “Pharmaceutical companies are developing new markets through B2C e-commerce sites. Vendors such as Merck are also able to reduce their marketing costs by reaching more consumers (both patients and physicians) for less cost with e-health offerings. The third approach is remote medical management via the telephone or electronic communication. Chronic disease is particularly suitable for remote management, especially when there is continuity between the patient and service provider.” |
Telemonitoring cases
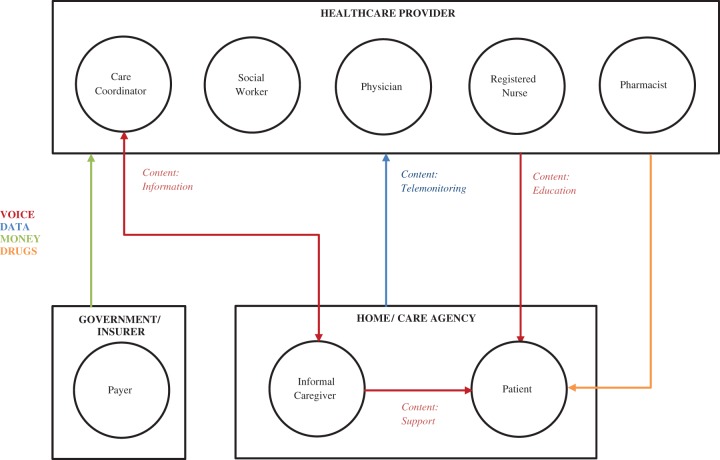
In the B2B model (Figure 1) ICT is used for communication between the patient and the telehealth team, which consists of a care coordinator, a physician, a social worker, a pharmacist, and a registered nurse—all based in a hospital. This model of healthcare delivery is also referred to as “hospital-to-home” telemedicine.31 During the multidisciplinary rounds, each patient is assessed according to their physiological signals, which are transmitted by the telemonitoring devices, and according to their personal goals/motivation. Via interactive dashboards, the team can easily spot a patient whose condition is deteriorating and who therefore needs more help. They help discharged patients by caring for them in an outpatient setting via technology. In the B2B operation this is usually via some sort of eHub—“a virtual implementation by a large corporation with specialized departments spread over the territory, e.g. city, region or country.”30
Figure 1.
Individual and institutional communication in the B2B model for telemonitoring patients with chronic diseases.
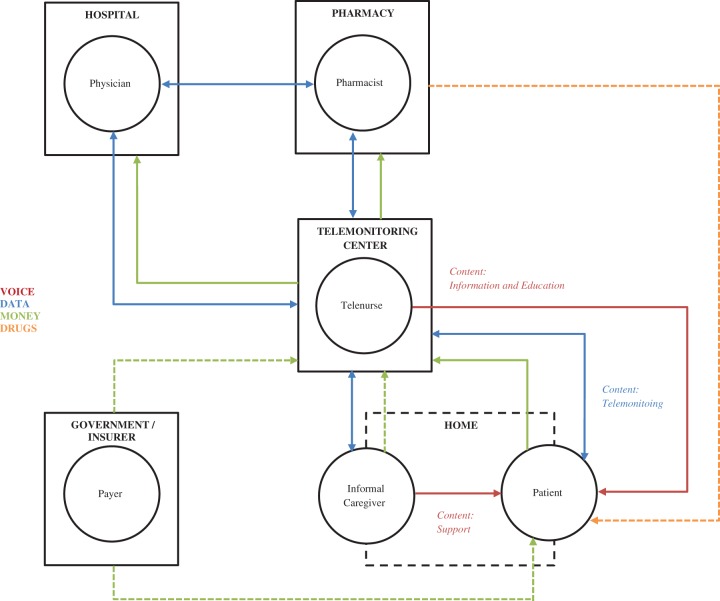
In the B2C model (Figure 2) the communication takes place between a telemonitoring nurse, based on a telemonitoring center (in our design), and the rest of the stakeholders (including the patient) in their respective organizations.29 The telemonitoring nurse monitors the physiological data daily, aided by smart algorithms. This nurse places a call to the patient every fortnight in order to assess their therapy adherence, emotional state and—if the patient is chronically ill—their wellbeing. Telenurses act as healthcare navigators, helping patients with the complexities of both the healthcare system and the disease and, as personal health coaches, they provide a helping hand to patients and informal caregivers. In this respect, the B2C model is a mixture of a high-touch and high-tech approach in chronic disease management. The dashed lines in Figure 2 represent possible scenarios that go beyond the one we created for the purpose of this assessment: (1) a reimbursement by government/insurer to a patient directly, (2) a payment by government/insurer to telemonitoring center for a cohort of patients, and (3) a payment by informal caregiver to telemonitoring center. In the literature, we also found scenarios where drugs are sent from a pharmacy to a patient via post.
Figure 2.
Individual and institutional communication in the B2C model for telemonitoring patients with chronic diseases.
In the cases, we designed monitoring (in both the B2B and the B2C model) to take place via a smartphone connected to an array of devices, depending on the severity of the disease (blood pressure meter, weighing scale, medication dispenser, etc.). The patient either has a direct relationship with the telehealth provider or with a hospital/service network/care organization.35 The telemonitoring team uses the care coordination tool (i.e. a series of interactive dashboards that unify the signals and readings from different patients) connected to a document-based service platform (i.e. electronic patient record) to follow the progress of the disease.33 A telemonitoring platform allows the team to analyze the root cause of the events (e.g. hospitalization) in order to prevent or avoid them, and to amend therapy. The outcomes are constantly measured and reassessed for both the patients and the program. The gathering of the data is unobtrusive and continuous, i.e. runs in the background of the care coordination processes. All the participants in the care process have access to the monitoring data and the disease progression charts. Patients can follow an exercise program with remote monitoring and coaching via a mobile multimedia medical system.32
Customization of the telemonitoring service, via smart algorithms using educational content, surveys, information provision, games, etc., is a crucial part of the value creation in the B2C approach. The value proposition in this case is delivered via telecom operators. Value in the B2C model is captured by cost and risk reduction, and increase in convenience and usability. It has a similar proposition to B2B, where customers essentially buy “peace of mind,” but with more convenience as the service runs on a personal device and is considered “device-agnostic.”
Care coordination in B2B and B2C telemonitoring
The care coordination in the B2B case (Figure 1) is organized between the places of activity, rather than between the participants in the activity. The activity performed via voice communication is intermittent patient support, while the data gathering and analysis runs continuously in the background. The telehealth team meets in a physical location (i.e. hospital) and communicates with other physical locations (i.e. home) where the other two participants are present—the patient and the informal caregiver. The care coordinators are needed in both physical locations—the care coordinator in the hospital and the informal caregiver in the home. This adds a layer of complexity to the care process and subsequently increases costs. The principal interdependencies in this activity system are location based—all participants in the care process, except the patient, are “exchangeable,” while the locations are “fixed.”
The care coordination in the B2C case (Figure 2) is organized between the players in the activity system and rarely between the places. The patient in this system is able to receive care on the move and at home. In the B2C business model, a telemonitoring nurse is a central character and, just like a personal health coach, manages the players and the resources in the care continuum. This reduces costs as there is no need to coordinate staff at both locations. The interdependencies lie between the persons in the care process (the telenurse, the informal caregiver, and the patients) and not between the places of care. The institutional interdependencies are digitized and automated—via data transfer, digital prescriptions, and access to interactive dashboards—which enables all players to have timely and accurate information at hand.
Activity system and transaction costs in B2B and B2C telemonitoring
The design elements and the design themes differ in the B2B and the B2C activity system for telemonitoring patients with chronic diseases. The content is the same in both cases, but the structure (i.e. hospital versus telemonitoring center) and the governance differ. In the B2B case the hospital providing the service is also responsible for the governance and operation of the service (together with the equipment manufacturer), while in the B2C case the official governing body of the jurisdiction should be in charge (or, in the absence of a competent body, an international healthcare organization). This is necessary due to the legal, ethical, and socioeconomic factors associated with telecare.36 Thus, the novelty of the B2C case lies in the structure and governance. Also, the customer (i.e. patient) in the B2C case is not locked-in and can opt out from the service at any time. This helps with the continuity of the service. And, finally, the complementarities in the two cases differ. In the B2B case community services (via the social worker and care coordinator) generate value for the patient, while clinical trials generate value for the hospitals and the equipment manufacturer. In the B2C model there are different complementarities, e.g. monitoring comorbidities benefiting the patient, population monitoring benefiting the government, and big data gathering benefiting the equipment manufacturer. The design elements and themes of both the B2B and the B2C activity system frameworks are presented in Table 2, where the transaction costs are explored in the efficiency domain.
Table 2.
Assessment of the B2B and B2C models for telemonitoring chronic diseases in the activity system design framework.
| Design | B2B | B2C | |
|---|---|---|---|
| Elements | |||
| Content | What activities should be performed? | Telemonitoring, education, and patient support. | Telemonitoring, education, and patient support. |
| Structure | How should they be linked and sequenced? | The care coordination takes place between the telehealth team in the hospital and the team at home (i.e. between a hospital and a home). The team meets in a specific location at a specific time, reviews the patient’s data, and engages in an audio/video conversation with the patient and a personal health coach at home. | The care coordination takes place between the members of the care team (i.e. telemonitoring nurse, informal caregiver, and patient) via voice communication and with the institutions it takes place via data sharing (i.e. telemonitoring center, hospital, and pharmacy). Voice communication takes place every fortnight while data are shared continuously. |
| Governance | Who should perform them, and Where? | Hospital and technology partner (i.e. equipment manufacturer). The governance takes place in a clinical setting by licensed practitioners, while the equipment manufacturer is responsible for the system maintenance and data protection. | International and national governing bodies. In a jurisdiction where a government acts as an insurer it should perform licensing and supervision. In other geographies an international telehealth organization should provide governance. |
| Themes | |||
| Novelty | Adopt innovative content, structure, or governance | Innovative content, old structure, and governance. | Innovative content, structure, and governance. |
| Lock-In | Build in elements to retain business model stakeholders, e.g. customers | Customers/patients are locked in by the installation of the equipment in their home. | Customers/patients are not locked in and can opt out of the service at any time. |
| Complementarities | Bundle activities to generate more value | Community services generate value for the patient. Clinical trials generate value for the hospitals and the equipment manufacturer. | Monitoring comorbidities generates value for the patient. Population monitoring generates value for the government. Big data generate value for the equipment manufacturer. |
| Efficiency | Reorganize activities to reduce transaction costs | High search, negotiation, and enforcement costs. | Medium search costs, and low negotiation and enforcement costs |
B2B: business-to-business; B2C: business-to-consumer.
Source: Adapted from Zott and Amit.14
The transaction costs of the B2B case are relatively high. Customers (patients) can spend considerable time/resources in searching for the telemonitoring provider (via their physician) and understanding the disease-related implications of the program. Patients have to negotiate the eligibility in terms of the severity of the disease, location, and ongoing costs.37 In the end, patients need to enforce the contract either by installing/deinstalling the equipment in their home or by negotiating with the provider and insurance company to keep it after the trial has ended.37
In the B2C case, the expected reduction in search costs is due to easier access to information via the Internet (or mass media), the reduction in negotiation costs thanks to an app-store-based contract (predefined and only “a click away”), and the reduction in enforcement costs due to the ease of downloading the mobile app and joining the service, or deleting it (i.e. opting out). Patients can act freely in the marketplace because they are paying for the service, and this is promoting consumer-driven services in healthcare. The negotiating costs are virtually zero in the B2C case, as they are with all app-based services and contracts. The enforcement costs for telemonitoring chronic diseases are also close to zero, as the B2C model of digital service distribution puts the power into the hands of consumers (i.e. they can opt out at any time).
Discussion
We explored the activity system in the B2B and B2C telemonitoring applications for patients with chronic diseases, with the aim of understanding the care coordination and the economic principles that govern the effectiveness in both business models. We believe there are principal differences in several design elements (structure and governance) and themes (novelty, lock-in, complementarities, and efficiency), with lower transaction costs in the B2C model due to the lower search, negotiation, and enforcement costs. The business models of B2B and B2C telemonitoring, and the value propositions, are reviewed elsewhere in Chen et al.12 and Acheampong and Vimarlund38 but the activity systems are not.
In the B2B model the activity system is organized around the places while the governance of the system lies with hospitals (the true customers) and equipment manufacturers. The B2C model revolves around the players whose actions should be overseen by a government or insurer. The asymmetry of information, the structures, and the competences might give hospitals power over other agents in the healthcare market, namely patients (customers) and equipment manufacturers (suppliers). Patients have no say in procurement, and thus the demand for the B2B telemonitoring remains weak.
The B2B model creates a firmer lock-in than B2C, but for a limited time (e.g. until supported by insurance payments). On the other hand, patients can stay with the B2C telemonitoring service while transitioning to another healthcare provider/insurer, which ensures a long-term commitment. The B2C model also allows patients to procure the telemonitoring service at market prices, assuring a more equitable healthcare exchange.
There is some intrinsic uncertainty in relations between the agents in the marketplace that exist for long periods of time, such that agents in the exchange can exhibit undesirable behavior, i.e. opportunistic behavior.39 This opportunistic behavior means that an agent acts in their own interest, at the expense of all other agents.17 There are two applicable opportunistic behaviors40: opportunism due to the fact that an agent’s behavior is not visible, and opportunism due to the specific nature of the assets. The former is applicable to the B2C model (and can lead to moral hazard), while the latter is applicable to the B2B model of telemonitoring (the asset cannot be easily redeployed, and the participants in the exchange are bound to each other). The need to protect the parties from opportunistic behavior justifies the existence of governance structures.41 Beside national and international governing bodies, markets and hierarchies are proposed as alternative ways of governing these transactions.24
Pelletier-Fleury et al.17 used transaction cost economics as a conceptual framework for the analysis of barriers to the diffusion of telemedicine. They found that “the introduction of telemedicine shifts the costs associated with agents’ opportunism from patients to healthcare suppliers themselves.”17 These costs prevent the wider implementation of telemedicine and telemonitoring. Pelletier-Fleury et al.17 provided a solution for reducing the transaction costs associated with behavioral factors (bounded rationality and opportunism) and environmental factors (uncertainty and asset specificity) by creating an institutional arrangement associated with the healthcare transactions. Due to the high specificity of the telemedicine asset, and institutional uncertainty, they advocate the integration of transactions in a unified structure. We take their research one step further, by applying the same reasoning for telemonitoring chronic diseases in the B2B case (via hospitals), but also in the B2C case (via a telemonitoring center).
From this theoretical exercise, it would appear that the B2C model has advantages over the B2B model in the implementation of telemonitoring, such as supply chain optimization (with five instead of seven people involved in care coordination), low negotiation and enforcement costs, and long-term outlook. The communication between players is expected to be more efficient than between places. The patient is decoupled from interactions with hospitals and pharmacies, enabling healthcare services to be provided irrespective of the location of the agents. This not only potentially improves implementation of telemonitoring via the B2C model but also ensures easier access to healthcare.
Transaction cost theory posits that “the optimum organizational structure is one that achieves economic efficiency by minimizing the costs of exchange.”42 The costs are often a result of the imperfections in possession of information, by participants in the market, and the value that agents place on the exchange. The patient can be seen as an agent willing to invest in resources to mitigate these imperfections. However, the investment needed to do so is substantial, and in many cases detrimental to the effort. This is certainly true for the B2B model, where transaction costs are high but might not be true for the B2C. Even if a patient makes a “wrong” decision and incurs switching costs in the B2C model, they still might be smaller in absolute terms than transaction costs of the B2B model. This might be a promoting economic principle for B2C telemonitoring.
North43 proposed a theoretical framework for the measurement of transaction costs, i.e. the calculation of the value of all aspects of the good or service involved in a transaction. Measurement, being his first factor in his take on transaction costs, is related to his third, ideological attitudes and perceptions. They encapsulate each individual’s set of values, which influence one’s interpretation of the world. In a B2C model, consumers have to search and compare multiple sources of information, depending on how many suppliers partake in the market, with unknown quality compared to the information they receive from a provider such as a hospital or physician in the B2B model. By eliciting ideological values and perceptions, it is permissible that a person will find more value or quality in information given in the B2B model, via hospitals/physicians, than in the B2C model. However, the ease of finding information and the costs will remain the same, and they are in our opinion lower in the B2C model. The value of information, in respect to transaction costs but also cost-effectiveness in B2B and B2C telemonitoring of chronic diseases, is yet to be determined, and so is the expected value of perfect information, i.e. the price one should pay to get rid of uncertainty in one’s decision making.44
Our analysis was not without limitations. The literature search was performed by one author (ASG) while all authors were involved in the data analysis. For the literature review, a convenience sample was used. The creation of the telemonitoring cases was based on the sample of peer-reviewed and non-peer-reviewed sources (journal articles, conference papers, and case studies). The assessment of the design elements and themes of the activity system in both models was not impartial. The same is true for the assessment of the transaction costs in the efficiency domain. However, we believe that, given the aim of this study, the strategy applied was suitable to conceptually design the B2B and B2C cases and to explore the potential value of two business models in a descriptive and interpretative manner. Future research should test our models, for example by collecting empirical data from different sites where telemonitoring is applied to support care coordination.
Telemonitoring is commonly introduced to chronic disease patients via the B2B model and is implemented via arrangements between equipment manufacturers and care providers—homecare agencies, delivery systems, and health plans.45 This takes agency away from patients and burdens them heavily with search, negotiation, and enforcement costs. It renders the B2B model inefficient in comparison to the B2C model, because of the high exchange costs, which could explain the anemic uptake of telemonitoring so far and the suboptimal coordination of care.
The activity system perspective allowed us to see the complexities of care coordination in chronic disease management via innovation in the business model. The transaction costs framework was a useful way of considering the efficiency of introducing information systems to healthcare. The B2B and B2C cases created for telemonitoring chronic diseases principally differ in design elements (structure and governance) and design themes (novelty, lock-in, complementarities, and efficiency). In the B2B model, we believe the search costs are high, negotiation costs even higher (if possible), and enforcement costs the highest. In the B2C model the situations is completely the opposite—transaction costs are small in search, smaller in negotiation, and virtually zero in enforcement. Thus, implementation of telemonitoring for chronic diseases via the B2C model can potentially free up financial resources, which can either be used to support a greater number of people with the same technology or can be invested in new treatments and therapies.
Acknowledgements
We are grateful to Reinhold Grellmann who supported this research in his position of a Department Head, Professional Healthcare Services & Solutions, Philips Research.
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: A Grustam was an employee of Philips at the time of writing this manuscript. R Koymans is fully employed by Philips. JL Severens has received a consulting fee paid to his institution by Philips. A Cordella and HJM Vrijhoef declare no conflict of interest.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by Philips Research.
References
- 1.Murray CJL, Barber RM, Foreman KJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet 380; 2013: 2197–2223, http://linkinghub.elsevier.com/retrieve/pii/S014067361561340X (August 2015, accessed 11 October 2015). [DOI] [PMC free article] [PubMed]
- 2.Suhrcke M, Nugent R, Stuckler D, et al. Chronic disease: an economic perspective London: Oxford Health Alliance, http://www.sehn.org/tccpdf/Chronic%20disease%20economic%20perspective.pdf (2006, accessed 8 March 2016).
- 3.Abegunde DO, Mathers CD, Adam T, et al. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet 2007; 370: 1929–1938. [DOI] [PubMed] [Google Scholar]
- 4.Dall TM, Gallo PD, Chakrabarti R, et al. An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff 2013; 32: 2013–2020. [DOI] [PubMed] [Google Scholar]
- 5.Norris DSL, Glasgow RE, Engelgau MM, et al. Chronic disease management. Dis Manag Health Outcomes 2012; 11: 477–488. [Google Scholar]
- 6.Øvretveit J. Integrated care: models and issues. Göteb Nord Sch Public Health Brief Pap. http://scholar.google.com/scholar?cluster=15009307362389054865& hl=en&oi=scholarr (1998, accessed 8 March 2016).
- 7.Schultz EM and, McDonald KM. What is care coordination? Int J Care Coord 2014; 17: 5–24. [Google Scholar]
- 8.Kodner DL and, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications – a discussion paper. Int J Integr Care 2002; 2 http://www.ijic.org/index.php/ijic/article/viewArticle/67 (accessed 9 March 2016). [Mismatch] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sood S, Mbarika V, Jugoo S, et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E-Health 2007; 13: 573–590. [DOI] [PubMed] [Google Scholar]
- 10.WHO. Telemedicine: opportunities and developments in member states Geneva: World Health Organization, http://whqlibdoc.who.int/publications/2010/9789241564144_eng.pdf (2008, accessed 13 April 2016)
- 11.Paré G, Jaana M and, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc 2007; 14: 269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen S, Cheng A and, Mehta K. A review of telemedicine business models. Telemed J E-Health 2013; 19: 287–297. [DOI] [PubMed] [Google Scholar]
- 13.Chesbrough H and, Rosenbloom RS. The role of the business model in capturing value from innovation: evidence from Xerox Corporation’s technology spin-off companies. Ind Corp Change 2002; 11: 529–555. [Google Scholar]
- 14.Zott C and, Amit R. Business model design: an activity system perspective. Long Range Plann 2010; 43: 216–226. [Google Scholar]
- 15.Hopp F, Whitten P, Subramanian U, et al. Perspectives from the Veterans Health Administration about opportunities and barriers in telemedicine. J Telemed Telecare 2006; 12: 404–409. [DOI] [PubMed] [Google Scholar]
- 16.Willemse E, Adriaenssens J, Dilles T, et al. Do telemonitoring projects of heart failure fit the chronic care model? Int J Integr Care 2014; 14 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4109584/ (accessed 22 January 2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pelletier-Fleury N, Fargeon V, Lanoé J-L, et al. Transaction costs economics as a conceptual framework for the analysis of barriers to the diffusion of telemedicine. Health Policy 1997; 42: 1–14. [DOI] [PubMed] [Google Scholar]
- 18.Dahlman CJ. The problem of externality. J Law Econ 1979; 22: 141–162. [Google Scholar]
- 19.Engeström Y, Miettinen R and, Punamäki R-L. Perspectives on activity theory. Cambridge: Cambridge University Press, 1999, 484p.
- 20.Siggelkow N. Change in the presence of fit: the rise, the fall, and the renaissance of Liz Claiborne. Acad Manage J 2001; 44: 838–857. [Google Scholar]
- 21.Kleindorfer PR and, Wind Y. The network challenge: strategy, profit, and risk in an interlinked world . Pearson Prentice Hall: Wharton School Pub, 2009, 590p. [Google Scholar]
- 22.Williamson OE. Transaction-cost economics: the governance of contractual relations. J Law Econ 1979; 22: 233–261. [Google Scholar]
- 23.Williamson OE. The economic institutions of capitalism . New York: Simon and Schuster, 1985, 473p. [Google Scholar]
- 24.Cordella A. Transaction costs and information systems: does IT add up? J Inf Technol 2006; 21: 195–202. [Google Scholar]
- 25.Parkhe A. Strategic alliance structuring: a game theoretic and transaction cost examination of interfirm cooperation. Acad Manage J 1993; 36: 794–829. [Google Scholar]
- 26.Given L. The SAGE encyclopedia of qualitative research methods Thousand Oaks, CA: SAGE Publications, Inc., http://knowledge.sagepub.com/view/research/SAGE.xml (2008, accessed 5 May 2015).
- 27.Hsieh H-F and, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–1288. [DOI] [PubMed] [Google Scholar]
- 28.Griffioen E. Business model design for the healthcare sector: sustainable business model design for heart failure home telemonitoring opportunities in Western Europe Delft: Delft University of Technology, http://repository.tudelft.nl/view/ir/uuid:167949c6-aa52-4608-89dd-148a6f5025ab/ (2012, accessed 16 July 2015).
- 29.Wen HJ and, Tan J. The evolving face of telemedicine & e-health: opening doors and closing gaps in e-health services opportunities & challenges. In: 2003 Proceedings of the 36th annual Hawaii international conference on system sciences, 6–9 January 2003, Big Island, HI, USA, p.12. IEEE, http://ieeexplore.ieee.org/xpls/abs_all.jsp?arnumber=1174374 (2003, accessed 13 December 2015).
- 30.Shevchenko AA. B2B e-hubs in emerging landscape of knowledge based economy. Electron Commer Res Appl 2005; 4: 113–123. [Google Scholar]
- 31.Herzlinger R, Kindred N and, McKinley S. Philips-Visicu.pdf Cambridge, MA, USA: Harvard Business Publishing, 2014, https://cb.hbsp.harvard.edu/cbmp/product/313015-PDF-ENG. (2012, accessed 30 April 2016)
- 32.Kung H-Y, Hsu C-Y, Lin M-H, et al. Mobile multimedia medical system: design and implementation. IJMC 2006; 4: 595–620. [Google Scholar]
- 33.Lähteenmäki J, Leppänen J, Kaijanranta H, et al. Document-based service platform for telemedicine applications. In: VTT symposium on service science, technology and business, Helsinki, 2008, VTT Technical Research Centre of Finland, p.178, https://www.researchgate.net/profile/Kjell_Nikus2/publication/38288780_Document-based_service_platform_for_telemedicine_applications/links/540ea2f80cf2df04e756dfa0.pdf#page=180 (2008, accessed 30 May 2016).
- 34.Pels J, Schurmann N and, Garcia MC. BioScience Argentina: BioMobile and the telemedicine market. Emerg Markets Case Stud 2011; 1: 1–24. [Google Scholar]
- 35.Wac K and, Hausheer D. COPD24: From future internet technologies to health telemonitoring and teletreatment application. In: Twelfth IFIP/IEEE international symposium on integrated network management (IM 2011) and workshops, Dublin, Ireland, 2011, IEEE, pp.812–826.
- 36.Sethi R, Bagga G, Carpenter D, et al. Telecare: legal, ethical and socioeconomic factors. In: International conference on telehealth (Telehealth 2012), 2012, http://eprints.port.ac.uk/8336/ (accessed 21 December 2016).
- 37.Seto E, Leonard KJ, Cafazzo JA, et al. Perceptions and experiences of heart failure patients and clinicians on the use of mobile phone-based telemonitoring. J Med Internet Res 2012; 14: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3374534/ (accessed 21 December 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Acheampong F and, Vimarlund V. Business models for telemedicine services: a literature review. Health Syst, http://www.palgrave-journals.com/hs/journal/vaop/ncurrent/full/hs201420a.html (2014, accessed 10 March 2015). [Mismatch] [Google Scholar]
- 39.Barney JB and, Ouchi WG. Organizational economics: toward a new paradigm for understanding and studying organizations. 1st ed San Francisco, CA: Jossey-Bass, 1986, 514p. [Google Scholar]
- 40.Alchian AA and, Woodward S. The firm is dead; long live the firm a review of Oliver E. Williamson’s the economic institutions of capitalism. JSTOR 1988; 26. http://www.jstor.org/stable/2726609 (accessed 21 December 2015).
- 41.Williamson OE. Comparative economic organization: the analysis of discrete structural alternatives. Adm Sci Q 1991: 36: 269–296. [Google Scholar]
- 42.Young DS. Transaction cost economics In: Idowu SO, Capaldi N, Zu L, et al. (eds) Encyclopedia of corporate social responsibility. Berlin Heidelberg: Springer, 2013, pp.2547–2552. http://link.springer.com/referenceworkentry/10.1007/978-3-642-28036-8_221 (accessed 16 December 2015). [Google Scholar]
- 43.North DC. Transaction costs, institutions, and economic performance. San Francisco, CA: ICS Press, 1992. [Google Scholar]
- 44.Steuten L, Wetering G, van de Groothuis-Oudshoorn K, et al. A systematic and critical review of the evolving methods and applications of value of information in academia and practice. Pharmacoeconomics 2013; 31: 25–48. [DOI] [PubMed] [Google Scholar]
- 45.Coye MJ, Haselkorn A and, DeMello S. Remote patient management: technology-enabled innovation and evolving business models for chronic disease care. Health Aff 2009; 28: 126–135. [DOI] [PubMed] [Google Scholar]