Abstract
Objective
The purpose of this narrative systematic review was to summarise prognostic factors for return to work (RTW) among people with long-term neck/shoulder or back pain.
Methods
A systematic literature search was performed through three databases (Medline, CINAHL and PsycINFO) for studies published until February 2016. Only observational studies of people on work absence (≥2 weeks) due to neck/shoulder or back pain were included. The methodological quality of the included studies was assessed using guidelines for assessing quality in prognostic studies on the basis of Framework of Potential Biases. Factors found in the included studies were grouped into categories based on similarities and then labelled according to the aspects covered by the factors in the category.
Results
Nine longitudinal prospective cohort studies and one retrospective study fulfilled the inclusion criteria. From these, five categories of factors were extracted. Our findings indicate that recovery beliefs, health-related factors and work capacity are important for RTW among people with long-term neck or back pain. We did not find support for workplace factors and behaviour being predictive of RTW.
Conclusions
Our findings suggest that recovery beliefs, perceived health and work capacity may be important targets of intervention for people with long-term neck or back pain. However, more high-quality prospective studies are needed to confirm the results and improve our understanding of what is needed to facilitate RTW in this population.
Keywords: musculoskeletal, work ability, prognostic factors, sick leave
Strengths and limitations of this study.
The review identifies prognostic factors of importance for the natural course of return to work in people with long-term pain.
Findings are based on quality-assessed studies considering areas of potential bias.
Few high-quality studies prevent solid conclusions about prognostic factors in this population.
Since most studies concerned low back pain only, the results are less applicable to people with neck pain.
Introduction
Work absence due to musculoskeletal disorders (MSDs) is a considerable public health problem, as it results in workers’ compensation, medical expense as well as productivity loss.1–5 Low back pain (LBP) is considered one of the leading causes of work absence6–9 and neck/shoulder disorders are also among most common reasons for being absent from work.10–12 Despite improvements in objective measures of health, work absence has increased substantially in western European countries.4 13–15 It may be that workers have difficulties returning to work for reasons other than their health condition, for instance psychosocial problems.16–19
It follows that return to work (RTW) following MSDs is a complex process that is not solely dependent on physical ability. Studies have shown that it may also be affected by recovery beliefs, pain-related behaviours, work-related factors and health-related factors,17 20–29 but the results differ considerably between studies. Reasons for this may be heterogeneous samples, differences in measurements and the analytical strategy used for identifying the factors. Moreover, many studies have been conducted to identify risk factors for work absence,16 30–33 but their results cannot be readily inverted to indicate what is needed for people to RTW. To reduce work absence among people with MSDs, it is important to know which factors are important for RTW, and thereby what should be prioritised in the treatment/rehabilitation.
To date, most empirical studies on pain and RTW have focused on acute pain and LBP.31 33–35 Accordingly, most of previous systematic reviews addressing factors of importance for RTW have focused on people with acute pain. For example, Steenstra et al 20 found that workers’ recovery expectations are important factors affecting the likelihood and timing of RTW among workers with acute LBP. This was confirmed in a later review of RTW among people with non-chronic non-specific LBP.17 Hartvigsen et al 36 reviewed the evidence of psychosocial factors at work being important for RTW among people with LBP, and concluded that there is insufficient evidence of it.
To our knowledge, previous studies on factors affecting RTW among people with long-term (ie, not acute) pain in the neck/shoulder or back have not been systematically reviewed. It is possible that these factors differ from factors considered important for RTW among people with acute pain. Therefore, the aim of the present systematic review was to narratively summarise prognostic factors for RTW among people with long-term neck/shoulder or back pain.
Methods
Identification of studies
We performed an extensive search through each of the databases Medline, CINAHL and PsycINFO from its inception until February 2016 for observational studies published in English of prognostic factors for RTW among people with pain in the neck/shoulder or back. A detailed description of the search terms and search strategy is presented in the online supplementary appendix 1. The terms used in the search were defined based on the ideas behind the PICO model.37 We selected suitable keywords for P (population), I (intervention), O (outcome), while C (comparison) was excluded since comparison studies were not the focus for this study. Afterwards, the results from the three databases were combined. The reference list for each selected study was screened for additional relevant studies. Moreover, a search for studies that have cited each selected study was performed using the Scopus database, and reviews or meta-analyses were screened for relevant references or included studies.
Selection of studies
All authors independently screened the titles, abstracts and, if necessary, the full text of the articles for eligibility based on the inclusion criteria:
subjects’ age between 18 and 65 years
work absence ≥2 weeks
neck/shoulder or back pain.
Work absence was defined as part-time or full-time absenteeism from work. The lower limit of 2 weeks was set to avoid inclusion of studies on prognostic factors related to acute injury or trauma, since they might differ substantially from prognostic factors related to long-term pain. Accordingly, long-term pain in the neck, shoulder or back was defined as pain that was not attributed to acute injury or trauma requiring at least 2 weeks part-time or full-time absenteeism from work. The exclusion criteria were:
outcome not RTW
non-observational study (ie, review/meta-analysis, intervention study or clinical trial)
confounding rehabilitation programme
instrumental validation
population partly consisting of subjects fitting the inclusion criteria but for whom the results were not reported specifically.
Return to work can be described as an individual’s cognitive and behavioural response to no longer being absent from work due to sickness.38 Consequently, it can be measured in different ways. In the present review, RTW was defined as being back at work (part-time or full-time) for at least 1 day. Following this definition, any indicator of work resumption was acceptable.
Quality assessment
Two reviewers (MR, MH) independently assessed the methodological quality of the included studies using a set of criteria that was adapted from ‘guidelines for assessing the quality in prognostic studies on the basis of Framework of Potential Biases.’39 It included six quality assessment criteria with focus on the key areas of potential bias in prognostic studies: study population, study attrition, measurement of prognostic factors, measurement of outcomes, measurement of and controlling for confounding variables, and analysis approaches (table 1). In the second criterion, the limits for response rate and loss to follow-up were set to 65% and 35%, respectively. They were considered relevant in light of declining participation rates in epidemiologic studies, and have been used in previous health-related research.40 41 In the fifth criterion, we considered age, gender, prior work absence and comorbidity as potentially important confounders to be accounted for in the analysis, as their association with RTW in people with neck/shoulder or back pain has previously been demonstrated.23 26 42–44
Table 1.
Quality assessment criteria
| 1 | Did the sample represent the population of interest? |
| 2 | Was loss to follow-up <35% and response rate >65%? |
| 3 | Were the prognostic factors measured with valid and reliable instruments? |
| 4 | Was the outcome of the study objectively measured? |
| 5 | Were important potential confounders (ie, age, gender, prior WA and comorbidity) appropriately accounted for in the analysis? |
| 6 | Was the statistical analysis appropriate? |
WA, work absence.
The reviewers graded each criterion as yes=2, partly=1 or no/unclear=0 on the basis of information provided in the articles. Criterion 1 (study population) was graded ‘partly’ if a subgroup of the population fulfilled our inclusion criteria. Criterion 2 (study attrition) was graded ‘partly’ if either the response rate exceeded 65% or the loss to follow-up was less than 35%. Criterion 3 (prognostic factors) was graded ‘partly’ if the validity and/or reliability was reported for some, but not all, measurements of prognostic factors.
Criterion 4 (outcomes) was graded ‘partly’ if some, but not all, outcomes were measured objectively. Criterion 5 (confounders) was graded ‘partly’ if some, but not all, listed variables were controlled for in the analysis. Criterion 6 (analysis) was graded ‘yes’ if a multiple regression model corresponding to the outcome measurement was used and the predictors were selected without relying on empirical information about the measured exposure,45 ‘partly’ if a multiple regression model corresponding to the outcomes measurement was used and stepwise or bivariate statistical analysis of each potential predictor’s association with the outcome was used to guide the selection of predictors in the model, and ‘no/unclear’ otherwise. In case of disagreement between the two reviewers, remaining reviewers also reviewed the article, and the judgement made by the majority of the reviewers determined the quality rating. A quality score for each study was calculated as the sum of all scores, thus ranging between 0 and 12 points where higher scores indicate better quality. No weighting was used, as we did not consider any area of potential bias to be more important than another.
Data synthesis
We identified main factors that were shown to be significantly (p<0.05) or non-significantly associated with RTW in the included studies. Factors that expressed related meanings, that is, based on similarities, were grouped together into categories. Afterwards, each category was labelled according to the factors investigated in the studies.
Results
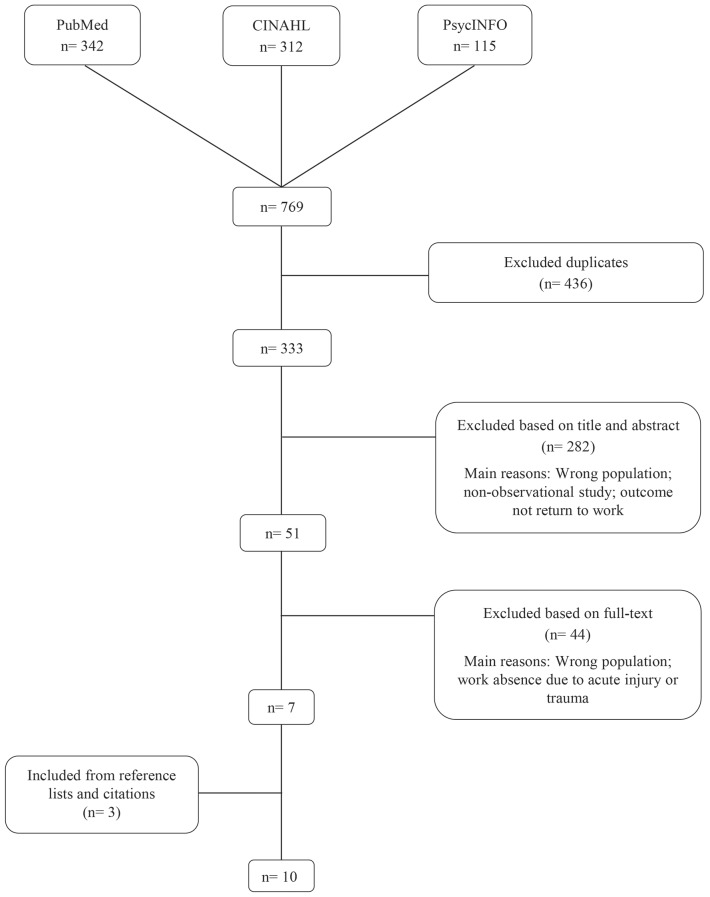
A flow diagram of the selection process is shown in figure 1. In total, 769 studies were identified from the databases search. After removing the duplicates, 333 studies remained. Out of these, 51 were considered eligible based on the title and abstract. When screening the 51 full texts, 7 studies met all of the inclusion criteria (see online supplementary appendix 2). In the additional search through reference lists and citations of the included studies, three studies fulfilled the inclusion criteria. As a result, a total of 10 studies46–55 remained for methodological quality assessment and synthesis of results.
Figure 1.
Flow diagram of the selection process. All authors independently screened the titles, abstracts and, if necessary, the full text of the articles.
These 10 studies originated from Sweden, Belgium, the USA, Canada and the Netherlands (table 2). All of them were longitudinal prospective cohort studies with a follow-up of 3–24 months, except one that was retrospective. They were conducted on populations with pain in the neck or low back that had been absent from work for at least 4 weeks. Table 2 describes each of the selected studies in terms of study design, study population, sample size, attrition and factors identified as significant and non-significant, respectively, in relation to the outcome RTW.
Table 2.
Characteristics and findings of the included studies
| Author (year) | Place of study | Study design | Length of follow-up | Study population | Sample size and dropout | Significant main factors* | Non-significant main factors | Measurements of RTW |
| Berglind and Gerner (2002)46 | Sweden | Prospective cohort | 24 months | Age: 18–55 years Gender: NA Pain: low back and neck Work absence: ≥8 weeks Pain duration: ≥8 weeks |
n=289 Response rate: NA Dropout: NA |
Work motivation | Work status (Yes/No) | |
| Du Bois et al (2009)49 | Belgium | Prospective cohort | 6 months | Age: 18–64 years Gender: male and female Pain: low back Work absence: ≥4 weeks Pain duration: ≥4 weeks |
n=390 Response rate: 89% Dropout: 0% |
Disability Pain behaviour Fear avoidance beliefs Type of work Prior pain duration |
Work status (Yes/No) |
|
| Gallagher et al (1995)47 | USA | Prospective cohort | 6 months | Age: ≥18 years Gender: male and female Pain: low back Work absence: ≥24 weeks Pain duration: ≥24 weeks |
n=169 Response rate: NA Dropout: 6% |
Compensation status Use of lawyer |
Work status (Yes/No) |
|
| Gross et al (2004) part I50 | Canada | Retrospective cohort (two cohorts) | 12 months | Age: x̅=41 (c1), 40 (c2), SD=10 (c1), 9 (c2) years Gender: male and female Pain: low back Work absence :≥6 weeks Pain duration: ≥6 weeks |
n=150 (c1), NA (c2) Response rate: 76% (c1), NA (c2) Dropout: 32% (c1), 34% (c2) |
Functional capacity | Time until suspension of time-loss benefits, time until claim closure | |
| Gross and Battié (2005)51 | Canada | Prospective cohort | 12 months | Age: x̅=42, SD=11 years Gender: male and female Pain: low back Work absence: ≥6 weeks Pain duration: ≥6 weeks |
n=138 Response rate: 70% Dropout: 54% |
Recovery beliefs | Time until suspension of time-loss benefits, time until claim closure | |
| Hansson et al (2006)52 | Sweden | Prospective cohort | 24 months | Age: 18–59 years Gender: male and female Pain: low back or neck Work absence: ≥4 weeks Pain duration: ≥4 weeks |
n=1575 Response rate: 64%–79% Dropout: 28%–55% |
Quality of life Disability |
Prevalence of work resumption | |
| Kuijer et al (2012)53 | Netherlands | Prospective cohort | 12 months | Age: 18–55 years Gender: male Pain: low back Work absence: ≥6 weeks Pain duration: ≥6 weeks |
n=72 Response rate: NA Dropout: 4% |
Work ability | Age Functional capacity |
Time until working ≥4 weeks |
| Schultz et al (2004)54 | Canada | Prospective cohort | 3 months | Age: 18–60 years Gender: male and female Pain: low back Work absence: ≥4 weeks Pain duration: ≥4 weeks |
n=781 Response rate: 32% Dropout: 15% |
Health transition Recovery expectations |
Coworker support | Work status (Yes/No) |
| Schultz et al (2005)48 | Canada | Prospective cohort | 3 months | Age: 18–60 years Gender: male and female Pain: low back Work absence: 4–6 weeks Pain duration: ≥4 weeks |
n=111 Response rate: NA Dropout: 9% |
Recovery expectations Symptoms/complaints |
Vitality Mental health |
Work status (Yes/No) |
| van der Giezen et al (2000)55 | Netherlands | Prospective cohort | 12 months | Age:18–60 years Gender: male and female Pain: low back Work absence: ≥12 weeks Pain duration: ≥12 weeks |
n=328 Response rate: 91% Dropout=9% |
Age General health Job satisfaction Breadwinner Pain intensity |
Work status (Yes/No) |
Quality scores
For the 10 selected studies, the quality scores ranged from 4 to 9 points. The studies were classified as low quality (0–4 points), medium quality (5–8 points) and high quality (9–12 points) (table 3).
Table 3.
Methodological quality scores of the included studies
| Author (year) | Representative sample of relevant population | Study attrition (loss to follow-up and response rate) | Valid and reliable instruments for predictors | Objectively measured outcomes | Controlled for age/gender/prior WA/comorbidity |
Appropriate statistical analysis | Quality score |
| Berglind and Gerner (2002)46 | 2 | 0 | 0 | 2 | 0 | 0 | 4 |
| Du Bois et al (2009)49 | 2 | 2 | 0 | 0 | 0 | 1 | 5 |
| Gallagher et al (1995)47 | 1 | 1 | 0 | 0 | 1 | 1 | 4 |
| Gross et al (2004), part I50 | 2 | 2 | 1 | 2 | 1 | 1 | 9 |
| Gross and Battié (2005)51 | 2 | 1 | 1 | 1 | 0 | 0 | 5 |
| Hansson et al (2006)52 | 2 | 1 | 0 | 2 | 0 | 0 | 5 |
| Kuijer et al (2012)53 | 1 | 1 | 0 | 2 | 1 | 2 | 7 |
| Schultz et al (2004)54 | 2 | 2 | 0 | 1 | 0 | 1 | 6 |
| Schultz et al (2005)48 | 2 | 1 | 0 | 0 | 0 | 1 | 4 |
| van der Giezen et al (2000)55 | 2 | 2 | 0 | 0 | 1 | 1 | 6 |
2=criterion is satisfied; 1=criterion is partly satisfied; 0=criterion is not satisfied or cannot be determined.
Maximum quality score=12; 0–4 points were considered low quality, 5–8 points were considered medium quality and 9–12 points were considered as high quality.
WA, work absence.
In the synthesis of results, five categories of the factors were extracted: recovery beliefs, health-related factors, workplace factors, work capacity and behaviour (table 4). Each of them is described in detail below.
Table 4.
Categorisation of factors
| Factors | Measurement | Categories |
| Recovery beliefs46 51 | Expectations of Recovery Scale, single questions | Recovery beliefs |
| Recovery expectations48 54 | Work-related Recovery Expectations Questionnaire | |
| Quality of life52 | EuroQol | Health-related factors |
| Health transition54 | Short Form (36) Health Survey | |
| Vitality48 | Short Form (36) Health Survey | |
| Mental health48 | Short Form (36) Health Survey | |
| General health55 | Short Form (36) Health Survey | |
| Type of work49 | Single question | Workplace factors |
| Coworker support54 | Single question | |
| Job satisfaction55 | Job Satisfaction Scale | |
| Disability49 52 | Von Korff’s pain and disability score, single questions | Work capacity |
| Prior pain duration49 | Single question | |
| Functional capacity50 53 | Functional capacity evaluation lifting tests, Isernhagen Work Systems Functional Capacity Evaluation | |
| Work ability53 | Work Ability Index | |
| Pain intensity55 | Pain Complaint Questionnaire | |
| Symptoms/complaints48 | Single questions | |
| Pain behaviour49 | Pain Behaviour Scale | Behaviour |
| Fear avoidance beliefs49 | Fear Avoidance Beliefs Questionnaire |
EuroQol, European Quality of Life Scale.
Gallagher et al. (1995) was not included since the factors Compensation status and Use of lawyer could not readily be categorized with other factors.
Recovery beliefs
Recovery beliefs comprise many aspects, such as believing that you will be able to function or work in the presence or absence of pain, or that you will be in control of your situation.56 They were evaluated as predictors of RTW in two low and two medium-quality studies.46 48 51 54 All studies reported a significant positive association between recovery beliefs and RTW, when the predictor was measured by the Expectations of Recovery Scale, the Work-related Recovery Expectations Questionnaire, and single questions, respectively (table 4).
Health-related factors
Health is a multifaceted concept, and more than merely the absence of disease.57 It involves several dimensions, for example, quality of life and vitality. It can also be separated into physical and mental components. Among the reviewed studies, the association between health-related factors and RTW was investigated in four studies of low and medium qualities. The medium-quality studies consistently reported that health, in terms of health-related quality of life, health transition and general health, was a significant predictor of RTW.52 54 55 In the low-quality study, no significant association between vitality, mental health and RTW was found.48 Table 4 shows the instruments used to measure the health-related factors.
Workplace factors
Three medium-quality studies investigated the association between workplace factors and RTW. Two of them showed that type of work (blue colour work) and job satisfaction, respectively, significantly related to RTW,49 55 whereas one study found no significant association between coworker support and RTW.54 The different predictors were measured using single questions and the Job Satisfaction Scale (table 4).
Work capacity
Several studies investigated the predictive ability of factors related to work capacity for RTW. Among them, two medium-quality studies found that pain intensity and prior pain duration were significantly associated with RTW.49 55 In one low-quality and two medium-quality studies, self-rated disability was also identified as a significant predictor of RTW.48 49 52 Work ability, measured by the Work Ability Index, contributed significantly to RTW in one medium-quality study.53 One high-quality and one medium-quality study investigated the prognostic value of functional capacity tests for RTW, and found different results.50 53 In the high-quality study, findings from functional capacity lifting tests significantly predicted RTW, whereas in the medium-quality study, findings from functional capacity evaluation involving several tasks showed no significant association with RTW. More information about the measurement of the factors is presented in table 4.
Behaviour
Pain behaviour and fear avoidance beliefs were investigated in one medium-quality study, where both were identified as significant predictors for RTW.49 In the study, pain behaviour was measured by the Pain Behaviour Scale, and fear avoidance beliefs with the Fear Avoidance Beliefs Questionnaire (table 4).
Discussion
In the present systematic review, we synthesised the results from observational studies of prognostic factors for RTW among people with long-term neck or back pain. A total of 10 studies were included from the literature search. Among them, one was classified as high quality, six as medium quality and three as low-quality studies according to our quality assessment criteria. From the studies, five categories of factors were extracted: recovery beliefs, health-related factors, workplace factors, work capacity and behaviour.
Recovery beliefs
Our findings, suggesting that recovery beliefs are important for RTW, are consistent with previous reviews of people with back pain showing that recovery beliefs are associated with better health outcomes and RTW.17 22 One possible explanation for recovery beliefs being related to RTW is that when people believe that they will not recover from the illness, they may experience lower competence and motivation for returning to work.17 21 58 The fact that simple measurements of recovery beliefs can be used to predict RTW may be useful in practice, when determining which treatment/rehabilitation to apply.
Health-related factors
Previous reviews of people with acute, subacute and non-specific LBP17 59 have shown that health is an important predictor of RTW. Among the studies included in this review, the results were not entirely consistent. Considering the quality of the studies, and the different aspects of health investigated, it appears that health-related factors should be paid attention to in relation to RTW. It seems reasonable that perceived health is positively associated with RTW, since healthy people are more likely to feel capable of working.20 23 60 For rehabilitation purposes, however, more information about which aspects of health are important for RTW is needed to provide targeted interventions for reducing work absence among people with long-term neck or back pain. To achieve this, more in-depth analyses of components of health that are important for RTW are needed.
Workplace factors
The diversity in results as well as workplace factors investigated in the studies prevents any solid conclusions from being drawn. While it is conceivable that type of work performed is important for RTW, it would likely depend on which types of work are considered, and it is not clear how this information could be useful in practice without more knowledge about the work demands involved. Previous reviews have found that job satisfaction cannot predict failure to RTW in patients with non-chronic non-specific LBP,17 and that coworker support is important for work disability following low back injury.16 61 Taken together, our results concerning the importance of workplace factors for RTW among people with long-term neck or back pain are inconclusive. More research is needed to confirm or refute this.
Work capacity
Among the studies of factors related to work capacity, the findings were mostly consistent. While self-rated measures of work capacity in terms of pain, disability or work ability can significantly predict RTW among people with long-term pain in the neck or back, the ability of functional capacity evaluation tests to do so may be affected by how the tests are performed. Our results are in agreement with previous reviews. For example, Crook et al 62 found that functional disability was an important prognostic factor of work outcome for people with low-back injury, and Verkerk et al 63 found evidence of a positive influence of lower pain intensity on RTW among people with non-specific LBP. It appears, therefore, that work capacity is important to be considered in the treatment/rehabilitation of people with MSDs in the neck or back.
Behaviour
Since factors relating to behaviour were investigated in only one study, no solid conclusions about its relation to RTW in this population can be drawn. Previous reviews are also inconsistent. Iles et al 17 concluded that fear avoidance beliefs are predictive of RTW among people with non-chronic non-specific LBP. However, Pincus et al 64 found little evidence to link fear of pain with poor outcome in acute LBP. This discrepancy may be due to differences in the populations studied and/or in the methods used for assessing the factors.
In two of the included studies, the impact of age on RTW was reported.53 55 In most studies, however, age is treated as a confounding factor, and the significance of it is not specifically reported. For that reason, and the fact that it cannot be targeted in treatment/rehabilitation, we have refrained from drawing conclusions from the reported findings. Interestingly, the study by van der Giezen et al 55 reported that being a breadwinner was positively associated with RTW among people with LBP. As it is the only study that has addressed the importance of responsibilities towards others in returning to work, no solid conclusions can be drawn about its importance. However, it may be an important factor to adjust for in future studies of RTW among people with MSDs.
Methodological considerations regarding the articles in the review
In most of the studies we retrieved during our literature search, no distinction was made between sick leave, absenteeism, work absence and time out of work. These are not standardised terms, but rather vary from country to country. For consistency, we used work absence throughout the paper.
Our definition of RTW allowed it to be measured differently in the studies. Some studies based it on records46 51 52 and others on self-report,49 51 53–55 and the studies differed in the duration and proportion of work needed to be defined as RTW. It is possible that more consistent use of definitions across studies would have affected the results obtained in the present study.
As effect sizes were not reported consistently in the studies, our conclusions were based on the information provided concerning the significant and non-significant factors for RTW. Only one study received a high-quality score based on the six methodological criteria for assessing the quality of prognostic studies. Surprisingly, no study reported the statistical power of the analysis performed, and in most of the studies the validity and reliability of the instruments used was not reported.
Strengths and limitations of the systematic review
Previous reviews on prognostic factors of RTW have focused largely on people with acute pain. The present review highlights predictors for RTW among people with long-term pain in the neck or back by considering observational studies only. Thereby, it contributes to previous findings by addressing factors of importance for patients with long lasting pain in their natural course of RTW.
The strength of the present systematic review is that we searched for studies in three databases covering a wide range of research papers, and that we used a long time interval for each of the databases so as to access as much as possible of relevant literature. We used clear inclusion and exclusion criteria with respect to the population, exposures and study outcome. We also assessed the quality of the studies and confirmed our findings among the authors. Only observational studies were included to minimise potential sources of bias and study the natural course of RTW. The quality of the studies was assessed by considering six important potential sources of bias in studies of prognostic factors.39 Since we considered them to be equally important for study quality, they were summarised into a single quality score. The quality score was then divided into tertiles to indicate the level of quality (low/medium/high) of the studies, thereby allowing quality as well as quantity to be considered in the synthesis of results.
One potential limitation is that only journals publishing studies in English were included, which may have led to the exclusion of important studies from our search. Furthermore, the small number of published studies on prognostic factors for RTW among people with long-term neck or back pain prevents us from drawing solid conclusions concerning predictive factors of RTW in this population. Moreover, as most of the included studies concerned LBP only, our results may be less applicable to people with neck pain. Although pain patients were investigated in all included studies, the aetiology of the pain was likely different. Some of the studies reported the origin of the pain,49 50 but others did not do so specifically.52 This may have affected our results.
Conclusion
In the present review, we identified five categories of factors from studies of RTW among people absent from work (≥2 weeks) due to long-term neck or back pain. Our results indicate that recovery beliefs, health-related factors and work capacity are important for RTW in this population. However, few studies have been conducted on this population, and the quality of the studies was generally not high. Thus, we call for more high-quality prospective studies that can improve our understanding of what is needed to facilitate RTW for people with long-term neck or back pain.
bmjopen-2016-014939supp001.pdf (183.3KB, pdf)
bmjopen-2016-014939supp002.pdf (82.7KB, pdf)
Supplementary Material
Acknowledgments
We would like to express our gratitude and appreciation to the librarian Malin Almstedt Jansson for assisting us in developing the search strategy.
Footnotes
Contributors: MR codeveloped the search strategy, performed the search, screened and quality assessed the articles, and drafted the manuscript. MLK codeveloped the search strategy, screened articles, contributed to the quality assessment of the articles and reviewed the initial drafts of the manuscript. AN codeveloped the search strategy, screened articles, contributed to the quality assessment of the articles and reviewed the initial drafts of the manuscript. MH conceived the study, codeveloped the search strategy, screened and quality assessed the articles, and reviewed the initial drafts of the manuscript. All authors have read and approved the final manuscript.
Funding: This project was supported by University of Gävle (Dnr. 2015/424).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data sets generated during and/or analysed during the current study are available from the corresponding author upon request.
References
- 1. Henderson M, Glozier N, Holland Elliott K. Long term sickness absence: Is caused by common conditions and needs managing. BMJ 2005;330:802–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Frank JW, Brooker AS, DeMaio SE, et al. . Disability resulting from occupational low back pain. Part II: what do we know about secondary prevention? A review of the scientific evidence on prevention after disability begins. Spine 1996;21:2918–29. [DOI] [PubMed] [Google Scholar]
- 3. Abenhaim L, Rossignol M, Gobeille D, et al. . The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine 1995;20:791–5. 10.1097/00007632-199504000-00010 [DOI] [PubMed] [Google Scholar]
- 4. Alexanderson K. Sickness absence: a review of performed studies with focused on levels of exposures and theories utilized. Scand J Soc Med 1998;26:241–9. [DOI] [PubMed] [Google Scholar]
- 5. Lancourt J, Kettelhut M. Predicting return to work for lower back pain patients receiving worker's compensation. Spine 1992;17:629–40. 10.1097/00007632-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 6. Ihlebaek C, Hansson TH, Laerum E, et al. . Prevalence of low back pain and sickness absence: a "borderline" study in Norway and Sweden. Scand J Public Health 2006;34:555–8. 10.1080/14034940600552051 [DOI] [PubMed] [Google Scholar]
- 7. Besen E, Young AE, Shaw WS. Returning to work following low back pain: towards a model of individual psychosocial factors. J Occup Rehabil 2015;25:25–37. 10.1007/s10926-014-9522-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gallagher RM, Rauh V, Haugh LD, et al. . Determinants of return-to-work among low back pain patients. Pain 1989;39:55–67. 10.1016/0304-3959(89)90175-9 [DOI] [PubMed] [Google Scholar]
- 9. Kool JP, Oesch PR, de Bie RA. Predictive tests for non-return to work in patients with chronic low back pain. Eur Spine J 2002;11:258–66. 10.1007/s005860100335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nyman T, Grooten WJ, Wiktorin C, et al. . Sickness absence and concurrent low back and neck-shoulder pain: results from the MUSIC-Norrtälje study. Eur Spine J 2007;16:631–8. 10.1007/s00586-006-0152-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Leboeuf-Yde C, Fejer R, Nielsen J, et al. . Consequences of spinal pain: do age and gender matter? A Danish cross-sectional population-based study of 34,902 individuals 20-71 years of age. BMC Musculoskelet Disord 2011;12:39 10.1186/1471-2474-12-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Borg K, Hensing G, Alexanderson K. Prediction of future low levels of sickness absence among young persons sick listed with back, neck, or shoulder diagnoses. Work 2004;23:159–67. [PubMed] [Google Scholar]
- 13. Waddell G. Preventing incapacity in people with musculoskeletal disorders. Br Med Bull 2006;78:55–69. 10.1093/bmb/ldl008 [DOI] [PubMed] [Google Scholar]
- 14. Ahrberg Y, Landstad BJ, Bergroth A, et al. . Desire, longing and vanity: emotions behind successful return to work for women on long-term sick leave. Work 2010;37:167–77. 10.3233/WOR-2010-1067 [DOI] [PubMed] [Google Scholar]
- 15. Hansson T, Jensen I. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 6. sickness absence due to back and neck disorders. Scand J Public Health Suppl 2004;63:109–51. 10.1080/14034950410021862 [DOI] [PubMed] [Google Scholar]
- 16. Dekkers-Sánchez PM, Hoving JL, Sluiter JK, et al. . Factors associated with long-term sick leave in sick-listed employees: a systematic review. Occup Environ Med 2008;65:153–7. 10.1136/oem.2007.034983 [DOI] [PubMed] [Google Scholar]
- 17. Iles RA, Davidson M, Taylor NF. Psychosocial predictors of failure to return to work in non-chronic non-specific low back pain: a systematic review. Occup Environ Med 2008;65:507–17. 10.1136/oem.2007.036046 [DOI] [PubMed] [Google Scholar]
- 18. Josephson M, Heijbel B, Voss M, et al. . Influence of self-reported work conditions and health on full, partial and no return to work after long-term sickness absence. Scand J Work Environ Health 2008;34:430–7. 10.5271/sjweh.1289 [DOI] [PubMed] [Google Scholar]
- 19. Gustafsson K, Lundh G, Svedberg P, et al. . Psychological factors are related to return to work among long-term sickness absentees who have undergone a multidisciplinary medical assessment. J Rehabil Med 2013;45:186–91. 10.2340/16501977-1077 [DOI] [PubMed] [Google Scholar]
- 20. Steenstra IA, Verbeek JH, Heymans MW, et al. . Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med 2005;62:851–60. 10.1136/oem.2004.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Heymans MW, de Vet HC, Knol DL, et al. . Workers' beliefs and expectations affect return to work over 12 months. J Occup Rehabil 2006;16:685–95. 10.1007/s10926-006-9058-8 [DOI] [PubMed] [Google Scholar]
- 22. Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you'll do? A systematic review of the evidence for a relation between patients' recovery expectations and health outcomes. CMAJ 2001;165:174–9. [PMC free article] [PubMed] [Google Scholar]
- 23. Burdorf A, Naaktgeboren B, Post W. Prognostic factors for musculoskeletal sickness absence and return to work among welders and metal workers. Occup Environ Med 1998;55:490–5. 10.1136/oem.55.7.490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Linton SJ. Occupational psychological factors increase the risk for back pain: a systematic review. J Occup Rehabil 2001;11:53–66. 10.1023/A:1016656225318 [DOI] [PubMed] [Google Scholar]
- 25. Dunstan DA, MacEachen E. Bearing the brunt: co-workers' experiences of work reintegration processes. J Occup Rehabil 2013;23:44–54. 10.1007/s10926-012-9380-2 [DOI] [PubMed] [Google Scholar]
- 26. Alexopoulos EC, Konstantinou EC, Bakoyannis G, et al. . Risk factors for sickness absence due to low back pain and prognostic factors for return to work in a cohort of shipyard workers. Eur Spine J 2008;17:1185–92. 10.1007/s00586-008-0711-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gouttebarge V, Kuijer PP, Wind H, et al. . Criterion-related validity of functional capacity evaluation lifting tests on future work disability risk and return to work in the construction industry. Occup Environ Med 2009;66:657–63. 10.1136/oem.2008.042903 [DOI] [PubMed] [Google Scholar]
- 28. Hagen EM, Svensen E, Eriksen HR. Predictors and modifiers of treatment effect influencing sick leave in subacute low back pain patients. Spine 2005;30:2717–23. 10.1097/01.brs.0000190394.05359.c7 [DOI] [PubMed] [Google Scholar]
- 29. Steenstra IA, Ibrahim SA, Franche RL, et al. . Validation of a risk factor-based intervention strategy model using data from the readiness for return to work cohort study. J Occup Rehabil 2010;20:394–405. 10.1007/s10926-009-9218-8 [DOI] [PubMed] [Google Scholar]
- 30. Alexanderson KA, Borg KE, Hensing GK. Sickness absence with low-back, shoulder, or neck diagnoses: an 11-year follow-up regarding gender differences in sickness absence and disability pension. Work 2005;25:115–24. [PubMed] [Google Scholar]
- 31. Storheim K, Brox JI, Holm I, et al. . Predictors of return to work in patients sick listed for sub-acute low back pain: a 12-month follow-up study. J Rehabil Med 2005;37:365–71. 10.1080/16501970510040344 [DOI] [PubMed] [Google Scholar]
- 32. Eshøj P, Jepsen JR, Nielsen CV. Long-term sickness absence - risk indicators among occupationally active residents of a danish county. Occup Med 2001;51:347–53. 10.1093/occmed/51.5.347 [DOI] [PubMed] [Google Scholar]
- 33. Allebeck P, Mastekaasa A. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 5. risk factors for sick leave - general studies. Scand J Public Health Suppl 2004;63:49–108. 10.1080/14034950410021853 [DOI] [PubMed] [Google Scholar]
- 34. Borg K, Hensing G, Alexanderson K. Risk factors for disability pension over 11 years in a cohort of young persons initially sick-listed with low back, neck, or shoulder diagnoses. Scand J Public Health 2004;32:272–8. 10.1080/14034940310019524 [DOI] [PubMed] [Google Scholar]
- 35. Fritz JM, Wainner RS, Hicks GE. The use of nonorganic signs and symptoms as a screening tool for return-to-work in patients with acute low back pain. Spine 2000;25:1925–31. 10.1097/00007632-200008010-00010 [DOI] [PubMed] [Google Scholar]
- 36. Hartvigsen J, Lings S, Leboeuf-Yde C, et al. . Psychosocial factors at work in relation to low back pain and consequences of low back pain; a systematic, critical review of prospective cohort studies. Occup Environ Med 2004;61:e2. [PMC free article] [PubMed] [Google Scholar]
- 37. Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res 2012;22:1435–43. 10.1177/1049732312452938 [DOI] [PubMed] [Google Scholar]
- 38. Wasiak R, Young AE, Roessler RT, et al. . Measuring return to work. J Occup Rehabil 2007;17:766–81. 10.1007/s10926-007-9101-4 [DOI] [PubMed] [Google Scholar]
- 39. Hayden JA, Côté P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med 2006;144:427–37. 10.7326/0003-4819-144-6-200603210-00010 [DOI] [PubMed] [Google Scholar]
- 40. Gold JE, Hallman DM, Hellström F, et al. . Systematic review of biochemical biomarkers for neck and upper-extremity musculoskeletal disorders. Scand J Work Environ Health 2016;42:103–24. 10.5271/sjweh.3533 [DOI] [PubMed] [Google Scholar]
- 41. Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol 2007;17:643–53. 10.1016/j.annepidem.2007.03.013 [DOI] [PubMed] [Google Scholar]
- 42. Busch H, Göransson S, Melin B. Self-efficacy beliefs predict sustained long-term sick absenteeism in individuals with chronic musculoskeletal pain. Pain Pract 2007;7:234–40. 10.1111/j.1533-2500.2007.00134.x [DOI] [PubMed] [Google Scholar]
- 43. Okurowski L, Pransky G, Webster B, et al. . Prediction of prolonged work disability in occupational low-back pain based on nurse case management data. J Occup Environ Med 2003;45:763–70. 10.1097/01.jom.0000079086.95532.e9 [DOI] [PubMed] [Google Scholar]
- 44. Opsahl J, Eriksen HR, Tveito TH. Do expectancies of return to work and Job satisfaction predict actual return to work in workers with long lasting LBP? BMC Musculoskelet Disord 2016;17:481 10.1186/s12891-016-1314-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Heiden M, Mathiassen SE, Garza J, et al. . A comparison of two strategies for building an exposure prediction Model. Ann Occup Hyg 2016;60:74–89. 10.1093/annhyg/mev072 [DOI] [PubMed] [Google Scholar]
- 46. Berglind H, Gerner U. Motivation and return to work among the long-term sicklisted: an action theory perspective. Disabil Rehabil 2002;24:719–26. 10.1080/09638280210124301 [DOI] [PubMed] [Google Scholar]
- 47. Gallagher RM, Williams RA, Skelly J, et al. . Workers' Compensation and return-to-work in low back pain. Pain 1995;61:299–307. 10.1016/0304-3959(94)00190-P [DOI] [PubMed] [Google Scholar]
- 48. Schultz IZ, Crook J, Berkowitz J, et al. . Predicting return to work after low back injury using the Psychosocial risk for Occupational Disability Instrument: a validation study. J Occup Rehabil 2005;15:365–76. 10.1007/s10926-005-5943-9 [DOI] [PubMed] [Google Scholar]
- 49. Du Bois M, Szpalski M, Donceel P. Patients at risk for long-term sick leave because of low back pain. Spine J 2009;9:350–9. 10.1016/j.spinee.2008.07.003 [DOI] [PubMed] [Google Scholar]
- 50. Gross DP, Battié MC, Cassidy JD. The prognostic value of functional capacity evaluation in patients with chronic low back pain: part 1: timely return to work. Spine 2004;29:914–9. 10.1097/00007632-200404150-00019 [DOI] [PubMed] [Google Scholar]
- 51. Gross DP, Battié MC. Work-related recovery expectations and the prognosis of chronic low back pain within a workers' compensation setting. J Occup Environ Med 2005;47:428–33. 10.1097/01.jom.0000158706.96994.a5 [DOI] [PubMed] [Google Scholar]
- 52. Hansson E, Hansson T, Jonsson R. Predictors for work ability and disability in men and women with low-back or neck problems. Eur Spine J 2006;15:780–93. 10.1007/s00586-004-0863-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kuijer PP, Gouttebarge V, Wind H, et al. . Prognostic value of self-reported work ability and performance-based lifting tests for sustainable return to work among construction workers. Scand J Work Environ Health 2012;38:600–3. 10.5271/sjweh.3302 [DOI] [PubMed] [Google Scholar]
- 54. Schultz IZ, Crook J, Meloche GR, et al. . Psychosocial factors predictive of occupational low back disability: towards development of a return-to-work model. Pain 2004;107:77–85. 10.1016/j.pain.2003.09.019 [DOI] [PubMed] [Google Scholar]
- 55. van der Giezen AM, Bouter LM, Nijhuis FJ. Prediction of return-to-work of low back pain patients sicklisted for 3-4 months. Pain 2000;87:285–94. 10.1016/S0304-3959(00)00292-X [DOI] [PubMed] [Google Scholar]
- 56. Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J 2003;12:149–65. 10.1007/s00586-002-0508-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Johansson H, Weinehall L, Emmelin M. "It depends on what you mean": a qualitative study of Swedish health professionals' views on health and health promotion. BMC Health Serv Res 2009;9:191 10.1186/1472-6963-9-191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Heijbel B, Josephson M, Jensen I, et al. . Return to work expectation predicts work in chronic musculoskeletal and behavioral health disorders: prospective study with clinical implications. J Occup Rehabil 2006;16:169–80. 10.1007/s10926-006-9016-5 [DOI] [PubMed] [Google Scholar]
- 59. Schaafsma FG, Whelan K, van der Beek AJ, et al. . Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev 2013;8:CD001822 10.1002/14651858.CD001822.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Linton SJ, Halldén K. Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin J Pain 1998;14:209–15. 10.1097/00002508-199809000-00007 [DOI] [PubMed] [Google Scholar]
- 61. Shaw WS, Pransky G, Fitzgerald TE. Early prognosis for low back disability: intervention strategies for health care providers. Disabil Rehabil 2001;23:815–28. [DOI] [PubMed] [Google Scholar]
- 62. Crook J, Milner R, Schultz IZ, et al. . Determinants of occupational disability following a low back injury: a critical review of the literature. J Occup Rehabil 2002;12:277–95. 10.1023/A:1020278708861 [DOI] [PubMed] [Google Scholar]
- 63. Verkerk K, Luijsterburg PA, Miedema HS, et al. . Prognostic factors for recovery in chronic nonspecific low back pain: a systematic review. Phys Ther 2012;92:1093–108. 10.2522/ptj.20110388 [DOI] [PubMed] [Google Scholar]
- 64. Pincus T, Vogel S, Burton AK, et al. . Fear avoidance and prognosis in back pain: a systematic review and synthesis of current evidence. Arthritis Rheum 2006;54:3999–4010. 10.1002/art.22273 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-014939supp001.pdf (183.3KB, pdf)
bmjopen-2016-014939supp002.pdf (82.7KB, pdf)