Abstract
Objectives:
The aim of this study was to determine the respective contribution of professional characteristics, team attributes, team processes, and team emergent states on the job satisfaction of 315 mental health professionals from Quebec (Canada).
Methods:
Job satisfaction was measured with the Job Satisfaction Survey. Independent variables were organized into four categories according to a conceptual framework inspired from the Input-Mediator-Outcomes-Input Model. The contribution of each category of variables was assessed using hierarchical regression analysis.
Results:
Variations in job satisfaction were mostly explained by team processes, with minimal contribution from the other three categories. Among the six variables significantly associated with job satisfaction in the final model, four were team processes: stronger team support, less team conflict, deeper involvement in the decision-making process, and more team collaboration. Job satisfaction was also associated with nursing and, marginally, male gender (professional characteristics) as well as with a stronger affective commitment toward the team (team emergent states).
Discussion and Conclusion:
Results confirm the importance for health managers of offering adequate support to mental health professionals, and creating an environment favorable to collaboration and decision-sharing, and likely to reduce conflicts between team members.
Keywords: Mental health professionals, job satisfaction, team processes, team emergent states, team attributes, professional’s characteristics
Mental health work is acknowledged to be more stressful than that in other medical fields.1 Mental health professionals have to cope with difficult patients,2 including some with multiple mental and substance use disorders who might be more aggressive or violent and present suicidal behaviors,3–6 thus requiring vast amounts of time and energy from several resources. Moreover, mental health professionals are often exposed to criticism from relatives of individuals with mental disorders7 while, at the same time, undergoing organizational and administrative constraints.1,4 Mental health work is also less valued and more stigmatizing than work in other health fields.8,9 Several studies have found that psychiatrists and other mental health professionals were particularly exposed to burnout, drug/alcohol abuse, and suicide.10 Similarly, mental health nursing is considered more stressful than other specialties, which may explain the shortage of mental health nurses.11 Due to their difficult work conditions, mental health professionals are thus particularly affected by any change in the mental healthcare system.12,13
In the last decade, most industrial countries have reformed their mental healthcare system to reduce costs and increase effectiveness. These reforms have encouraged the shift from psychiatric hospital to more community-based services. While teamwork has a long history in mental health, most recent reforms encouraged greater collaboration between mental health service providers and professionals from diverse disciplines. For example, as part of the 2005 global reform of its healthcare system, the Quebec government merged several general hospitals, community local health centers, and nursing homes, thus creating 95 health and social services centers (HSSCs) mandated to coordinate health services within their respective local health service networks. Primary care mental teams were set up in each HSSC, which involved transferring professionals from specialized mental health services, others who had previously worked in community local health centers, and newcomers. The Quebec mental health reform also promoted teamwork, especially the endorsement of shared care initiatives involving psychiatrists and general practitioners. These changes had a major impact on mental health professionals’ practices because they have brought uncertainty.2 Mental health professionals transferred from specialized services to mental health primary care units had to deal with scarcer resources.14 Teamwork also implies a certain loss of professional autonomy, with implications for possible role ambiguity among professionals as well as heightened stress15 and interpersonal friction.13
While mental health reforms have focused on improving recovery and satisfaction among individuals with mental disorders,16 it is also essential to consider job satisfaction among mental health professionals. There are several definitions of job satisfaction, but it is usually recognized as a positive emotional state that a worker has about their job or work experience.17 In addition to this emotional feeling, job satisfaction depends on the fulfillment of the worker’s needs.18,19 Job satisfaction is in fact a subjective comparison between the wants or expectations of a worker and the reality he or she faces,18,20 and between the rewards that a worker receives for their work versus the rewards they feel they should receive.11 Job satisfaction includes several aspects, such as working conditions, remuneration, advancement possibilities, and the quality of supervision and relationships with co-workers.20 In addition to being essential to the health and well-being of professionals, job satisfaction is strongly associated with quality21,22 and continuity of services, which allows the establishment of an effective therapeutic relationship that ensures recovery of patients. Contented professionals are more likely to stay with their team.23 Conversely, disaffected professionals may tend to harbor negative feelings toward the clientele2 and be absent or leave prematurely24 due to burnout.25 Job satisfaction is also among key outcomes of teamwork in the health field.24,26
Most studies on job satisfaction have focused on only one group of professionals (usually nurses or social workers) rather than the broad range of professions in the mental health field. Moreover, no study has considered the perceived job satisfaction among mental health professionals working in diversified local health services networks, including both primary and specialized care. Job satisfaction is as much the object of quantitative and qualitative studies, which explains the wide range of independent variables (IVs) assessed in those studies. Often, job satisfaction is assessed together with factors associated with job dissatisfaction, that is, stress, burnout, turnover, or intent to leave, which explains the broad interest in personality traits (e.g. hardiness, self-esteem, emotional intelligence, and resilience) of the professionals.9,18,27–30
Job satisfaction is related to professional characteristics, relationships with team members, and expectations of mental health professionals regarding their workplace and organization.7 Various models have described categories of variables associated with job satisfaction. According to Herzberg et al.’s31 motivation-hygiene theory, job satisfaction and job dissatisfaction each depend on distinct factors. While satisfaction could be associated with factors intrinsically related to the work (i.e. motivators such as challenging work, recognition, and opportunity of personal achievement), dissatisfaction might be associated with extrinsic factors such as salary, benefits, and interpersonal relations.11 Another popular model in the health field is the Input-Process-Output (IPO) Model,32 which holds that outputs such as job satisfaction are influenced by inputs (e.g. team composition and organizational culture) and mediating processes (e.g. communication and coordination). Inputs include organizational, team, and individual resources; processes refer to actions performed by team members; and outputs are outcomes resulting from inputs and processes.33 Using this model, Korner et al.26 found an association between organizational culture and job satisfaction, mediated by interprofessional teamwork. The Input-Mediator-Outcomes-Input (IMOI) Model,34 comprising professional characteristics, team attributes, team processes, and team emergent states, that we have used in this study is derived from the IPO model. A particularity of the former is that it makes a distinction among mediators between team processes (i.e. conditions affecting teamwork such as group support or interdependence) and team emergent states (i.e. motivations such as trust among staff members or affective commitment toward the group).35 Another characteristic of the IMOI Model is that the influence of one category on another is not linear but cyclical: outcomes may become inputs.34 In the IMOI Model, professional characteristics (e.g. age and type of profession) and team attributes (e.g. composition and setting) thus influence team processes and team emergent states which, in turn, have an impact on job satisfaction and other outcomes, and the latter may then influence inputs and mediators.
Regarding professional characteristics that may be included in the IMOI Model, several studies have found a negative association between job satisfaction and some professions. In the mental health sector, job satisfaction was lower among nurses,36 social workers,3,37 and other professionals,24 as opposed to physicians or psychologists.38 Other studies have identified links between job satisfaction and professional characteristics such as age and length of experience,39 with younger professionals being more likely to be dissatisfied and leave their job.8,38 The association between job satisfaction and a specific gender is not as clear. Regarding team attributes, a shortage of professionals may result in heavier caseloads and thus contribute indirectly to lower job satisfaction.36 Another factor is the work setting: studies have found, for example, that nurses in forensic services were happier in their job than those working in other mental health services.40 Considering that some mental disorders (e.g. personality disorders) have been reported as more stressful than others,41 it is possible that job satisfaction is also more likely associated with certain clienteles. Furthermore, job satisfaction has been reported to be associated with several team processes such as collaboration,3 autonomy,42 involvement in decision-making,40 support from the organization and from supervisors and co-workers,41 informational self-efficacy,43 fewer team conflicts,40,44 and recovery-oriented services.45 Considering that knowledge-sharing promotes competence,46 we may presume that an association exists between this team process and job satisfaction. Furthermore, familiarity between co-workers and team interdependence are probably linked indirectly with team support and thus with job satisfaction. Links have also been found between job satisfaction and some emergent states such as trust,40,47 affective commitment toward the team,40,47 and team climate.36,40,47 Since an adequate work role performance helps to clarify the respective role of each team member,48 it is probable that this team process influences job satisfaction. Finally, the link between belief in the advantages of interdisciplinary collaboration and job satisfaction has not yet been assessed in the literature. However, it seems logical to think that this belief may help reduce team conflicts.
To our knowledge, the IMOI Model has not been used previously to assess job satisfaction in the health field in general or in mental health more particularly. Moreover, the relative contribution of professional characteristics, team attributes, team processes, and team emergent states on job satisfaction among mental health professionals has not yet been investigated. Hierarchical regression analysis is an advantageous method to assess the contribution of these various categories of variables in explaining variance in job satisfaction.This study thus aims to identify variables associated with job satisfaction among 315 mental health professionals working in four local health service networks in the province of Quebec (Canada) and to assess the relative contributions of professional characteristics and team attributes (i.e. inputs), team processes, and team emergent states (mediators) to job satisfaction (output). Under the IMOI Model, mediators would affect more directly job satisfaction than inputs. In consequence, we hypothesized that team processes and team emergent state variables would be the variables having the greatest influence on job satisfaction.
Methods
Study design, sample, and data collection
This study came on the heels of a major reform of the mental healthcare system in Quebec (Canada), which implemented mental health teams within primary care services and promoted greater collaboration between primary care and specialized mental health services. In Canada, healthcare delivery is mainly public and managed by provincial governments. Health and social services networks in Quebec are grouped under the same government department and administered under nine service programs including mental health. The Quebec Ministry of Health and Social Services is responsible for healthcare, which is provided freely for the most part. Between 2005 and 2015, Health and Social Service Centers (HSSCs, n = 95) were mandated to provide quality care in their respective local health service networks. Mental health services include specialized services offered in psychiatric hospitals or general hospitals and primary care delivered by medical clinics, psychologists in private practices, community-based organizations, or self-help groups (e.g. crisis centers).
The study included mental health professionals from four local healthcare service networks in Quebec (Canada) chosen because of their differences in terms of geography (e.g. urban or semi-urban) and services offered (e.g. presence or not of a psychiatric hospital). Team supervisors (or managers), composed of mental health professionals previously identified by an advisory committee of representatives from the four local health service networks, provided a list of potential study participants. Participant professionals had to be members of a public specialized service team or mental health primary care team, which included at least three professionals from at least two disciplines (e.g. nursing and social work).
Data were collected between May 2013 and June 2014. A total of 466 mental health professionals were approached to respond to a questionnaire that comprised standardized scales and questions on their socio-professional characteristics. The study also recruited 41 team managers who were supervisors of the professionals participating in the study. Managers answered a different questionnaire covering five aspects: (1) patient characteristics, (2) team characteristics, (3) clinical activities, (4) network integration strategies, and (5) frequency and satisfaction of interactions with network teams/organizations. Only the two first aspects were treated in this study. The advisory committee validated instruments and facilitated data collection. The research ethics board of a mental health university institute approved the study protocol.
Variables, conceptual framework, and instruments
The dependent variable (DV) “Job Satisfaction” was assessed using the Job Satisfaction Survey,49 a 20-item scale assessing five sub-elements (supervision, contingent reward, operating procedures, co-workers, and nature of the work). As remuneration is regulated by the Quebec government, items dealing with this aspect were not considered in this study. Cronbach’s alpha in this study varied between 0.63 (co-workers) and 0.77 (contingent reward).
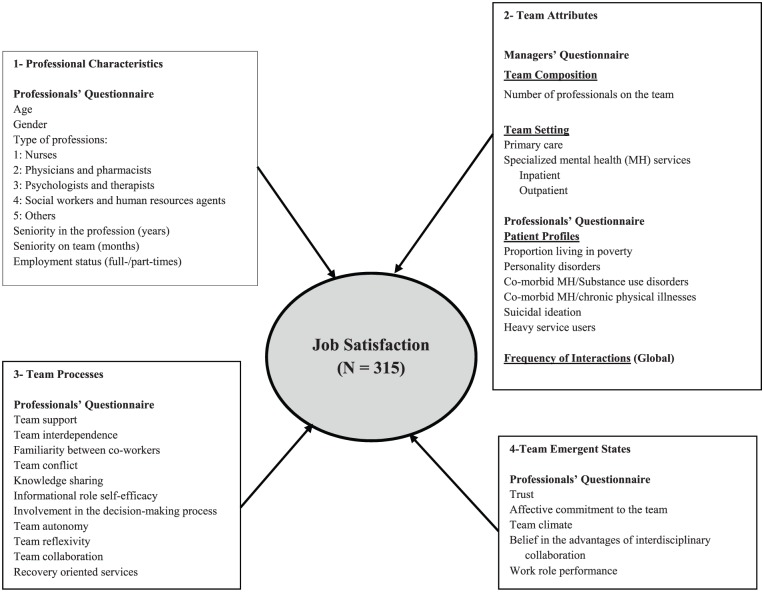
A conceptual framework based on the IMOI Model34 and the literature on job satisfaction guided the analysis (Figure 1). IVs were classified into four categories: (1) professional characteristics, (2) team attributes, (3) team processes, and (4) team emergent states. Six variables from the professionals’ questionnaire covered professional characteristics: age, gender, type of profession (nurses, physicians/pharmacists, psychologists/therapists, social workers/human resources agents, and others), seniority in the profession, seniority on the team, and employment status (full- or part-time). Team attributes included one variable (frequency of interactions) from the professionals’ questionnaire and three from the managers’ questionnaire. The latter were (1) team composition, (2) work setting (primary care, specialized inpatient mental health services, and specialized outpatient mental health services), and (3) patient profiles (proportion living in poverty, heavy service users, and various case histories comprising personality disorders, co-morbid mental and substance use disorders, co-morbid mental disorders and chronic physical illnesses, and suicidal ideation).
Figure 1.
Conceptual framework.
Team processes figuring in the conceptual framework were assessed using 11 standardized scales, while five others were used for team emergent states (Table 1). Due to the large number of variables covered by the study, the shortest standardized scales were prioritized. All standardized scales were translated and validated in French, except for three (team collaboration, informational self-efficacy, and belief in the advantages of interdisciplinary collaboration) that were originally in French.
Table 1.
Description of standardized instruments included in the study.
| Measures and references | Description | Cronbach’s alpha coefficients from their original validation |
|---|---|---|
| Dependent variable | ||
| Job satisfaction49 | 20 items; 5 sub-dimensions | 0.90 |
| Independent variables | ||
| For team processes | ||
| Team support50 | 4 items | 0.84–0.85 |
| Team interdependence51 | 20 items | 0.77–0.88 |
| Familiarity between co-workers52 | 5 items | 0.78–0.88 |
| Team conflict53 | 9 items | 0.93–0.94 |
| Knowledge sharing54 | 5 items | 0.93 |
| Informational role self-efficacy55 | 5 items | 0.93 |
| Involvement in decision-making process56 | 3 items | 0.88 |
| Team autonomy56 | 3 items | 0.76 |
| Team reflexivity57 | 3 items | 0.79 |
| Collaboration58 | 14 items | 0.77–0.91 |
| Recovery Orientation59 | 32 items; 5 sub-dimensions | 0.76–0.90 |
| For team emergent states | ||
| Trust60 | 4 items | 0.90 |
| Affective commitment toward the team61 | 5 items | 0.86–0.92 |
| Team climate62 | 19 items; 4 sub-dimensions | 0.60–0.84 |
| Belief in interdisciplinary collaboration63 | 5 items | 0.92 |
| Work role performance64 | 18 items | 0.90 |
Analyses
Preliminary analyses
Analyses were conducted using SPSS 24th edition. First, the database was screened for outliers and missing values, and the latter was treated using multiple imputation techniques. This method consists of running multiple sets of regression analyses with variables pertaining to the same category (e.g. socio-demographic variables), ending up with the most likely response the participant could have given in place of the missing data, considering that they had responded in a given way to other questions. The frequency distribution of categorical variables and central tendency measures (means and standard deviations) for continuous variables were calculated. The DV was normally distributed (skewness: –0.037; kurtosis: 0.332).
Multi-level analysis
In view of the nested nature of variables, analyses were performed to assess the need for considering the contextual level (i.e. teams) above the individual level. The intra-class correlation was gauged to determine homogeneity within teams and heterogeneity between teams. Using maximum likelihood estimation with random effects, the significance of clustering at team level was estimated by means of the Wald Z test.
Hierarchical regression analysis
Associations between the DV and each IV were assessed separately using analysis of variance (ANOVA) and t-test, with alpha set at 0.10. The IVs that were found to have a significant association with the DV were used to build the hierarchical linear regression model, with alpha set at 0.05. The four blocks of variables presented in Figure 1 were entered successively to assess the individual contribution of each set of variables within the block and, more importantly, to estimate the contribution of the last model after all previously introduced variables were controlled. For the first block, the backward elimination technique was used so that only variables significantly associated with the DV were retained in the model, using an alpha of 0.10 for elimination. For the second model, variables significantly associated with the DV in the first model were introduced by the forced entry method, and variables pertaining to the second block were introduced using backward elimination. Successive rounds of variables were introduced similarly using the forced entry and backward elimination techniques to build the third and fourth models. Explained variance was estimated for each model, along with the goodness of fit (ANOVA F test and p-value).
Results
Sample
A total of 315 mental health professionals, out of the 466 approached, took part in the study, for a response rate of 68%. No significant differences were found between participants and non-participants with respect to distribution for type of team (χ2 (1, N = 466) = 0.79; p = 0.68) and gender (χ2 (1, N = 466) = 0.03; p = 0.87). Regarding socio-demographic profile, the mean age of participants was 43, with a larger proportion of women (70%) than men. Nurses were the most common profession (30%), followed by social workers and human resources agents (27%), psychologists and therapists (22%), and other mental health professionals (17%). Average seniority was 9 years within the profession and 3 years within the team. Most mental health professionals were working full-time (78%). Finally, almost a third of participants worked on primary care teams (32%), whereas more than half belonged to outpatient specialized care teams (56%) and the remainder to inpatient specialized care teams (12%). As regards patients taken on by mental health professionals, 37% suffered from severe mental health disorders (bipolar disorder and other psychoses), 21% had personality disorders, and 20% had experienced suicidal ideation. These participant characteristics and others are detailed in Table 2.
Table 2.
Descriptive statistics (N = 315).
| Min | Max | N/Mean | %/SD | |||
|---|---|---|---|---|---|---|
| 1. Professional characteristics | Age | 24.0 | 68.0 | 43.3 | 10.5 | |
| Gender | Female | 219 | 69.5 | |||
| Males | 96 | 30.5 | ||||
| Professions | Nurses | 94 | 29.8 | |||
| Physicians and pharmacists | 15 | 4.8 | ||||
| Psychologists and therapists | 68 | 21.6 | ||||
| Social workers and human resources agents | 85 | 27.0 | ||||
| Other mental health professionals | 53 | 16.8 | ||||
| Seniority in the profession (in years) | 0.0 | 38.0 | 9.0 | 10.8 | ||
| Seniority on team (in years) | 0.0 | 27.0 | 3.1 | 4.6 | ||
| Employment status | Full-time | 246 | 78.1 | |||
| Part-time | 69 | 21.9 | ||||
| 2. Team attributes | Clientele | Personality disorders | 2.0 | 90.0 | 30.6 | 21.3 |
| Co-morbid mental health/chronic physical illnesses | 2.0 | 93.0 | 34.4 | 21.6 | ||
| Suicidal ideation | 0.0 | 95.0 | 27.9 | 19.9 | ||
| Heavy service users | 0.0 | 90.0 | 26.0 | 24.0 | ||
| Severe mental health disorders (bipolar disorder and other psychoses) | 2.0 | 149.9 | 66.9 | 37.2 | ||
| Team setting | Primary healthcare | 101 | 32.1 | |||
| Outpatient specialized healthcare | 176 | 55.9 | ||||
| Inpatient specialized healthcare | 38 | 12.1 | ||||
| Number of professionals on the team | 1.0 | 16.0 | 8.0 | 3.5 | ||
| Proportion living in poverty | 5.0 | 23.3 | 14.2 | 8.1 | ||
| Frequency of interactions | 32.0 | 204.0 | 95.4 | 31.3 | ||
| 3. Team processes | Team support | 1.0 | 7.0 | 4.8 | 1.2 | |
| Team interdependence | 4.6 | 20.7 | 13.7 | 3.1 | ||
| Familiarity between co-workers | 1.6 | 7.0 | 5.4 | 0.9 | ||
| Team conflict | 3.0 | 21.0 | 9.0 | 2.9 | ||
| Knowledge sharing | 1.8 | 7.0 | 5.7 | 0.9 | ||
| Informational role self-efficacy | 16.0 | 100.0 | 81.1 | 14.4 | ||
| Involvement in decision process | 1.0 | 7.0 | 5.0 | 1.4 | ||
| Team autonomy | 1.0 | 7.0 | 4.9 | 1.3 | ||
| Team reflexivity | 1.0 | 7.0 | 4.6 | 1.2 | ||
| Team collaboration | 8.5 | 28.0 | 19.3 | 3.8 | ||
| Recovery-oriented services | 2.2 | 6.8 | 5.1 | 0.7 | ||
| 4. Team emergent states | Trust | 1.0 | 7.0 | 5.2 | 1.2 | |
| Affective commitment toward the team | 1.0 | 7.0 | 4.9 | 1.2 | ||
| Team climate | 7.9 | 27.8 | 20.5 | 3.4 | ||
| Belief in the advantages of interdisciplinary collaboration | 3.0 | 7.0 | 6.2 | 0.7 | ||
| Work role performance | 23.7 | 42.0 | 34.6 | 3.3 | ||
| Job satisfaction | 11.3 | 35.0 | 24.8 | 3.6 | ||
SD: standard deviation.
Attempt to run multi-level analysis
The 315 mental health professionals came from 49 teams, which had an average of six members (ranging from 3 to 16) and represented nine different healthcare groups. Specialized service groups thus comprised hospital units, day hospitals, assertive community treatment programs, outpatient clinics, and rehabilitation programs. Primary care groups included mental health evaluation units and treatment teams, as well psychosocial basic teams, and intensive case management programs. An average of 35 professionals (ranging from 30 to 55) worked in each group. Intra-class correlation was calculated on variables of interest and was found to be elevated (83.9%). The effect of clustering was then calculated using a maximum likelihood ratio with random effects and was found to be non-significant (Wald Z = 1.377; p = 168), meaning that the nested nature of the data into group types did not bring a plus value to the individual level model.
Hierarchical regression analysis
Table 3 presents variables found to be significantly associated with the DV in bivariate analyses. The four blocks of variables presented in Table 3 were entered consecutively in the regression modeling presented in Table 4. From Block 1, professional characteristics, the variables gender and professions were retained in the model after backward elimination. Males were found to be positively associated and nurses negatively associated. The second block, team attributes, maintained only one variable: the proportion of personality disorders among patients, negatively related to job satisfaction. The third block, team processes, retained four variables. Three of them, that is, team collaboration, team support, and involvement in the decision-making process, were positively associated, while team conflict had a negative association. The fourth block, team emergent states, retained only one variable: affective commitment toward the team, which was positively associated. Along with the latter, three previously entered variables were retained and were positively associated: team collaboration, team support, and involvement in the decision-making process (team processes). Two variables were negatively associated: nursing profession (professional characteristics) and team conflict (team processes). Finally, a variable was positively, but marginally, associated: male gender (professional characteristics). As shown in the last two columns of Table 4, no collinearity was found between variables in this regression model. The predictive value of the model was strong (ANOVA: F = 33.300; p < 0.001). The total variance explained by variables in the model was excellent at 47%.
Table 3.
Variables associated with job satisfaction among mental health professionals: bivariate analyses (N = 315).
| Standardized coefficients |
t | Significance | |||
|---|---|---|---|---|---|
| Beta | |||||
| 1. Professional characteristics | Gender | Males | 0.125 | 2.221 | 0.027 |
| Professions | Nurses | −0.114 | −2.021 | 0.044 | |
| Physicians and pharmacists | 0.113 | 2.012 | 0.045 | ||
| 2. Team attributes | Clientele | Personality disorders | −0.127 | −2.268 | 0.024 |
| Co-morbid mental health/chronic physical illnesses | 0.112 | 1.987 | 0.048 | ||
| Type of care | Inpatient specialized care | 0.098 | 1.748 | 0.081 | |
| 3. Team processes | Team support | 0.486 | 9.841 | <0.001 | |
| Team interdependence | 0.238 | 4.333 | <0.001 | ||
| Familiarity between co-workers | 0.188 | 3.387 | 0.001 | ||
| Team conflict | −0.380 | −7.267 | <0.001 | ||
| Knowledge sharing | 0.281 | 5.186 | <0.001 | ||
| Informational role self-efficacy | 0.160 | 2.873 | 0.004 | ||
| Involvement in decision-making process | 0.461 | 9.181 | <0.001 | ||
| Team autonomy | 0.233 | 4.236 | <0.001 | ||
| Team reflexivity | 0.313 | 5.835 | <0.001 | ||
| Team collaboration | 0.492 | 9.990 | <0.001 | ||
| Recovery-oriented services | 0.357 | 6.769 | <0.001 | ||
| 4. Team emergent states | Trust | 0.392 | 7.546 | <0.001 | |
| Affective commitment toward the team | 0.415 | 8.059 | <0.001 | ||
| Team climate | 0.529 | 11.031 | <0.001 | ||
| Belief in the advantages of interdisciplinary collaboration | 0.276 | 5.079 | <0.001 | ||
| Work role performance | 0.333 | 6.239 | <0.001 | ||
Table 4.
Variables associated with job satisfaction among mental health professionals: hierarchical linear regression model (N = 315).
| Model 1: professional characteristics |
Model 2: team attributes |
Model 3: team processes |
Model 4: team emergent states |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SC β | p | SC β | p | SC β | t | p | 95.0% CI for β |
Collinearity statistics |
|||||
| Lower bound | Upper bound | Tolerance | VIF | ||||||||||
| (Constant) | <0.001 | <0.001 | <0.001 | 13.277 | <0.001 | 13.795 | 18.596 | ||||||
| Gender (males) | 0.133 | 0.018 | 0.126 | 0.024 | 0.076 | 0.076 | 0.073 | 1.720 | 0.086 | −0.082 | 1.225 | 0.968 | 1.033 |
| Professions (nurses) | −0.122 | 0.029 | 0.134 | 0.017 | −0.122 | 0.005 | 0.119 | −2.807 | 0.005 | −1.590 | −0.279 | 0.975 | 1.026 |
| Ratio of personality disorders within the clientele | 0.132 | 0.018 | 0.001 | 0.986 | 0.010 | 0.220 | 0.826 | −0.013 | 0.016 | 0.922 | 1.085 | ||
| Team collaboration | 0.216 | <0.001 | 0.175 | 3.251 | 0.001 | 0.065 | 0.263 | 0.605 | 1.653 | ||||
| Team support | 0.259 | <0.001 | 0.260 | 5.404 | <0.001 | 0.508 | 1.091 | 0.756 | 1.323 | ||||
| Team conflict | −0.249 | <0.001 | 0.243 | −5.555 | <0.001 | −0.405 | −0.193 | 0.915 | 1.093 | ||||
| Involvement in decision-making process | 0.229 | <0.001 | 0.194 | 3.750 | <0.001 | 0.244 | 0.782 | 0.652 | 1.534 | ||||
| Affective commitment toward the team | 0.121 | 2.375 | 0.018 | 0.061 | 0.647 | 0.671 | 1.490 | ||||||
| Goodness of fit | |||||||||||||
| ANOVA: F | 4.889 | 5.190 | 36.697 | 33.300 | |||||||||
| ANOVA: p | 0.008 | 0.002 | <0.001 | <0.001 | |||||||||
| Total variance explained: R2 | 0.030 | 0.048 | 0.456 | 0.465 | |||||||||
CI: confidence interval; VIF: variance inflation factor; ANOVA: analysis of variance; SC β: standardized coefficient beta.
Discussion
The results partially confirm our hypothesis: job satisfaction was strongly associated with team processes but very little with team emergent states. The hierarchical model used for this study revealed that team processes contributed for 39% of the 47% variance explaining job satisfaction among mental health professionals, while there was minimal influence from professional characteristics, team attributes, and team emergent states. Indeed, four of the six variables associated with job satisfaction in the final model were team processes: stronger team support, less team conflict, deeper involvement in decision-making, and closer team collaboration. Those results are consistent with previous studies that have found that team processes were significant predictors of job satisfaction.12 It confirms Kanter’s65 theory that job satisfaction is not so much the result of professional attributes, but rather of empowering structures,44 which suggests that creating favorable conditions in the workplace is essential to job satisfaction.12 Team support was the variable which contributed the most to job satisfaction among mental health professionals, which is coherent with the literature.12,36 This support may be material or emotional.66 Adequate support from supervisors and co-workers helps reduce the workload of team members,67 prevents burnout and the effects of emotional strain,27 improves staff retention,67 and promotes individual growth, and development among professionals.21 Mental health teams especially depend on proper support from supervisors to help them face challenges related to treatment and follow-up of patients with severe mental disorders.68 Even in challenging circumstances, mental health professionals can be committed to their job and respond more ably to problems when they sense that they are well supported within their workplace.12 Conversely, inadequate clinical supervision or support from co-workers increases feelings of incompetence,69 stress,30 and job dissatisfaction.70 A study of community mental health nurses found that those having less support from their manager also had more negative attitudes toward their patients.71
The negative association between team conflicts and job satisfaction has often been reported in the literature.72 Interpersonal frictions thus have the most detrimental effect on team effectiveness.73 Conflicts between team members are an important factor of burnout and turnover12 because they affect trust, collaboration, and team performance.74 Disputes may arise when there is ambiguity regarding the task of each professional during patient follow-up, which may hinder recovery.13 A team needs to learn to handle and solve conflicts48 in order to achieve desirable outcomes.75 Open dialog, negotiation, and compromise are characteristics of a well-functioning team.76
According to the literature, job satisfaction improves when workers are involved in decision-making.77,78 Conversely, professionals having less decisional power usually suffer from more stress30,79 and are less content with their work.12 Involvement in the decision-making process requires equality between team members76 as well as the recognition of their individual expertise. According to a study, nurses can maintain a safe personal boundary when they are allowed to make decisions autonomously.27
Team collaboration includes communication, synchronicity, and coordination (implicit and explicit) between members.58 Effective collaboration promotes trust among staff80 and reduces the risk of role ambiguity, which is strongly linked to task conflicts81 and job dissatisfaction.44 Improved collaboration allows a team to reach peak effectiveness.75 Nurses were the only participants whose professional status had a significant association with job satisfaction in the final model (i.e. negative association), which is consistent with the literature. Mental health nurses experienced major stress from frequent interaction with patients affected by severe problems.2 They were more at risk than other mental health professionals for exposure to violence or aggression from patients.8,82 Moreover, they must often navigate between conflicting expectations of patients, relatives, other professionals, and managers.4 Finally, other mental health professionals often failed to seek their opinions.76
The marginal association between job satisfaction and male gender may reflect the fact that men find it easier than women to reconcile the demands of their job and home activities.30 Yet, these results may also reflect the nature of our sample which consisted of relatively more men in higher status professions (e.g. psychiatrists and general practitioners), as opposed to predominantly women in lower status professions (e.g. nursing). Moreover, studies have found that “hardiness,” that is, an effective personality trait for resisting high levels of stress,83 was a protective factor against stress among nurses.30,82,84 One such study suggested that men working in nursing would demonstrate more hardiness than women.30
Regarding team attributes, it is noteworthy that the only variable associated with job satisfaction was the ratio of patients with personality disorders. Some studies have identified patients with borderline personality disorders as those representing the greatest challenge for the mental health practice.41 This clientele is characterized by self-destructive behaviors, impulsivity, instability, anger, crises, and suicide attempts41 and are acknowledged as heavy users of emergency services and other specialized mental health services.85,86 Antisocial personality disorders are also strongly associated with aggressive behaviors and criminality.5 However, the influence of personality disorders on job satisfaction was eliminated when variables related to team processes were introduced. Strong team and organizational support, collaboration and harmony among team members, and the opportunity for them to share in the decision-making process may help overcome the critical challenges posed by demanding clients. Furthermore, it was interesting to see that job satisfaction was not associated with the type of mental health team, as indicated by both bivariate and multi-level analyses.
Contrary to our hypothesis, team emergent states had the least influence on job satisfaction among mental health professionals. Those results seemed in opposition with Herzberg et al.’s31 motivation-hygiene theory holding that motivations would be the most important factor of job satisfaction. Although an association with job satisfaction was found in the bivariate analyses for each of the five variables from team emergent states, only affective commitment toward the team was included in the final model. It is possible that most emergent states (e.g. trust and work role performance) were in fact strongly related to team processes and therefore did not bring much more to the final model. Such commitment may also be dependent on team processes.14,76 Several studies report that social support fosters commitment among team members.7 Strong leadership is another factor promoting individual dedication and job satisfaction.35 Mental health professionals having a high affective commitment toward their team are less likely to quit.61 Moreover, they are more apt to make team values on their own and apply them in their daily practice.23 Previous studies have found an association between affective commitment toward the team and job satisfaction.22,40,87
Limitations
This study has some limitations. First, our data were cross-sectional. It is therefore impossible to determine whether IVs promoted job satisfaction or vice versa. Second, as our sample represented mental health professionals from various professions, care teams, and local health service networks, the results may not be generalized to other samples consisting of one specific profession or type of mental health team. Third, certain professions (e.g. physicians and pharmacists) and types of mental health teams (e.g. emergency department teams and inpatient care teams) were underrepresented in our study. Fourth, we did not have information on every variable identified in the literature in association with job satisfaction,24 for example, individual job-related variables such as benefits, and caseloads, or variables regarding personality traits (e.g. hardiness). Finally, organizational culture was not assessed in this study, even though certain types of organizational culture are thought to be associated with job satisfaction.
Conclusion
This study was innovative in assessing the respective contributions of professional characteristics, team attributes, team processes, and team emergent states on job satisfaction. It was also original in assessing job satisfaction among mental health professionals from several disciplines, team types, and local health service networks, with many variables classified within a conceptual framework based on the IMOI Model. The results show that job satisfaction among mental health professionals is more a function of team processes than professional characteristics, team attributes, or team emergent states. Those results have important clinical applications because mental health managers may encourage the implementation of positive team processes, globally and within each team. It confirms that it is essential for health managers to offer adequate support to mental health professionals; supervisors should also create an environment favorable to collaboration and decision-sharing and likely to reduce conflicts among staff. Interventions such as training programs and proactive supervisory support could be recommended to increase job satisfaction among mental health professionals and indirectly improve the quality of services offered to their patients.
Acknowledgments
The Fonds de recherche du Quebec Santé (FRQS) provided generous support for this study, which we would like to gratefully acknowledge. We also thank participants in the research, including the advisory committee and network respondents, members of the research team, and editorial assistants.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the Ethic Board of the Douglas Mental Health University Institute (MP-IUSMD-11-037).
Funding: The author(s) disclosed receipt ot the following financial support for the research, autorship and/or publication of this article: This study is supported by the Fonds de recherche du Québec Santé (FRQS).
Informed consent: Informed consent was obtained from all participants, each of whom signed a consent form.
References
- 1. Cottrell S. Occupational stress and job satisfaction in mental health nursing: focused interventions through evidence-based assessment. J Psychiatr Ment Health Nurs 2001; 8: 157–164. [DOI] [PubMed] [Google Scholar]
- 2. Melchior ME, Bours GJ, Schmitz P, et al. Burnout in psychiatric nursing: a meta-analysis of related variables. J Psychiatr Ment Health Nurs 1997; 4: 193–201. [DOI] [PubMed] [Google Scholar]
- 3. Onyett S. Revisiting job satisfaction and burnout in community mental health teams. J Ment Health 2011; 20: 198–209. [DOI] [PubMed] [Google Scholar]
- 4. Cleary M. The realities of mental health nursing in acute inpatient environments. Int J Ment Health Nurs 2004; 13: 53–60. [DOI] [PubMed] [Google Scholar]
- 5. Dickens G, Piccirillo M, Alderman N. Causes and management of aggression and violence in a forensic mental health service: perspectives of nurses and patients. Int J Ment Health Nurs 2013; 22: 532–544. [DOI] [PubMed] [Google Scholar]
- 6. Ward L. Mental health nursing and stress: maintaining balance. Int J Ment Health Nurs 2011; 20: 77–85. [DOI] [PubMed] [Google Scholar]
- 7. Hamaideh SH. Burnout, social support, and job satisfaction among Jordanian mental health nurses. Issues Ment Health Nurs 2011; 32: 234–242. [DOI] [PubMed] [Google Scholar]
- 8. Alsaraireh F, Quinn Griffin MT, Ziehm SR, et al. Job satisfaction and turnover intention among Jordanian nurses in psychiatric units. Int J Ment Health Nurs 2014; 23: 460–467. [DOI] [PubMed] [Google Scholar]
- 9. Rössler W. Stress, burnout, and job dissatisfaction in mental health workers. Eur Arch Psychiatry Clin Neurosci 2012; 262: S65–S69. [DOI] [PubMed] [Google Scholar]
- 10. Volpe U, Luciano M, Palumbo C, et al. Risk of burnout among early career mental health professionals. J Psychiatr Ment Health Nurs 2014; 21: 774–781. [DOI] [PubMed] [Google Scholar]
- 11. Holmberg C, Caro J, Sobis I. Job satisfaction among Swedish mental health nursing personnel: revisiting the two-factor theory. Int J Ment Health Nurs. Epub ahead of print 10 April 2017. DOI: 10.1111/inm.12339. [DOI] [PubMed] [Google Scholar]
- 12. Acker GM. The effect of organizational conditions (role conflict, role ambiguity, opportunities for professional development, and social support) on job satisfaction and intention to leave among social workers in mental health care. Community Ment Health J 2004; 40: 65–73. [DOI] [PubMed] [Google Scholar]
- 13. Jones A. Multidisciplinary team working: collaboration and conflict. Int J Ment Health Nurs 2006; 15: 19–28. [DOI] [PubMed] [Google Scholar]
- 14. Edwards D, Burnard P, Coyle D, et al. Stress and burnout in community mental health nursing: a review of the literature. J Psychiatr Ment Health Nurs 2000; 7: 7–14. [DOI] [PubMed] [Google Scholar]
- 15. Gilboa S, Shirom A, Fried Y, et al. A meta-analysis of work demand stressors and job performance: examining main and moderating effects. Pers Psychol 2008; 61: 227–271. [Google Scholar]
- 16. Farrell GA, Dares G. Nursing staff satisfaction on a mental health unit. Aust N Z J Ment Health Nurs 1999; 8: 51–57. [DOI] [PubMed] [Google Scholar]
- 17. Locke EA. The nature and causes of job satisfaction. In: Dunnette M. (ed.). The handbook of industrial and organizational psychology. Chicago, IL: Rand McNally College Publishing, 1976, pp. 1297–1349. [Google Scholar]
- 18. Goh YS, Lee A, Chan SW, et al. Profiling nurses’ job satisfaction, acculturation, work environment, stress, cultural values and coping abilities: a cluster analysis. Int J Nurs Pract 2015; 21: 443–452. [DOI] [PubMed] [Google Scholar]
- 19. Coomber B, Barriball KL. Impact of job satisfaction components on intent to leave and turnover for hospital-based nurses: a review of the research literature. Int J Nurs Stud 2007; 44: 297–314. [DOI] [PubMed] [Google Scholar]
- 20. Fisher CD. Why do lay people believe that satisfaction and performance are correlated? Possible sources of a commonsense theory. J Organiz Behav 2003; 24: 753–777. [Google Scholar]
- 21. Mohr DC, Young GJ, Meterko M, et al. Job satisfaction of primary care team members and quality of care. Am J Med Qual 2011; 26: 18–25. [DOI] [PubMed] [Google Scholar]
- 22. Ward M, Cowman S. Job satisfaction in psychiatric nursing. J Psychiatr Ment Health Nurs 2007; 14: 454–461. [DOI] [PubMed] [Google Scholar]
- 23. Medina MN. Conflict, individual satisfaction with team, and training motivation. Team Perform Manag 2016; 22: 223–239. [Google Scholar]
- 24. Chang WY, Ma JC, Chiu HT, et al. Job satisfaction and perceptions of quality of patient care, collaboration and teamwork in acute care hospitals. J Adv Nurs 2009; 65: 1946–1955. [DOI] [PubMed] [Google Scholar]
- 25. Chen KY, Yang CM, Lien CH, et al. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci 2013; 10: 1471–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Korner M, Wirtz MA, Bengel J, et al. Relationship of organizational culture, teamwork and job satisfaction in interprofessional teams. BMC Health Serv Res 2015; 15: 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Edward KL, Hercelinskyj G, Giandinoto JA. Emotional labour in mental health nursing: an integrative systematic review. Int J Ment Health Nurs 2017; 26: 215–225. [DOI] [PubMed] [Google Scholar]
- 28. Itzhaki M, Peles-Bortz A, Kostistky H, et al. Exposure of mental health nurses to violence associated with job stress, life satisfaction, staff resilience, and post-traumatic growth. Int J Ment Health Nurs 2015; 24: 403–412. [DOI] [PubMed] [Google Scholar]
- 29. Zheng Z, Gangaram P, Xie H, et al. Job satisfaction and resilience in psychiatric nurses: a study at the Institute of Mental Health, Singapore. Int J Ment Health Nurs 2017; 26: 612–619. [DOI] [PubMed] [Google Scholar]
- 30. Abdollahi A, Abu Talib M, Yaacob SN, et al. Hardiness as a mediator between perceived stress and happiness in nurses. J Psychiatr Ment Health Nurs 2014; 21: 789–796. [DOI] [PubMed] [Google Scholar]
- 31. Herzberg F, Mausner B, Synderman BB. The motivation to work. New York: Wiley, 1959. [Google Scholar]
- 32. Cohen SG, Bailey DE. What makes teams work: group effectiveness research from the shop floor to the executive suite. J Management 1997; 23: 239–290. [Google Scholar]
- 33. Madrid HP, Totterdell P, Niven K, et al. Leader affective presence and innovation in teams. J Appl Psychol 2016; 101: 673–686. [DOI] [PubMed] [Google Scholar]
- 34. Ilgen DR, Hollenbeck JR, Johnson M, et al. Teams in organizations: from input-process-output models to IMOI models. Annu Rev Psychol 2005; 56: 517–543. [DOI] [PubMed] [Google Scholar]
- 35. Mathieu J, Maynard MT, Rapp T, et al. Team effectiveness 1997–2007: a review of recent advancements and a glimpse into the future. J Manag 2008; 34: 410–477. [Google Scholar]
- 36. Lee H, Cummings GG. Factors influencing job satisfaction of front line nurse managers: a systematic review. J Nurs Manag 2008; 16: 768–783. [DOI] [PubMed] [Google Scholar]
- 37. Evans S, Huxley P, Gately C, et al. Mental health, burnout and job satisfaction among mental health social workers in England and Wales. Br J Psychiatry 2006; 188: 75–80. [DOI] [PubMed] [Google Scholar]
- 38. Edwards D, Burnard P, Owen M, et al. A systematic review of the effectiveness of stress-management interventions for mental health professionals. J Psychiatr Ment Health Nurs 2003; 10: 370–371. [DOI] [PubMed] [Google Scholar]
- 39. Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA 2011; 305: 2009–2010. [DOI] [PubMed] [Google Scholar]
- 40. Happell B, Martin T, Pinikahana J. Burnout and job satisfaction: a comparative study of psychiatric nurses from forensic and a mainstream mental health service. Int J Ment Health Nurs 2003; 12: 39–47. [DOI] [PubMed] [Google Scholar]
- 41. Bland AR, Rossen EK. Clinical supervision of nurses working with patients with borderline personality disorder. Issues Ment Health Nurs 2005; 26: 507–517. [DOI] [PubMed] [Google Scholar]
- 42. Judge TA, Thoresen CJ, Bono JE, et al. The job satisfaction-job performance relationship: a qualitative and quantitative review. Psychol Bull 2001; 127: 376–407. [DOI] [PubMed] [Google Scholar]
- 43. Nielsen K, Yarker J, Randall R, et al. The mediating effects of team and self-efficacy on the relationship between transformational leadership, and job satisfaction and psychological well-being in healthcare professionals: a cross-sectional questionnaire survey. Int J Nurs Stud 2009; 46: 1236–1244. [DOI] [PubMed] [Google Scholar]
- 44. Dallender J, Nolan P. Mental health work observed: a comparison of the perceptions of psychiatrists and mental health nurses. J Psychiatr Ment Health Nurs 2002; 9: 131–137. [DOI] [PubMed] [Google Scholar]
- 45. Osborn LA, Stein CH. Mental Health Care Providers’ views of their work with consumers and their reports of recovery-orientation, job satisfaction, and personal growth. Community Ment Health J 2016; 52: 757–766. [DOI] [PubMed] [Google Scholar]
- 46. Acker GM. The challenges in providing services to clients with mental illness: managed care, burnout and somatic symptoms among social workers. Community Ment Health J 2010; 46: 591–600. [DOI] [PubMed] [Google Scholar]
- 47. Ogresta J, Rusac S, Zorec L. Relation between burnout syndrome and job satisfaction among mental health workers. Croat Med J 2008; 49: 364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kilpatrick K, Lavoie-Tremblay M, Ritchie JA, et al. Advanced practice nursing, health care teams, and perceptions of team effectiveness. Health Care Manag 2011; 30: 215–226. [DOI] [PubMed] [Google Scholar]
- 49. Spector PE. Measurement of human service staff satisfaction: development of the job satisfaction survey. Am J Community Psychol 1985; 13: 693–713. [DOI] [PubMed] [Google Scholar]
- 50. Spreitzer GM. Social structural characteristics of psychological empowerment. Acad Manag J 1996; 39: 483–504. [Google Scholar]
- 51. Rossi ME. The development and validation of the comprehensive team interdependence scale. MA Thesis, University of South Florida, Tampa, FL, 2008. [Google Scholar]
- 52. Maynard MT. The impact of experience and familiarity: an examination in project teams. Storrs, CT: University of Connecticut, 2007. [Google Scholar]
- 53. Jehn KA, Mannix EA. The dynamic nature of conflict: a longitudinal study of intragroup conflict and group performance. Acad Manag J 2001; 44: 238–251. [Google Scholar]
- 54. Bock GW, Zmud RW, Kim YG, et al. Behavioral intention formation in knowledge sharing: examining the roles of extrinsic motivators, social-psychological forces, and organizational climate. MIS Quart 2005; 29: 87–111. [Google Scholar]
- 55. Chiocchio F, Lebel P, Dube JN. Informational role self-efficacy: a validation in interprofessional collaboration contexts involving healthcare service and project teams. BMC Health Serv Res 2016; 16: 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Campion MA, Papper EM, Medsker GJ. Relations between work team characteristics and effectiveness: a replication and extension. Pers Psychol 1996; 49: 429–452. [Google Scholar]
- 57. De Dreu CK. Cooperative outcome interdependence, task reflexivity, and team effectiveness: a motivated information processing perspective. J Appl Psychol 2007; 92: 628–638. [DOI] [PubMed] [Google Scholar]
- 58. Chiocchio F, Grenier S, O’Neill TA, et al. The effects of collaboration on performance: a multilevel validation in project teams. IIJPOM 2012; 4: 1–37. [Google Scholar]
- 59. O’Connell M, Tondora J, Croog G, et al. From rethoric to routine; assessing perceptions of recovery-oriented practices in a state mental health addiction system. Psychiatr Rehabil J 2005; 28: 378–386. [DOI] [PubMed] [Google Scholar]
- 60. Simons TL, Peterson RS. Task conflict and relationship conflict in top management teams: the pivotal role of intragroup trust. J Appl Psychol 2000; 85: 102–111. [DOI] [PubMed] [Google Scholar]
- 61. Allen NJ, Meyer JP. The measurement and antecedents of affective, continuance and normative commitment to the organization. JOOP 1990; 63: 1–18. [DOI] [PubMed] [Google Scholar]
- 62. Anderson NR, West MA. Measuring climate for work group innovation: development and validation of the team climate inventory. J Organ Behav 1998; 19: 235–258. [Google Scholar]
- 63. Sicotte C, D’Amour D, Moreault M-P. Interdisciplinary collaboration within Quebec community health care centres. Soc Sci Med 2002; 55: 991–1003. [DOI] [PubMed] [Google Scholar]
- 64. Griffin MA, Neal A, Parker SK. A new model of work role performance: positive behavior in uncertain and interdependent contexts. Acad Manag J 2007; 50: 327–347. [Google Scholar]
- 65. Kanter R. Men and women of the corporation. New York: Basic Books, 1993. [Google Scholar]
- 66. Chou RJ, Robert SA. Workplace support, role overload, and job satisfaction of direct care workers in assisted living. J Health Soc Behav 2008; 49: 208–222. [DOI] [PubMed] [Google Scholar]
- 67. Yanchus NJ, Periard D, Osatuke K. Further examination of predictors of turnover intention among mental health professionals. J Psychiatr Ment Health Nurs 2017; 24: 41–56. [DOI] [PubMed] [Google Scholar]
- 68. Webster L, Hackett RK. Burnout and leadership in community mental health systems. Adm Policy Ment Health 1999; 26: 387–399. [DOI] [PubMed] [Google Scholar]
- 69. Hooper ME, Browne G, O’Brien AP. Graduate nurses’ experiences of mental health services in their first year of practice: an integrative review. Int J Ment Health Nurs 2016; 25: 286–298. [DOI] [PubMed] [Google Scholar]
- 70. Hyrkäs K. Clinical supervision, burnout, and job satisfaction among mental health and psychiatric nurses in Finland. Issues Ment Health Nurs 2005; 26: 531–556. [DOI] [PubMed] [Google Scholar]
- 71. Hannigan B, Edwards D, Coyle D, et al. Burnout in community mental health nurses: findings from the all-Wales stress study. J Psychiatr Ment Health Nurs 2000; 7: 127–134. [DOI] [PubMed] [Google Scholar]
- 72. De Dreu CK, Weingart LR. Task versus relationship conflict, team performance, and team member satisfaction: a meta-analysis. J Appl Psychol 2003; 88: 741–749. [DOI] [PubMed] [Google Scholar]
- 73. Kozlowski SWJ, Bell B. Work groups and teams in organizations. In: Weiner IB, Schmidt NW, Highouse S. (eds) Handbook of psychology, industrial and organizational psychology. London: Wiley, 2003, pp. 333–375. [Google Scholar]
- 74. Chiocchio F. Indicateurs pertinents à la collaboration dans le milieu de la santé - cadre conceptuel et inventaire de mesures. Montréal, QC, Canada: Université de Montréal, 2012. [Google Scholar]
- 75. Miles SJ, Mangold G. Leadership in high-performance teams: a model for superior team performance. Team Perform Manag 2002; 8: 113–121. [Google Scholar]
- 76. Cleary M, Horsfall J. Teamwork and teambuilding: considering retreats. Issues Ment Health Nurs 2015; 36: 78–80. [DOI] [PubMed] [Google Scholar]
- 77. Papathanasiou IV, Kleisiaris CF, Tsaras K, et al. General satisfaction among healthcare workers: differences between employees in medical and mental health sector. Mater Sociomed 2015; 27: 225–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Gavartina A, Zaroti S, Szecsenyi J, et al. Practice assistants in primary care in Germany—associations with organizational attributes on job satisfaction. BMC Fam Pract 2013; 14: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Lloyd C, King R, Chenoweth L. Social work, stress and burnout: a review. JMH 2002; 11: 255–265. [Google Scholar]
- 80. Chiocchio F, Forgues D, Paradis D, et al. Teamwork in integrated design projects: understanding the effects of trust, conflict, and collaboration on performance. PMJ 2011; 42: 78–91. [Google Scholar]
- 81. McTiernan K, McDonald N. Occupational stressors, burnout and coping strategies between hospital and community psychiatric nurses in a Dublin region. J Psychiatr Ment Health Nurs 2015; 22: 208–218. [DOI] [PubMed] [Google Scholar]
- 82. Rodney V. Nurse stress associated with aggression in people with dementia: its relationship to hardiness, cognitive appraisal and coping. J Adv Nurs 2000; 31: 172–180. [DOI] [PubMed] [Google Scholar]
- 83. Kobasa SC. Stressful life events, personality, and health: an inquiry into hardiness. J Pers Soc Psychol 1979; 37: 1–11. [DOI] [PubMed] [Google Scholar]
- 84. Garrosa E, Rainho C, Moreno-Jimenez B, et al. The relationship between job stressors, hardy personality, coping resources and burnout in a sample of nurses: a correlational study at two time points. Int J Nurs Stud 2010; 47: 205–215. [DOI] [PubMed] [Google Scholar]
- 85. Shaikh U, Qamar I, Jafry F, et al. Patients with borderline personality disorder in emergency departments. Front Psychiatry 2017; 8: 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Amianto F, Ferrero A, Piero A, et al. Supervised team management, with or without structured psychotherapy, in heavy users of a mental health service with borderline personality disorder: a two-year follow-up preliminary randomized study. BMC Psychiatry 2011; 11: 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Onyett S, Pillinger T, Muijen M. Job satisfaction and burnout among members of community mental health teams. J Ment Health 1997; 6: 55–66. [DOI] [PubMed] [Google Scholar]