Abstract
Background
Shoulder pain secondary to acromioclavicular joint pain is a common presentation in primary and secondary care but is often poorly managed as a result of uncertainty about optimal treatment strategies. Osteoarthritis is the commonest cause. Although acromioclavicular pain can be treated non-operatively and operatively, there appears to be no consensus on the best practice pathway of care for these patients, with variations in treatment being common place. The present study comprises a scoping review of the current published evidence for the management of isolated acromioclavicular pain (excluding acromioclavicular joint dislocation).
Methods
A comprehensive search strategy was utilized in multiple medical databases to identify level 1 and 2 randomised controlled trials, nonrandomised controlled trials and systematic reviews for appraisal.
Results
Four systematic reviews and two randomised controlled trials were identified. No direct studies have compared the benefits or risks of conservative versus surgical management in a controlled environment.
Conclusions
High-level studies on treatment modalities for acromioclavicular joint pain are limited. As such, there remains little evidence to support one intervention or treatment over another, making it difficult to develop any evidenced-based patient pathways of care for this condition.
Level of evidence: 2A
Keywords: acromioclavicular joint, arthroscopic surgery, corticosteroid injection, distal clavicular excision, pain
Introduction
Acromioclavicular joint (ACJ) pain is a common cause of shoulder pain in adults. The incidence of ACJ pain is reported to be between 0.5 to 2.9/1000/year in primary care.1,2 Injuries are a common precipitating cause, occurring through direct impact on the joint or a fall on an outstretched arm. Arthritis is the main cause of pain, and it develops as a consequence of constant stress on the joint, often in people who perform repeated overhead lifting activities.3 Arthritis is often associated with distal clavicular osteolysis.4,5 Damage to the ACJ can be synchronous with damage to the supraspinatus tendon and osteophytes from the arthritic joint may contribute to subacromial impingement exacerbating and producing further shoulder pain. Patients usually localize their pain to the AC joint. The most sensitive tests for ACJ pain are acromioclavicular point tenderness and the Paxinos test (reported as 96% and 79%, respectively) but both carry low specificity.6 Bone scans have been used in selected cases to confirm damage at the ACJ,6 although plain radiography and magnetic resonance imaging are usually investigations of choice.
Despite its prevalence in primary and secondary care, the management of ACJ pain appears to be highly variable with uncertainty as to whether surgical or non-operative management is effective. As such, the management of ACJ pain appears to be determined by the degree of pain and disability. Non-operative management is usually considered first, with activity modification, physical therapy modalities, oral analgesics and injections of corticosteroid and local anaesthetic all being options. It is suggested that injections can provide good pain relief and be a helpful diagnostic test, but seem to be ineffective as a long term therapy.7
Surgical treatments involve distal clavicular excision (DCE), which was initially performed as an open procedure, first described in 1941.8 However, the procedure is now commonly performed arthroscopically.9 The procedure aims to produce a ‘gap’ between acromion and clavicle and involves resecting bone mainly from the distal end of the clavicle without compromising joint stability. The arthroscopic approach is considered to result in minimal trauma and quicker rehabilitation.
With the growing need to develop evidenced-based patient pathways for many common joint conditions, we aimed to conduct a scoping review evaluating the quality of published literature and the efficacy of surgical and non-operative (conservative) treatments for adults with AC joint pain.
Materials and methods
Data sources
Systematic reviews, level 1 and 2 randomized controlled trials (RCT) and controlled nonrandomized trials (CNT) were identified by searching Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Medline, Embase, NHS Evidence, Database of Abstracts of Reviews of Effects, National Guideline Clearing House, DARE and Health Technology Assessments. Studies were limited to those published in the English language without any date restrictions. The key words utilized for the search included acromioclavicular, acromioclavicular joint, acromioclavicular pain, decompression, excision, reconstruction, debridement, open, arthroscopic, physiotherapy, injection, painkiller, analgesia.
Quality appraisal
Two reviewers (SC and LB) independently assessed the titles and abstracts of all retrieved searches to determine their relevance and eligibility for inclusion. Any discrepancies were discussed and resolved by a third independent investigator (JR).
The quality of the included studies was evaluated using the validated consolidation of standards of reporting trials (CONSORT)10 tool. The identified systematic reviews were appraised using the assessment of multiple systematic reviews (AMSTAR)11 tool. Both validated assessment tools utilize questionnaires that facilitate critical evaluation of the methodology, quality and strength of evidence and conclusions. Kappa statistics were used to assess inter-rater agreement.
Study selection and eligibility criteria
Inclusion criteria consisted of articles evaluating the management of ACJ pain secondary to osteoarthritis (OA), arthrosis or distal clavicle osteolysis. Non-operative (conservative) treatments considered in this review included analgesics, physiotherapy, injections and immobilisation in a sling. This review includes consideration of the following surgical management options for ACJ pain as either a single or combined procedure: open acromioclavicular joint reconstruction, arthroscopic acromioclavicular joint reconstruction, open excision, arthroscopic excision and arthroscopic debridement. Studies were excluded if they considered patients with ACJ dislocations.
All outcome measures used were documented and included the Oxford Shoulder Score, Constant–Murley Score, Disabilities of the Arm, Shoulder and Hand (DASH), Oxford Instability Score, American Shoulder and Elbow Surgeons Score (ASES), Western Ontario Shoulder Instability Index (WOSI),12 Darrow score for acromioclavicular separation,13 Hospital for Special Surgery (HSS) shoulder assessment,14 Loyola, Neer shoulder score,15 Athletic shoulder scoring system (ATH score), the Simple Shoulder Test (SST),16 Matsen,17 Rowe Score for Instability18 and Single Assessment Numeric Evaluation (SANE).19
Results
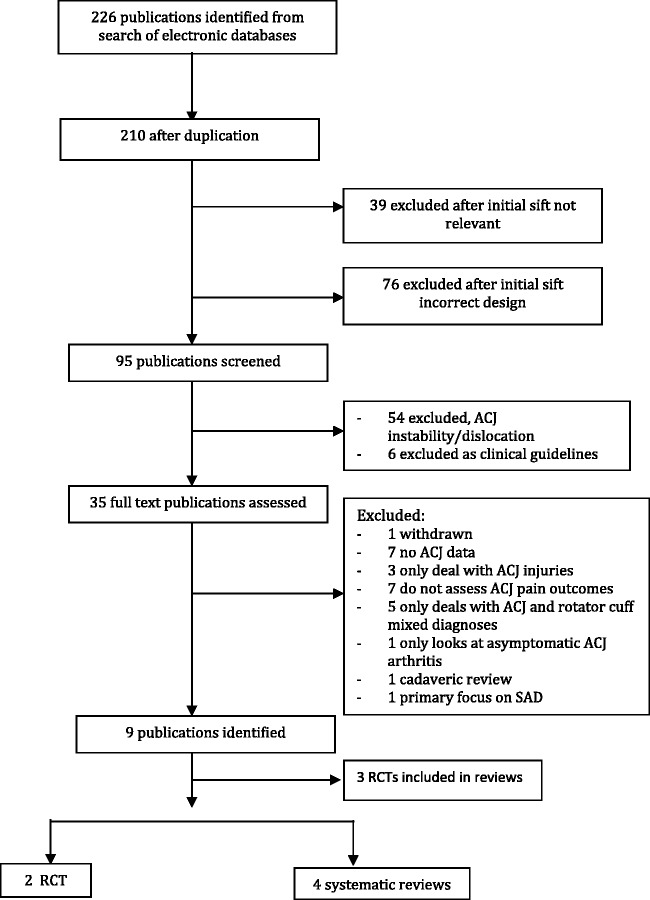
The initial search only generated 226 references, which were reduced to 210 after removal of duplicated studies. Of these, 39 were excluded and 76 were inappropriately designed. The remaining 95 articles were assessed by two reviewers; only four systematic reviews and five primary studies were identified as having met the inclusion criteria. From the five primary studies, three were removed because they had been included in the systematic reviews. Details of the search and exclusion process are provided in Figure 1. A summary of the characteristics of the identified reviews and studies is included in Table 1.
Figure 1.
Schematic representation of literature review and selection process to identify relevant studies and reviews. ACJ, acromioclavicular joint; RCT, randomized controlled trial; SAD, sub-acromial decompression.
Table 1.
Characteristics of studies evaluating management options for ACJ pathologies.
| Study | Study type | Inclusions and exclusions | Outcomes | Interventions | Results | Conclusions | Level of evidence |
|---|---|---|---|---|---|---|---|
| Pensak et al.48 | Systematic review | Inclusion: studies in peer-reviewed journals Ezxclusion: not in English, not in peer-reviewed journals | • ASES • Constant • Darrow (pain) • HSS • Loyola • MASES • Matsen • Neer • Radiography • SF-36 • Shoulder ROM • Subjective pain response • UCLA • VAS | Open DCE: 9 trials, 287 resections, 284 patients35–43 | 79% good/excellent results Mean follow-up 4.9 years | Arthroscopic and open DCE both improve pain and objective scores Insufficient evidence regarding open versus arthroscopic procedure Similarly favourable results if concomitant procedure performed Arthroscopic DCE gives quicker recovery and return to sports (direct approach quickest recovery) Trend for worse outcomes for DCE following traumatic event | Level III |
| Arthroscopic DCE: 6 studies, 142 resections in total29–34 | 92.5% good/excellent results Mean follow-up 2.2 years | ||||||
| Open versus arthroscopic DCE: 1 study, 17 patients51 | Arthroscopic VAS score decreased (p = 0.03), open no change (p = 0.11) 1-year follow-up | ||||||
| Direct versus Indirect arthroscopic DCE: 1 study, 34 patients52 | Direct method improved ASES (p = 0.00051) and ATH (p = 0.00144) over indirect at 6 weeks, no difference at 27 months. Faster return to sports with direct (p < 0.001) | ||||||
| DCE with concomitant procedure: 7 studies, 212 patients9,44–49 | 95% good/excellent results, 3.2-year mean follow-up | ||||||
| Post-traumatic ACJ DCE: 6 studies, 133 patients31,37–39,42,44 | 23% poor results, No follow-up mentioned | ||||||
| Rabalais et al.26 | Systematic review | Inclusion: studies in peer-reviewed journals Exclusion: Review articles, textbook chapters, poster presentations, meeting abstracts, case reports, and biomechanical studies | • 10-cm VAS scale • ASES • Darrow • Loyola • Matsen • Neer • Radiographs • SF-36 • Shoulder ROM • Strength • Subjective pain score • UCLA | Open DCE: 9 studies, 289 patients35–43 | 76.3% satisfactory results, 4.9-year mean follow-up | Arthroscopic and open DCE both significantly improve pain and objective scores Similarly favourable results if concomitant procedure performed Conflicting results for coplaning Conflicting results for DCE following traumatic events | Level III |
| Isolated arthroscopic DCE: 6 studies 146 patients29–34 | 92.5% satisfactory results, 2.2-year mean follow-up | ||||||
| DCE with subacro mial decompression or rotator cuff repair: 7 studies, 212 patients9,44–49 | 94% good/excellent results, 3.2-year mean follow-up | ||||||
| Coplaning: 3 studies, 100 patients53–55 | 17% with postoperative ACJ symptoms 2.7-year mean follow-up | ||||||
| DCE after fracture or low-grade separation: 6 studies, 130 subjects31,37–39,42,44 | 23% poor results No follow-up mentioned | ||||||
| Anterior-posterior translation after DCE: 1 study, 17 subjects56 | Increased translation correlates with increased pain, p < 0.009 | ||||||
| Buchbinder et al. 22 | Systematic review | Inclusion: randomized and pseudo-randomized trials of shoulder pain in patients older than 18 years. If various regional pain disorders, included if present shoulder data separately or 90% of participants with shoulder pain Exclusion: shoulder pain less than 3 weeks, rheumatoid arthritis, polymyalgia rheumatica, fractures | • Subjective pain assessment • Clinical examination of shoulder | Intra-articular, subacromial and acromioclavicular steroid injections (n = 47) versus physiotherapy (n = 35) or manipulation (n = 32) for mixed shoulder diagnoses22 | Steroid injections offer improved pain relief over physiotherapy (WMD −2.30, 95% CI −4.10 to −0.50) and manipulation (WMD −3.40, 95% CI −5.46 to −1.34), Follow-up 11 weeks | No evidence for efficacy of steroid injections versus physiotherapy or manipulation for ACJ pain No evidence for efficacy of steroid injections specifically for ACJ pain | Level II |
| Anatomical steroid and LA injection (n = 43) versus tender point injection (n = 39) for mixed shoulder diagnoses23 | Anatomical injections superior of tender point injections for pain improvement (RR 2.96, CI 1.62 to 5.42). Follow-up 1 week | ||||||
| Peterson et al.25 | Review article | Inclusion: not mentioned Exclusion: not mentioned | • ACJ Osteoarthritis symptoms, Constant score • Subjective pain response using VAS scale • Shoulder ROM | Intra-articular steroid injection for ACJ OA (n = 25) 5-year follow-up25 | Improvement in Constant score at 5 years (p = 0.005) | No conclusive results. Larger sample size and longer follow-up needed | Level III |
| Intra-articular guided ACJ injection (n = 50) 15-minute response(27) | Mean pain relief of 38% in patients at 15 minutes | ||||||
| Intra-articular steroid ACJ injection (n = 18), ROM assessment at 2 weeks(26) | Range of extension (p < 0.05) and pain (p < 0.01) improved. If degenerative ACJ, horizontal flexion improved (p < 0.05) | ||||||
| Sabeti-Aschraf et al.20 | Randomised controlled trial | Inclusion: VAS score at rest > 4, tender spot at AC joint, positive AAT, age 18 years to 80 years, absence of local skin irritation Exclusion: Diabetes mellitus, anticoagulation, pregnancy, glenohumeral osteoarthritis, mental disorders | • 10-cm VAS scale at rest • 10-cm VAS scale under pressure at the joint area • AAT • CMS | US-guide ACJ injection (n = 10) versus palpation-guided ACJ injection (n = 10) 3 week follow-up | CMS (p < 0.0004), AAT (p < 0.0423) both improved after 3 weeks. VAS rest (p < 0.2574) and VAS pain (p < 0.1166) no improvement. No intergroup differences in CMS (p = 0.5120), AAT (p = 0.2944), VAS rest (p = 0.8743), VAS pain (p = 0.5120) | No evidence for improvement at 3-week follow-up after steroid injection No difference between US-guided and palpation method intra-articular injections | Level II |
| Sabeti-Aschraf et al.21 | Randomised controlled trial | Inclusion: age 18 years to 80 years, VAS score > 4 for 4 weeks, tender spot at AC joint, crossover test, Constant-Murley < 65 Exclusion: previous surgery, trauma, Rockwood type 2 or greater, diabetes mellitus, allergy to lignocaine, pregnancy, glenohumeral osteoarthritis, mental disorders, massive AC joint arthritis with loss of joint space | • CMS • Cross-over Arm Test • 10-cm VAS-p on palpation • 10-cm VAS-n at night | US-guide intra- articular ACJ injection (n = 53) versus US-guided peri-articular ACJ injection (n = 53) | Clinical improvement in all four domains at 1 hour and 3 weeks (p < 0.0001) | Evidence for improvement at 3-week follow-up after steroid injection of either intra-articular or peri-articular injection | Level II |
| 3-week follow-up | No intergroup differences in CMS (p = 0.2408), COAT (p value not specified), VAS-p (p = 0.0608), VAS-n (p value not specified) | No difference between peri-articular or intra-articular ACJ injections in all parameters |
ACJ, acromio clavicular joint; AAT, Arm Adduction Test; ASES, American Shoulder and Elbow Surgeons; CI, confidence interval; CMS, Constant–Marley Score; DCE, distal clavicular excision; HSS, Hospital for Special Surgery; MASES, Modified American Shoulder and Elbow Surgeons; OA, osteoarthritis; RR, risk ratio; ROM, range of motion; SF-36, Short-Form 36; US, ultrasound; VAS, visual analogue scale; WMD, weighted mean difference.
Thirty-two primary studies relevant to acromioclavicular joint pathology were included in the four systematic reviews published between 1998 and 2007. There was substantial overlap between two systematic reviews, with 22 studies appearing in both papers, the remaining 10 studies only appeared in a single review.
Quality assessment
The inter-rater agreement was good with a kappa value of 0.863 (SE of kappa 0.056, 95% confidence interval 0.754 to 0.973). Apart from one Cochrane review, the other systematic reviews were of poor methodological quality because they only addressed a few of the AMSTAR criteria. The four reviews were predominantly based on lower level studies and therefore could not be classed as level I evidence. One study did not set clear inclusion or exclusion criteria and only one review included a list of excluded studies or addressed the issue of publication bias.
Therapeutic injections
Sabeti-Aschraf et al.20 conducted a small randomized trial of 20 patients to evaluate whether US guidance for the infiltration of the symptomatic ACJ improves outcomes when compared to the traditional palpation method. Outcome measures were recorded at 1 week, 2 weeks and 3 weeks post injection. There were significant improvements in all tested variables from baseline to the first and second week of follow-up. By the third week, ACJ pain and tenderness returned to baseline levels, although the improvement in function was still significant. There were no significant differences between both groups, with the investigators proposing a poorer than expected result in the US guided group could be secondary to cartilage or meniscoid damage as a result of precise guidance of the needle into the joint.
In addition, Sabeti-Aschraf et al.21 conducted a multi-centered controlled trial with 106 symptomatic arthritic ACJs to compare the efficacy of intra-articular and peri-articular joint injections. Outcomes were measured at 1 hour, 1 week and 3 weeks post-injection and recorded using the Constant–Murley score, cross-over arm test and visual analogue scale (VAS) to assess pain on palpation and pain at night. Significant improvements in both groups were detected at all three stages from baseline. A significant improvement in pain in the intra-articular group was only identified on the cross-over arm test; however, no significant difference could be identified at any other stage or using any other outcome measure. This study was only utilized to assess the short-term improvements from steroid injections.
Buchbinder et al.22 (AMSTAR 11/11) examined the evidence for the efficacy and safety of corticosteroid injections for the treatment of adults with shoulder pain. This Cochrane review was conducted following a peer reviewed a priori protocol and only included randomised or pseudo-randomised controlled trials. Two included studies addressed the management of a population with mixed diagnoses, which included patients with ACJ pathology. One randomized trial23 demonstrated a significant benefit favouring steroid injections over physiotherapy and manipulation with respect to pain at the end of treatment. Patients had a range of diagnoses and the investigators did not report the exact proportion of patients who had ACJ pathology. Another randomized trial,24 comparing anatomical steroid injection to trigger or tender point injection, demonstrated significantly greater symptomatic relief with functional injections in participants with shoulder pain at 1 week. However, only 11 of the 92 patients in the study had a diagnosis of ACJ ‘strain’ and it is not clear which treatment groups these patients were assigned to. It was concluded in the present review that there is little evidence to either support or refute the efficacy of steroid injections for all forms of shoulder pain.
Peterson et al.25 (AMSTAR 5/11) performed a review of the literature to evaluate the level of evidence concerning the effectiveness of therapeutic joint injections into various peripheral joints. The review met five of the 11 AMSTAR criteria. The reviewers did not set out their inclusion and exclusion criteria or provide adequate details regarding their search strategy. Although the search was focused primarily on level I and II evidence, lower level studies were considered in the absence of any other evidence.
Three prospective cohort studies investigating therapeutic injections for ACJ osteoarthritis/arthropathy were reviewed. There was approximately a 25% reduction in symptoms, lasting at least 12 months in a 5-year follow-up study. Two studies reported an improvement in pain 15 minutes post injection, and improvements in pain and range of motion 2 weeks post injection; no longer-term follow-up was reported in these studies. The present review concluded that larger sample sizes with a longer follow-up are required to evaluate this form of treatment.
Open and arthroscopic distal clavicle excision
Rabalais et al.26 (AMSTAR 8/11) reviewed studies describing the surgical management of symptomatic ACJ pathology. They concluded that the literature supports surgical excision for ACJ osteoarthritis and osteolysis; however, these recommendations were based on level III or level IV evidence consisting largely of retrospective case series. Patients reported to have had ‘good’ or ‘excellent’ results in primary studies were grouped into the category of having a ‘satisfactory’ outcome. Six studies evaluating 146 patients receiving isolated arthroscopic DCE reported satisfactory outcomes in 92.5% (range 85% to 100%) at a mean follow-up of 2.2 years.27–32 Three of these studies used the direct approach27–29 and three used the indirect approach,30–32; however, the investigators did not compare the outcomes of the two arthroscopic techniques. The nine open DCE studies33–41 demonstrated greater variability with satisfactory outcomes ranging from 50% to 100% and a mean satisfaction of 76.3%. These studies included 189 patients over a mean follow up of 4.9 years (range 2.1 years to 9 years).
There have been seven studies that have investigated outcomes of DCE (open or arthroscopic) with concomitant procedures.9,42–47 These results need to be interpreted with caution because the surgeries were not limited solely to addressing the ACJ but involved concomitant procedures such as sub-acromial decompression and rotator-cuff repairs. 94% (range 87% to 100%) of a total 212 patients reported good or excellent outcomes at an mean follow-up of 3.2 years, demonstrating success rates similar to isolated arthroscopic DCE. Six studies reported poor outcomes in 23% of the 130 patients receiving open or arthroscopic DCE for post-traumatic aetiologies (fracture or low grade separations).29,35–37,40,42 Although there was a trend for poorer outcomes in this group, especially for grade II separations, the results between the studies were conflicting.
Pensak et al.48 (AMSTAR 6/11) performed a limited search for articles reporting on outcomes of distal clavicle excision for acromioclavicular joint arthritis or acromioclavicular osteolysis. The majority of studies that were included were level IV case series, all of which were included in the previous surgical review by Rabalais et al.26 who agreed with the conclusions of the previous paper and a further two RCTs were included. The investigators concluded that the arthroscopic procedure, specifically through the direct approach, enabled a faster return to activities at the same time as obtaining similar long-term outcomes compared to the open procedure. Of the two RCTs, one study had compared open and indirect arthroscopic DCE in a group of 17 patients with ACJ pain nonresponsive to conservative measures.49 Earlier recovery and/or better outcomes were reported in the arthroscopic group, and a statistically significant improvement in the VAS pain score from baseline to 1 year was identified for only the arthroscopic group. The sample size was insufficiently powered and investigators suggested that the identified trends could be attributed to the treatment of other intra-articular pathology (debridement of superior aspect of the glenoid labrum and rotator cuff tears) identified in 50% of the arthroscopic group. The other randomized study by Charron et al.50 compared direct and indirect arthroscopic approaches in 34 athletes with osteolysis or post-traumatic osteoarthrosis. Both groups had excellent outcomes; however, the direct group had significantly higher functional scores at 2 and 6 weeks postoperatively, and these patients also had a significantly quicker return to sport.
Discussion
This scoping review has critically evaluated studies published in English pertaining to operative and non-operative management of ACJ pain (excluding ACJ instability). Four systematic reviews were identified, two of which looked at operative treatments26,48 and two reviews focused on non-operative, injections into the ACJ.22,25 Generally, the quality of the systematic reviews was good rather than high because three of the systematic reviews presented comprehensive literature reviews that identified relevant studies and key data. One of the reviews failed to identify clear inclusion and exclusion criteria.25 The patient populations studied were not always clearly identified, and some bias was introduced by the fact that many patients with ACJ pathologies also had other concomitant shoulder pathologies, such as rotator cuff tears, making it difficult to delineate the cause of shoulder pain and effectiveness of subsequent treatments. Quantitative analyses of the published literature could not be performed because of the heterogenous populations, the presence of concomitant pathologies, variable treatment options and the outcome measures used. There was no standardization in the assessment parameters or assessment tools and there was wide variation in the outcome scores used to assess functional outcome, making collation of data from different studies not possible. There is a need for assessment and consensus of outcome scores for ACJ pathology.
Although the literature suggests that open and arthroscopic surgical excision for ACJ osteoarthritis and osteolysis can consistently result in pain relief and improved outcomes in the majority of patients, the present review reveals a lack of primary evidence regarding treatments and treatment pathways for ACJ pain. At no point have arthroscopic surgery, open surgery, steroid injections and rehabilitation programmes been compared directly.
A number of reviews and studies have tried to evaluate the effectiveness of steroid injections into the ACJ, through comparison with placebo treatments and physiotherapy.22–24 The efficacy of steroid delivery was further evaluated by a small study concluding that ultrasound guided injections did not improve pain compared to techniques reliant upon blind injections only.20 However, with only 20 subjects, the study is underpowered. Furthermore, a larger suitably powered study evaluated the difference between peri-articular and intra-articular injections under image guidance and showed no significant difference in the majority of scores up to 3 weeks post-injection.21 That study did not evaluate any long-term benefits of steroid injections. Therefore, there is no clear evidence that steroid injection is either effective or ineffective in treating ACJ pain and few studies report long-term outcomes. Similarly, there is no strong evidence comparing steroid treatment to physiotherapy.
Conclusions
Despite the prevalence of the AC Joint causing pain and disability, this up-to-date review of the management of ACJ pain highlights the need for further evidence comparing the efficacy of both operative (open and arthroscopic) and non-operative treatment modalities. This lack of useful literature on the management of ACJ pain means that we are currently destined to continue to treat this problem ‘traditionally’ with physiotherapy and ACJ steroid injection, followed finally by surgery.
Acknowledgements
We would like to acknowledge and thank the Royal College of Surgeons in England and the British Orthopaedic Association for providing financial support to commission the undertaking of the literature search.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The paper has not been presented at any society or meeting.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical review and patient consent
Ethical approval or patient consent was not required for this Review Article.
Level of evidence
Level 2A
References
- 1.van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995; 54: 959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ostor AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL. Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology (Oxford) 2005; 44: 800–805. [DOI] [PubMed] [Google Scholar]
- 3.Buss DD, Watts JD. Acromioclavicular injuries in the throwing athlete. Clin Sports Med 2003; 22: 327–341. [DOI] [PubMed] [Google Scholar]
- 4.Henry MH, Liu SH, Loffredo AJ. Arthroscopic management of the acromioclavicular joint disorder. A review. Clin Orthop Relat Res 1995; 316: 276–283. [PubMed] [Google Scholar]
- 5.Beals RK, Sauser DD. Nontraumatic disorders of the clavicle. J Am Acad Orthop Surg 2006; 14: 205–214. [DOI] [PubMed] [Google Scholar]
- 6.Walton J, Mahajan S, Paxinos A, et al. Diagnostic values of tests for acromioclavicular joint pain. J Bone Joint Surg Am 2004; 86A: 807–812. [DOI] [PubMed] [Google Scholar]
- 7.Jacob AK, Sallay PI. Therapeutic efficacy of corticosteroid injections in the acromioclavicular joint. Biomed Sci Instrum 1997; 34: 380–385. [PubMed] [Google Scholar]
- 8.Gurd FB. the treatment of complete dislocation of the outer end of the clavicle: an hitherto undescribed operation. Ann Surg 1941; 113: 1094–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kay SP, Ellman H, Harris E. Arthroscopic distal clavicle excision. Technique and early results. Clin Orthop Relat Res 1994; 301: 181–184. [PubMed] [Google Scholar]
- 10.Begg C, Cho M, Eastwood S, et al. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA 1996; 276: 637–639. [DOI] [PubMed] [Google Scholar]
- 11.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methool 2007; 7: 10–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability – The Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med 1998; 26: 764–772. [DOI] [PubMed] [Google Scholar]
- 13.Darrow JC, Smith JA, Lockwood RC. A New Conservative Method for Treatment of Type-Iii Acromioclavicular Separations. Orthop Clin North Am 1980; 11: 727–33. [PubMed] [Google Scholar]
- 14.Mancuso CA, Altchek DW, Craig EV, et al. Patients' expectations of shoulder surgery. J Shoulder Elbow Surg 2002; 11: 541–549. [DOI] [PubMed] [Google Scholar]
- 15.Neer CS., II Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970; 52: 1077–1089. [PubMed] [Google Scholar]
- 16.Lippitt SB, Harryman DT, Matsen FA. A practical tool for evaluating function – the Simple Shoulder Test. In: Matsen F, Hawkins RJ. (eds). The shoulder: A balance of mobility and stability, Rosemont: American Academy of Orthopaedic Surgeons, 1993, pp. 501–518. [Google Scholar]
- 17.Matsen FA, III, Ziegler DW, DeBartolo SE. Patient self-assessment of health status and function in glenohumeral degenerative joint disease. J Shoulder Elbow Surg 1995; 4: 345–351. [DOI] [PubMed] [Google Scholar]
- 18.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am 1978; 60: 1–16. [PubMed] [Google Scholar]
- 19.Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the single assessment numeric evaluation method and two shoulder rating scales – outcomes measures after shoulder surgery. Am J Sports Med 1999; 27: 214–221. [DOI] [PubMed] [Google Scholar]
- 20.Sabeti-Aschraf M, Ochsner A, Schueller-Weidekamm C, et al. The infiltration of the AC joint performed by one specialist: ultrasound versus palpation a prospective randomized pilot study. Eur J Radiol 2010; 75: e37–e40. [DOI] [PubMed] [Google Scholar]
- 21.Sabeti-Aschraf M, Stotter C, Thaler C, et al. Intra-articular versus periarticular acromioclavicular joint injection: a multicenter, prospective, randomized, controlled trial. Arthroscopy 2013; 29: 1903–1910. [DOI] [PubMed] [Google Scholar]
- 22.Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 2003; 1: CD004016–CD004016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Winters JC, Sobel JS, Groenier KH, Arendzen HJ, Meyboom-de Jong B. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: randomised, single blind study. BMJ 1997; 314: 1320–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hollingworth GR, Ellis RM, Hattersley TS. Comparison of injection techniques for shoulder pain: results of a double blind, randomised study. BMJ 1983; 287: 1339–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peterson C, Hodler J. Evidence-based radiology (part 2): Is there sufficient research to support the use of therapeutic injections into the peripheral joints? Skeletal Radiol 2010; 39: 11–18. [DOI] [PubMed] [Google Scholar]
- 26.Rabalais RD, McCarty E. Surgical treatment of symptomatic acromioclavicular joint problems: a systematic review. Clin Orthop Relat Res 2007; 455: 30–37. [DOI] [PubMed] [Google Scholar]
- 27.Auge WK, II, Fischer RA. Arthroscopic distal clavicle resection for isolated atraumatic osteolysis in weight lifters. Am J Sports Med 1998; 26: 189–192. [DOI] [PubMed] [Google Scholar]
- 28.Bigliani LU, Nicholson GP, Flatow EL. Arthroscopic resection of the distal clavicle. Orthop Clin North Am 1993; 24: 133–141. [PubMed] [Google Scholar]
- 29.Zawadsky M, Marra G, Wiater JM, et al. Osteolysis of the distal clavicle: long-term results of arthroscopic resection. Arthroscopy 2000; 16: 600–605. [DOI] [PubMed] [Google Scholar]
- 30.Gartsman GM. Arthroscopic resection of the acromioclavicular joint. Am J Sports Med 1993; 21: 71–77. [DOI] [PubMed] [Google Scholar]
- 31.Kay SP, Dragoo JL, Lee R. Long-term results of arthroscopic resection of the distal clavicle with concomitant subacromial decompression. Arthroscopy 2003; 19: 805–809. [DOI] [PubMed] [Google Scholar]
- 32.Tolin BS, Snyder SJ. Our technique for the arthroscopic Mumford procedure. Orthop Clin North Am 1993; 24: 143–151. [PubMed] [Google Scholar]
- 33.Worcester JN, Jr, Green DP. Osteoarthritis of the acromioclavicular joint. Clin Orthop Relat Res 1968; 58: 69–73. [PubMed] [Google Scholar]
- 34.Cahill BR. Osteolysis of the distal part of the clavicle in male athletes. J Bone Joint Surg Am 1982; 64: 1053–1058. [PubMed] [Google Scholar]
- 35.Petersson CJ. Resection of the lateral end of the clavicle. A 3 to 30-year follow-up. Acta Orthop Scand 1983; 54: 904–907. [DOI] [PubMed] [Google Scholar]
- 36.Scavenius M, Iversen BF, Sturup J. Resection of the lateral end of the clavicle following osteolysis, with emphasis on non-traumatic osteolysis of the acromial end of the clavicle in athletes. Injury 1987; 18: 261–263. [DOI] [PubMed] [Google Scholar]
- 37.Cook FF, Tibone JE. The Mumford procedure in athletes. An objective analysis of function. Am J Sports Med 1988; 16: 97–100. [DOI] [PubMed] [Google Scholar]
- 38.Petchell JF, Sonnabend DH, Hughes JS. Distal clavicular excision: a detailed functional assessment. Aust NZJ Surg 1995; 65: 262–266. [DOI] [PubMed] [Google Scholar]
- 39.Novak PJ, Bach BR, Jr, Romeo AA, Hager CA. Surgical resection of the distal clavicle. J Shoulder Elbow Surg 1995; 4: 35–40. [DOI] [PubMed] [Google Scholar]
- 40.Eskola A, Santavirta S, Viljakka HT, Wirta J, Partio TE, Hoikka V. The results of operative resection of the lateral end of the clavicle. J Bone Joint Surg Am 1996; 78: 584–587. [DOI] [PubMed] [Google Scholar]
- 41.Slawski DP, Cahill BR. Atraumatic osteolysis of the distal clavicle. Results of open surgical excision. Am J Sports Med 1994; 22: 267–271. [DOI] [PubMed] [Google Scholar]
- 42.Martin SD, Baumgarten TE, Andrews JR. Arthroscopic resection of the distal aspect of the clavicle with concomitant subacromial decompression. J Bone Joint Surg Am 2001; 83A: 328–335. [DOI] [PubMed] [Google Scholar]
- 43.Lozman PR, Hechtman KS, Uribe JW. Combined arthroscopic management of impingement syndrome and acromioclavicular joint arthritis. J South Orthop Assoc 1995; 4: 177–181. [PubMed] [Google Scholar]
- 44.Snyder SJ, Banas MP, Karzel RP. The arthroscopic Mumford procedure: an analysis of results. Arthroscopy 1995; 11: 157–164. [DOI] [PubMed] [Google Scholar]
- 45.Levine WN, Barron OA, Yamaguchi K, Pollock RG, Flatow EL, Bigliani LU. Arthroscopic distal clavicle resection from a bursal approach. Arthroscopy 1998; 14: 52–56. [DOI] [PubMed] [Google Scholar]
- 46.Lesko PD. Variation of the arthroscopic Mumford procedure for resecting the distal clavicle. J South Orthop Assoc 2001; 10: 194–200. [PubMed] [Google Scholar]
- 47.Daluga DJ, Dobozi W. The influence of distal clavicle resection and rotator cuff repair on the effectiveness of anterior acromioplasty. Clin Orthop Relat Res 1989, pp. 117–123. [PubMed] [Google Scholar]
- 48.Pensak M, Grumet RC, Slabaugh MA, Bach BR., Jr Open versus arthroscopic distal clavicle resection. Arthroscopy 2010; 26: 697–704. [DOI] [PubMed] [Google Scholar]
- 49.Freedman BA, Javernick MA, O'Brien FP, Ross AE, Doukas WC. Arthroscopic versus open distal clavicle excision: comparative results at six months and one year from a randomized, prospective clinical trial. J Shoulder Elbow Surg 2007; 16: 413–418. [DOI] [PubMed] [Google Scholar]
- 50.Charron KM, Schepsis AA, Voloshin I. Arthroscopic distal clavicle resection in athletes: a prospective comparison of the direct and indirect approach. Am J Sports Med 2007; 35: 53–58. [DOI] [PubMed] [Google Scholar]