Abstract
Background
Bone-grafting procedures for recurrent shoulder instability produce low recurrence rates, although they are associated with complications such as graft non-union. Inadequate screw purchase is considered to play a causative role. However, excessive screw length can endanger neurovascular structures. The present study aimed to investigate how type and length of screws influences construct rigidity in a simplified glenoid model.
Methods
Testing was performed on composite polyurethane foam models with material properties and abstract dimensions of a deficient glenoid and an bone graft. Three screw types (cannulated 3.75 mm and 3.5 mm and solid 4.5 mm) secured the graft in a bicortical–bicortical, bicortical–unicortical and unicortical–unicortical configuration. Biomechanical testing consisted of applying axial loads when measuring graft displacement.
Results
At 200 N, graft displacement reached 0.74 mm, 0.27 mm and 0.24 mm for the unicortical–unicortical and 0.40 mm, 0.25 mm and 0.24 mm for the unicortical–bicortical configuration of the 3.75 mm, 3.5 mm and 4.5 mm screw types. The 3.75 mm screw incurred significant displacements in the unicortical configurations compared to the bicortical–bicortical method (p < 0.001).
Conclusions
The present study demonstrates that common screw types resist physiological shear loads in a bicortical configuration. However, the 3.75 mm screws incurred significant displacements at 200 N in the unicortical configurations. These findings have implications regarding hardware selection for bone-grafting procedures.
Keywords: biomechanical, coracoid, fixation, Latarjet, non-union, pseudarthrosis, screw
Introduction
Anterior glenoid rim reconstruction by bone grafting is increasingly used in the treatment of anterior shoulder instability.1 Coracoid process transfer procedures such as described by Latarjet2 and Bristow3, iliac crest grafts as described by Eden and Hybbinette4–6 and, recently, distal tibia7 and glenoid allografts8 have been used for this purpose. Large series have reported low recurrence rates after coracoid transfer procedures, demonstrating superiority over standard soft tissue repairs for high-risk patients. 9–11 However, anterior bone grafting procedures are associated with a 30% risk of complications and 7% risk of re-operation.12 Graft pseudarthrosis or non-union between the coracoid process and the glenoid neck is seen in 9.4% of cases after Bristow–Latarjet. Such non-unions are often incidental findings,13 yet symptomatic graft non-union may require revision surgery as a result of pain or recurrent instability.14–16 Revision surgery after failed anterior bone grafting is technically demanding and not without risk.14,15 The aetiology of graft pseudarthrosis is multifactorial. Bone-to-bone healing is influenced by contact gap, blood supply, hormonal milieu, neural regulation and mechanobiological environment.17–19 The initial shear fixation stability is a recognized parameter for successful healing and is directly influenced by the fixation method.20,21 Some studies have suggested a causative association between insufficient screw purchase and graft pseudarthrosis.22,23 However, rigid fixation must be weighed against the risks of excessive screw length such as neurological injury.24 The present study aimed to investigate whether screw design and length may influence glenoid-graft construct rigidity and thus contribute to graft non-union and failure.
Materials and Methods
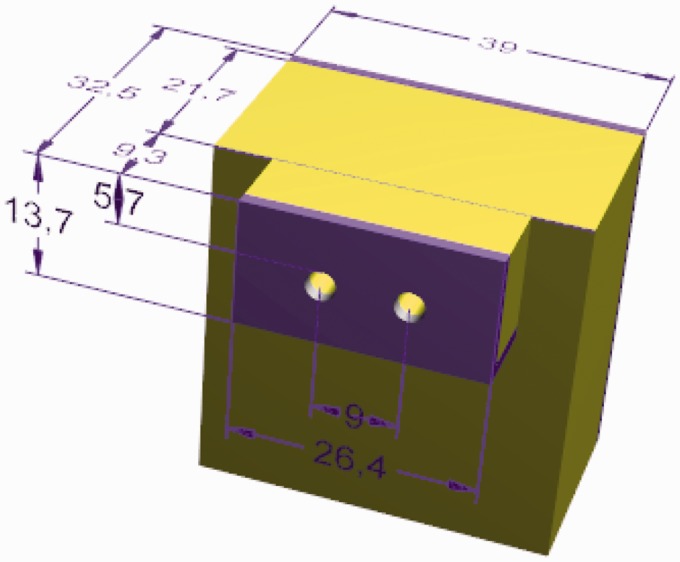
Testing was performed on polyurethane foam block models to limit the experimental difficulties resulting from the use of human cadaveric bone such as inconstant anatomical dimensions, degenerative changes and variable bone quality. The generic 20 pound/cubic foot rectangular foam blocks were fitted with a 2 mm thick short fibre filled epoxy resin laminate to replicate the material properties of cancellous bone with a cortical shell (Sawbones Inc., Vashon, WA, USA).25–27 The resin layer was machined down to a thickness of 1.5 mm to match physiological human glenoid cortex thickness.25 Cancellous and cortical density were 20 pounds/square foot and 102 pounds/square foot, respectively. The rectangular block measured 21.7 mm× 39 mm × 40 mm, representing the average glenoid width and height after creation of a 25% defect (Fig. 1).28 The anterior bone grafts were created from the same material. The composite graft dimensions, 13.7 mm× 9.3 mm× 26.4 mm were based on previously published measurements of harvested coracoid processes because these are the most frequently used grafts. However, a simple quadrangular shape was chosen to allow extrapolation of results to other types of grafts such as tibial plafond allografts and iliac crest autografts.29 Similarly to clinical conditions with significant glenoid bone loss, the model contains a flat anterior cancellous surface apposed to a flat cancellous graft surface.30
Figure 1.
Three-dimensional drawing of the stylized foam bone model consisting of coracoid with pilot drill holes and glenoid. Light colour indicates cancellous bone; darker colour indicates cortical bone. Measurements are shown in millimeters.
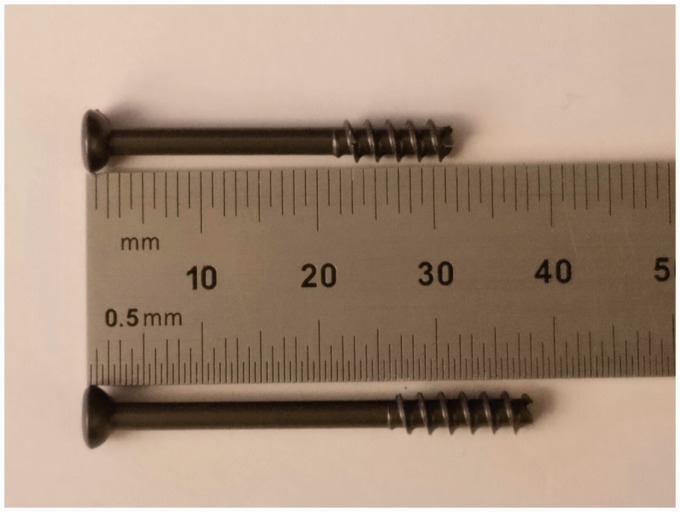
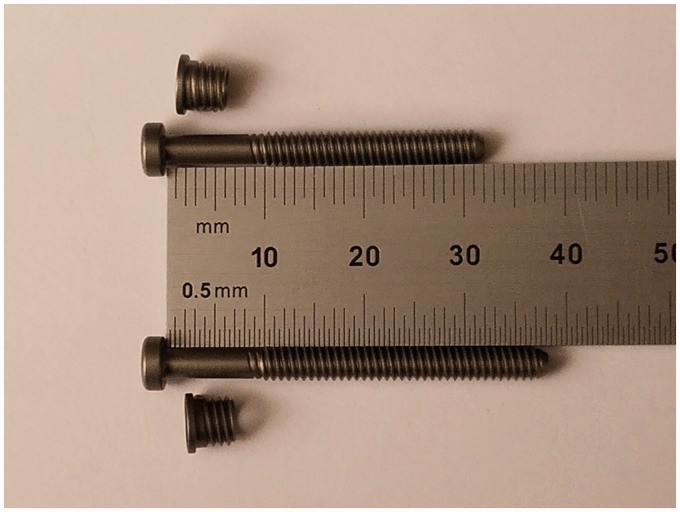
Three commonly used screws were selected for the experiment. The Arthrex 3.75 mm titanium cannulated screw (Arthrex, Naples, FL, USA) (Fig. 2), the Mitek 3.5 mm titanium cannulated Bristow–Latarjet Instability Shoulder Screw (Depuy Synthes Mitek Sports Medicine, Raynham, MA, USA) (Fig. 3) and the Synthes 4.5 mm steel Large Fragment LCP System Malleolar Screw (Synthes, West Chester, PA, USA) (Fig. 4). The Arthrex screws (major diameter 3.75 mm, shaft diameter 2.4 mm, thread pitch 1.8 mm), part of the Glenoid Bone Loss Instrument Set, are self-drilling, self-tapping screws. They are partially threaded, and a popular choice when performing a Congruent-Arc Latarjet procedure.31 The Mitek system (major diameter 3.5 mm, shaft diameter 3.0 mm, thread pitch 0.75 mm) includes titanium Top Hats, which are used as position holders and are inserted prior to screw insertion to prevent graft fracture. The partially threaded stainless steel Synthes screws (major diameter 4.5 mm, shaft diameter 2.9 mm, thread pitch 1.75 mm) are used for fracture fixation as part of the Synthes Large Fragment set. They are considered the ‘gold standard’ in glenoid bone block fixation. Technical specifications are listed in Table 1.30
Figure 2.
Photograph of the Arthrex 3.75 mm titanium cannulated screw.
Figure 3.
Photograph of the Mitek 3.5 mm titanium cannulated Bristow-Latarjet instability shoulder screw.
Figure 4.
Photograph of the Synthes 4.5 mm steel Large Fragment LCP System malleolar screw.
Table 1.
Specifications and dimensions of screws used in this study.
| Manufacturer | Description | Size | Part number | Nominal length (mm) | Intra-osseous length (mm) | Thread pitch | Shaft length | Thread length | Shaft/thread length ratio |
|---|---|---|---|---|---|---|---|---|---|
| Arthrex | Screw, partially Threaded | 3.75 | AR-7000-32S | 32 | 30 | 1.8 | 20 | 8 | 40% |
| AR-7000-38S | 38 | Bicortical | 1.8 | 24 | 10 | 42% | |||
| Mitek | Bristow – Latarjet instability shoulder screw | 3.5 | 285121 | 32 (modified to 30) | 30 | 0.75 | 10 | 20 | 200% |
| 285117 | 38 | Bicortical | 0.75 | 13 | 28 | 280% | |||
| Synthes | Malleolar screw | 4.5 | 215.035 | 35 | 30 | 1.75 | 10 | 12 | 92% |
| 215.045 | 45 | Bicortical | 1.75 | 10 | 16 | 84% |
Short and long screws lengths were selected for each screw type (Table 1). Combinations of short and/or long screws allowed for testing in three configurations: (i) both screws with unicortical purchase (unicortical–unicortical); (ii) one unicortical and one bicortical screw (unicortical–bicortical); and (iii) both screws with bicortical purchase (bicortical–bicortical). Six constructs of each screw type and length configuration were produced, amounting to a total of 54 models. Short screw lengths were selected from the manufacturer’s available range per type to minimize the variability of effective intraglenoidal length. Intra-osseous length was set at 30 mm for all screws (Table 1), replicating a realistic intra-operative scenario. Long screw lengths were chosen to guarantee bicortical purchase beyond the screws' spike tip. Two parallel pilot holes were drilled 9 mm apart, centred on the anterior cortical graft side and tapped according to the manufacturer’s instructions. Screws were inserted and tightened with a digital torque measuring screw driver (Model STC50CN; Tonichi, Buffalo Grove, IL, USA). Average torque of ‘two-finger tightness’ was determined from the authors’ mean torque measurements.
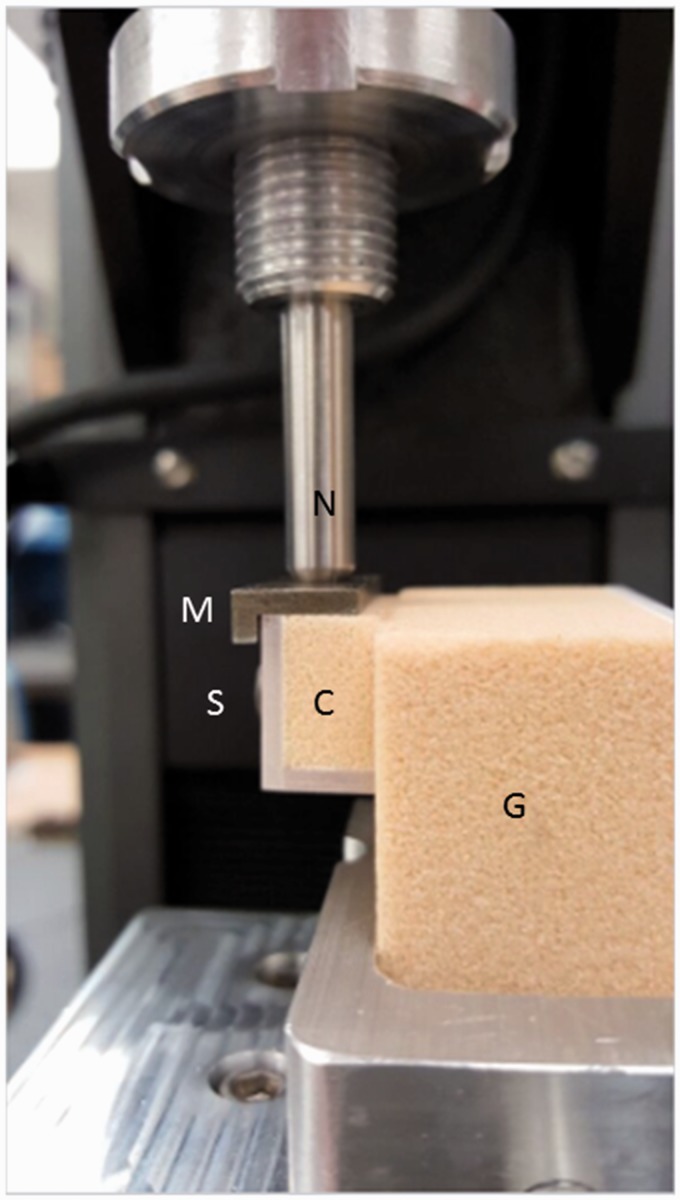
After screw insertion, bone blocks were loaded into a vice and subjected to a cyclic loading staircase protocol based on previous work by Giles et al.32,33 Testing apparatus consisted of an Instron Model 5944 (Instron, Norwood, MA, USA). The system was manually pre-loaded with 2 N to 5 N of force centered on the ‘articular’ side of the graft removing all slack from the system. The load and displacement of the grafts were then zeroed and the staircase protocol initiated. Loads were applied evenly with the help of a metal plate covering the lateral or ‘articular’ surface of the graft. These simulated loads are an approximation of physiological loading that may occur in the immediate postoperative period.34 Additional loading of the graft by action of the conjoint tendon was omitted from our experiment for three reasons. First, this allows generalization of the results to all types of grafts, not exclusively the coracoid process grafts of the Latarjet-type procedures. Second, the direction and magnitude of conjoint tendon pull in the postoperative period has not been quantified accurately in the literature. Third, construct fixation strength is not considered to differ greatly between simulated loads in a pulling or pushing mode. Loading was repeated for 100 cycles at a frequency of 1 Hz. Load increments were 0 N to 5 N, 5 N to 10 N, 10 N to 25 N, 25 N to 50 N, 50 N to 100 N, 100 N to 150 N and 150 N to 200 N. Graft displacement was measured continuously (Fig. 5). Failure was set at 0.8 mm of shear displacement, based on previously published fracture healing data.20,21
Figure 5.
Photograph of mounted model during load application. G, glenoid model; C, coracoid model; S, screwhead; M, metal plate; N, loading nose.
Statistical analysis
Graft displacement was recorded as the final displacement during the last cycle of each loading increment. If an 0.8 mm displacement was achieved before maximum loading was completed, the cyclic loading was discontinued and the load and displacement at that point recorded. Statistical analyses of displacement data was performed by means of an analysis of variance (ANOVA) test for each loading step. In the case of a significant result, further analysis composed by a series of t-tests was performed. p < 0.05 was considered statistically significant. Power analyses were calculated with pilot data a priori, indicating that six models per condition would achieve a minimum power of β = 0.8.
Results
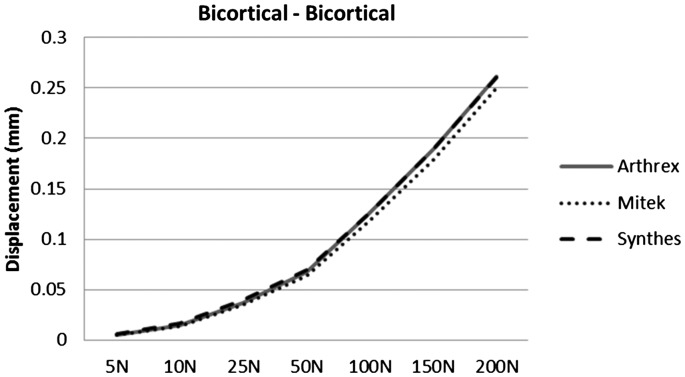
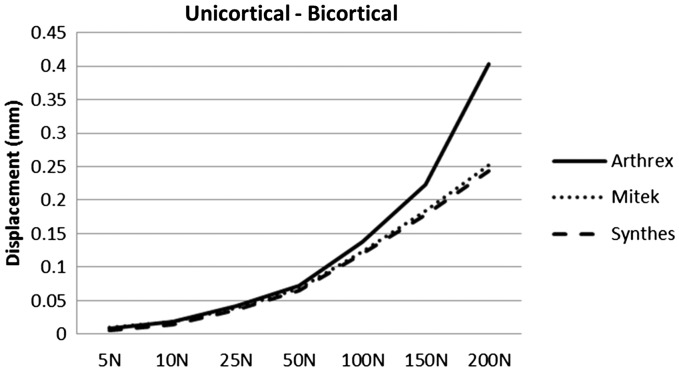
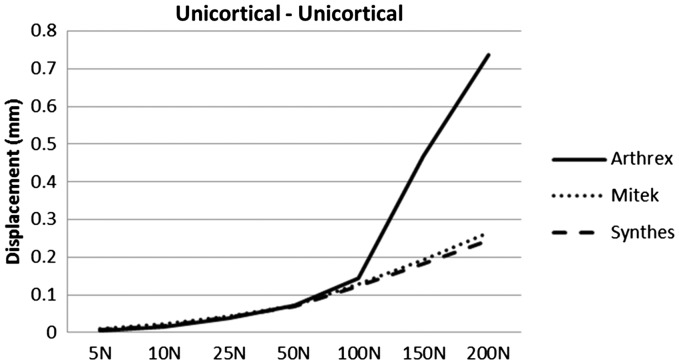
Graft configuration with two bicortical screws demonstrated maximal displacements of 0.26 mm, 0.26 mm and 0.25 mm (SD 0.01 mm, 0.02 mm and 0.04 mm) at 200 N loads for the cannulated Arthrex 3.75, cannulated Mitek 3.5 and solid Synthes 4.5 screws, respectively (Fig. 6). ANOVA statistical analysis did not show a significant difference between the final displacements at any of the incremental loads. Graft fixation with a unicortical and a bicortical screw exhibited a significant difference in final displacements at 100 N (p = 0.016), 150 N (p = 0.003) and 200 N (p = 0.002). Maximal displacement at 200 N reached 0.40 mm, 0.25 mm and 0.24 mm (SD 0.12 mm, 0.02 mm and 0.01 mm) for the respective screw types (Fig. 7). Similarly, graft fixation with two unicortical screws resulted in a significant difference of displacements at 100 N (p = 0.005), 150 N (p < 0.001) and 200 N (p < 0.001). Maximal observed graft displacements were 0.74 mm, 0.27 mm and 0.24 mm (SD 0.04 mm, 0.01 mm and 0.01 mm) for Arthrex, Mitek and Synthes screws, respectively (Fig. 8).
Figure 6.
Line chart showing displacement (mm) versus loading (N) for the bicortical–bicortical configuration.
Figure 7.
Line chart showing displacement (mm) versus loading (N) for the bicortical–unicortical configuration.
Figure 8.
Line chart showing displacement (mm) versus loading (N) for the unicortical-unicortical configuration.
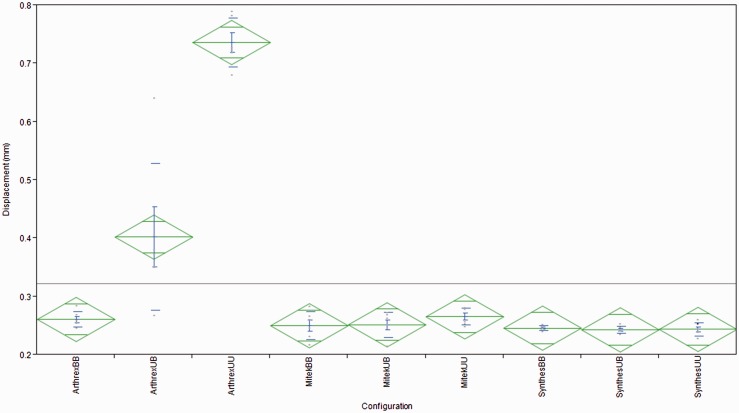
ANOVA per screw type revealed a significant statistical difference at 200 N for the cannulated Arthrex screw 3.75 mm between the two unicortical and two bicortical configurations, as well as between the two unicortical and unicortical–bicortical configurations. The observed displacements were 0.74 mm (SD 0.04 mm) and 0.26 mm (SD 0.01 mm) (p < 0.001) and 0.74 mm (SD 0.04 mm) and 0.40 mm (SD 0.13 mm) (p < 0.001). ANOVA comparison between the unicortical–bicortical and two bicortical configurations did not reach statistical significance. Similarly, comparisons for the cannulated Mitek 3.5 mm screws showed a trend towards greater displacements in the unicortical fixation compared to the unicortical–bicortical or bicortical fixation. However, these differences were not statistically significant. The solid Synthes 4.5 mm screws at the 200 N loading demonstrated the smallest variation of all three screw types. There were there no statistically significant differences in graft displacement between the three configurations, nor were there any trends (Fig. 9).
Figure 9.
Diamond plot showing displacement (mm) per configuration per screw-type. Green diamonds indicate confidence interval. Blue error bar indicates mean error. Blue lines indicate standard deviation. BB, bicortical–bicortical; UB, unicortical–bicortical; UU, unicortical–unicortical.
Discussion
The Latarjet–Bristow and similar anterior glenoid bone grafting procedures are increasingly used in the treatment of patients with recurrent shoulder instability and glenoid bone deficiency.1 Although recurrence is infrequent or even absent in some series,9,35,36 a relatively high complication and reoperation rate has been reported.12,13,37,38 Clinical studies have shown the importance of correct graft-to-bone healing.14–16 However, construct strength and rigidity have to be weighed against hardware complications. As such, the fixation technique remains an area of debate.
The present biomechanical study confirms that three screw types, commonly used in the setting of glenoid bone grafting, resist repetitive physiological shear loads without clinically significant displacement when both screws attain bicortical purchase. Additionally, the present study demonstrates that, where the cannulated Mitek and solid Synthes screws performed satisfactorily in a unicortical–unicortical and unicortical–bicortical configuration, the cannulated Arthrex screws showed significantly larger shear displacement during the higher loads in those configurations. The Arthrex screws exhibited the smallest shaft diameter, the coarsest pitch, a larger thread rise and the lowest shaft/thread length ratio of the three screw types in this experiment (Table 1). The mechanism behind the inferior performance in unicortical configuration may be a result of a combination of the smaller amount of cancellous ‘bone’ in shear (coarse pitch and short thread length), the larger bending moment about the fulcrum point (low shaft/thread length ratio) and the passage of large threads creating bone voids (large thread rise), which may weaken the supportive bone stock.
Studies examining the biomechanical rigidity of fixation techniques for glenoid bone loss are sparse. Weppe et al.22 compared the load to failure of a bicortical screw technique versus a bioabsorbable interference screw. In ten cadaver specimens, the median load to failure was 202 N and 110 N for the bicortical screws and the interference screw, respectively. Alvi et al.34 compared energy and cycles to failure between 3.5 mm stainless steel cortical screws and 4.0 mm stainless steel partially threaded cannulated cancellous screws. No statistically significant differences in either parameter were found.
Load to catastrophic failure is an important parameter; however, in the present study subclinical displacement was chosen as the primary outcome parameter. The experimental set-up aimed to recreate the immediate postoperative environment before bony healing occurs. It was not the intention to simulate in vivo loading of anterior glenoid bone grafts in the present study, merely to assess immediate postoperative construct stability. Although, active motion is typically deliberately minimized during this postoperative period, it is assumed that early micromotion plays a role in the development of pseudarthrosis. The threshold for clinically significant displacement of the graft was based on previous literature on fracture healing as adopted by Giles et al.32
Non-union of a coracoid or other bone block following an anterior glenoid augmentation procedure is a recognized and clinically significant complication. Non-union may result in recurrent instability and the need for revision surgery. Griesser et al.12 evaluated performed a systematic review, analyzing 45 studies (1904 shoulders). They reported a non-union rate of 9.1%.12 Mizuno et al.11 reported an incidence of 1.5% in a series of 68 patients and Dumont36 reported an incidence of 1.7% in a series of 62 patients. It has, however, been established that standard radiographic techniques are not suited to evaluate bony healing accurately.39
Graft position may play a role in the development of graft pseudarthrosis. Grafts placed inferiorly on the glenoid can lead to poor inferior screw purchase and decreased rotational stability, resulting in a weak biomechanical construct.22 Grafts placed too cranially can lead to recurrent instability40,41 or suprascapular nerve injury.24,42 Grafts placed too medial or lateral can result in recurrence or secondary osteoarthritis, respectively.43,44 Willemot et al.45 recently described ideal graft positioning in the sagittal plane depending on the direction of dislocation. Proponents of arthroscopic anterior glenoid grafting procedures have cited more accurate graft placement under direct visualization as a possible advantage over open procedures.46
Screw depth has not been studied extensively in its relationship to graft fixation. Although most technique guides stress the placement of both superior and inferior screws in a bicortical fashion to maximize fixation strength, it is our experience that evaluation of bicortical position without the use of a postoperative computed tomography scan can be difficult. To avoid complications associated with excessive posterior screw protrusion, some surgeons will accept one or two unicortical screws. The results of the present study suggest that some commonly used solid and cannulated screws allow for one or even both screws to be placed in a unicortical manner without compromising the construct rigidity.
Limitations
The limitations of the present study were those inherent to a biomechanical study using clinical parameters in a nonclinical testing environment. The decision to use Sawbones (Sawbone Inc.) was made to increase the reproducibility and uniformity of the experiment. Most biomechanical studies related to graft fixation are performed on cadavers, yet the variability of cadaveric bone has been shown to be highly unpredictable. Mechanical properties of cadaver bone have up to 19 times the inter-specimen variability compared to uniform bone models.47 An abstract rectangular representation of the glenoid and graft was chosen instead of an exact anatomic model. This allowed for the elimination of anatomic and mechanical variability as a confounding factor. Moreover, in the case of large glenoid defects, a relatively flat cancellous anterior glenoid surface is mated with a prepared flat cancellous graft surface, which is why it was considered that an abstract flat shape would not diminish the applicability of the results. However, the use of non-anatomic geometry remains a limitation of the present study. The conjoint tendon, capsular structures and rotator cuff action may influence graft loading postoperatively. Human factors that may affect micromotion at time zero such as soft tissue and conjoint tendon traction were not simulated in this experimental set-up. Furthermore, although the cyclic loading protocol is a peer-reviewed standard for testing graft fixation strength, this experiment did not aim to simulate the actual physiological loading environment after anterior glenoid bone grafting. The intention of the test was to assess different graft fixation modalities under carefully controlled laboratory settings.
Conclusions
The present study confirms that three common screw types used for fixation of bone grafts to the glenoid can resist simulated physiological shear loads when placed in a bicortical–bicortical configuration. Furthermore, the present study shows that the cannulated 3.5 mm Mitek and solid 4.5 mm Synthes screws were also able to resist the applied loads without producing clinically significant displacement in either a unicortical/bicortical or unicortical/unicortical configuration, whereas the 3.75 mm cannulated Arthrex screws failed to do so. Further studies are required to validate the findings and explore biomechanical rigidity of novel fixation techniques.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: J. Burns, A. Castagna and O. Verborgt are paid consultants for ConMed Linvatec. The study was performed at the research facilities of ConMed Linvatec. ConMed Linvatec products were not tested as part of this study. There exists no financial bias related to the subject of this experiment.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical review and Patient Consent
Ethical review and patient consent were not required for this non-cadaveric biomechanical study.
Level of evidence
Basic science
References
- 1.Beran MC, Donaldson CT, Bishop JY. Treatment of chronic glenoid defects in the setting of recurrent anterior shoulder instability: a systematic review. J Shoulder Elbow Surg 2010; 19: 769–780. [DOI] [PubMed] [Google Scholar]
- 2.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir 1954; 49: 994–997. [PubMed] [Google Scholar]
- 3.Helfet AJ. Coracoid transplantation for recurring dislocation of the shoulder. J Bone Joint Surg Br 1958; 40B: 198–202. [DOI] [PubMed] [Google Scholar]
- 4.Warner JJP. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med 2006; 34: 205–212. [DOI] [PubMed] [Google Scholar]
- 5.Steffen V. Rim reconstruction with autogenous iliac crest for anterior glenoid deficiency: forty-three instability cases followed for 5–19 years. J Shoulder Elbow Surg 2013; 22: 550–559. [DOI] [PubMed] [Google Scholar]
- 6.Auffarth A, Kralinger F, Resch H. Anatomical glenoid reconstruction via a J-bone graft for recurrent posttraumatic anterior shoulder dislocation. Oper Orthop Traumatol 2011; 23: 453–461. [DOI] [PubMed] [Google Scholar]
- 7.Provencher MT, Ghodadra N, LeClere L, et al. Anatomic osteochondral glenoid reconstruction for recurrent glenohumeral instability with glenoid deficiency using a distal tibia allograft. Arthroscopy 2009; 25: 446–452. [DOI] [PubMed] [Google Scholar]
- 8.Skendzel JG, Sekiya JK. arthroscopic glenoid osteochondral allograft reconstruction without subscapularis takedown: technique and literature review. Arthroscopy 2011; 27: 129–135. [DOI] [PubMed] [Google Scholar]
- 9.Hovelius LK, Sandstrom BC, Rosmark DL, et al. Long-term results with the Bankart and Bristow-Latarjet procedures: recurrent shoulder instability and arthropathy. J Shoulder Elbow Surg 2001; 10: 445–452. [DOI] [PubMed] [Google Scholar]
- 10.Bessiere C, Trojani C, Carles M, et al. The open Latarjet procedure is more reliable in terms of shoulder stability than arthroscopic Bankart repair. Clin Orthop Relat Res 2014; 472: 2345–2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mizuno N, Denard PJ, Raiss P, et al. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 2014; 23: 1691–1699. [DOI] [PubMed] [Google Scholar]
- 12.Griesser MJ, Joshua HD, Hussain WM, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg 2013; 22: 286–292. [DOI] [PubMed] [Google Scholar]
- 13.Gupta A, Delaney R, Petkin K, et al. Complications of the Latarjet procedure. Curr Rev Musculoskelet Med 2015; 8: 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lunn JV, Castellano-Rosa J, Walch G. Recurrent anterior dislocation after the Latarjet procedure: Outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elbow Surg 2008; 17: 744–750. [DOI] [PubMed] [Google Scholar]
- 15.Young DC, Rockwood CA. Complications of a failed Bristow procedure and their management. J Bone Joint Am 1991; 73: 969–981. [PubMed] [Google Scholar]
- 16.Boileau P, Mercier N, Old J. Arthroscopic Bankart- Bristow-Latarjet (2B3) procedure: how to do it and tricks to make it easier and safe. Orthoped Clin NA 2010; 41: 381–392. [DOI] [PubMed] [Google Scholar]
- 17.Claes L, Augat P, Suger G, et al. Influence of size and stability of the osteotomy gap on the success of fracture healing. J Orthop Res 1997; 15: 577–84. [DOI] [PubMed] [Google Scholar]
- 18.Einhorn TA. The science of fracture healing. J Orthop Trauma 2005; 19: S4–S6. [DOI] [PubMed] [Google Scholar]
- 19.Jagodzinski M, Krettek C. Effect of mechanical stability on fracture healing – an update. Injury 2007; 38(Suppl 1): S3–S10. [DOI] [PubMed] [Google Scholar]
- 20.Schell H, Epari DR, Kassi JP, et al. The course of bone healing is influenced by the initial shear fixation stability. J Orthop Res 2005; 23: 1022–108. [DOI] [PubMed] [Google Scholar]
- 21.Augat P, Burger J, Schorlemmer S, et al. Shear movement at the fracture site delays healing in a diaphyseal fracture model. J Orthop Res 2006; 21: 1011–1017. [DOI] [PubMed] [Google Scholar]
- 22.Weppe F, Magnussen RA, Lustig S, et al. A biomechanical evaluation of bicortical metal screw fixation versus absorbable interference screw fixation after coracoid transfer for anterior shoulder instability. YJARS 2011; 27: 1358–1363. [DOI] [PubMed] [Google Scholar]
- 23.Walch G, Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. TSES 2000; 1: 256–261. [Google Scholar]
- 24.Lädermann A, Denard PJ, Burkhart SS. Injury of the suprascapular nerve during Latarjet procedure: an anatomic study. YJARS 2012; 28: 316–321. [DOI] [PubMed] [Google Scholar]
- 25.Mimar R, Limb D, Hall RM. Evaluation of the mechanical and architectural properties of glenoid bone. J Shoulder Elbow Surg 2008; 17: 336–41. [DOI] [PubMed] [Google Scholar]
- 26.Lehtinen JT, Tingart MJ, Apreleva M, et al. Total, trabecular, and cortical bone mineral density in different regions of the glenoid. J Shoulder Elbow Surg 2004; 13: 344–348. [DOI] [PubMed] [Google Scholar]
- 27.Tingart MJ, Apreleva M, Lehtinen J, et al. Anchor design and bone mineral density affect the pull-out strength of suture anchors in rotator cuff repair: which anchors are best to use in patients with low bone quality? Am J Sports Medicine 2004; 32: 1466–1473. [DOI] [PubMed] [Google Scholar]
- 28.Iannotti JP, Gabriel JP, Schneck SL, et al. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg 1992; 74: 491–500. [PubMed] [Google Scholar]
- 29.Young AA, Baba M, Neyton L, et al. Coracoid graft dimensions after harvesting for the open Latarjet procedure. J Shoulder Elbow Surg 2012; 22: 485–488. [DOI] [PubMed] [Google Scholar]
- 30.Young AA, Maia R, Berhouet J, et al. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg 2011; 20: S61–S69. [DOI] [PubMed] [Google Scholar]
- 31.Burkhart SS, De Beer JF, Barth JRH, et al. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy: J Arthroscopic Rel Surg 2007; 23: 1033–1041. [DOI] [PubMed] [Google Scholar]
- 32.Giles JW, Puskas G, Welsh M, et al. Do the traditional and modified latarjet techniques produce equivalent reconstruction stability and strength? Am J Sports Med 2012; 40: 2801–2807. [DOI] [PubMed] [Google Scholar]
- 33.Giles JW, Puskas GJ, Welsh MF, et al. Suture anchor fixation of bony Bankart fractures: comparison of single-point with double-point ‘suture bridge’ technique. Am J Sports Med 2013; 41: 2624–2631. [DOI] [PubMed] [Google Scholar]
- 34.Alvi HM, Monroe EJ, Muriuki M, et al. Latarjet fixation: a cadaveric biomechanical study evaluating cortical and cannulated screw fixation. Orthop J Sports Med 2016; 4 2325967116643533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mizuno K, Nabeshima Y, Hirohata K. Analysis of Bankart lesion in the recurrent dislocation or subluxation of the shoulder. Clin Orthop Relat Res 1993; 288: 158–165. [PubMed] [Google Scholar]
- 36.Dumont GD, Fogerty S, Rosso C, et al. The arthroscopic latarjet procedure for anterior shoulder instability: 5-year minimum follow-up. Am J Sports Med 2014; 42: 2560–2566. [DOI] [PubMed] [Google Scholar]
- 37.Joshi MA, Young AA, Balestro J-C, et al. The Latarjet-Patte procedure for recurrent anterior shoulder instability in contact athletes. Clin Sports Med 2013; 32: 731–739. [DOI] [PubMed] [Google Scholar]
- 38.Shah AA, Butler RB, Romanowski J, et al. Short-term complications of the Latarjet procedure. J Bone Joint Surg 2012; 94: 495–501. [DOI] [PubMed] [Google Scholar]
- 39.Kraus TM, Graveleau N, Bohu Y, et al. Coracoid graft positioning in the Latarjet procedure. Knee Surg Sports Traumatol Arthrosc 2016; 24: 496–501. [DOI] [PubMed] [Google Scholar]
- 40.Hovelius L, Körner L, Lundberg B, et al. The coracoid transfer for recurrent dislocation of the shoulder. Technical aspects of the Bristow-Latarjet procedure. J Bone Joint Surg 1983; 65: 926–934. [PubMed] [Google Scholar]
- 41.Huguet D, Pietu G, Bresson C, et al. Anterior instability of the shoulder in athletes: apropos of 51 cases of stabilization using the Latarjet-Patte intervention. Acta Orthop Belg 1996; 62: 200–206. [PubMed] [Google Scholar]
- 42.Shishido H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: an anatomic study. J Shoulder Elbow Surg 2001; 10: 372–376. [DOI] [PubMed] [Google Scholar]
- 43.Young A, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg 1998; 80: 841–852. [DOI] [PubMed] [Google Scholar]
- 44.Hovelius L, Sandström B, Olofsson A, et al. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg 2012; 21: 647–660. [DOI] [PubMed] [Google Scholar]
- 45.Willemot LB, Eby SF, Thoreson AR, et al. Iliac bone grafting of the intact glenoid improves shoulder stability with optimal graft positioning. J Shoulder Elbow Surg 2015; 24: 533–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Verborgt O, Van den Bogaert G, Debeer P. Arthroscopic bone block augmentation of the anterior glenoid through the rotator interval: a cadaveric feasibility study. J Shoulder Elbow Surg 2013; 22: 458–462. [DOI] [PubMed] [Google Scholar]
- 47.Little JP, Horn TJ, Marcellin-Little DJ, et al. Development and validation of a canine radius replica for mechanical testing of orthopedic implants. Am J Vet Res 2012; 73: 27–33. [DOI] [PubMed] [Google Scholar]