Abstract
The Latarjet procedure is a well-known, safe and reliable technique to treat primary or recurrent anterior dislocations or subluxations, with or without hyperlaxity, with or without glenoid bone loss. Both the open and the arthroscopic methods produce excellent clinical results, with a low rate of recurrent instability. There have been concerns of a higher surgical complication rate associated with this procedure, however, large reviews reported an overall complication rate in the open Latarjet procedure of 15%. Meticulous surgical technique and a good understanding of the local anatomy can help to avoid the complications but postoperative shoulder arthritis and frequent bone block osteolysis remain unsolved additional challenges, which require further research. There are 2 main factors to further improve the clinical outcome and patient satisfaction: careful patient selection with good surgical indication, and reducing complications with adequate surgical techniques. The aim of this study is to provide the current overview of the contraindications and complications of the Latarjet procedure.
Keywords: anterior instability, complications, contraindications, Latarjet procedure, shoulder, shoulder instability
Introduction
Recurrent anterior shoulder instability is often caused by glenoid and/or humeral bony defects additional to the soft tissue injuries.1–3 Increased surgical failure of the soft tissue repair alone is usually associated with significant bony defects or inadequate soft tissue availability.1–3 For this reason, patients with bony defects and recurrent anterior shoulder instability were managed with different glenoid restoring procedures, In 1954, Latarjet suggested that the coracoid process can be transferred and fixed with a screw to the margin of the glenoid.4 This bone block technique with an augmentation of the anteroinferior part of the glenoid has clear advantages especially in cases with significant bone loss, although the mechanism is still not fully understood. The possible mechanism has been described previously as a triple effect:5
The dynamic ‘sling’ effect of the conjoint tendon acting on the subscapularis and capsule in certain arm position (probably the most important effect6).
The ‘bony effect’ of increasing the glenoid surface area.
The ‘Bankart effect’ of repairing the capsulolabral complex to the bone or the stump of the coraco-acromial ligament (CAL) to the capsule.
This open technique also has several modifications: (i) CAL repair to the capsule; (ii) the use of two screws for stable fixation of the bone block; and (iii) the subscapularis horizontal splitting approach, which can protect the muscle and allow for immediate postoperative exercises even in external rotation.5,7,8 Further variations have been reported recently: the position and alignment of the transferred coracoid,9,10 including intra- or extra-articular placement (which may reduce postoperative osteoarthritis11), techniques of bone block fixation12–15 with or without the repair of the capsulolabral structures, and performing the surgery arthroscopically assisted.16–19
Although the reported clinical results and outcomes are usually successful with this procedure, several complications have also been reported, including infection, frozen shoulder, haematoma formation, symptomatic implants, fracture or non-union of the coracoid graft, neurological complications, arthritis and recurrence of instability. In particular, the risk of recurrence and the long-term outcomes of this procedure strongly depend on the correct positioning of the bone graft. A position that is too lateral or overhangs may result in the graft causing cartilage damage on the humeral head and early osteoarthritis.20,21,22–24 A position that is too medial is associated with a higher risk of recurrence.25,26
Previously, there have been some concerns about the rate of these complications after the Latarjet procedure, although more recent large reviews described an overall complication rate of 15% with the open Latarjet procedure.27
Excellent clinical results have been reported with both the open and the arthroscopic techniques, with a low rate of failure;15 however, on the basis of the current data, the open technique is probably still considered the gold standard because the arthroscopic technique is more time-consuming and has higher direct costs.28
It is well-known that primary or recurrent anterior dislocations or subluxations, with or without glenoid bone loss and hyperlaxity, are the best indications for the Latarjet procedure.8 However, there are two main factors to further improve the clinical outcomes and patient satisfaction: (i) careful patient selection with good indication and (ii) avoiding complications with adequate surgical techniques. These factors are discussed in the present review.
Contraindications of the Latarjet procedure
Recurrent anterior instability associated with massive irreparable rotator cuff tear and in the older population (>50 years old)
Instability can be associated with rotator cuff tears in older patients.29–34 The indication for surgery is based on the instability or the pain secondary to the rotator cuff tear. The type of the surgical technique depends on the reparability of the rotator cuff, which requires assessment with systematic preoperative imaging (the size and retraction of the tear, fatty infiltration of the rotator cuff muscle). If there is repairable cuff tendon and no significant glenoid bone loss, then Bankart repair with the management of the rotator cuff is a good solution. Walch et al.8 have also reported successful Latarjet procedure combined with open rotator cuff repair (small- to medium-sized supraspinatus tears) using the same surgical incision but rotating the arm to help the surgical exposure. Arthroscopic techniques may be an ideal solution, although its results need to be further evaluated. Currently, there is no evidence in literature, although recent research project may further clarify the results of the Latarjet technique in older patients, especially the potentially increased risk of bone block complications (fracture, non-union) as a result of the bone quality and accelerated degenerative changes (Domos and Walch, unpublished data). In our experience, the Latarjet surgery is a relative contraindication in older patients because we observed two kinds of special complex complications:
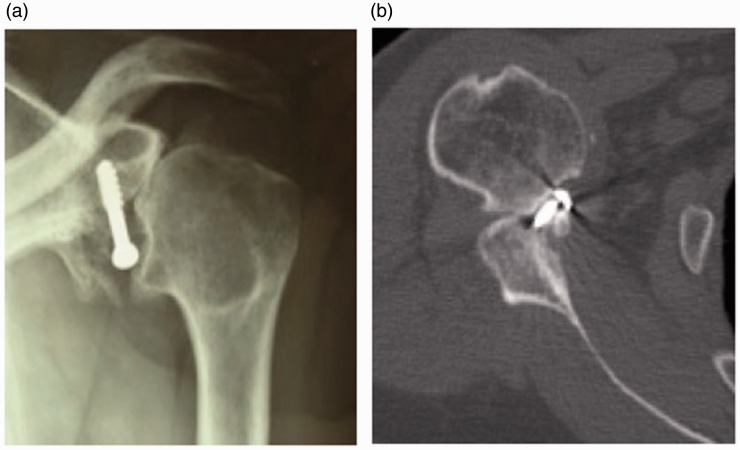
Static anterior instability of the humeral head (HH), with anteroinferior subluxation and progressive osteonecrosis of the HH in contact with the bone block (Fig. 1).
Irreducible inferior subluxation of the HH: this is probably caused by the non-elastic part of the subscapularis, which is pulled down by the transferred coracoid and the conjoint tendon, consequently allows permanent and irreducible humeral head subluxation (Fig. 2).
Figure 1.
Static anterior instability of the humeral head (HH) and avascular necrosis of HH in contact with bone block. (a) Antero-posterior plain radiograph. (b) Axial computed tomography scan.
Figure 2.
Inferior static subluxation of the humeral head after Latarjet procedure in a 55-year-old lady.
When the rotator cuff is not repairable (severe fatty infiltration, retraction), the Latarjet procedure is contraindicated. Walch et al.35 recommended primarily treating the instability because the management of the cuff tear depends on the status of the involved soft tissues, the patients’ age and motivation. In this case, an isolated stabilization by the Trillat procedure restored the stability in 86% of the patients; however, this type of surgery has 64% of the rate of osteoarthritis in the older age group.35 After failure of these procedures, reverse shoulder arthroplasty (RSA) remains the only possible surgical treatment.
First traumatic dislocation in the older population with or without large glenoid rim fracture
This is also relative contraindication of the Latarjet procedure, for the above-mentioned reasons, and the usually successful conservative treatment should be the first-line method if concentric HH position is associated with even a largely displaced glenoid fragment.36
Voluntary anterior dislocators or subluxators
These are absolute contraindications to the Latarjet procedure because laxity is difficult to correct by surgery. The results reported in this group of patients were always extremely poor37 with many medicolegal and litigation issues and a long-term special non-operative regime should be the initial option.
Patients with uncontrolled epilepsy
When neurological treatment is not or only partially efficient, any recurrence of seizures leads to fracture of the coracoid bone block, with a typical 90° bending of the two screws (Fig. 3). Complete neurological stability and control is mandatory before undertaking the treatment of recurrent shoulder dislocation in epileptic patients.38
Figure 3.
Typical aspect of failure after Latarjet procedure in epileptic patient: large Hill-Sachs lesion and bending of the screws.
Unstable painful shoulder and microinstability
The young athlete with vague shoulder pain is a common problem. This can be challenging to diagnose and is often caused by SLAP (superior labrum anteroposterior) lesions, partial rotator cuff tears, internal impingement or biceps pathologies.39–44 Anteroinferior instability of the shoulder without any subluxation or dislocation episodes can be another diagnosis as described by Boileau et al.45 This form of shoulder instability, which has been termed ‘unstable painful shoulder’, is often misdiagnosed. It usually involves the young athlete with hyperlaxity, with a history of forceful overextension or direct trauma to the shoulder, presenting with localized pain anteriorly, which can be reproduced with the anterior apprehension test (arm in abduction and external rotation = ABER) and relieved with the relocation test. Arthroscopic techniques with labrum reinsertion or anteroinferior capsule plication, or both, can lead to a successful treatment and a return to sport.
Microinstability is a new concept so no well-accepted definition yet exists. It describes any rotational or directional pathological laxity that leads to abnormal shoulder mechanics without dislocation.41,46 Microtrauma, inactivity or immobilization can be the cause and, initially, conservative treatment is recommended by managing the aggravating factor (e.g. abnormal throwing mechanics). If symptoms are persistent, surgery with standard arthroscopic techniques may be appropriate.
We can consider both of these described conditions as anterior instability usually without Bankart lesion (i.e. in a throwing athlete), which is contraindication to the Latarjet procedure.
Prosthetic anterior instability (subluxation or dislocation)
Prosthetic instability, after anatomic total shoulder arthroplasty, is one of the main reasons for reintervention. The main causes are soft tissue deficiency (i.e subscapularis rupture), bone loss, or malpositioning of humeral and/or glenoid components as a result of technical mistakes. It is the most difficult complication to manage, as seen from the high rate of recurrences.47 If there are adequate component positions, then subscapularis reconstruction,48 pectoralis major tendon transfer49 and autograft/allograft reconstruction of the anterior capsule50,51 are possible treatment options, with variable results. A case report also described the Latarjet procedure, which achieved a successful treatment of an unstable anatomic total shoulder arthroplasty.47 Because no appropriate evidence yet exists, we believe that these conditions are not successfully addressed with a Latarjet procedure and RSA is a more reliable salvage procedure.
Locked anterior dislocation
Locked anterior dislocation typically results not only from trauma or seizure,52 but also may be seen with massive rotator cuff tear as described by Neer.53 Concomitant lesions are common, including Hill-Sachs and Bankart lesions; massive glenoid bone loss, rotator cuff tears and subsequently severe glenohumeral osteoarthritis also occur.52,54 The results of different procedures, such as Bankart capsulolabral repair, remplissage, coracoid transfer, bone-grafting for younger patients and arthroplasty, have been reported.14,55–58 However, the ability to restore the stability of the shoulder is variable and the overall failure rate is fairly high. Chronic locked anterior shoulder dislocation is rarely reported, and most of the studies were only case reports or small case series.52,57,59–61 In our opinion, this pathology should not be treated with Latarjet technique because of the risk of redislocation, HH osteonecrosis and osteoarthritis. In elderly patients conservative treatment or (if symptomatic) RSA are advised.
Post-traumatic inferior subluxation
This is a relatively rare transient phenomenon as a result of temporary deltoid inhibition. Because it spontaneously resolves with conservative treatment, it does not need to be treated surgically and the Latarjet procedure does not help to reduce this problem.62
Static anterior subluxation
The static anterior subluxation of the humeral head with coracoid impingement, as observed in massive rotator cuff tears involving the subscapularis tendon, and as in the case of prosthetic instabilities, is not successfully corrected with the Latarjet procedure, which is contraindicated in our experience.
Anterior instability with intraarticular incarceration of the subscapularis and/or the long head of the biceps
These are rare pathologies and, in our opinion, they are also relative contraindications for Latarjet procedure.
Complications of the Latarjet procedure
Recurrence
The reported recurrence rate of instability after Latarjet procedure can be as low as 1% to 3%, with appropriate indication and technique.8,15 Failures are related to either incorrect patient selection, technical errors or complications: fracture of the coracoid process, malpositioning of the coracoid (too medial or too low) so the humeral head can dislocate above the transferred coracoid process. The ideal position of the graft is flush with the articular surface in the axial, and below the equator of the glenoid, in the sagittal plane.15 The management of failed Latarjet procedure depends on the quality and position of the bone block. If the acutely fractured or malpositioned graft is viable with intact conjoint tendon insertion, potentially bone block repositioning and refixation with screws or small specific buttress plate may work, although only personal experience is available. If no significant graft osteolysis or malpositioning, open63 or arthroscopic64–66 capsular plication can be performed. In this case, an arthroscopic extraarticular capsular reinforcement with artificial ligament, which is a modification of a technique by Sanchez et al.,67 has been also described as a limited personal experience. If there is significant bone block osteolysis, the recurrence after a Latarjet procedure can be managed with a modified Eden-Hybinette procedure,26,68 or distal tibia allograft.69 In the case of recurrence with adequate coracoid graft and large Hill-Sachs lesion, secondary remplissage or partial humeral head resurfacing procedures may be useful.70
Persistent apprehension at ABER position can also be problematic for professional athletes. This can be theoretically reduced by additional soft tissue repair (labral fixation and/or capsular shift) to the Latarjet procedure. However, a recent large multicentre study reported that the apprehension test improved markedly and, at the last follow-up, no patients had apprehension with external rotation elbow at side (ER1), with only 11% of patients having it for external rotation at 90° of abduction (ER2) and 4% for external rotation at 140° of abduction, with no differences between techniques (open versus arthroscopic Latarjet with or without capsule and ligament reattachments).15
Neurological complications
Large reviews reported approximately 1% rate of neurovascular injury, although it has been reported as high as 20% in some series.15,71 To reduce this risk, it is recommended to avoid extensive dissection around the coracoid without exposing the medial border of the conjoint tendon and the surgeon must always stay lateral to this tendon. There is usually no need to explore or locate the musculocutaneous or the axillary nerves routinely. The self-retaining retractors could also be the cause for nerve stretching and their sizes and positions should be adapted to the morphology of the patient and their use should be limited to strict necessity. The management of nerve injuries is expectant with regular follow-ups and appropriate investigation with referral, if no improvements.72,73
Haematoma
Haematoma is an uncommon complication (1% to 2%) and it can be avoided by achieving haemostasis during the procedure or using a drain or bone wax to the coracoid osteotomy site.15 The operated arm can be rested in a sling for 2 weeks postoperatively. Generally, only cold packs and oral analgesia are required as treatment. Any large or progressively enlarging haematoma requires surgical drainage.
Infection
There is a risk of infection after open or arthroscopic Latarjet, although this is rare (1.5%).15 Most cases are managed with irrigation, debridement and appropriate antibiotic therapy. In cases of severe infection, it may be necessary to remove all the metalwork to achieve complete eradication of the infection, with a prolonged course of intravenous antibiotics. Infection can be the cause of failure of the bone block and recurrence of instability. After the complete clearance of the infection, a revision Eden-Hybinette procedure, can be performed.74
Stiffness and loss of external rotation
Stiffness, especially the overall loss of external rotation (ER1), with the use of open subscapularis splitting approach or arthroscopic techniques are usually only approximately 5° without any significant differences between the methods.15 However, other studies reported stiffness, significant loss of external rotation after this procedure.20,24,75,76 The main cause of stiffness after anterior shoulder stabilization is subscapularis tenotomy and repair. This muscle must be respected whatever procedure has been chosen.77 The important key steps in the open technique: (i) the use of a horizontal subscapularis-splitting approach;8,20,78–80 (ii) repair of the CAL stump to the capsule with the arm in maximal ER1;8,79,80 and (iii) immediate postoperative rehabilitation, as well as self-stretching exercises.
Bone block non-union
Pseudoarthrosis of the coracoid process can occur in 1.5% to 9% of cases and are usually related to unicortical or single screw fixation.8,71,79 It can also occur potentially in older patients as a result of poor bone quality, although this has no significant influence on the clinical outcome.25 Malpositioned graft (too inferior), as a result of insufficient purchase of the inferior screw in the bone, may lead to fibrous nonunion because rotational stability can be difficult to achieve with a single superior screw. Early and aggressive rehabilitation protocol can be another cause.
To encourage bone healing, Walch and Boileau,8 Mizuno et al.79 and Young et al.80 recommended:8,79,80
Preparing flat cancellous bone surfaces of the coracoid graft and anteroinferior glenoid site.
Using a typically 2 cm to 3 cm long coracoid graft after a carefully planned osteotomy.
Placing the bone block in the ‘lying position’ to increase the surface area for bone contact and union.
Using two bicortical compression screws placed perpendicular to the graft and parallel to the glenoid face to achieve stable fixation.
Standardized patient-led rehabilitation protocol, with self-stretching exercises.
Bone block fracture
Fracture of the transferred graft occurs in 1.5% of cases and it usually occurs within 3 months of surgery.37 Intra-operative overtightening of the screws, older age and excessive decortication of the undersurface of the coracoid can lead to an iatrogenic bone block fracture.71,79 Similarly to the graft non-union, the bone block fracture has no significant influence on the clinical result25 and it can be minimized by:
Using a careful ‘two finger’ screw tightening technique with the screwdriver.
Graft preparation with appropriately sized drills.
Drill holes spaced wide apart in the graft.
Intra-operative coracoid fracture can be treated, depending on fracture type and bone quality (augmented fixation with a smaller screw or a bioabsorbable anchor, buttress plate or iliac crest bone graft as the Eden-Hybinette procedure).81
Bone block resorption
Partial lysis of the coracoid occurs frequently but only rarely leads to persistent apprehension and unsatisfactory outcomes. The position of the bone block has no effect on the frequency of this complication. The resorption most commonly involves the superior and superficial part of the coracoid. This can be minimized by avoiding complete devascularization of the graft and by limiting soft tissue and pectoralis minor release to no further than the tip of the coracoid process. It has also been reported that the bone block undergoes significantly more osteolysis in patients without anterior glenoid bone defects (glenoid augmentation) compared to those with significant glenoid bone loss (glenoid restoration), which suggests that the stabilizing effect is mostly a result of the sling and capsular effect.82,83 However, this bone block resorption is usually without increased recurrence of instability or poor clinical outcome, and no specific management is required unless too proud and/or symptomatic metalwork.84,85
Balestro et al.86 have also reported that using bio-absorbable screws for fixation was associated with severe osteolysis (67% of cases) and almost complete resorption of the coracoid bone block, although the newer and more promising bio-compression screws require further investigations.
Osteoarthritis
Postoperative osteoarthritis is usually present, as with any type of intra-articular surgery (20% to 25%).21–24,27,79 There is no difference in the rate of this complication between open bone block transfer and open anterior capsulolabral fixation.22,24,27 The statistically influencing factors are: preoperative pre-existing osteoarthritis (which progresses in 50% of cases), older age at the first dislocation and at the time of the intervention, longer postoperative delay, preoperative fracture of the anterior glenoid rim, severe Hill-Sachs lesions, and high-demand sports.20,23,87–97 Technical mistakes, such as laterally overhanging coracoid process, are also a cause for postoperative arthritis.20,23,79 It is recommended to check the final position of the coracoid by visualization and palpation. If overhanging is present, the position of the graft should be adjusted or the bone block surface should be trimmed with a high-speed burr. Also, avoiding intra-articular screw placement and screw washers are important with respect to reducing the risk of degenerative changes later. Some modifications, such as capsular re-attachement and extra-articular graft placement, can potentially reduce the risk of postoperative osteoarthritis.11
Implant related
The use of implants close to the glenohumeral joint can cause problems. Anterior pain and focal tenderness especially with the arm in external rotation and adduction can be explained with the irritation or inflammation of the subscapularis muscle as a result of proud screw heads with a healed graft. Occasionally, too long screws can also cause pain at the posterior aspect of the shoulder. These can be treated successfully with the removal of the symptomatic screws (< 5% risk).15
Recently, a wedge profile buttress plate, which can also cause soft tissue irritation, has been introduced to theoretically improve the fixation of the bone block and to reduce the osteolysis of the bone graft.13,85
However, other alternative new fixation techniques with an Endobutton (Smith & Nephew, Endoscopy, Andover, MA) have been described in literature, with promising results, although there is a need for further long-term results.14–16
Summary
The Latarjet procedure is a safe and reliable technique for managing anterior instability, especially with associated glenoid bone defects. With appropriate patient selection, surgical indication (primary or recurrent anterior dislocations or subluxations, with or without hyperlaxity, with or without glenoid bone loss) and systematic surgical technique, with precise graft positioning regardless of which specific modifications are used, the Latarjet procedure can prevent recurrent anterior instability, in most cases avoiding the reported major complications associated with this procedure. However, postoperative shoulder arthritis and frequent bone block osteolysis remain unsolved additional challenges, which require further research and long-term studies.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
No ethical review or patient consent was required for this study.
References
- 1.Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006; 88: 1755–1763. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000; 16: 677–694. [DOI] [PubMed] [Google Scholar]
- 3.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 2000; 82: 35–46. [DOI] [PubMed] [Google Scholar]
- 4.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir 1954; 49: 994–997. [PubMed] [Google Scholar]
- 5.Patte D, Debeyre J. Recurrent dislocation of the shoulder. Encycl Med Chir Paris Technique Chirurgical Orthopedie 1980; 44265: 4–4. 4-02. [Google Scholar]
- 6.Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Shoulder Elbow Surg 2013; 95: 1390–1397. [DOI] [PubMed] [Google Scholar]
- 7.Walch G. The anterior recurrent dislocation of the shoulder. Rev Chir Orthop 1991; 77: 177–192. [Google Scholar]
- 8.Walch G, Boileau P. Latarjet–Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg 2000; 3: 136–141. [Google Scholar]
- 9.Boileau P, Thélu CÉ, Mercier N, Ohl X, Houghton-Clemmey R, Carles M. Arthroscopic Bristow–Latarjet combined with Bankart repair restores shoulder stability in patients with glenoid bone loss. Clin Orthop Relat Res 2014; 472: 2413–2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Beer JF. Glenoid bone defects. Open Latarjet with congruent arc modification. Orthop Clin N Am 2010; 41: 407–15. [DOI] [PubMed] [Google Scholar]
- 11.Bouju Y, Gadéa F, Stanovici J, Moubarak H, Favard L. Shoulder stabilization by modified Latarjet-Patte procedure: results at a minimum 10 years' follow-up, and role in the prevention of osteoarthritis. Orthop Traumatol Surg Res 2014; 100: S213–S218. [DOI] [PubMed] [Google Scholar]
- 12.Alvi HM, Monroe EJ, Muriuki M, Verma RN, Marra G, Saltzman MD. Latarjet fixation: a cadaveric biomechanical study evaluating cortical and cannulated screw fixation. Orthop J Sports Med 2016; 4: 2325967116643533–2325967116643533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaudhary D, Goyal A, Joshi D, Jain V, Mohindra M, Mehta N. Clinical and radiological outcome after mini-open Latarjet technique with fixation of coracoid with Arthrex wedge mini-plate. J Clin Orthop Trauma 2016; 7: 23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gendre P, Thélu CE, D'Ollonne T, Trojani C, Gonzalez JF, Boileau P. Coracoid bone block fixation with cortical buttons: an alternative to screw fixation? Orthop Traumatol Surg Res 2016; 102: 983–987. [DOI] [PubMed] [Google Scholar]
- 15.Metais P, Clavert P, Barth J, et al. Preliminary clinical outcomes of Latarjet-Patte coracoid transfer by arthroscopy vs. open surgery: prospective multicentre study of 390 cases. French Arthroscopic Society. Orthop Traumatol Surg Res 2016; 102: S271–S276. [DOI] [PubMed] [Google Scholar]
- 16.Boileau P, Gendre P, Baba M, et al. A guided surgical approach and novel fixation method for arthroscopic Latarjet. J Shoulder Elbow Surg 2016; 25: 78–89. [DOI] [PubMed] [Google Scholar]
- 17.Dumont GD, Fogerty S, Rosso C, Lafosse L. The arthroscopic Latarjet procedure for anterior shoulder instability: 5-year minimum follow-up. Am J Sports Med 2014; 42: 2560–2566. [DOI] [PubMed] [Google Scholar]
- 18.Ranne JO, Kainonen TU, Lehtinen JT, Heinonen OJ. Modified arthroscopic Latarjet procedure with coracoid exteriorization for treatment of anterior glenohumeral instability. Arthrosc Tech 2013; 2: 361–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taverna E, Garavaglia G, Ufenast H, D'Ambrosi R. Arthroscopic treatment of glenoid bone loss. Knee Surg Sports Traumatol Arthrosc 2016; 24: 546–556. [DOI] [PubMed] [Google Scholar]
- 20.Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Shoulder Elbow Surg 1998; 80: 841–852. [DOI] [PubMed] [Google Scholar]
- 21.Hovelius L, Saeboe M. Neer Award 2008: arthropathy after primary anterior shoulder dislocation 223 shoulders prospectively followed up for twenty-five years. J Shoulder Elbow Surg 2009; 18: 339–347. [DOI] [PubMed] [Google Scholar]
- 22.Hovelius L, Sandstrom B, Rosmark DL, Saebo M, Sundgren KH, Malmqvist BG. Long-term results with the Bankart and Bristow-Latarjet procedures: recurrent shoulder instability and arthropathy. J Shoulder Elbow Surg 2001; 10: 445–452. [DOI] [PubMed] [Google Scholar]
- 23.Hovelius L, Sandstrom B, Sundgren K, Saebo M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I clinical results. J Shoulder Elbow Surg 2004; 13: 509–516. [DOI] [PubMed] [Google Scholar]
- 24.Hovelius L, Vikerfors O, Olofsson A, Svensson O, Rahme H. Bristow-Latarjet and Bankart: a comparative study of shoulder stabilization in 185 shoulders during a seventeen year follow-up. J Shoulder Elbow Surg 2011; 20: 1095–1101. [DOI] [PubMed] [Google Scholar]
- 25.Hovelius L, Sandstrom B, Olofsson A, Svensson O, Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg 2012; 21: 647–660. [DOI] [PubMed] [Google Scholar]
- 26.Lunn JV, Castellano-Rosa J, Walch G. Recurrent anterior dislocation after the Latarjet procedure: outcome after revision using a modified Eden-Hybinette operation. J Shoulder Elbow Surg 2008; 17: 744–750. [DOI] [PubMed] [Google Scholar]
- 27.Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Latarjet, Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy 2014; 30: 1184–1211. [DOI] [PubMed] [Google Scholar]
- 28.Randelli P, Fossati C, Stoppani C, Evola FR, De Girolamo L. Open Latarjet versus arthroscopic Latarjet: clinical results and cost analysis. Knee Surg Sports Traumatol Arthrosc 2016; 24: 526–532. [DOI] [PubMed] [Google Scholar]
- 29.Gumina S, Postacchini F. Anterior dislocation of the shoulder in the elderly patient. J Bone Joint Surg Am 1997; 79: 540–543. [DOI] [PubMed] [Google Scholar]
- 30.Hawkins RJ, Bell RH, Hawkins RH, Koppert GJ. Anterior dislocation of the shoulder in the older patient. Clin Orthop Relat Res 1986; 206: 192–195. [PubMed] [Google Scholar]
- 31.Neviaser RJ, Neviaser TJ, Neviaser JS. Concurrent rupture of the rotator cuff and anterior dislocation of the shoulder in the older patient. J Bone Joint Surg Am 1988; 70: 1308–1311. [PubMed] [Google Scholar]
- 32.Pevny T, Hunter RE, Freeman JR. Primary traumatic anterior shoulder dislocation in patients 40 years of age and older. Arthroscopy 1998; 14: 289–294. [DOI] [PubMed] [Google Scholar]
- 33.Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am 1956; 38A: 957–977. [PubMed] [Google Scholar]
- 34.Simonet WT, Cofield RH. Prognosis in anterior shoulder dislocation. Am J Sports Med 1984; 12: 19–24. [DOI] [PubMed] [Google Scholar]
- 35.Walch G, Neyret P, Charret P. L’opération de Trillat pour luxation récidivante antérieure de l’épaule. Résultats à long terme de 250 cas avec un recul moyen de 11,3 ans. Lyon Chir 1989; 85: 25–31. [Google Scholar]
- 36.Maquieira GJ, Espinosa N, Gerber C, Eid K. Non-operative treatment of large anterior glenoid rim fractures after traumatic anterior dislocation of the shoulder. J Bone Joint Surg Br 2007; 89: 1347–1351. [DOI] [PubMed] [Google Scholar]
- 37.Walch G, Agostini JY, Levigne C, Nové-Josserand L. Recurrent anterior and multidirectional instability of the shoulder. Rev Chir Orthop Reparatrice Appar Mot 1995; 81: 682–690. [PubMed] [Google Scholar]
- 38.Raiss P, Lin A, Mizuno N, Melis B, Walch G. Results of the Latarjet procedure for recurrent anterior dislocation of the shoulder in patients with epilepsy. J Bone Joint Surg Br 2012; 94: 1260–1264. [DOI] [PubMed] [Google Scholar]
- 39.Andrews JR, Carson WG, Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med 1985; 13: 337–341. [DOI] [PubMed] [Google Scholar]
- 40.Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The ‘‘dead arm’’ revisited. Clin Sports Med 2000; 19: 125–158. [DOI] [PubMed] [Google Scholar]
- 41.Castagna A, Nordenson U, Garofalo R, Karlsson J. Minor shoulder instability. Arthroscopy 2007; 23: 211–215. [DOI] [PubMed] [Google Scholar]
- 42.Savoie FH, III, Papendik L, Field LD, Jobe C. Straight anterior instability: lesions of the middle glenohumeral ligament. Arthroscopy 2001; 17: 229–235. [DOI] [PubMed] [Google Scholar]
- 43.Townley CO. The capsular mechanism in recurrent dislocation of the shoulder. J Bone Joint Surg Am 1950; 32: 370–380. [PubMed] [Google Scholar]
- 44.Walch G, Boileau P, Noel ED. Impingement of the deep surface of the supraspinatus tendon on the posteriosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg 1992; 1: 238–245. [DOI] [PubMed] [Google Scholar]
- 45.Boileau P, Zumstein M, Balg F, Penington S, Bicknell RT. The unstable painful shoulder (UPS) as a cause of pain from unrecognized anteroinferior instability in the young athlete. J Shoulder Elbow Surg 2011; 20: 98–106. [DOI] [PubMed] [Google Scholar]
- 46.Chambers L, Altchek DW. Microinstability and internal impingement in overhead athletes. Clin Sports Med 2013; 32: 697–707. [DOI] [PubMed] [Google Scholar]
- 47.Endres NK, Warner JJ. Anterior instability after total shoulder replacement: salvage with modified Latarjet procedure. A report of 2 cases. J Shoulder Elbow Surg 2010; 19: 1–5. [DOI] [PubMed] [Google Scholar]
- 48.Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elbow Surg 2005; 14: 492–496. [DOI] [PubMed] [Google Scholar]
- 49.Jost B, Puskas GJ, Lustenberger A, Gerber C. Outcome of pectoralis major transfer for the treatment of irreparable subscapularis tears. J Bone Joint Surg Am 2003; 85A: 1944–1951. [DOI] [PubMed] [Google Scholar]
- 50.Alcid JG, Powell SE, Tibone JE. Revision anterior capsular shoulder stabilization using hamstring tendon autograft and tibialis tendon allograft reinforcement: minimum two-year follow-up. J Shoulder Elbow Surg 2007; 16: 268–722. [DOI] [PubMed] [Google Scholar]
- 51.Iannotti JP, Antoniou J, Williams GR, Ramsey ML. Iliotibial band reconstruction for treatment of glenohumeral instability associated with irreparable capsular deficiency. J Shoulder Elbow Surg 2002; 11: 618–23. [DOI] [PubMed] [Google Scholar]
- 52.Dodds SD, Medvecky MJ. Chronic bilateral locked anterior shoulder fracture dislocations. Am J Orthop 2008; 37: 364–368. [PubMed] [Google Scholar]
- 53.Neer CS, II, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am 1983; 65: 1232–44. [PubMed] [Google Scholar]
- 54.Rouhani A, Navali A. Treatment of chronic anterior shoulder dislocation by open reduction and simultaneous Bankart lesion repair. Sports Med Arthrosc Rehabil Ther Technol 2010; 16: 15–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abdelhady AM. Neglected anterior shoulder dislocation: open remplissage of the Hill-Sachs lesion with the infraspinatus tendon. Acta Orthop Belg 2010; 76: 162–165. [PubMed] [Google Scholar]
- 56.Matsoukis J, Tabib W, Guiffault P, et al. Primary unconstrained shoulder arthroplasty in patients with a fixed anterior glenohumeral dislocation. J Bone Joint Surg Am 2006; 88: 547–552. [DOI] [PubMed] [Google Scholar]
- 57.Mehta V. Humeral head plasty for a chronic locked anterior shoulder dislocation. Orthopedics 2009; 32: 52–52. [DOI] [PubMed] [Google Scholar]
- 58.Paladini P, Merolla G, De Santis E, Campi F, Porcellini G. Long-term subscapularis strength assessment after Bristow-Latarjet procedure: isometric study. J Shoulder Elbow Surg 2012; 21: 42–47. [DOI] [PubMed] [Google Scholar]
- 59.Galano GJ, Dieter AA, Moradi NE, Ahmad CS. Arthroscopic management of a chronic primary anterior shoulder dislocation. Am J Orthop 2010; 39: 351–355. [PubMed] [Google Scholar]
- 60.Kubiak G, Fabis J. Clinical improvement after 2 years one stage bilateral open reduction of chronic anterior shoulder dislocations with internal fixation of greater tuberosity fractures. Case study. Ortop Traumatol Rehabil 2013; 15: 175–181. [DOI] [PubMed] [Google Scholar]
- 61.Thomas DP, Graham GP. Missed bilateral anterior fracture dislocations of the shoulder. Injury 1996; 27: 661–662. [DOI] [PubMed] [Google Scholar]
- 62.Kahlon A. Transitory inferior dislocation of shoulder in a child after humerus fracture. J Coll Physicians Surg Pak 2014; 24: 444–445. [PubMed] [Google Scholar]
- 63.Guity MR, Roques B, Mansat P, Bellumore Y, Mansat M. Painful or unstable shoulder after coracoid transfer: result of surgical treatment. Rev Chir Orthop Reparatrice Appar Mot 2002; 88: 349–358. [PubMed] [Google Scholar]
- 64.Boileau P, Richou J, Lisai A, Chuinard C, Bicknell RT. The role of arthroscopy in revision of failed open anterior stabilization of the shoulder. Arthroscopy 2009; 25: 1075–1084. [DOI] [PubMed] [Google Scholar]
- 65.Castagna A, Garofalo R, Melito G, Markopoulos N, De Giorgi S. The role of arthroscopy in the revision of failed Latarjet procedures. Musculoskelet Surg 2010; 94(Suppl 1): S47–S55. [DOI] [PubMed] [Google Scholar]
- 66.Cuéllar A, Cuéllar R, de Heredia PB. Arthroscopic revision surgery for failure of open Latarjet technique. Arthroscopy 2017; 33: 910–917. [DOI] [PubMed] [Google Scholar]
- 67.Sanchez M, Cuellar R, Garcia A, Albillos J, Azofra J. Anterior stabilization of the shoulder by means of an artificial capsular reinforcement and arthroscopy – Part II: results. J Long Term Eff Med Implants 2000; 10: 199–209. [Google Scholar]
- 68.Giannakos A, Vezeridis PS, Schwartz DG, Jany R, Lafosse L. All-Arthroscopic revision Eden-Hybinette procedure for failed instability surgery: technique and preliminary results. Arthroscopy 2017; 33: 39–48. [DOI] [PubMed] [Google Scholar]
- 69.Provencher MT, Ghodadra N, LeClere L, Solomon DJ, Romeo AA. Anatomic osteochondral glenoid reconstruction for recurrent glenohumeral instability with glenoid deficiency using a distal tibia allograft. Arthroscopy 2009; 25: 446–452. [DOI] [PubMed] [Google Scholar]
- 70.Longo UG, Loppini M, Rizzello G, et al. Remplissage, humeral osteochondral grafts, Weber osteotomy, and shoulder arthroplasty for the management of humeral bone defects in shoulder instability: systematic review and quantitative synthesis of the literature. Arthroscopy 2014; 30: 1650–1666. [DOI] [PubMed] [Google Scholar]
- 71.Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg 2013; 22: 286–292. [DOI] [PubMed] [Google Scholar]
- 72.Lädermann A, Denard PJ, Burkhart SS. Injury of the suprascapular nerve during Latarjet procedure: an anatomic study. Arthroscopy 2012; 28: 316–321. [DOI] [PubMed] [Google Scholar]
- 73.Southam JD, Greis PE. Delayed, transient musculocutaneous nerve palsy after the Latarjet procedure. J Shoulder Elbow Surg 2012; 21: 8–11. [DOI] [PubMed] [Google Scholar]
- 74.Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 2012; 94: 495–501. [DOI] [PubMed] [Google Scholar]
- 75.Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007; 23: 1033–1041. [DOI] [PubMed] [Google Scholar]
- 76.Singer GC, Kirkland PM, Emery RJ. Coracoid transposition for recurrent anterior instability of the shoulder. A 20-year follow up study. J Bone Joint Surg Br 1995; 77: 73–76. [PubMed] [Google Scholar]
- 77.Maynou C, Cassagnaud X, Mestdagh H. Function of subscapularis after surgical treatment for recurrent instability of the shoulder using a bone-block procedure. J Bone Joint Surg Br 2005; 87: 1096–1101. [DOI] [PubMed] [Google Scholar]
- 78.Dos Santos RB, Kauffman FN, de Lima GP, Ferreira AM, Dos Santos SM, Aguiar JL. Evaluation of isometric strength and fatty infiltration of the subscapularis in Latarjet surgery. Acta Ortop Bras 2015; 23: 129–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mizuno N, Denard PJ, Raiss P, Melis B, Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 2014; 23: 1691–1699. [DOI] [PubMed] [Google Scholar]
- 80.Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg 2011; 20(2 Suppl): S61–S69. [DOI] [PubMed] [Google Scholar]
- 81.Gupta A, Delaney R, Petkin K, Lafosse L. Complications of the Latarjet procedure. Curr Rev Musculoskelet Med 2015; 8: 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Di Giacomo G, de Gasperis N, Costantini A, De Vita A, Beccaglia MA, Pouliart N. Does the presence of glenoid bone loss influence coracoid bone graft osteolysis after the Latarjet procedure? A computed tomography scan study in 2 groups of patients with and without glenoid bone loss. J Shoulder Elbow Surg 2014; 23: 514–518. [DOI] [PubMed] [Google Scholar]
- 83.Moroder P, Hirzinger C, Lederer S, et al. Restoration of anterior glenoid bone defects in posttraumatic recurrent anterior shoulder instability using the J-bone graft shows anatomic graft remodelling. Am J Sports Med 2012; 40: 1544–1550. [DOI] [PubMed] [Google Scholar]
- 84.Di Giacomo G, Costantini A, de Gasperis N, et al. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: a computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg 2011; 20: 989–995. [DOI] [PubMed] [Google Scholar]
- 85.Di Giacomo G, Costantini A, de Gasperis N, et al. Coracoid bone graft osteolysis after Latarjet procedure: a comparison study between two screws standard technique vs mini-plate fixation. Int J Shoulder Surg 2013; 7: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Balestro JC, Young A, Maccioni C, Walch G. Graft osteolysis and recurrent instability after the Latarjet procedure performed with bioabsorbable screw fixation. J Shoulder Elbow Surg 2015; 24: 711–718. [DOI] [PubMed] [Google Scholar]
- 87.Bigliani LU, Weinstein DM, Glasgow MT, Pollock RG, Flatow EL. Glenohumeral arthroplasty for arthritis after instability surgery. J Shoulder Elbow Surg 1995; 2: 87–94. [DOI] [PubMed] [Google Scholar]
- 88.Buscayret F, Edwards TB, Szabo I, Adeleine P, Coudane H, Walch G. Glenohumeral arthrosis in anterior instability before and after surgical treatment: incidence and contributing factors. Am J Sports Med 2004; 32: 1165–1172. [DOI] [PubMed] [Google Scholar]
- 89.Chapnikoff D, Besson A, Chantelot C, Fontaine C, Migaud H, Duquennoy A. Bankart procedure: clinical and radiological long-term outcome. Rev Chir Orthop Reparatrice Appar Mot 2000; 86: 558–565. [PubMed] [Google Scholar]
- 90.Fabre T, Abi-Chahla ML, Billaud A, Geneste M, Durandeau A. Long-term results with Bankart procedure: a 26-year follow-up study of 50 cases. J Shoulder Elbow Surg 2010; 19: 318–323. [DOI] [PubMed] [Google Scholar]
- 91.O’Driscoll SW, Evans DC. Long-term results of staple capsulorrhaphy for anterior instability of the shoulder. J Bone Joint Surg Am 1993; 75: 249–258. [DOI] [PubMed] [Google Scholar]
- 92.Ogawa K, Yoshida A, Matsumoto H, Takeda T. Outcome of the open Bankart procedure for shoulder instability and development of osteoarthritis: a 5- to 20-year follow-up study. Am J Sports Med 2010; 38: 1549–1557. [DOI] [PubMed] [Google Scholar]
- 93.Pelet S, Jolles BM, Farron A. Bankart repair for recurrent anterior glenohumeral instability: results at twenty-nine years’ follow-up. J Shoulder Elbow Surg 2006; 15: 203–207. [DOI] [PubMed] [Google Scholar]
- 94.Privitera DM, Bisson LJ, Marzo JM. Minimum 10-year follow-up of arthroscopic intra-articular Bankart repair using bioabsorbable tacks. Am J Sports Med 2012; 40: 100–107. [DOI] [PubMed] [Google Scholar]
- 95.Rosenberg BN, Richmond JC, Levine WN. Long-term followup of Bankart reconstruction: incidence of late degenerative glenohumeral arthrosis. Am J Sports Med 1995; 23: 538–544. [DOI] [PubMed] [Google Scholar]
- 96.Zuckerman JD, Matsen FA. Complications about the glenohumeral joint related to the use of screws and staples. J Bone Joint Surg Am 1984; 66: 175–180. [PubMed] [Google Scholar]
- 97.Zwaag HVD, Brand R, Obermann WR, Rozing PM. Glenohumeral osteoarthrosis after Putti-Platt repair. J Shoulder Elbow Surg 1999; 8: 252–258. [DOI] [PubMed] [Google Scholar]