Abstract
Men who do not seek help for mental health problems may experience unnecessary suffering which ultimately affects the well-being of themselves and others. Gendered manifestations of depressive symptoms may play an important role in why some men do not seek help for mental health issues. Using data from 2,382 male respondents in the National Comorbidity Survey Replication, the authors examined the relationship that both traditional and male-typical symptoms of depression had on the help-seeking behaviors of men. Traditional symptoms increased the odds of seeking help for depression for all men. Male-typical symptoms, however, did not increase the odds of seeking help for depression or another mental health concern. Both traditional and male-typical symptoms increased the odds of initially seeking help from a medical provider, and men with male-typical symptoms had an overall higher likelihood of seeking help from a medical provider. Consequently, it is important that medical professionals assess for depression even when it is not a presenting concern.
Keywords: depression, men, gender, help seeking, masculinity
Approximately one in nine men will be diagnosed with major depressive disorder (MDD) in their lifetime (Parker & Brotchie, 2010). Although women are about twice as likely to be diagnosed with depression, men are four times as likely to die from suicide (Oquendo et al., 2002), suggesting that many men have undiagnosed mental health issues. Research indicates that rates of undiagnosed depression are substantially higher in men than women (Angst et al., 2002; Magovcevic & Addis, 2008; Potts, Burnam, & Wells, 1991). Compounding the problem, men seek mental health help far less often than women (Addis & Mahalik, 2003) and those who do are less likely to be appropriately diagnosed (Afifi, 2007). For example, women are more likely to be diagnosed with MDD than men, even when they score the same on a standardized diagnostic instrument (Afifi, 2007), indicating that clinicians may have unconscious gender bias in their diagnostic judgment.
Underdiagnosis of mental health issues, like depression, in men may be the result of differences in how men and women manifest symptoms. Various factors, including gender socialization, lead many men to exhibit depressive feelings through male-typical depressive symptoms (Cochran & Rabinowitz, 2000). These symptoms can include aggression, irritability, violence, substance abuse, risky behavior, or somatic complaints—none of which are included in the current Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnosis criteria for MDD (Addis, 2008; Cochran & Rabinowitz, 2000; Fava et al., 2010; Levant, 1992; Mahalik et al., 2003; Martin, Neighbors, & Griffith, 2013; Real, 1997). Compounding the issue is the lack of a widely used standardized instrument addressing male-typical symptoms in depression, another potential contributor to the underdiagnosis of depression in men.
Since many male-typical symptoms of depression are externalized, they not only affect the well-being of depressed men but also the individuals in their lives. Impulsive reactions, like violence or angry verbal responses, can induce negative emotions and traumatic responses in family members (Lynch & Kilmartin, 2013). Self-destructive male-typical symptoms, such as substance abuse, can also have a negative effect by limiting a man’s connection to his children, significant others, and acquaintances in healthy ways (Arenas & Greif, 2000). Depressed men are also less likely to demonstrate positive parental behaviors such as nurturing, warmth, sensitivity, and engagement, and more likely to be withdrawn, negative, and detached (Wilson & Durbin, 2010). In light of these important issues and effects, the present study seeks to address this gap by exploring how depression symptomology affects help-seeking behaviors in a nationally generalizable sample.
Literature Review
Help Seeking Among Depressed Men
Despite the widespread prevalence of mental health disorders, only one quarter to one third of people with a diagnosable mental disorder seek help (Andrews, Issakidis, & Carter, 2001; Gonzalez, Tinsley, & Kreuder, 2002). Failure to seek help is a particular problem for men, who see professionals at about half the rate of women (Addis & Mahalik, 2003; Fields & Cochran, 2011; Fridgen et al., 2013; Vogel, Heimerdinger-Edwards, Hammer, & Hubbard, 2011). This difference has largely been attributed to the pervasive impact of masculine norms, which emphasize the importance of self-sufficiency, strength, and invulnerability (Addis & Mahalik, 2003; Evans, Frank, Oliffe, & Gregory, 2011; Pederson & Vogel, 2007). Help seeking is also strongly stigmatized among men, who often believe they will be criticized or ostracized if they see a mental health professional (Vogel, Wade, & Hackler, 2007). Stigmatization may be particularly strong among men with male-typical depressive symptoms, since they are the most likely to adhere to socially constructed gender norms and endorse hegemonic masculine ideals (see Addis & Mahalik, 2003, for a full discussion of these issues). Overall, these trends suggest that men who demonstrate male-typical symptoms of depression may be particularly unlikely to seek help.
A substantial body of research has examined the relationship between gender and help-seeking behaviors. Yet nearly all of the current literature uses a sex-differences framework, which fails to address within-gender differences in help-seeking behaviors (Addis & Mahalik, 2003; Shafer & Wendt, 2015). Male-typical issues, such as masculine norms and alexithymia, may limit men’s ability to express sadness or other traditional symptoms of depression. As a result, men may underreport their depressive feelings and forgo treatment. (Addis, 2008; Levant, 1992). Instead of directly expressing their sadness, depressed men may channel their negative emotions into externalized behaviors, such as yelling, violence, and substance abuse (Addis, 2008; Levant, 1992; Mahalik et al., 2003; Real, 1997). Similarly, many men may be unaware that their behaviors are associated with depression (Lynch & Kilmartin, 2013). Overall, these factors may help contribute to decreased help seeking in men and a lower likelihood of developing an episode of major depression as defined by traditional depressive symptoms. However, these same factors may increase their likelihood of developing negative male-typical behaviors such as substance abuse or aggression (Nolen-Hoeksema, Parker, & Larson, 1994).
Although past research has identified that men often express their depressive feelings through externalized male-typical symptoms, little is known about how these symptoms influence the likelihood of help seeking for mental health issues. In other words, despite research indicating that some men may be more likely to express depressive feelings through externalizing male-typical symptoms, current research has not examined how symptoms influence help-seeking behaviors in a nationally representative sample. An increased understanding of how both traditional and male-typical depressive symptoms influence help-seeking behaviors can provide clinicians with guidance on how to help men as individuals, rather than a collective group. Understanding the role of depressive symptoms in help seeking can also help researchers and public health officials better understand how to provide improved psychoeducation and mental health promotion (Hammer & Vogel, 2010). As such, the present study seeks to further illuminate how help-seeking behaviors in men who exhibit male-typical symptoms of depression differ from men with more traditional symptoms.
Provider Type
In addition to pursuing a better understanding of the relationship between male-typical symptoms of depression and help-seeking behaviors among men, the present study also addresses from whom men seek help. The importance of this question is underscored by the fact that treatment modality varies across provider type. Medical providers, like family doctors and psychiatrists, typically adhere to a medical model, while mental health professionals, like social workers, are more likely to use psychological or ecological models (Suls & Rothman, 2004). The differences between the two are nontrivial. Practitioners of the medical model primarily focus on the underlying biological causes of mental health disorders, while an ecological (sometimes referred to as the person-in-environment model) approach considers how biology and environment interact together to contribute to mental health concerns (Suls & Rothman, 2004). Though the medical model excels in addressing physical health issues, it may prove ineffective when applied to mental health concerns. In particular, the medical model primarily focuses on diagnoses, while sometimes overlooking individuals who do not meet the complete diagnostic criteria but still have significant problems (Gutkin, 2012). This may be particularly problematic for men with male-typical symptoms since their depressive symptoms may not conform to traditional diagnosis criteria (Martin et al., 2013). These men may not meet a strict application of DSM criteria for MDD, but their symptomatic behaviors demonstrate a need for support and treatment.
Strong adherence to the medical model may also lead clinicians to overlook important environmental factors that contribute to mental health problems (Gutkin, 2012). As noted earlier, prior research suggests that masculine norms may play a significant role in the manifestation of depressive symptoms in men and, as a result, an ecological model provides a potentially fuller explanation of depression among men (Cochran & Rabinowitz, 2000; Fields & Cochran, 2011; Martin et al., 2013). The inclusion of environmental factors within an ecological model also allows for interventions at the larger community level. By targeting problematic environmental factors, such as unhealthy masculine norms or public stigma around help seeking, an ecological model encourages prevention in addition to case-by-case remediation (Gutkin, 2012).
Men who strongly adhere to masculine norms may be less likely to seek help from mental health professionals due to perceived stigma around talking about emotional or psychological concerns (Vogel et al., 2011). As a result, we hypothesize that men with male-typical symptoms who do seek help will be more likely to seek help from a medical provider than from a mental health professional.
Method
Data and Sample
Data came from the National Comorbidity Survey Replication (NCS-R), a nationally representative survey investigating the prevalence of mental health disorders. The NCS-R was included as part of the 2001 to 2003 Collaborative Psychiatric Epidemiology Surveys, and targeted English-speaking adults aged 18 years or older in the contiguous United States. Respondents were selected from a multistage probability sample (Kessler et al., 2004). Interviewers met respondents face-to-face and used computer-assisted personal interviewing due to the sensitive nature of the questions. The NCS-R was administered in two parts between February 2001 and April 2003 and consisted of 5,143 females and 4,139 males. Part I was administered to all respondents and included a core diagnosis assessment. Part II was administered only to respondents who met the lifetime criteria for at least one core disorder, plus a 1-in-3 probability subsample of other respondents. Because the variables utilized in this article were in both Parts I and II of the survey, the final sample consists of men who had taken both sections of the NCS-R (n = 2,382). Demographically, the majority of the sample was currently employed non-Latino Whites between the ages of 30 and 55. Most respondents were married or cohabiting and identified as Protestant. Relatively even spreads existed for region, education, and income. See Table 1 for a more complete summary of sample demographics.
Table 1.
Demographic Information.
| Percentage of total (N = 2,296) | Mean traditional symptoms index score | Mean male-typical symptoms index score | |
|---|---|---|---|
| Total | 100.0 | 2.10 | 1.98 |
| Age (years) | |||
| 18-30a | 26.9 | 1.76 | 2.19 |
| 31-55a | 52.1 | 2.49 | 2.09 |
| >55 | 21.1 | 1.55 | 1.44 |
| Marital status | |||
| Married/cohabiting | 61.9 | 1.87 | 1.86 |
| Divorced/separated/widoweda | 14.7 | 3.07 | 2.22 |
| Never married | 23.4 | 2.09 | 2.13 |
| Education (years) | |||
| <12a | 16.1 | 1.85 | 2.13 |
| 12 | 29.5 | 2.09 | 2.01 |
| 13-15 | 28.3 | 2.20 | 2.12 |
| 16+a | 25.6 | 2.16 | 1.68 |
| Race | |||
| Non-Hispanic Whitea | 75.8 | 2.14 | 1.95 |
| African Americana | 10.8 | 1.67 | 2.06 |
| Hispanic | 8.8 | 2.14 | 2.02 |
| Other | 4.6 | 2.38 | 2.21 |
| Employment status | |||
| Employed | 72.5 | 2.02 | 2.00 |
| Unemployed | 2.2 | 1.67 | 1.38 |
| Not in labor forcea | 25.2 | 2.37 | 1.96 |
| Religion | |||
| Protestant | 48.2 | 2.03 | 1.89 |
| Catholic | 23.2 | 1.91 | 1.85 |
| Other religion | 8.4 | 2.35 | 1.96 |
| No religion | 19.9 | 2.38 | 2.34 |
| Income | |||
| 0-30,000 | 26.0 | 2.13 | 2.06 |
| 30,001-70,000 | 38.8 | 2.17 | 2.05 |
| 70,001-200,000 | 31.0 | 1.99 | 1.83 |
| 200,000+ | 4.2 | 2.02 | 1.89 |
| Region | |||
| Northeast | 18.6 | 2.00 | 1.98 |
| Midwest | 29.0 | 2.16 | 1.96 |
| South | 31.1 | 1.88 | 1.88 |
| Westa | 21.3 | 2.43 | 2.14 |
Significant difference in mean scores, p < .05.
Measures
Dependent Variables
In the first part of the analyses, three separate dependent variables were used. As seen in other studies, examining help-seeking behaviors for depression (Khazanov, Cui, Merikangas, & Angst, 2015; Sosulski & Woodward, 2013; Woodward, Taylor, & Chatters, 2011), the question “Did you ever in your life talk to a professional about your sadness/discouragement/lack of interest?” was used to assess past help-seeking behaviors, specifically for depression. For the second dependent variable, a dummy measure was created indicating whether the respondent had sought help for a general mental health concern other than depression, including irritability, various anxiety disorders, sleep issues, anger attacks, obsessive–compulsive disorder, and mania. It is important to note that while many of these items may be comorbid with depression (Fava et al., 2000; Fava et al., 2010; Winkler, Pjrek, & Kasper, 2005), only sleep issues are captured by DSM diagnostic criteria. The third dependent variable was a dummy variable indicating if the respondent had sought help for both depression and another mental health concern. For the second part of the analyses, a categorical variable indicated whether the respondent had initially sought help from a medical provider (including a psychiatrist), a mental health professional (such as a social worker, marriage and family therapist, or counselor), any other professional (such a religious leader, herbalist, or any other healer), or did not seek help.
Key Independent Variables
There were two key independent variables: An index of traditional DSM criteria for depression and an index of male-typical symptoms of depression. The traditional depression index used the same items as the Collaborative Psychiatric Epidemiology Surveys (2007) major depressive episode guideline, which asked respondents to retrospectively report on various symptoms they experienced during their most severe depressive episode. The traditional symptoms index closely followed the DSM criteria for a major depressive episode and included symptoms of depressed mood, loss of interest, change in appetite, sleep dysregulation, psychomotor agitation or retardation, loss of energy, feelings of worthlessness, diminished ability to concentrate, and suicidal thoughts, plans, or behaviors. The data did not, however, allow for an examination of mixed episodes, physiological conditions, or bereavement (Sections B, D, and E of the DSM diagnostic criteria).
For the second key independent variable, male-typical symptoms of depression, an index containing male-typical symptoms as defined by the current literature was created (Martin et al., 2013; Winkler et al., 2005). The index was also based on the Masculine Symptoms Scale, a previous index that used male-typical symptoms contained in the NCS-R data set (Martin et al., 2013). The male-typical symptom index included items related to stress, irritability, aggression, risky behaviors, hyperactivity, and substance abuse, none of which are included in DSM criteria for MDD. Variables in the scales were measured either “yes” or “no,” with the traditional symptoms index ranging from 0 to 9 and the male-typical symptoms index ranging from 0 to 6. The scales were scored by counting the number of symptoms to which the respondents had answered “yes.”
Controls
A number of statistical controls were also included in the analyses to account for other factors that influence help-seeking behaviors. Minority status has been correlated with decreased help-seeking behavior (Alegría et al., 2008; Cummings & Druss, 2011), so racial/ethnic identification was controlled for using mutually exclusive dummy variables for non-Hispanic White, non-Hispanic Black, Hispanic/Latino, and other race/ethnicity. Prior research has also indicated that marital status plays a role in the frequency of help-seeking behaviors (Wang et al., 2005). As a result, marital status was controlled for with a categorical variable indicating whether an individuals was currently married or cohabiting, divorced or widowed, or never married. Likewise, it is possible that being a parent might influence help-seeking behaviors, so a control for current parental status was also included. Finally, controls for sociodemographic characteristics such as income, religion, current employment status, and region of current residency were included in the analyses.
Data Analysis
Data analysis had two aims: The first was to explore the relationship between male-typical symptoms and the odds of men seeking help for depression, and the second was to understand where men with male-typical symptoms initially sought help. Three logistic regressions models were used to accomplish the first aim. The first model looked at the main effects of DSM and male-typical symptoms on help-seeking behaviors of men who had only sought help for depression. The second model examined the main effects for men who had sought help for both depression and another mental health concern. Finally, the third model included interaction effects for both men who had only sought help for depression and men who had sought help for both depression and another mental health concern. To accomplish the second aim of understanding, where men with male-typical symptoms initially sought help, the dependent variable indicated whether the respondent initially sought help from a medical provider, a mental health professional, an informal source of help, or did not seek help. Multinomial logistic regressions were conducted to make comparisons between each potential outcome.
Results
As demonstrated in Table 1, the total mean score was 2.10 for the traditional symptom index and 1.98 for the male-typical symptom index. The relatively low mean scores were expected because the sample included men who met the lifetime criteria for any disorder, as well as a one in three subsample of men who did not meet the criteria for any disorder. As a result, the distribution was positively skewed with the majority of men endorsing no traditional depressive symptoms and few male-typical symptoms. t Tests identified that the traditional index and male-typical index mean scores were significantly different for men who were between the ages of 18 and 55 years; were divorced, separated, or widowed; had less than 12 or more than 16 years of education; were non-Hispanic White or African American; were not in the labor force; or who lived in the West. Across most of these categories, respondents scored higher on the traditional symptom index than the male-typical index, though this trend was reversed for men under the age of 30 or who were African American.
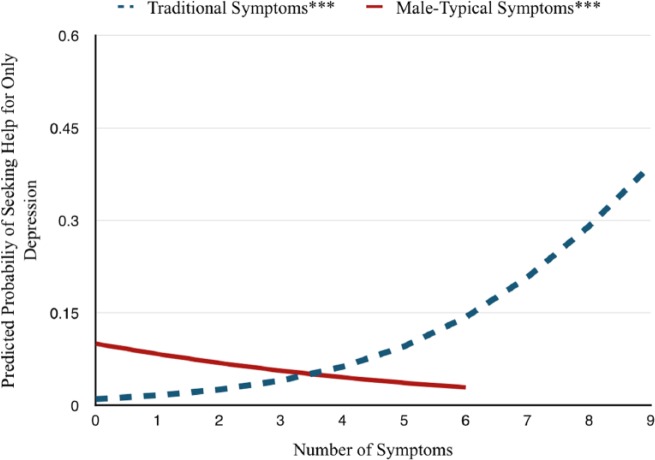
The main effects of depressive symptoms on help-seeking behaviors are reported in Table 2. The left half focuses on men who sought help exclusively for depression. The results indicate that help seeking is associated with the endorsement of traditional depressive symptoms. In fact, the odds of seeking help for depression increased 60% with each additional symptom. Conversely, additional male-typical symptoms of depression decreased the likelihood of seeking help for exclusively for depression. Each additional male-typical symptom was associated with a 23% decrease in the odds of help seeking. None of the controls significantly affected the odds of seeking help for only depression. Figure 1 shows that the predicted probabilities for only seeking help for depression increased from 1% to 39% with increasing traditional symptoms and decreased from 10% to 3% with increasing male-typical symptoms.
Table 2.
Logistic Regression Predicting Lifetime Help Seeking, Main Effects.
| Variables | Help seeking: Depression only |
Help seeking: Depression and other mental health concern |
||
|---|---|---|---|---|
| OR | SE | OR | SE | |
| Male-typical symptoms | 0.769*** | 0.055 | 1.106 | 0.072 |
| Traditional symptoms | 1.604*** | 0.058 | 1.925*** | 0.082 |
| Income | 1.035 | 0.021 | 1.001 | 0.021 |
| Parental status | 0.950 | 0.250 | 0.965 | 0.237 |
| Midwest | 1.025 | 0.288 | 0.452** | 0.123 |
| South | 0.743 | 0.224 | 0.464** | 0.130 |
| West | 0.884 | 0.273 | 0.614 | 0.176 |
| Age | 1.014 | 0.009 | 1.001 | 0.008 |
| Divorced | 1.107 | 0.300 | 2.280** | 0.555 |
| Never married | 1.740 | 0.535 | 0.793 | 0.234 |
| Black | 0.663 | 0.259 | 0.291** | 0.110 |
| Hispanic | 0.492 | 0.220 | 0.411* | 0.157 |
| Other race | 1.133 | 0.488 | 0.542 | 0.222 |
| Education (years) | ||||
| 12 | 0.791 | 0.258 | 1.080 | 0.325 |
| 13-15 | 1.134 | 0.356 | 1.242 | 0.370 |
| 16+ | 0.833 | 0.281 | 2.188* | 0.688 |
| Unemployed | 0.600 | 0.477 | 2.074 | 1.342 |
| Not in labor force | 0.841 | 0.204 | 1.511 | 0.343 |
| Catholic | 0.901 | 0.243 | 0.603 | 0.159 |
| No religion | 1.123 | 0.282 | 0.859 | 0.205 |
| Other religion | 0.821 | 0.293 | 0.962 | 0.303 |
| Constant | 0.008*** | 0.005 | 0.006*** | 0.004 |
| Observations | 2,284 | 2,234 | ||
Note. OR = odds ratio; SE = standard error.
p < .05. **p < .01. ***p < .001.
Figure 1.
Relationship between depressive symptoms and probability of seeking help for depression.
***p < .001.
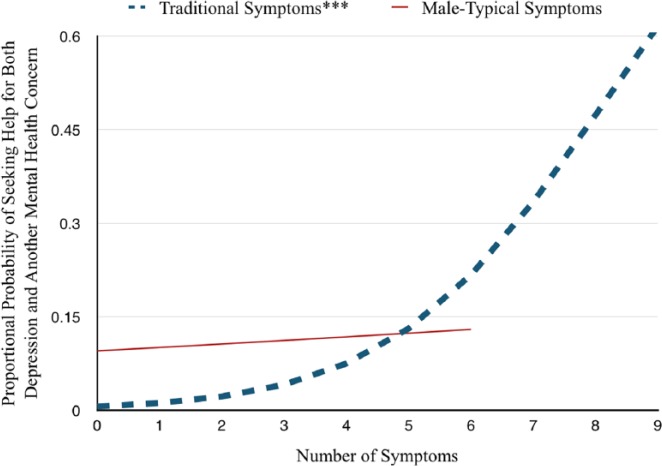
In the right-hand columns of Table 2, the results for help seeking for depression and other mental health concerns are reported. The odds of help seeking increased by 93% with each additional traditional symptom. However, additional male-typical symptoms had no significant association with the odds of help seeking. Figure 2 shows that traditional symptoms increased the predicted probabilities of seeking help for both depression and another mental health concern from 1% to 62%, while male-typical symptoms did not significantly correlate with the predicted probabilities. Additional factors that increased the odds of seeking help for both depression and another mental health concern included having 16 or more years of education and being divorced, separated, or widowed. Living in the South or Midwest, or being non-Hispanic Black or Hispanic/Latino, however, decreased the odds of seeking help for both depression and another mental health concern.
Figure 2.
Relationship between depressive symptoms and probability of seeking help for both depression and another mental health concern.
***p < .001.
It is possible that depressive symptoms interact with one another to influence help-seeking behavior. As a result, interactions between traditional and male-typical symptoms were included in the regression model and are reported in Table 3. Results indicated that male-typical symptoms reduce the positive effect of traditional symptoms on help seeking for depression. The interaction term was not significantly related to whether individuals sought help for both depression and other mental health concerns.
Table 3.
Logistic Regression Predicting Lifetime Help Seeking, Interactive, and Main Effects.
| Variables | Help seeking: Depression only |
Help seeking: Depression and other mental health concern |
||
|---|---|---|---|---|
| OR | SE | OR | SE | |
| Male-typical symptoms | 1.248 | 0.209 | 1.312 | 0.266 |
| Traditional symptoms | 1.856*** | 0.120 | 2.037*** | 0.161 |
| Male-typical × traditional | 0.928** | 0.022 | 0.975 | 0.027 |
| Income | 1.034 | 0.022 | 1.000 | 0.021 |
| Parental status | 0.960 | 0.254 | 0.966 | 0.237 |
| Midwest | 1.029 | 0.291 | 0.454** | 0.123 |
| South | 0.742 | 0.225 | 0.465** | 0.130 |
| West | 0.887 | 0.276 | 0.615 | 0.176 |
| Age | 1.015 | 0.009 | 1.001 | 0.008 |
| Divorced | 1.073 | 0.293 | 2.235** | 0.545 |
| Never married | 1.754 | 0.541 | 0.794 | 0.234 |
| Black | 0.654 | 0.257 | 0.292** | 0.110 |
| Hispanic | 0.473 | 0.213 | 0.407* | 0.156 |
| Other race | 1.157 | 0.501 | 0.545 | 0.222 |
| Education (years) | ||||
| 12 | 0.790 | 0.259 | 1.077 | 0.323 |
| 13-15 | 1.112 | 0.350 | 1.232 | 0.365 |
| 16+ | 0.830 | 0.282 | 2.178* | 0.683 |
| Unemployed | 0.595 | 0.480 | 2.065 | 1.345 |
| Not in labor force | 0.890 | 0.217 | 1.533 | 0.349 |
| Catholic | 0.930 | 0.252 | 0.608 | 0.160 |
| No religion | 1.107 | 0.279 | 0.855 | 0.204 |
| Other religion | 0.828 | 0.299 | 0.965 | 0.304 |
| Constant | 0.003*** | 0.002 | 0.004*** | 0.003 |
| Observations | 2,284 | |||
Note. OR = odds ratio; SE = standard error.
p < .05. **p < .01. ***p < .001.
The analysis also provided information about how male-typical symptoms influence where men initially seek help. Overall, 30% (n = 695), of men sought help from a medical professional, 18% (n = 413) sought help from a mental health professional, 3% sought help from other professional sources such as spiritualists or healers, and the remaining 48% (n = 1,110) reported not seeking help. As identified by the relative risk ratios reported in Table 4, both traditional and male-typical depressive symptoms increased the odds of seeking help from a medical professional as compared with a mental health provider, informal help, or not seeking help. For example, each traditional symptom increased the odds of initially seeking help from a medical provider by 6% when compared with a mental health professional and by 18% when compared with not seeking help. Male-typical symptoms were not significantly related to the odds of seeking help from a medical provider as compared with a mental health professional, but were related with a 39% increase in the odds as compared with not seeking help. Figure 3 and Figure 4 shows the predicted probabilities of seeking help from the various provider types based on the number of depressive symptoms present. Overall, male-typical symptoms of depression were related to a higher probability of initially seeking help from a medical provider than were traditional symptoms.
Table 4.
Relationship Between Depressive Symptoms and Where Men Initially Seek Help.
| Traditional symptoms RRR | Male-typical symptoms RRR | |
|---|---|---|
| Mental health professional vs. medical professional | 0.940** | 0.925 |
| Mental health professional vs. informal help | 1.034 | 0.935 |
| Mental health professional vs. not seeking help | 1.133*** | 1.385*** |
| Medical professional vs. informal help | 1.101* | 1.011 |
| Medical professional vs. not seeking help | 1.206*** | 1.498*** |
| Informal help vs. not seeking help | 1.10* | 1.48*** |
Note. RRR = relative risk ratio. All controls were included in the model, but excluded from the table for parsimony.
p < .05. **p < .01. ***p < .001.
Figure 3.
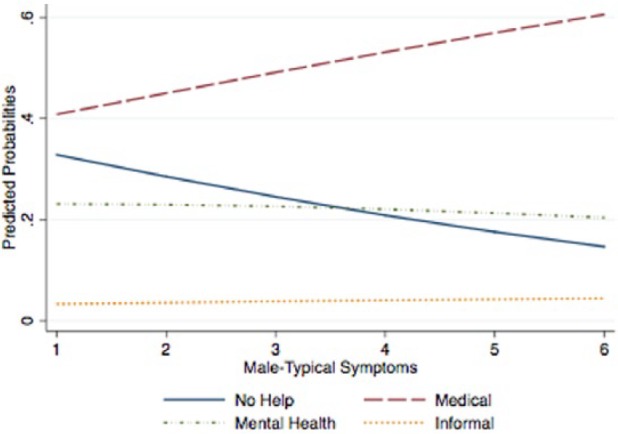
Relationship between male-typical symptoms and initial provider for depression.
Figure 4.
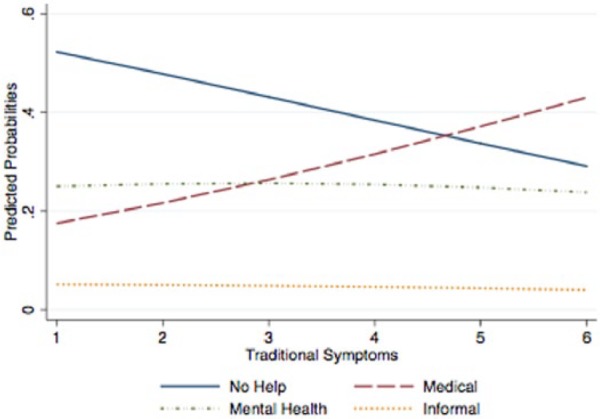
Relationship between traditional symptoms and initial provider for depression.
Discussion
Male-typical depressive symptoms have important systemic effects—not only affecting men’s well-being but also the health of women, children, and communities (Arenas & Greif, 2000; Wilson & Durbin, 2010). Destructive behaviors including aggressiveness, violence, and substance abuse, have wide-ranging effects on families, friends, and acquaintances (Arenas & Greif, 2000; Wilson & Durbin, 2010). Seeking help for one’s problems may help mitigate these wide-ranging negative effects. However, masculine norms and attitudes often lead men to refuse help, particularly for mental health issues (Fields & Cochran, 2011; Fridgen et al., 2013). Given this background, this article addressed how male-typical symptoms of depression affect help-seeking behavior. The results indicated that male-typical symptoms did not significantly increase the odds of seeking help for depression. This is particularly problematic for men whose traditional symptoms lie below the DSM threshold for MDD but who also demonstrate male-typical symptoms. These men experience a significant amount of distress, but the current results report that they are among the least likely to seek help for depression.
Depression is diagnosed about twice as often in women as men (Parker & Brotchie, 2010), suggesting that men may feel uncomfortable seeking help for what is often seen as a feminine problem. Furthermore, men who seek help for a mental health concern other than depression may relegate any comorbid depression to a secondary concern rather than the primary presenting issue and thus may be less likely to clearly express needing treatment for depression. Because of this, it is imperative that clinicians understand the relationship between male-typical symptoms and depression so that they can assess and properly treat any underlying depression. One way that this can be achieved is through the administration of gender-sensitive depression inventories to men who demonstrate male-typical symptoms but do not indicate that depression is a significant issue in their lives (Martin et al., 2013). Individual, familial, and community education about the relationship between male-typical symptoms and depression is also important and will likely reduce the stigma associated with seeking help. As an example, Hammer and Vogel (2010) developed a brochure which focused more on male-typical symptoms of depression than traditional symptoms of depression. They reported that the male-sensitive brochure improved attitudes toward seeking help and decreased self-stigma more so than a control brochure. Continuing research about the prevalence of male-typical symptoms of depression as well as their relationship with help-seeking behaviors will further assist in developing male-sensitive awareness campaigns.
The analyses also revealed that men with male-typical symptoms of depression were more likely to initially seek help from medical provider than men with traditional depression symptoms. Coupled with the fact that many masculine depressive symptoms can be categorized as other mental health concerns, like substance abuse, it is important for all helping professionals, including medical providers, to assess for the possibility of underlying depression in men. Men who initially seek help from a medical provider may be less likely to receive continuing follow-up care than those initially diagnosed by a psychiatrist or other mental health specialties (Kniesner, Powers, & Croghan, 2005; Wang et al., 2005). Thus, men exhibiting male-typical symptoms are in “double jeopardy”; they are less likely to seek help for depression, and when they do, they are less likely to receive adequate follow-up care.
The reduced frequency of help seeking for men with male-typical symptoms also affects families and communities. Men are overwhelmingly the perpetrators of control-based violence against women and children (Kimmel, 2002), and early interventions targeting male-typical symptoms may potentially reduce future acts of domestic violence related to an undiagnosed depression. Depression also has significant and negative effects on positive parental behaviors (Lynch & Kilmartin, 2013; Wilson & Durbin, 2010), thus detrimentally influencing the entire family unit. By promoting individual, clinical, and community awareness of the relationship between depressive symptoms and help-seeking behaviors, clinicians can potentially reduce the prevalence of undiagnosed depression, promote recovery for suffering men, and reduce violent or criminal behaviors related to male-typical symptoms of depression.
There are certain limitations to this study, particularly regarding the generalizability of the data set. While the data contained a large representative sample, it did not include individuals who were institutionalized, including incarcerated men and men in in-patient treatment. This excludes many men who may be severely depressed, including men in a hypermasculinized environment who may be more likely to have expressed depressive feelings through male-typical symptoms such as substance abuse and aggression. It also excludes all non-English speakers, thus reducing its ability to examine the role of culture in depressive symptoms and help-seeking behavior. Additionally, the data were originally collected between 2001 and 2003, which weakens its temporal relevance and highlights the need for additional data regarding masculine norms, mental health, and help-seeking behaviors. The data also lacked information regarding adherence to masculine norms, thus preventing the exploration of how masculine norm adherence influences the likelihood of demonstrating male-typical symptoms of depression. Furthermore, because the present study used secondary data analysis, not all constructs were ideally fit for this study. For example, many of the items in the independent variable scales asked respondents to recall past symptoms, though research demonstrates recall of prior depressive symptoms is poor (Wells & Horwood, 2004). Assessing current or more recent depressive symptoms and help-seeking behaviors would likely produce more accurate results than relying on retrospective reporting. Additionally, while the majority of the items asked respondents to indicate if they had ever experienced the specific symptoms, the items assessing for stress and sleep problems asked about whether the respondent had experienced them in the past few months. Despite these limitations, the present study reveals the worrisome trend that men with male-typical symptoms of depression may be less likely to seek and receive treatment for their underlying depression.
This study reveals important areas for further research. One such area is the relationship between adherence to masculine norms and male-typical symptoms of depression. While current research theorizes that higher endorsement of masculine norms increases the odds of exhibiting male-typical symptoms of depression, this has not been tested in a nationally representative sample. Additionally, the present study only provides a cursory look at the role of race and ethnicity in depressive symptoms. Future research is needed to illuminate any potential connections between ethnicity, male-typical symptoms, and help-seeking behaviors. Furthermore, a wide net was cast on potential masculine depressive symptoms, some of which are symptoms of other mental health issues or diagnosable mental health problems in their own right. This was done because the current article is an initial exploration of the relationship between depressive symptom typologies and help seeking. Finally, future research is also needed to understand how male-typical symptoms are correlated with help-seeking behaviors in cases of comorbid depression and anxiety. A better understanding of these connections would further indicate which men are at an increased risk for male-typical symptoms of depression and assist in the development of clinical and community interventions.
The relationship between initial provider type and treatment outcomes also warrants future research. While initially seeking help from a psychiatrist or other mental health specialty may be related to an increased likelihood of follow-up care (Kniesner et al., 2005; Wang et al., 2005), little research examines how initial provider type predicts ultimate treatment outcomes among depressed men in general, and no current research explores the relationship between provider type and treatment outcomes for men with male-typical symptoms of depression. Finally, while the current study identified that men with male-typical symptoms of depression were more likely to initially seek help from a medical provider, possible explanations for this connection were unable to be effectively examined.
More and more research has looked at the prevalence and impact of male-typical symptoms among depressed men (Addis, 2008; Cochran & Rabinowitz, 2000; Magovcevic & Addis, 2008; Martin et al., 2013; Rabinowitz & Cochran, 2008). These male-typical symptoms include irritability, aggression, substance abuse, and risky behavior. Current research, however, has not directly explored the relationship between male-typical symptoms and help-seeking behaviors among men. The present study identified that male-typical symptoms were not associated with an increased likelihood of seeking help for depression. The presence of male-typical symptoms also increased the likelihood of initially seeking help from a medical provider.
The findings that male-typical symptoms of depression do not significantly increase the odds of seeking help for depression has notable consequences for men demonstrating these symptoms as well as for those with whom they interact. As research further reveals the relationship between male-typical symptoms of depression and help-seeking behaviors, clinicians will be better equipped to recognize and treat men with nontraditional expressions of depression. The effective treatment of these self-destructive and aggressive male-typical symptoms will potentially reduce incidents of violence against women and children, promote involved fathering, and reduce rates of undiagnosed depression among men.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Addis M. E. (2008). Gender and depression in men. Clinical Psychology: Science and Practice, 15, 153-168. doi: 10.1111/j.1468-2850.2008.00125.x [DOI] [Google Scholar]
- Addis M. E., Mahalik J. R. (2003). Men, masculinity, and the contexts of help seeking. American Psychologist, 58, 5-14. doi: 10.1037/0003-066X.58.1.5 [DOI] [PubMed] [Google Scholar]
- Afifi M. (2007). Gender differences in mental health. Singapore Medical Journal, 48, 385-391. [PubMed] [Google Scholar]
- Alegría M., Chatterji P., Wells K., Cao Z., Chen C.-N., Takeuchi D., . . . Meng X. L. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services, 59, 1264-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Issakidis C., Carter G. (2001). Shortfall in mental health service utilisation. British Journal of Psychiatry, 179, 417-425. doi: 10.1192/bjp.179.5.417 [DOI] [PubMed] [Google Scholar]
- Angst J., Gamma A., Gastpar M., Lépine J. P., Mendlewicz J., Tylee A. (2002). Gender differences in depression: Epidemiological findings from the European DEPRES I and II studies. Depression Research in European Society Study, 5, 201-209. [DOI] [PubMed] [Google Scholar]
- Arenas M. L., Greif G. L. (2000). Issues of fatherhood and recovery for VA substance abuse patients. Journal of Psychoactive Drugs, 32, 339-341. [DOI] [PubMed] [Google Scholar]
- Cochran S. V., Rabinowitz F. E. (2000). Men and depression: Clinical and empirical perspectives. San Diego, CA: Academic Press. [Google Scholar]
- Collaborative Psychiatric Epidemiology Surveys. (2007). DSM-IV major depressive episode. Retrieved from http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/20240
- Cummings J. R., Druss B. G. (2011). Racial/ethnic differences in mental health service use among adolescents with major depression. Journal of the American Academy of Child & Adolescent Psychiatry, 50, 160-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J., Frank B., Oliffe J. L., Gregory D. (2011). Health, illness, men and masculinities (HIMM): A theoretical framework for understanding men and their health. Journal of Men’s Health, 8, 7-15. doi: 10.1016/j.jomh.2010.09.227 [DOI] [Google Scholar]
- Fava M., Hwang I., Rush A. J., Sampson N., Walters E. E., Kessler R. C. (2010). The importance of irritability as a symptom of major depressive disorder: Results from the National Comorbidity Survey Replication. Molecular Psychiatry, 15, 856-867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava M., Rankin M. A., Wright E. C., Alpert J. E., Nierenberg A. A., Pava J., Rosenbaum J. F. (2000). Anxiety disorders in major depression. Comprehensive Psychiatry, 41, 97-102. [DOI] [PubMed] [Google Scholar]
- Fields A. J., Cochran S. V. (2011). Men and depression: Current perspectives for health care professionals. American Journal of Lifestyle Medicine, 5, 92-100. [Google Scholar]
- Fridgen G. J., Aston J., Gschwandtner U., Pflueger M., Zimmermann R., Studerus E., . . . Riecher-Rössler A. (2013). Help-seeking and pathways to care in the early stages of psychosis. Social Psychiatry & Psychiatric Epidemiology, 48, 1033-1043. [DOI] [PubMed] [Google Scholar]
- Gonzalez J. M., Tinsley H. E. A., Kreuder K. R. (2002). Effects of psychoeducational interventions on opinions of mental illness, attitudes toward help seeking, and expectations about psychotherapy in college students. Journal of College Student Development, 43, 51-63. [Google Scholar]
- Gutkin T. B. (2012). Ecological psychology: Replacing the medical model paradigm for school-based psychological and psychoeducational services. Journal of Educational & Psychological Consultation, 22, 1-20. doi: 10.1080/10474412.2011.649652 [DOI] [Google Scholar]
- Hammer J. H., Vogel D. L. (2010). Men’s help seeking for depression: The efficacy of a male-sensitive brochure about counseling. The Counseling Psychologist, 38, 296-313. [Google Scholar]
- Kessler R. C., Patricia B., Chiu W. T., Olga D., Steven H., Eva H., . . . Hui Z. (2004). The US National Comorbidity Survey Replication (NCS-R): Design and field procedures. International Journal of Methods in Psychiatric Research, 13, 69-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazanov G. K., Cui L., Merikangas K., Angst J. (2015). Treatment patterns of youth with bipolar disorder: Results from the National Comorbidity Survey—Adolescent Supplement (NCS-A). Journal of Abnormal Child Psychology, 43, 391-400. doi: 10.1007/s10802-014-9885-6 [DOI] [PubMed] [Google Scholar]
- Kimmel M. S. (2002). “Gender symmetry” in domestic violence: A substantive and methodological research review. Violence Against Women, 8, 1332-1363. [Google Scholar]
- Kniesner T. J., Powers R. H., Croghan T. W. (2005). Provider type and depression treatment adequacy. Health Policy, 72, 321-332. [DOI] [PubMed] [Google Scholar]
- Levant R. F. (1992). Toward the reconstruction of masculinity. Journal of Family Psychology, 5, 379-402. doi: 10.1037/0893-3200.5.3-4.379 [DOI] [Google Scholar]
- Lynch J., Kilmartin C. (2013). The pain behind the mask: Overcoming masculine depression. New York, NY: Routledge. [Google Scholar]
- Magovcevic M., Addis M. E. (2008). The Masculine Depression Scale: Development and psychometric evaluation. Psychology of Men & Masculinity, 9, 117-132. [Google Scholar]
- Mahalik J. R., Locke B. D., Ludlow L. H., Diemer M. A., Scott R. P. J., Gottfried M., Freitas G. (2003). Development of the Conformity to Masculine Norms Inventory. Psychology of Men & Masculinity, 4, 3-25. doi: 10.1037/1524-9220.4.1.3 [DOI] [Google Scholar]
- Martin L. A., Neighbors H. W., Griffith D. M. (2013). The experience of symptoms of depression in men vs women: Analysis of the national comorbidity survey replication. JAMA Psychiatry, 70, 1100-1106. doi: 10.1001/jamapsychiatry.2013.1985 [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., Parker L. E., Larson J. (1994). Ruminative coping with depressed mood following loss. Journal of Personality and Social Psychology, 67, 92-104. [DOI] [PubMed] [Google Scholar]
- Oquendo M. A., Kamali M., Ellis S. P., Grunebaum M. F., Malone K. M., Brodsky B. S., . . . Mann J. J. (2002). Adequacy of antidepressant treatment after discharge and the occurrence of suicidal acts in major depression: A prospective study. American Journal of Psychiatry, 159, 1746-1751. doi: 10.1176/appi.ajp.159.10.1746 [DOI] [PubMed] [Google Scholar]
- Parker G., Brotchie H. (2010). Gender differences in depression. International Review of Psychiatry, 22, 429-436. doi: 10.3109/09540261.2010.492391 [DOI] [PubMed] [Google Scholar]
- Pederson E. L., Vogel D. L. (2007). Male gender role conflict and willingness to seek counseling: Testing a mediation model on college-aged men. Journal of Counseling Psychology, 54, 373-384. doi: 10.1037/0022-0167.54.4.373 [DOI] [Google Scholar]
- Potts M. K., Burnam M. A., Wells K. B. (1991). Gender differences in depression detection: A comparison of clinician diagnosis and standardized assessment. Psychological Assessment, 3, 609-615. [Google Scholar]
- Rabinowitz F. E., Cochran S. V. (2008). Men and therapy: A case of masked male depression. Clinical Case Studies, 7, 575-591. doi: 10.1177/1534650108319917 [DOI] [Google Scholar]
- Real T. (1997). I don’t want to talk about it: Overcoming the legacy of male depression. New York, NY: Fireside. [Google Scholar]
- Shafer K., Wendt D. (2015). Men’s mental health: A call to social workers. Social Work, 60, 105-112. [DOI] [PubMed] [Google Scholar]
- Sosulski M. R., Woodward A. T. (2013). African American women living with mental disorders: Factors associated with help seeking from professional services and informal supports. Social Work in Public Health, 28, 660-671. [DOI] [PubMed] [Google Scholar]
- Suls J., Rothman A. (2004). Evolution of the biopsychosocial model: Prospects and challenges for health psychology. Health Psychology, 23, 119-125. [DOI] [PubMed] [Google Scholar]
- Vogel D. L., Heimerdinger-Edwards S. R., Hammer J. H., Hubbard A. (2011). “Boys don’t cry”: Examination of the links between endorsement of masculine norms, self-stigma, and help-seeking attitudes for men from diverse backgrounds. Journal of Counseling Psychology, 58, 368-382. doi: 10.1037/a0023688 [DOI] [PubMed] [Google Scholar]
- Vogel D. L., Wade N. G., Hackler A. H. (2007). Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. Journal of Counseling Psychology, 54, 40-50. doi: 10.1037/0022-0167.54.1.40 [DOI] [Google Scholar]
- Wang P. S., Lane M., Olfson M., Pincus H. A., Wells K. B., Kessler R. C. (2005). Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 629-640. [DOI] [PubMed] [Google Scholar]
- Wells J. E., Horwood L. J. (2004). How accurate is recall of key symptoms of depression? A comparison of recall and longitudinal reports. Psychological Medicine, 34, 1001-1011. [DOI] [PubMed] [Google Scholar]
- Wilson S., Durbin C. E. (2010). Effects of paternal depression on fathers’ parenting behaviors: A meta-analytic review. Clinical Psychology Review, 30, 167-180. [DOI] [PubMed] [Google Scholar]
- Winkler D., Pjrek E., Kasper S. (2005). Anger attacks in depression: Evidence for a male depressive syndrome. Psychotherapy and Psychosomatics, 74, 303-307. doi: 10.1159/000086321 [DOI] [PubMed] [Google Scholar]
- Woodward A. T., Taylor R. J., Chatters L. M. (2011). Use of professional and informal support by Black men with mental disorders. Research on Social Work Practice, 21, 328-336. [DOI] [PMC free article] [PubMed] [Google Scholar]