Abstract
The challenges of providing quality respiratory care to persons living in rural or remote communities can be daunting. These populations are often vulnerable in terms of both health status and access to care, highlighting the need for innovation in service delivery. The rapidly expanding options available using telehealthcare technologies have the capacity to allow patients in rural and remote communities to connect with providers at distant sites and to facilitate the provision of diagnostic, monitoring, and therapeutic services. Successful implementation of telehealthcare programs in rural and remote settings is, however, contingent upon accounting for key technical, organizational, social, and legal considerations at the individual, community, and system levels. This review article discusses five types of telehealthcare delivery that can facilitate respiratory care for residents of rural or remote communities: remote monitoring (including wearable and ambient systems; remote consultations (between providers and between patients and providers), remote pulmonary rehabilitation, telepharmacy, and remote sleep monitoring. Current and future challenges related to telehealthcare are discussed.
Keywords: Telehealth, remote monitoring, rural, remote, access to health care
The falling costs of information and communication technologies (ICTs) and digital storage, higher computing speeds, and new options for high-speed bandwidth have created unprecedented opportunities to deploy telehealthcare to improve health outcomes.1 These rapid advances in the capabilities of digital technologies, however, have often outpaced the capacity of health-care systems to operationally and effectively integrate these changes. While the technologies may be ready for deployment, accounting for the features of the context in which the technologies are to be implemented, such as rurality and remoteness, requires careful consideration. Thoughtfultelehealthcare program design that meaningfully engages both patients and providers in rural and remote communities, and importantly enhances care and improves outcomes, is paramount to success.
Given the World Health Organization’s (WHO) definition of telehealthcare, which emphasizes delivery of health services where distance is a critical factor, improving access to health care for people living in rural and remote communities should be a key outcome of digital health technology use. The unique social and physical features of each rural or remote environment, however, can present challenges to the successful implementation of digital technology in the service delivery of health care, making it unlikely that one solution will apply equally to all settings and situations. The following article will provide a practical, clinical overview of the potential of digital technologies that can support the provision of care for people living with respiratory diseases such as chronic obstructive pulmonary disease (COPD), asthma, and sleep apnea in rural and remote communities. While we recognize the importance of care encompassing the range of multi-morbidities and needs that occur concomitantly with respiratory illness, the focus of this article relates specifically to care of respiratory conditions.
The contexts of rural and remote communities
In 2014, 50% of the world’s population was considered to be rural, with the most concentrated rural populations located in the developing countries of Asia and Africa.2 There is considerable variability between countries in the parameters used to classify communities as rural or remote. Classifications are contingent on factors such as the country’s geographical size, population distribution, and transportation infrastructure. Remote and rural communities exist on a continuum of remoteness, where remoteness can be interpreted as:
limited access to a range of services, some of which are available in smaller and others in larger centres; the remoteness of a location can thus be measured in terms of how far one has to travel to centres of various sizes.3
Significant diversity among rural and remote communities within the same country must also be considered, with each community possessing a unique history, population, economic and social infrastructure, and distance from larger centers.3 There are commonalities, however, that characterize remote communities in particular. According to Slack et al.,4 these characteristics often include a harsh climate, small population base, lower incomes and levels of education than are found in non-remote areas, and a higher proportion of indigenous residents. Remoteness, by definition, means increased cost and limited access to goods, transportation, and services, including health care.4 Air transportation, the availability of which is highly dependent on financial resources and climatic conditions, is typically the most common mode of accessing physician care from remote communities through regional or specialized referral centres.5 People residing in remote communities can also frequently be considered both vulnerable in terms of health and underserved in terms of health care,6,7 highlighting the importance of finding novel solutions to address inequalities in access.
At a population level, health status is often inversely proportional to the degree of remoteness.8 In spite of the enormous differences between high- and low-resource countries, access to adequate health care in rural and remote environments is a universal challenge.9 For example, compared to urban dwellers, rural and remote Canadians experience shorter life expectancy, higher mortality rates, higher rates of smoking, higher prevalence of risk factors for chronic illness, higher hospitalization rates, greater utilization of emergency room services,10and less access to after-hours care.11
Particularly salient to our discussion of the use of telehealthcare by rural and remote communities is consideration of available local infrastructure. Telehealthcare is an option only when electricity is available and adequate ICT infrastructure exists.1 These requirements present particular challenges for mounting telehealthcare programs in remote communities in general, but for those located in low-resource countries in particular. Technology-related barriers to the use of telehealthcare include the costs of equipment, transport, and maintenance; unstable electrical power supplies; lack of or unreliable Internet connectivity; and limited band-width.1 Recognizing that broadband connectivity is a powerful resource in the emerging information economy, significant effort is being expended in many countries to bridge the “digital divide.”12 Emerging cost-effective solutions for providing non-fixed line broadband and Internet access to sparsely populated regions encompass technologies such as ultrahigh throughput capacity satellites and Compressed Transmission Systems that replace large cellular transmission base stations with palm-sized devices that can be mounted to existing elevated structures.13 Solutions such as these will increasingly enable the provision of telehealthcare to patients in rural and remote communities in both high- and low-resource countries.
Telehealthcare
Telehealthcare is a broad term used to encompass the delivery of health-care services and information through ICT. It includes clinical applications such as remote monitoring, live videoconferencing between patients and providers, and access to specialist services such as consultation and medical imaging, as well as nonclinical services such as provider training, administrative meetings, and continuing education of health professionals using ICT services.1 In terms of respiratory care, remote monitoring, consultations, pulmonary rehabilitation (PR), pharmacy, and sleep monitoring can promote the patient–provider relationship and will each be discussed in subsequent sections (Figure 1).
Figure 1.
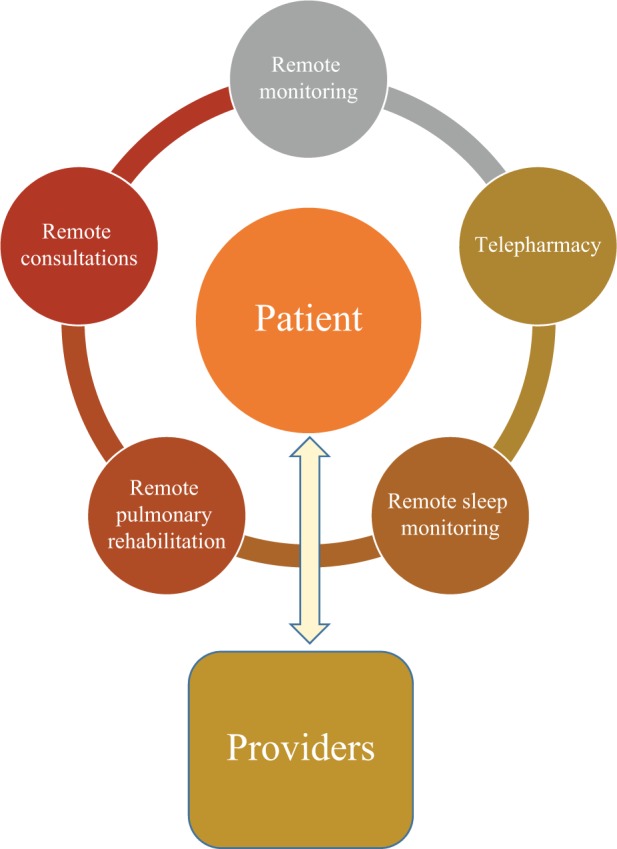
Telehealthcare applications to promote respiratory cares.
Telehealthcare can promote patient-centered care by facilitating communication between patients, their carers, and providers; supporting self-management with provider feedback; improving medication management, including correct use and adherence to prescribed medications; and mitigating issues related to poor health literacy.1,14
The technologies employed in telehealthcare include live videoconferencing, the Internet, imaging, streaming media, and both terrestrial and wireless communications.15 “Store-and-forward” telehealth involves the capture and storage of digital images, video, audio, and observations of daily living such as medication adherence, diet, and exercise on client devices, which are then securely transmitted to a remote provider.16 This asynchronous technology is effective in situations where immediate responses are not critical. Synchronous or real-time technology involves two-way interactions such as videoconferencing. At present, the widely used telehealthcare service globally is in cardiology/electrocardiology.1
Technical, organizational, social, and legal considerations must all be taken into account in order to implement a successful telehealthcare program (Figure 2).1,17 One or more barriers, however, are often present and must be addressed, especially in rural and remote settings. Technical issues include security, image resolution, and technical support. Robust security measures such as institutional firewalls can inadvertently prevent the sharing of information, while organizational policies and legislation related to data security may require significant revision.17 Because rural and remote telehealthcare programs may be collaborating with providers beyond their own jurisdictional authority, negotiation may need to occur with multiple health authorities to overcome these issues. The transmission of high-resolution image and videos demands significant bandwidth as well as cameras capable of providing the resolution required. For rural and remote settings in particular, adequate local information technology (IT) support is often costly and difficult to access.
Figure 2.
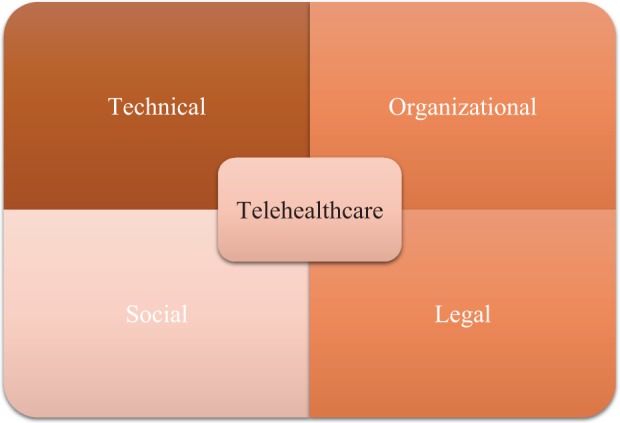
Key considerations for successful telehealthcare implementation.
Organizationally, the relatively high workforce turnover in rural and remote environments can result in staff who have not been adequately trained in the use of the technology. The lack of convincing evidence demonstrating the cost-effectiveness and economic benefits of telehealthcare programs has also slowed investment in infrastructure and programs.18 Human and cultural factors such as lack of understanding and acceptance of telehealthcare by providers and/or patients and language barriers are essential to factor into implementation design.18 Scalable and sustainable telehealthcare solutions must be developed alongside the “networked social solutions” that make the technology work.19 Legal considerations, particularly patient privacy, informed consent, and confidentiality issues related to data transfer, storage, and sharing, as well as provider authentication and liability concerns, represent a major obstacle to telehealthcare implementation in many jurisdictions.1 The practical challenges to effective implementation of telehealthcare in rural and remote settings are many.
One strategy to mitigate a number of these challenges in rural and remote communities may be greater utilization of mobile health (m-Health) devices (such as mobile phones, short message service, smartphones, personal digital assistants, and devices that work on wireless technology or bluetooth compatible devices) to improve health-care delivery.20,21 Close to three quarters of the world’s population now has access to mobile phones with increasingly powerful technical capacities, making this an especially attractive option for low-resource countries (WHO).
With their popularity, availability, portability, technological capacity, and integration into everyday life, mobile phones have enormous potential to enhance health-care delivery globally.20 Users have strong attachments to their mobile phones and a tendency to carry them at all times, creating new opportunities for frequent or continuous symptom monitoring and connecting patients with providers. In particular, m-Health has been widely used for the delivery of programs such as smoking cessation.20 Pooled results from over 9000 participants that were reported in a Cochrane systematic review22 found that mobile phone interventions (text messaging alone or in combination with an Internet-based “QuitCoach” or video messaging) significantly increased smokers’ long-term quit rates compared with control programs (risk ratio: 1.71; 95% confidence interval: 1.47–1.99).
Hamine et al.20 examined how m-Health technologies impacted adherence to chronic disease management programs. They reported high usability, feasibility, and acceptability for mobile Adherence interventions, significant improvements in adherence behaviors in half of studies, and significant improvements in disease-specific clinical outcomes in just over one-third of the studies. Patients’ primary concerns with m-Health included dependence on professional supervision, unnecessary medicalization, and undue anxiety if the technology failed. Difficulties in understanding and using the technology were reported, including technical issues such as too many menus and small buttons. For providers, concerns included the amount of time and effort required to review data and respond in a timely way. Costs, increased clinical workload and workflow problems, maintaining up-to-date records and concerns about loss of privacy, and overdependence on technology were some of the concerns. These are new concerns that are not apparent or applicable in the absence of this technology.
Consumer digital health solutions that allow patients to access health information online through patient portals, apps, and devices are increasingly being used to promote patient engagement in care.23,24These solutions can simplify interactions with the health-care system (e.g. through e-prescribing and e-scheduling of appointments), provide communication tools that permit patients to be informed partners in care (e.g. patient portals), and provide virtual care such as remote patient monitoring, all of which may be especially valuable to patients who reside far from major centers.
Remote monitoring
Use of remote monitoring is increasingly common in health care. Remote monitoring consists of the following elements: (a) electronic transfer of self-report or biometric data (e.g. oxygen saturation, pulse rate, and blood pressure) over a distance, (b) use of a device located in the patient’s home or on her/his person (mobile device), and (c) personalized feedback from a health-care professional who exercises their skills and judgment in the provision of tailored advice to the patient or automated feedback based on a predetermined algorithm.25
Interest in remote monitoring programs to support patients with chronic respiratory disease is evident in the growing number of studies on this subject elsewhere.26–34 For COPD, systematic reviews and meta-analyses on the impact of remote monitoring have reported significant reductions in the odds ratios of emergency department attendance and hospitalization for patients with COPD using remote monitoring, but no improvement in quality of life or mortality32; no evidence of reduction in acute exacerbations25; and improvements in physical activity levels.33 For asthma, remote monitoring was found to be associated with a significant reduction in hospitalizations over a 12-month period, with a more marked effect in those with severe asthma who were managed primarily in secondary care settings, but no difference in quality of life.34 These reviews have uniformly called for additional studies to build the evidence base related to the clinical and cost-effectiveness of remote monitoring in respiratory populations.
Case management, which is a collaborative process aimed at comprehensively meeting an individual’s and family’s health needs,35 is often, but not always, a key component of remote monitoring programs. While the efficacy of case management in reducing hospital re-admission is subject to debate and continues to be studied, Casas et al.36 demonstrated a reduction in re-admissions in a case management program for patients with COPD that was facilitated by IT.
New technologies, such as wearable and ambient systems, are rapidly expanding the possibilities for telehealthcare as a result of miniaturization of sensors and electronic circuits and the growing rates of smart phone utilization.37 Smart wearable systems include a wide range of wearable or implantable devices, such as sensors, actuators, smart fabrics, power supplies, wireless communication networks, processing units, multimedia devices, user interfaces, software, and algorithms for data capture, processing, and decision support.38 Wearable sensors, whose capabilities include physiological, biochemical, and motion sensing, are being developed with both diagnostic and monitoring applications.36 These systems are able to measure vital signs, such as body and skin temperature, heart rate (HR), arterial blood pressure, blood oxygen saturation (SpO2), electrocardiograms, electroencephalograms, and respiratory rate. Ninety percent accuracy in measuring respiratory rate was achieved using miniaturized acoustic sensors (microphones) on the neck to record acoustic signals associated with breathing by Corbishley and Rodriguez-Villegas.39 Ear-worn activity sensors have been used to provide early detection of the decreases in activity levels that may be associated with exacerbations of COPD.40 Biochemical sensors were tested by Ahn41 for estimating blood gas concentration. Garments that integrate sensing capabilities have allowed for embedding of sensors to collect electrocardiographic and electromyographic data. It is anticipated that the ability to print full circuit boards on fabric will rapidly advance the use of wearable technology.37 Ambient systems (pervasive networks) may have the potential to contribute to patient wellness through a broad range of activities, including memory support, information on health questions, automatic medication dispensing, and emergency communications and services.
Remote consultations
Remote consultations may occur between providers or between patients and providers. The value of remote consultations between providers in underserved communities and medical specialists located in major urban centers has been recognized for decades and typically occurred informally using the telephone. More than 40 years ago, Moore et al.42 compared satisfaction with remote consultations via television versus telephone between physicians and nurse practitioners. Since that time, dedicated sites for telehealth have become more common in some countries. Remote consultations can now be facilitated though live videoconferencing, which offers the advantages of visual information and enhanced interaction and may occur over integrated services digital network digital phone lines, network Internet Protocol (IP), or a suitable mobile phone.43
Almost 6000 telehealthcare sites that provide live videoconferencing are currently available in Canada, which is considered a global leader in this area.15 These sites provide service to 21% of the Canadian population in rural or remote areas, including 284 First Nations and 46 Inuit communities.15 Mental health and addictions services comprised more than half of Canadian telehealth services, and respiratory services were not well represented as a telehealth service, although may have been included in the Chronic Disease Services (1.2% total).
A public, state-wide telehealth service to support professionals in remote areas of the Brazilian state of Minas Gerais was recently described by Alkmim and colleagues18 who noted that development of a viable telehealth service requires a strong collaborative network that includes specialists, educational and research institutions, government, and IT providers and funders. Success of this service was found to be contingent upon the ability to meet the real needs of local health providers in addressing service demands; availability of simple and low-cost technology; and incorporate at least some face-to-face components, such as workshops and personal visits to the remote area. The significant effort expended to develop strong relationships between users and providers was found to be an essential element of success. Another key message from this report was that “Telehealth users have a natural tendency to resist altering their work routine unless doing so clearly leads to improved solutions to frequently encountered problems.”18
Robotic remote presence technology is being deployed to provide physician expertise to providers in some remote communities in North America. A remote presence robot, equipped with a digital stethoscope, ultrasound, and other basic diagnostic equipment, allows a remotely located physician to view videos, images, and graphs in real time on the computer screen and to guide providers to perform various diagnostic tests. Mendez reported on the use of robotic remote presence in a nurse-staffed clinic in an Inuit community with significant health challenges in Canada’s Far North.44 The wirelessly controlled robot was equipped with headphones, microphones, a joystick to maneuver the robot in real time, a digital stethoscope, and a printer capable of providing digitally signed hard copies of orders and recommendations from the physician in charge of the remote session. A decrease of 60% in air evacuations in cases where it normally would have been considered was reported,44 resulting in significant cost avoidance. High levels of satisfaction were reported by the patients, physicians, and nurses involved. Positive outcomes have also been reported for the use of robotic telepresence in critical care settings,45–48 treatment of stroke,49–51 telementoring for surgical procedures,52–55 and diagnostic tests,56,57 including just-in-time training on the International Space Station.56
While digital technology has been used to bridge the gap between health-care providers in underserved communities and medical specialists58 for some time, remote consultations between specialists and patients are becoming increasingly commonplace. Use of telehealth sites allow patients to be seen by specialists without having to make the trek to a distant city. These have significantly reduced wait times for some specialist appointments and patient travel time and costs. In southeastern Ontario, Canada, 34,000 telemedicine appointments took place in 2014–2015, an increase of 29% from the previous year,59 suggesting that use of this technology is growing rapidly in Canada.
Regulations related to the practice of medicine using telehealthcare vary widely between jurisdictions. The American Medical Association60 supports the practice of prescribing medication using telemedicine technologies, provided that a patient–physician relationship has first clearly been established. The Australian Medical Association61 welcomed plans for expansion of telemedicine service by the Labour Party to provide services to patients who would otherwise limited or no access to these services.
Remote Pulmonary Rehabilitation
Given that PR is one of the cornerstones of COPD management and that there continues to be limited access to PR programs for those individuals who would benefit,62–64 remote PR may be another strategy to increase capacity and mitigate the inconvenience and costs associated with traveling to a central location.
Live videoconferencing of PR programs to participants in remote settings has been reported in Scotland and Canada. Participants at five sites in Scotland were linked by videoconferencing to a remote “hub” where the PR program was led by a central physiotherapist and supervised locally by a physiotherapy assistant.65 While data collection for walking distances and respiratory questionnaires was a challenge for this project, Godden et al.65 reported carbon savings estimates of between 111 and 568 kg and cost savings of £55 per patient for the telehealth program. The telehealth classes increased the number of participants by approximately 30%. In the Canadian study, participants in nine small communities traveled to local telehealth sites for videoconferenced rehabilitation sessions identical to the standard sessions offered in the hospital setting and received on-site supervision from a trained health-care professional.66 Quality of life scores and exercise capacity were similar between the remote and hospital-based PR groups,66 suggesting that remote delivery of PR programs is a viable option.
Home-based PR programs using digital technologies have been reported in several studies. Dinesen and colleagues67 described co-innovation of a tele-rehabilitation program, together with patients with COPD, their relatives, health-care providers, and other stakeholders. This program provided patients with a telehealth monitor box which provided real-time biometric data to remote providers. Patients and families were also able to view their own data on a web portal and allow district nurses and general practitioners to access their data. Because respiratory complications are a major cause of morbidity and mortality in patients with neuromuscular diseases,68 Garuti and colleagues69 ran a pilot study with 13 patients with diseases such as muscular dystrophy and concluded that home respiratory rehabilitation together with remote transmission of physiological and clinical data was feasible for this group of patients. While there has been relatively little research examining the effectiveness and safety of PR in settings without access to specialized professionals and equipment,61 some work is being initiated in this area. In examining the feasibility of using remote pulse oximetry for a future in-home PR program, Tang et al.70 found that remote measurements of SpO2 and HR were valid when compared to conventional face-to-face measurements.
Telepharmacy
Timely access to pharmacists and to prescription medications has been recognized as integral to the delivery of appropriate, patient-centered health care in remote, rural, and northern communities.71 Strategies to mitigate the barriers to accessing pharmacy services have resulted in the creation of several models of telepharmacy. A telepharmacy is a full service operation that includes prescription medications, remote pharmacists, pharmaceutical utilization review, patient education, and counseling provided to a remote site using a range of technologies.72
One telepharmacy model allows for pharmacists to provide pharmacy services, consultation, and supervision via live videoconferencing or videophone while the physical drug dispensing at the remote site is provided by a pharmacy technician.73 This model is widely used in the United States with positive outcomes. For example, interactive compressed video counseling used to teach rural adolescents metered-dose inhaler technique was found to be superior compared to written instructions alone.74
Another model deploys the use of automated drug dispensing (packaging and labeling) technologies such as kiosks in remote communities provides for prescription medications to be accessed even in those communities that conventional telepharmacy cannot reach.75 In 2011, the Ontario Rural and Northern Health Care Panel recommended the deployment of emerging telepharmacy technologies as safe, cost-effective, and implementable solutions to address pharmacy needs in remote communities.76 The innovative MedCentre kiosks accredited under Ontario’s new guidelines address the barriers of cost, time, language, and scarcity of personnel and supporting infrastructure.76 PharmaTrust MedCentres are fully automated, pharmacist-controlled prescription medication remote dispensing units that integrate prescription scanning and identification, patient–pharmacist teleconferencing, and automated drug dispensing into a single portable kiosk.76 Early indications suggest a high level of consumer satisfaction with the service, although formal evaluation remains ongoing.
Disadvantages of telepharmacy include reluctance or inability to use the technology, particularly for older persons.77 The pharmacist’s ability to fully assess a patient’s condition is limited to some extent when face-to-face interaction is not present. Kiosks have also have specific limits to the number of medications that can be stocked. As with all dispensing, pharmaceutical misadventure (errors related to any aspect of medication prescribing, dispensing, administration, and monitoring)78remains a risk.71
Remote sleep monitoring
For patients in rural and remote communities who require evaluation of sleep-disordered breathing, remote sleep monitoring (home sleep tests or HSTs) can provide a viable alternative to in-lab sleep disorders evaluation,79 although there continue to be concerns about reliability of the technology compared to the gold standard of in-lab evaluation. Continuous improvements in the fidelity of recording, though, have vastly improved the ability of multichannel HSTs to demonstrate excellent correlation with in-facility polysomnography. Further study of the potential role of remote sleep monitoring is needed.
Current and future challenges in telehealthcare
As technology has become more affordable, more powerful, and more ubiquitous in modern life, an appreciation for the potential of technology to improve care and reduce costs has driven the growing interest in telehealthcare. May80 suggests that telehealthcare developed as an effort to “discipline the demand” anticipated to be generated by the growing populations of older adults with chronic illnesses, a perspective which contributes to the eagerness of funders and governments to implement telehealthcare programs.
The absence of evidence on cost-effectiveness and economic benefits remains a daunting challenge for adoption of telehealthcare programs. Findings from the WHO Global Observatory on e-Health Survey1 indicated that the most prevalent barrier to implementation of telehealthcare programs was the perception that costs were too high, highlighting the need for robust economic evaluations of these programs. Legal issues surrounding patient privacy and confidentiality were also a major barrier for developed countries, as were organizational cultures unaccustomed and/or resistant to delivering care using ICTs.
Organizational cultures can pose significant obstacles to integrating and embedding telehealthcare technologies into existing health-care systems. Normalization (the routine embedding of a program in everyday practice) of telehealthcare was examined by May and colleagues.81 This study suggests that successful normalization (four stages: implementation, adoption, translation, and stabilization) of telehealthcare services was contingent upon a positive link with a policy level sponsor, development of supportive organizational structures, enrolment of cohesive, cooperative groups, and the development of new procedures and protocols by professionals. Complexity at each of the four levels is frequently underestimated, resulting in the failure of telehealthcare programs to become integrated as mainstream health services.
Important ethical issues related to telehealthcare remain unresolved. Because, in part, large trials of telehealthcare have cast doubt upon whether these technologies can result in improved clinical outcomes or cost savings, understandings of the role of health technologies continue to evolve.80According to Greenhalgh,82 the voices of users (patients) have been essentially absent in the development of telehealthcare programs to this point. Ongoing user and carer involvement is a characteristic of ethical telehealthcare.83 Key questions related to telehealthcare posed by May80 include whether telehealthcare compensates for the withdrawal of face-to-face relationships in health-care delivery and whether the redistribution of the burden of care to patients, families, and social networks associated with telehealthcare is, in fact, sustainable, or even desirable. “Telehealthcare distributes more work amongst fewer people, and makes being a patient more difficult because it adds a new burden of co-ordinating and managing technologies and fragmented services”.80 For residents of rural and remote communities, these issues may be tempered by the enhanced access to health care made possible by telehealthcare.
The enormous capacity of telehealthcare technologies to organize and collect patient data has both positive and negative consequences. Epidemiological surveillance using telehealthcare for public health concerns may prove to be a powerful tool in the near future. The ability to provide surveillance can also result in unexpected outcomes with important clinical implications. Protests by French citizens were reported in the popular media84 in response to the government’s plan in 2014 to require an electronic sensor on continuous positive airway pressure devices to monitor use. Below a certain level of use, patients could be deemed noncompliant and reimbursement for the devices denied. It is likely that the nature and volume of ethical concerns related to telehealthcare will become increasingly common as these technologies are more widely implemented.
Conclusions
The realities of limited access to health care, together with the uniqueness of rural and remote communities and global initiatives to reduce the use of fossil fuels, create an appropriate context for the use of telehealthcare and related technologies. Additional study, however, is necessary to more fully understand how best to use these technologies, their potential benefit to patient care and health outcomes, and the overall economic implications of telehealthcare. The impact of telehealthcare on both patients and their families, as well as on healthcare providers and the health-care system, must also be meaningfully appreciated and characterized. Shifting the disease-focused paradigm that has characterized much of the telehealthcare literature to one that addresses the diverse medical, emotional, and support needs of people living with respiratory illness is a change that is yet to be apparent in the literature. Nonetheless, telehealthcare holds significant promise as a technology to improve access for people living in rural and remote communities.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. World Health Organization. Telemedicine: Opportunities and developments in member states, http://www.who.int/goe/publications/goe_telemedicine_2010.pdf (2010, accessed 9 September 2015). [Google Scholar]
- 2. United Nations. Population Division. Population Facts, http://www.un.org/en/development/desa/population/publications/pdf/popfacts/PopFacts_2014-3.pdf (2014, accessed 12 September 2015).
- 3. Australian Institute of Health and Welfare. Rural, regional and remote health: a guide to remoteness classifications. Rural Health Series No. 4, http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442459567 (2004, accessed 30 August 2015).
- 4. Slack E, Bourne LS, Gertler MS. Small, rural and remote communities: the anatomy of risk, http://www.law-lib.utoronto.ca/investing/reports/rp18.pdf (2003, accessed 10 August 2015).
- 5. Young TK, Chatwood S. Health care in the North: what Canada can learn from its circumpolar neighbors. CMAJ 2011; 183(2): 209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brundisini F, Giacomini M, DeJean D, et al. Chronic disease patients’ experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser [Internet], http://www.hqontario.ca/en/documents/eds/2013/full-report-OCDM-rural-health-care.pdf (2013, accessed 9 August 2015). [PMC free article] [PubMed]
- 7. Satariano WA, Scharlach AE, Lindeman D. Aging, place and technology: towards improving access and wellness in older populations. J Aging Health 2014; 26(8): 1373–1389. [DOI] [PubMed] [Google Scholar]
- 8. Phillips A. Health status differentials across rural and remote Australia. Aust J Rural Health 2009; 17: 2–9. [DOI] [PubMed] [Google Scholar]
- 9. Strasser R. Rural health around the world: challenges and solutions. Fam Pract 2003; 20: 457–463. [DOI] [PubMed] [Google Scholar]
- 10. Canadian Institute for Health Information. How healthy are rural Canadians? An assessment of their health status and health determinants. Ottawa: CIHI, https://secure.cihi.ca/…/rural_canadians_2006 (2006, accessed 21 August 2015). [Google Scholar]
- 11. Canadian Institute for Health Information. Disparities in primary care experiences among Canadians with ambulatory care sensitive conditions, https://secure.cihi.ca/free_products/PHC_Experiences_AiB2012_E.pdf (2012, accessed 4 August 2015).
- 12. Smillie-Adjarkwa C. Is the Internet a useful resources for indigenous women living in remote communities in Canada, Australia and New Zealand to access health care resources? http://www.yorku.ca/anthna/DigitalDivide.pdf (2005, accessed 21 September, 2015).
- 13. Theckadath D, Thomas TJ. Rural broadband deployment. Publication NO. 2011-57-E. Ottawa, Canada, Library of Parliament, http://www.parl.gc.ca/Content/LOP/ResearchPublications/2011-57-e.pdf (2011, accessed 21 September 2015).
- 14. Lao X, Zhang J, Bai C. The implication of telehealthcare in COPD management of China. Expert Rev Resp Med 2013; 7(5): 459–463. [DOI] [PubMed] [Google Scholar]
- 15. Canada Health Infoway. Telehealth benefits and adoption: connecting people and providers across Canada, https://www.infoway-inforoute.ca/en/component/edocman/resources/reports/334-telehealth-benefits-and-adoption-connecting-people-and-providers-summary (2011, accessed 1 September 2015).
- 16. Robert Wood Johnson Foundation. E-Primer 3: Health in everyday living, http://www.projecthealthdesign.org/media/file/E-primer_3.pdf (nd, accessed 22 September 2015).
- 17. Dixon BE, Hook JM, McGowan JJ. Using telehealth to improve quality and safety: Findings from the AHRQ Health IT portfolio, https://healthit.ahrq.gov/sites/default/files/docs/page/Telehealth_Issue_Paper_Final_0.pdf (2008, accessed 22 September 2015).
- 18. Alkmim MB, Figueira RM, Marcolino MS, et al. Improving patient access to specialized health care: the Telehealth Network of Minas Gerais, Brazil. Bull World Health Organ 2012; 90: 373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Greenhalgh T, Swinglehurst D. Studying technology use as social practice: the untapped potential of ethnography. BMC Med 2011; 9: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hamine S, Gerth-Guyette E, Faulx D, et al. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res 2015; 17(2): e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hardinge M, Rutter H, Velardo C, et al. Using a mobile health application to support self-management in chronic obstructive pulmonary disease: a six month cohort study. BMC Med Inform DecisMak 2013; 15: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whittaker R, McRobbie H, Bullen C, et al. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev 2012; 11: CD006611. [DOI] [PubMed] [Google Scholar]
- 23. Health Canada. Unleashing innovation: Excellent Healthcare for Canada. Report of the Advisory Panel on Healthcare Innovation, http://www.healthycanadians.gc.ca/publications/health-system-systeme-sante/report-healthcare-innovation-rapport-soins/alt/report-healthcare-innovation-rapport-soins-eng.pdf (2015, accessed 22 September 2015).
- 24. Barranco-Mendoza A, Persaud D. Virtual health-care communities: the use of web-based and mobile intelligent technologies for risk assessment and health management in rural and remote communities In: Kulig J, Williams A. (eds) Health in Rural Canada. Vancouver: UBC Press, 2012, pp. 178–196. [Google Scholar]
- 25. Criner GJ, Bourbeau J, Diekemper R, et al. Prevention of acute exacerbations of chronic obstructive pulmonary disease: American College of Chest Physician and Canadian Thoracic Society Guidelines. Chest 2015; 247(4): 894–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Clark NM, Gong ZM, Si JW, et al. A randomized trial of a self-regulation intervention for women with asthma. Chest 2007; 132: 88–97. [DOI] [PubMed] [Google Scholar]
- 27. de Toledo P, Jimenez S, delPozo F, et al. Telemedicine experience for chronic care in COPD. IEEE Trans InfTechnol Biomed 2006; 10: 567–573. [DOI] [PubMed] [Google Scholar]
- 28. Henderson C, Knapp M, Fernandez JL, et al. Cost effectiveness of telehealth for patients with long term conditions (Whole Systems Demonstrator telehealth questionnaire study): nested economic evaluation in a pragmatic, cluster randomised controlled trial. BMJ 2013; 346: f1035. [DOI] [PubMed] [Google Scholar]
- 29. Pinnock H, Hanley L, McCloughan L, et al. Effectiveness of telemonitoring integrated into existing clinical services on hospital admission for exacerbation of chronic obstructive pulmonary disease: research blind, multicenter, randomized controlled trial. BMJ 2013; 347: f6070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Trappenberg JCA, Niesink A, de Weert-van Oene GH, et al. Effects of telemonitoring in patients with Chronic Obstructive Pulmonary Disease. Telemed e-Health 2008; 14(2): 138–146. [DOI] [PubMed] [Google Scholar]
- 31. Vitacca M, Bianchi L, Guerra A, et al. Tele-assistance in chronic respiratory failure patients: a randomised clinical trial. Eur Respir J 2009; 33: 411–418. [DOI] [PubMed] [Google Scholar]
- 32. McLean S, Nurmatov U, Liu JL, et al. Telehealthcare for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2011; (7): CD007718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lundell S, Holmner A, Rehn B, et al. Telehealthcare in COPD: a systematic review and meta-analysis on physical outcomes and dyspnea. Resp Med 2015; 109(1): 11–26. [DOI] [PubMed] [Google Scholar]
- 34. McLean S, Chandler D, Nurmatov U, et al. Telehealthcare for asthma. Cochrane Database Syst Rev 2010; Oct 6(10): CD007717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Case Management Society of America. What is a case manager? http://www.cmsa.org/Home/CMSA/WhatisaCaseManager/tabid/224/Default.aspx (2015, accessed 22 September 2015).
- 36. Casas A, Troosters T, Garcia-Aymerich J, et al. Integrated care prevents hospitalisations for exacerbations in COPD patients. Eur Respir J 2006; 28: 123–130. [DOI] [PubMed] [Google Scholar]
- 37. Patel S, Park H, Bonato P, et al. A review of wearable sensors and systems with application in rehabilitation. J Neuro Eng Rehabil 2012; 9: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chan M, Esteve D, Fourniols J-Y, et al. Smart wearable systems: Current status and future challenges. Artif Intell Med 2012: 56: 137–156. [DOI] [PubMed] [Google Scholar]
- 39. Corbishley P, Rodriguez-Villegas E. Breathing detection: towards a miniaturized, wearable, battery-operated monitoring system. IEEE Trans Biomed Eng 2008; 55: 196–204. [DOI] [PubMed] [Google Scholar]
- 40. Atallah L, Zhang J, Lo BPL, et al. Validation of an ear worn sensor for activitymonitoring in COPD. Am J Respir Crit Care Med 2010; 181: A1211. [Google Scholar]
- 41. Ahn CH, Jin-Woo C, Beaucage G, et al. Disposable smart lab on a chip for point-of-care clinicaldiagnostics. Proc IEEE 2004; 92: 154–173. [Google Scholar]
- 42. Moore GT, Willemain TR, Bonanno R, et al. Comparison of television and telephone for remote medical consultation. NEJM 1975; 292(14): 729–732. [DOI] [PubMed] [Google Scholar]
- 43. NHS Institute for Innovation and Improvement. Video conferencing, http://www.institute.nhs.uk/building_capability/technology_and_product_innovation/video_conferencing.html (2013, accessed 22 September, 2015).
- 44. Mendez I, Jong M, Keays-White D, et al. The use of remote presence for health care delivery in a northern Inuit community: a feasibility study. Int J Circumpolar Health 2013; 72: 2 1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Angus DC, Kelley MA, Schmitz RJ, et al. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA 2000; 284: 2762–2770. [DOI] [PubMed] [Google Scholar]
- 46. McNelis J, Schwall GJ, Collins JF. Robotic remote presence technology in the surgical intensive care unit. J Trauma Acute Care Surg 2012; 72: 527–530. [DOI] [PubMed] [Google Scholar]
- 47. Sucher JF, Todd SR, Jones SL, et al. Robotic telepresence: a helpful adjunct that is viewed favorably by critically ill surgical patients. Am J Surg 2011; 202: 843–847. [DOI] [PubMed] [Google Scholar]
- 48. Vespa PM. Multimodality monitoring and telemonitoring in neurocritical care: from microdialysis to robotic telepresence. Curr Opin Crit Care 2005; 11: 133–138. [DOI] [PubMed] [Google Scholar]
- 49. Lai F. Stroke networks based on robotic telepresence. J Telemed Telecare 2009; 15: 135–136. [DOI] [PubMed] [Google Scholar]
- 50. Liman TG, Winter B, Waldschmidt C, et al. Telestroke ambulances in prehospital stroke management: concept and pilot feasibility study. Stroke 2012; 43: 2086–2090. [DOI] [PubMed] [Google Scholar]
- 51. Silva GS, Farrell S, Shandra E, et al. The status of telestroke in the United States: a survey of currently active stroke telemedicine programs. Stroke 2012; 43: 2078–2085. [DOI] [PubMed] [Google Scholar]
- 52. Agarwal R, Levinson AW, Allaf M, et al. The RoboConsultant: telementoring and remote presence in the operating room during minimally invasive urologic surgeries using a novel mobile robotic interface. Urology 2007; 70: 970–974. [DOI] [PubMed] [Google Scholar]
- 53. Mendez I, Hill R, Clarke D, et al. Robotic long-distance telementoring in neurosurgery. Neurosurgery 2005; 56: 434–440. [DOI] [PubMed] [Google Scholar]
- 54. Rothenberg SS, Yoder S, Kay S, et al. Initial experience with surgical telementoring in pediatric laparoscopic surgery using remote presence technology. J Laparoendosc Adv Surg Tech 2009; 19(Suppl 1): S219–222. [DOI] [PubMed] [Google Scholar]
- 55. Sereno S, Mutter D, Dallemagne B, et al. Telementoring for minimally invasive surgical training by wireless robot. Surg Innov 2007; 14: 184–191. [DOI] [PubMed] [Google Scholar]
- 56. Foale CM, Kaleri AY, Sargsyan AE, et al. Diagnostic instrumentation aboard ISS: just in-time training for non-physician crewmembers. Aviat Space Environ Med 2005; 76: 594–598. [PubMed] [Google Scholar]
- 57. Boniface KS, Shokoohi H, Smith ER, et al. Teleultrasound and paramedics: real-time remote physician guidance of the focused assessment with sonography for trauma examination. Am J Emerg Med 2011; 29: 477–481. [DOI] [PubMed] [Google Scholar]
- 58. Luk R, Ho M, Aoki PM. Asynchronous remote consultation for Ghana, http://arxiv.org/abs/0801.1927 (2008, accessed 22 September 2015).
- 59. Glauser W, Nolan M, Remfry A. Telemedicine on the rise across Canada, http://healthydebate.ca/2015/06/topic/telemedicine-across-canada (2015, accessed 22 September 2015).
- 60. American Medical Association. Telemedicine. Is prescription writing allowed? http://www.ama-assn.org/ama/pub/physician-resources/legal-topics/telemedicine.page (2015, accessed 22 September 2015).
- 61. Australian Medical Association. Telemedicine an important component of a modern health system, https://ama.com.au/ausmed/telemedicine-important-component-modern-health-system (2012, accessed 30 August 2015).
- 62. Camp P, Hernandez P, Bourbeau J, et al. Pulmonary rehabilitation in Canada: a report from the canadian thoracic society/canadian respiratory health professionals. Canadian Respir J 2015; 22(3): 147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Garvey C, Fullwood MD, Rigler J. Pulmonary rehabilitation exercise prescription in chronic obstructive lung disease: US survey and review of guidelines and clinical practices. J Cardiopulm Rehabil Prev 2013; 33(5): 314–322. [DOI] [PubMed] [Google Scholar]
- 64. Yohannes AM, Connolly MJ. Pulmonary rehabilitation programmes in the U.K.: a national representative survey. Clin Rehabil 2004; 18: 444–449. [DOI] [PubMed] [Google Scholar]
- 65. Godden D, McClusky C, Barrow M. Evaluation of remote pulmonary rehabilitation in Scotland: Final report, http://www.sctt.scot.nhs.uk/wp-content/uploads/Remote-PR-in-Scotland.pdf (2011, accessed 11 August 2015).
- 66. Stickland MK, Jourdain T, Wong EYL, et al. Using Telehealth technology to deliver pulmonary rehabilitation to patients with chronic obstructive pulmonary disease. Can Respir J 2011; 18(4): 216–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Dinesen B, Seeman J, Gustafsson J. Development of a program for tele-rehabilitation of COPD patients across sectors: co-innovation in a network. Int J Integr Care 2011; 11: e012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Perrin C, Unterborn JN, D’Ambrosio, et al. Pulmonary complications of chronic neuromuscular diseases and their management. Muscle Nerve 2004; 29: 5–27. [DOI] [PubMed] [Google Scholar]
- 69. Garuti G, Bagatti S, Verucchi E, et al. Pulmonary rehabilitation at home guided by telemonitoring and access to healthcare facilities for respiratory complications in patients with neuromuscular disease. Eur J Phys Rehabil Med 2013; 49: 51–57. [PubMed] [Google Scholar]
- 70. Tang J, Mandrusiak A, Russell T. The feasibility and validity of a remote pulse oximetry system for pulmonary rehabilitation: pilot study. Int J Telemed Appl 2012; 2012: 798791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Soon JA, Levine M. Rural pharmacy in Canada: pharmacist training, workforce capacity and research partnerships. Int J Circumpolar Health 2011; 70(4): 407–418. [DOI] [PubMed] [Google Scholar]
- 72. Angaran DM. Telemedicine and telepharmacy: current status and future implications. Am J Health Syst Pharm 1999; 56(14): 1405–1426. [DOI] [PubMed] [Google Scholar]
- 73. Nissen L, Tett S. Can telepharmacy provide pharmacy services in the bush? J Telemed Telecare 2003; 9(suppl 2): 39–41. [DOI] [PubMed] [Google Scholar]
- 74. Bynum AB, Hopkins D, Thomas A, et al. The effect of telepharmacy counseling on metered-dose inhaler technique among adolescents with asthma in rural Arkansas. Telemed J E-Health 2001; 7(3): 207–217. [DOI] [PubMed] [Google Scholar]
- 75. Gheilman G. Ontario’s remote drug dispensing policy as an innovation to improve prescription medication access in remote, rural and Northern communities, http://www.healthcouncilcanada.ca/n3w11n3/HIC/Galina%20Gheihman%20-%20HIC%20Essay%20-%20Individual%20-%20Health%20Policy.pdf (2011/2012, accessed 22 September 2015).
- 76. Rural and Northern Health Care Panel (RNHCP) Rural and Northern Health Care Framework/Plan Stage 1 Report. Ontario: Ministry of Health and Long-Term Care, http://www.health.gov.on.ca/en/public/programs/ruralnorthern/docs/exec_summary_rural_northern_EN.pdf (2011, accessed 22 September 2015).
- 77. Collins B, Borders TF, Tebrink K, et al. Utilization of prescription medications and ancillary pharmacy services among rural elders in West Texas: distance barriers and implications for telepharmacy. J Health Human Serv Admin 2007; 30(1): 75–97. [PubMed] [Google Scholar]
- 78. Marcum ZA, Handler SM, Boyce R, et al. Medication misadventures in the elderly: a year in review. Am J Ger Pharmacother 2010; 8(1): 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kayyali HA, Weimer S, Frederick C, et al. Remotely attended home monitoring of sleep disorders. Telemed e-Health 2008; 14(4): 371–374. [DOI] [PubMed] [Google Scholar]
- 80. May CR. Making sense of technology adoption in healthcare: meso-level considerations. BMC Med 2015; 13: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. May C, Harrison R, Finch T, et al. Understanding the normalization of telemedicine services through qualitative evaluation. J Am Med Inform Assoc 2003; 10: 596–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Greenhalgh T, Procter R, Wherton J, et al. What is assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med 2015; 13: 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Mort M, Roberts C, Pols J, et al. Ethical implications of home telecare for older people: a framework derived from a multisite participative study. Health Expect 2013; 18: 438–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Postel-Vinay N. Remote monitoring of sleep apnoea treatment in France raises concerns, http://www.theguardian.com/society/2014/jan/21/sleep-apnoea-remote-monitoring-france (2014, accessed 22 September 2015).


