Abstract
A conceptual model linking stigma-related stress and lesbian women’s alcohol use and related problems via social factors (i.e., social constraints and social isolation), depressive symptoms, and negative reinforcement drinking motives (i.e., coping and conformity) was tested. Self-identified lesbian women (N = 1048), age 18–35 years in the United States completed an online survey of discrimination, stigma consciousness, social isolation, social constraints, depressive symptoms, drinking motives, alcohol use and related problems. The hypothesized path model showed excellent model fit. The predicted pathway of stigma-related stressors to alcohol outcomes via social factors, depressive symptoms, and coping/conformity motives was largely supported. Results highlight the importance of social factors in linking stigma-related stress to alcohol use and related problems among lesbians. Understanding the underlying social mechanisms connecting stigma to negative health outcomes may help inform intervention efforts to reduce alcohol use and related problems among lesbians and associated health disparities.
Keywords: minority stress, alcohol problems, lesbian, social constraints, coping motives, conformity motives, discrimination, stigma
Lesbian women experience greater risk for hazardous drinking (e.g. heavy drinking and symptoms of alcohol dependence) than heterosexual women (McCabe, Hughes, Bostwick, West, & Boyd, 2009) yet relatively little is known about what explains this disparity. To increase our understanding of lesbians’ alcohol use and keeping in mind Hatzenbuehler’s (2009) assertion that sexual minority stigma “gets under the skin” via processes specific to sexual minority individuals as well as general psychological processes, we developed a conceptual model informed by two relevant theoretical frameworks: (1) minority stress theory (Hatzenbuehler, 2009; Meyer, 2003) and (2) the motivational model of alcohol use (Cooper, 1994; Cox & Klinger, 1988). Integrating these perspectives to examine alcohol use and related problems among lesbians, we propose that stigma-related stress is associated with social factors (i.e., difficulty talking with others about sexual identity, and social isolation) that are associated with depressive symptoms as well as negative reinforcement drinking motives which are then associated with alcohol use and related problems. Elaborating the pathways from stigma-related stress (discrimination) to alcohol use and related problems will provide a better understanding of the negative effects of prejudice as well as offer useful information that may be used to develop interventions to reduce health disparities.
Social Factors Linking Stigma-related Stress and Health Outcomes
Meyer’s (2003) central premise was that experiences of stigma, prejudice, and discrimination create a stressful social environment that increases vulnerability for mental health (and we would argue substance) problems (see also Williams & Mann, in press). As Hatzenbuehler (2009) emphasized, it is essential to identify underlying processes to increase our understanding of processes by which stigma is related to negative health outcomes, such as lesbians’ alcohol use and related problems, in order ultimately to reduce health disparities.
Social processes may moderate or mediate the association between stigma-related stress and health outcomes. Social isolation has been identified as an important mediator of the association between stigma and negative health outcomes (see review by Hatzenbuehler, Phelan, & Link, 2013). Among sexual minority men and women, social isolation mediated the relationship between stigma-related stress and psychological distress (Hatzenbuehler, Nolen-Hoeksema, & Dovidio, 2009), and social support indirectly explained proximal stigma-related stress and self-reported health (Williams, Mann, & Fredrick, in press). For lesbian and bisexual women, distal experiences of victimization (i.e., harassment and discrimination) and proximal stressors (i.e., internalized heterosexism and concealment) were indirectly related to substance use and mental health problems via social support and spirituality. Both victimization and internalized heterosexism were also directly linked to substance use (Lehavot & Simoni, 2011).
Another social factor expected to function as a mediator is difficulty talking with others about one’s sexual identity, or social constraints (Lepore, 2001). Those who have difficulty talking with others about stressful or traumatic events (or sexual identity) may not be able to process their negative emotional reactions resulting in increased distress. Although the empirical literature on social constraints has focused primarily on stressors such as cancer (Adams, Winger, & Mosher, 2015) and bereavement (e.g., Juth, Smyth, Carey, & Lepore, 2015), social constraints regarding sexual identity have been found to be associated with sexual minority stress and physical distress among lesbian women (Lewis, Derlega, Clarke, & Kuang, 2006). Furthermore, in a sample of lesbian women, social constraints and rumination/brooding were sequential mediators of the association between stigma consciousness, the expectation of others’ prejudice and discrimination, and psychological distress (Lewis, Milletich, Mason, & Derlega, 2014).
Previous research suggests that a negative social environment characterized by feelings of social isolation or one that constrains an individual’s willingness to talk with others or seek support is associated with negative affect and psychological distress. We propose that these social factors are also associated with negative reinforcement drinking motives, that is, drinking to regulate a negative emotional state or to avoid social rejection (Cooper, 1994).
Drinking Motives
According to the motivational model of alcohol use, individuals drink to obtain outcomes that fulfill a specific need (Cooper, 1994; Cox & Klinger, 1988). Drinking motives have been grouped into four broad categories: social, conformity, coping, and enhancement. Coping (i.e., drinking to reduce negative affect) and conformity (i.e., drinking to avoid social rejection) motives can be characterized as negatively reinforcing motives in which individual drink to avoid negative consequences that are either internal or external (Cox & Klinger, 1988). Coping motives have been shown to relate to problematic alcohol use (e.g., Merrill, Wardell, & Read, 2014) and, among motive types, have been shown to be the strongest predictor of alcohol problems (Kuntsche, Knibbe, Gmel, & Engels, 2005). Conformity-motivated drinking has also been shown to predict greater alcohol use (Stewart, Zvolensky, & Eifert, 2001) and drinking-related problems (Lewis et al., 2008; Roos, Pearson, & Brown, 2015). These studies highlight that drinking as a way to cope or avoid negative external experiences may represent a maladaptive type of drinking (Cooper, 1994) that increases an individual’s vulnerability to experiencing negative drinking consequences.
Evidence supports that poor mental health functioning is associated with drinking to relieve negative states. A review of drinking motivations found that poor mental health (e.g., depression, anxiety sensitivity) was associated with drinking to cope motives (Kuntsche et al., 2005). Coping and conformity motives are strongly endorsed by those with anxiety symptoms (Lewis et al., 2008; Stewart et al., 2001). Thus, it appears that depressive symptoms would be linked to negative drinking motives, which in turn increase problems associated with drinking. Indeed, prior research has shown that drinking motives mediate the effects of predictors on alcohol involvement, including negative emotions (e.g., Goldsmith, Tran, Smith, & Howe, 2009).
The Conceptual Model
The proposed conceptual model (see Figure 1) furthers understanding of how stigma-related stress is associated with alcohol use in lesbian women by examining two social factors (i.e., group specific social constraints regarding sexual identity and general social isolation). Moreover, the model suggests that stigma-related stress is linked to alcohol use and related problems via social factors that are then associated with depressive symptoms and negative reinforcement drinking motives; drinking motives are associated with alcohol use and related problems. While mediators of the association between distal and proximal sexual stigma-related stressors and negative outcomes have been studied among lesbians (Lehavot & Simoni, 2011; Lewis et al. 2014), ours is the first study to incorporate both social factors and drinking motives in an attempt to better explain hazardous drinking (quantity and related problems).
Figure 1.
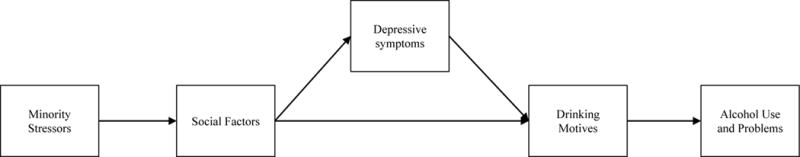
Proposed conceptual path model predicting alcohol use and problems among lesbian women.
Method
Participants and Procedure
Self-identified lesbians between 18 and 35 years of age were recruited by several United States research-based marketing firms and received incentives such as points that could be exchanged for gift cards, charitable donation, or cash. As part of a larger study, participants were required to be in a romantic relationship with another woman for at least three months. The research was approved by a university institutional review board. A total of 1,048 women completed the survey. Non-drinkers (i.e., women reporting 0 drinks per week; n = 79) were removed from analyses, leaving a sample of 969 current drinkers. The mean age of the sample was 28.80 years (SD = 4.24). Most women were White (78%) or Black (10%) and were mostly open about their sexual orientation with 64% completely out of the closet, 28% out of the closet most of the time, 6% half-in and half-out, and 2% in the closet most of the time or definitely in the closet. The median income range was $50,000-$59,999 and most participants had a Bachelor’s degree (38%) or higher (26%) followed by some college or Associate’s degree (30%).
Measures
Discrimination
Participants indicated how often they experienced discrimination because they were assumed to be lesbian in the past 12 months using a 5-point scale ranging from 1 (never) to 5 (very often). As this was a global assessment of sexual identity perceived discrimination, participants were free to interpret it in any meaningful way. This item is based on the assessment of discrimination used in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (cf. McCabe, Bostwick, Hughes, West, & Boyd, 2010). Higher scores indicated more discrimination.
Stigma consciousness
The Stigma Consciousness Questionnaire (Pinel, 1999) is 10-item scale assessing individuals’ expectations of being evaluated based on stereotypes and of rejection from others. Respondents used a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree) for items such as, “Most heterosexuals have a lot more homophobic thoughts than they actually express.” Higher scores indicating more stigma consciousness. Validity is demonstrated by associations with other measures of stigma-related stress among sexual minority women (e.g., Mason & Lewis, 2015). Cronbach’s α was .76 in the current study.
Social constraints
The original social constraints measure (Lepore, Silver, Wortman, & Wayment, 1996) was adapted to measure difficulty talking about lesbian identity and alienation from one’s social network (friends, family, intimate partner; Lewis et al., 2006). Participants responded to items such as “How often did you feel that you could discuss your feelings about your sexual identity with your (friends/family/intimate partner)” using a 6-point scale ranging from 1 (none of the time) to 6 (all of the time). Higher scores indicate more social constraints. Validity is demonstrated by correlations between social constraints regarding lesbian identity and sexual stigma-related stressors and distress (Lewis et al., 2006; 2014). Cronbach’s α was .82 in the current study.
Social isolation
Social isolation was measured with the 6-item Friendship Scale (Hawthorne, 2006). Participants used a 5-point scale ranging from 1 (almost always) to 5 (not at all to respond to items such as, “I felt isolated from other people.” Higher scores indicated more social isolation. Validity was demonstrated by associations with poorer well-being (Hawthorne 2006) and with facets of negative affect and emotion-focused coping among sexual minority women (Mason & Lewis, 2015). Cronbach’s α was .82 in the current study.
Depressive symptoms
The Center for Epidemiological Studies Depression Scale – Short Form (CES-D; Andresen, Malmgren, Carter, & Patrick, 1994), is a widely used 10-item measure assessing depressive symptoms over the past week with items such as “I felt depressed” and “I was happy.” Participants used a response scale ranging from 1 (rarely or none of the time) to 4 (most or all of the time). Higher scores indicated more depressive symptoms. Zhang et al. (2012) reported a strong correlation with the original long-form CES-D, r = .97. Cronbach’s α was .85.
Drinking motives
Two subscales of the Drinking Motives Questionnaire (Cooper, 1994) were used: the 5-item Coping subscale (e.g. to feel better, to forget about problems) and the 5-item Conformity subscale (e.g., to be liked, to fit in). Participants were asked, “The following is a list of reasons that some people give for drinking alcohol. Thinking of all the times you drink, how often would you say that you drink for each of the following reasons.” Participants responded with a scale from 1 (almost never/never) to 5 (all of the time) to items such as, “To forget about your problems” (coping) and “To fit in with a group you like” (conformity). Higher scores indicate stronger endorsement of the motive. Both subscales are associated with both heavy drinking and drinking problems (Cooper, 1994). Cronbach’s α were .88 and .83 for Coping and Conformity, respectively.
Drinking quantity
The Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985) includes a 7-day grid (i.e., Monday to Sunday) for reporting the number of standard drinks (i.e., 12 oz. beer, 1 ½ oz. of liquor, or 5 oz. of wine) typically consumed weekly over the past 90 days. Thus, for each day of the week, participants indicated the number of drinks they usually have on each day. Drinking quantity was calculated as the sum of drinks reported per week. The DDQ has convergent validity with other measures of alcohol use (Collins et al., 1985; Collins & Lapp, 1992).
Alcohol problems
Alcohol-related problems (e.g., impulsive behavior, health or interpersonal problems) were assessed over the past 90 days with the 15-item Short Index of Problems (SIP-2R; Miller, Tonigan, & Longabaugh, 1995). A scale ranging from 0 (not at all) to 3 (very much) was used to respond to items. Higher scores indicate greater severity. Using norms derived from a treatment seeking sample, for women, based on the past 30 days, scores between 0–8 is considered “Very Low,” while 34 and over as “Very High” (Miller et al., 1995). The SIP is associated with other measures of alcohol problems among outpatients (Alterman, Cacciola, Ivey, Habing, & Lynch, 2009). Cronbach’s α was .93.
Results
The descriptive statistics and bivariate correlations for the study variables are reported in Table 1. The sample reported a modest amount of discrimination (M = 2.15 on a 5-pt. scale) and stigma consciousness (M = 37.28 on a 70-pt. scale). Also, the sample reported an average of 8 drinks per week (SD = 8.02; Range = 1–60) and mean alcohol problems score of 2.06 (SD = 4.64, Range = 0–41). A third of the sample (n = 316; 32.6%) reported at least one binge drinking episode in the past week. Guidelines suggest that low-risk drinking for women is characterized by no more than seven drinks per week for women (NIAAA, n.d.) reflecting that our sample includes a range of risk levels for developing an alcohol use disorder.
Table 1.
Descriptive statistics and correlations of study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Discrimination | – | .34** | .30** | .22** | .27** | .16** | .07* | .04 | .14** |
| 2. Stigma consciousness | – | .35** | .29** | .26** | .20** | .10** | .00 | .12** | |
| 3. Social constraints | – | .47** | .44** | .31** | .32** | –.01 | .20** | ||
| 4. Social isolation | – | .64** | .40** | .28** | .01 | .24** | |||
| 5. Depressive symptoms | – | .49** | .29** | .11** | .32** | ||||
| 6. Coping motives | – | .44** | .33** | .49** | |||||
| 7. Conformity motives | – | .16** | .39** | ||||||
| 8. Drinks per week | – | .43** | |||||||
| 9. Alcohol problems | – | ||||||||
|
| |||||||||
| M | 2.13 | 37.31 | 31.75 | 10.95 | 7.31 | 8.84 | 6.22 | 8.00 | 2.06 |
| SD | 0.91 | 9.50 | 10.14 | 3.79 | 5.42 | 4.39 | 2.45 | 8.02 | 4.64 |
| Minimum | 1.00 | 12.00 | 15.00 | 6.00 | 0.00 | 5.00 | 5.00 | 1.00 | 0.00 |
| Maximum | 5.00 | 65.00 | 66.00 | 29.00 | 27.00 | 25.00 | 23.00 | 60.00 | 41.00 |
| Skewness | 0.61 | 0.07 | 0.64 | 1.13 | 1.01 | 1.48 | 2.92 | 2.41 | 4.23 |
| Kurtosis | 0.29 | –0.30 | –0.07 | 1.60 | 0.58 | 1.69 | 9.73 | 8.22 | 23.19 |
p < .01,
p < .05
The hypothesized path model (see Figure 1) was examined with Mplus version 7.3 (Muthén & Muthén, 2015). Bootstrapping with 5000 bootstrap replications was used to reduce the impact of non-normality and outliers (Shrout & Bolger, 2002). The following model fit indices were used as guidelines in evaluating model fit: comparative fit index (CFI) ≥ .95, Tucker-Lewis index (TLI) ≥ .95, root mean square error of approximation (RMSEA) ≤ .06, and standardized root mean square residual (SRMR) ≤ .08 (Hu & Bentler, 1999). Modification indices were checked to determine which paths could be added or removed to improve model fit. Bootstrapped confidence intervals were used to determine significance. The data were analyzed for missing data patterns. The analysis showed that less than 1% of data points were missing. Approximately 91% of respondents had complete data for all items. Missing data were handled with full information maximum liklihood estimation.
The hypothesized path model demonstrated good model fit, χ2 (16) = 74.00, p < .001, CFI = .97, TLI = .94, RMSEA = .06, 90% CI [.05, .08], and SRMR = .03. Consistent with both theory (e.g., self-medication hypothesis; Khantzian, 1995) and previous research (e.g., Gonzalez, Reynolds & Skewes, 2011), modification indices recommended adding a path from depressive symptoms to alcohol problems (MI = 15.48) indicating that a significant path still existed between depressive symptoms and alcohol-related problems after controlling for coping motives. Adding this path resulted in excellent model fit, χ2 (15) = 58.16, p < .001, CFI = .98, TLI = .95, RMSEA = .05, 90% CI [.04, .07], and SRMR = .03. See Figure 2 for the final model and variance accounted (i.e., R2) for in each of the endogenous variables. Direct and indirect path estimates and confidence intervals are displayed in Table 2.
Figure 2.
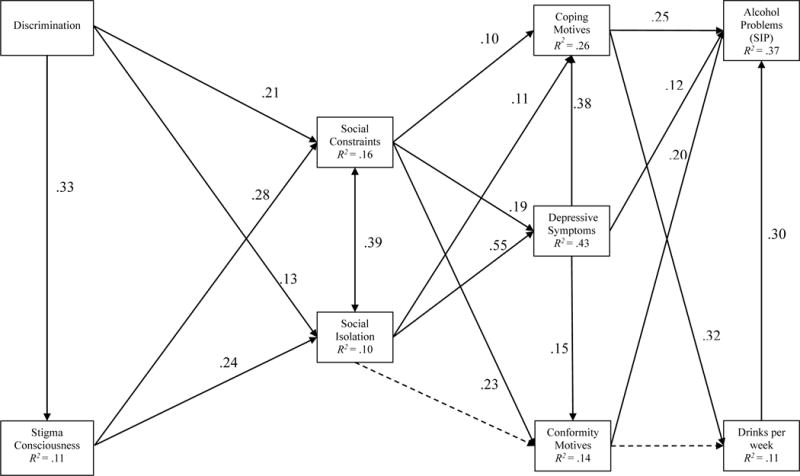
Path model predicting alcohol use and problems among lesbian women. Based on bootstrapped confidence intervals, solid lines represent significant effects and dash lines represent nonsignificant effects. There is a correlation between coping and conformity motives that is not depicted.
Table 2.
Path Estimates with Bootstrapped SEs and CIs
| Path | β | B | SE | 95% CI |
|---|---|---|---|---|
| Direct Paths | ||||
| Discrim→Stigma | 0.33 | 3.50 | 0.31 | [2.89, 4.10] |
| Discrim→SC | 0.21 | 2.38 | 0.39 | [1.62, 3.13] |
| Discrim→SI | 0.13 | 0.56 | 0.16 | [0.24, 0.88] |
| Stigma→SC | 0.28 | 0.30 | 0.04 | [0.23, 0.36] |
| Stigma→SI | 0.24 | 0.10 | 0.01 | [0.07, 0.12] |
| SC→Depress | 0.19 | 0.10 | 0.02 | [0.07, 0.13] |
| SC→Cope | 0.10 | 0.04 | 0.02 | [0.01, 0.07] |
| SC→Conform | 0.23 | 0.05 | 0.01 | [0.03, 0.08] |
| SI→Depress | 0.55 | 0.79 | 0.04 | [0.71, 0.88] |
| SI→Cope | 0.11 | 0.12 | 0.05 | [0.02, 0.22] |
| SI→Conform | 0.08 | 0.05 | 0.04 | [−.02, 0.12] |
| Depress→Cope | 0.38 | 0.31 | 0.04 | [0.24, 0.38] |
| Depress→Conform | 0.15 | 0.07 | 0.02 | [0.02, 0.11] |
| Depress→AP | 0.12 | 0.10 | 0.04 | [0.04, 0.18] |
| Cope→DPW | 0.32 | 0.58 | 0.08 | [0.43, 0.73] |
| Cope→AP | 0.25 | 0.26 | 0.05 | [0.18, 0.36] |
| Conform→DPW | 0.02 | 0.06 | 0.13 | [−00.19, 0.34] |
| Conform→AP | 0.20 | 0.38 | 0.11 | [0.19, 0.60] |
| DPW→AP | 0.30 | 0.18 | 0.03 | [0.13, 0.24] |
| Indirect Paths | ||||
| Discrim→Stigma→SC→Depress→Cope→DPW→AP | 0.001 | 0.003 | 0.001 | [0.002, 0.01] |
| Discrim→Stigma→SI→Depress→Cope→DPW→AP | 0.002 | 0.01 | 0.003 | [0.01, 0.02] |
| Discrim→Stigma→SI→Depress→Conform→AP | 0.001 | 0.01 | 0.004 | [0.002, 0.01] |
| Discrim→Stigma→SC→Depress→Conform→AP | 0.001 | 0.003 | 0.001 | [0.001, 0.01] |
| Discrim→Stigma→SI→Depress→Cope→AP | 0.004 | 0.02 | 0.01 | [0.01, 0.04] |
| Discrim→Stigma→SC→Depress→Cope→AP | 0.002 | 0.01 | 0.003 | [0.01, 0.02] |
| Discrim→Stigma→SC→Cope→AP | 0.002 | 0.01 | 0.01 | [0.004, 0.02] |
| Discrim→Stigma→SC→Conform→AP | 0.004 | 0.02 | 0.01 | [0.01, 0.04] |
| Discrim →SI→Depress→Conform→AP | 0.002 | 0.01 | 0.01 | [0.003, 0.03] |
| Discrim→SC→Depress→Conform→AP | 0.001 | 0.01 | 0.003 | [0.002, 0.02] |
| Discrim →SI→Depress→Cope→AP | 0.01 | 0.04 | 0.01 | [0.02, 0.07] |
| Discrim→SC→Depress→Cope→AP | 0.004 | 0.02 | 0.01 | [0.01, 0.04] |
| Discrim→SC→Conform→AP | 0.01 | 0.05 | 0.02 | [0.02, 0.10] |
| Discrim→SC→Cope→AP | 0.01 | 0.03 | 0.01 | [0.01, 0.06] |
Note. Discrim = discrimination; Stigma = stigma consciousness; SC = social constraints; SI = social isolation; Depress = depressive symptoms; Cope = coping motives; Conform = conformity motives; AP = alcohol problems; DPW = drinks per week.
Results revealed that discrimination was associated with more stigma consciousness, which was associated with both social factors. Social constraints were positively associated with depressive symptoms, coping motives, and conformity motives. Social isolation was associated with more depressive symptoms and coping motives but not conformity motives. Depressive symptoms were positively related to both coping and conformity motives as well alcohol-related problems. Coping motives predicted more drinks per week and alcohol-related problems. Conformity motives were associated with more alcohol-related problems, but were unrelated to drinks per week. Increased drinks per week were associated with more alcohol-related problems.
Additional Analyses
We tested two alternative models. The first model hypothesized that drinking motives would be associated with more drinking and alcohol-related problems, which would then be associated with increased depressive symptoms, followed by less social resources, and finally increased stigma-related stress. Consistent with Talley and Littlefield (2014), the second model hypothesized that stigma-related stress would be associated with increased depressive symptoms. In turn, depressive symptoms would be related to negative outcomes: 1) drinking outcomes (i.e., drinking to cope and drinking to conform, then in turn, more drinking and alcohol-related problems) and 2) fewer social resources (i.e., isolation and social constraints). Neither of these models demonstrated good model fit (alternative model 1: χ2 (20) = 301.17, p < .001, CFI = .88, TLI = .78, RMSEA = .12, 90% CI [.10, .13], SRMR = .10; alternative model 2: χ2 (18) = 200.93, p < .001, CFI = .92, TLI = .83, RMSEA = .10, 90% CI [.09, .12], and SRMR = .06. Therefore, we retained our original model.
Invariance testing was conducted to determine if model fit and path estimates differed by drinker risk status. Drinker risk status was conceptualized as those exhibiting typical binge drinking behavior or not (i.e., reporting consumption of 4 or more drinks on one occasion at least once in a typical week of drinking). Results indicated that model fit differed significantly for binge drinkers vs. non-binge drinkers. In a multi-group analysis comparing the model between binge drinkers and non-binge drinkers, there were several paths that were significantly different and improved model fit by allowing them to vary. However, the majority of these paths were only slightly different in strength of association (i.e., paths demonstrated the same sign and similar effect size). The only path that demonstrated a different pattern was the path from depressive symptoms to alcohol-related problems. This path was significant for binge drinkers (standardized beta = .25) and non-significant for non-binge drinkers (standardized beta = .03).
Discussion
Our conceptual model linking stigma-related stress and lesbians’ alcohol use and related problems via sexual minority specific and general social factors, depressive symptoms, and drinking motives was largely supported by the data. Distal perceived discrimination was associated with proximal stigma consciousness and both stigma-related stressors were associated with social constraints and social isolation. The paths in the model suggest that perceived discrimination may be internalized, resulting in expectations of being stereotyped and rejected by others, creating difficulty relating to, and being open with, others. As predicted, social isolation and social constraints were associated with depressive symptoms, and, as predicted, social constraints were associated with maladaptive drinking motives. There was also, as modeled, an indirect path from the social factors through depression to the drinking motives. Finally, both drinking motives were associated with alcohol-related problems, but only coping motives, not conformity motives, were associated with drinking quantity. Consistent with other literature, drinking to cope and drinking to conform were associated with drinking problems, even after controlling for alcohol use (Cooper, 1994). Consistent with theory (Khantazian, 1995) and research (e.g., Gonzalez et al., 2011) a path from depressive symptoms to alcohol-related problems was added to the model. The data indicated that experiences of stigma funnel through social factors to negative affect and then directly to alcohol-related problems, even adjusting for maladaptive drinking motives. This path may reflect a pattern of isolation and solitary drinking related to mood disturbance (Keough, O’Connor, Sherry, & Stewart, 2015). Furthermore, a comparison of binge drinkers vs. non-binge drinkers demonstrated that this path from depressive symptoms to alcohol-related problems was significant for binge drinkers but not for non-binge drinkers, reinforcing the idea that the role of depression is more important among lesbian women engaging in hazardous drinking.
Our results support previous findings that experiences of discrimination produce a variety of negative outcomes (Hatzenbuehler, 2009; Williams & Mann, in press), through social and coping processes (Hatzenbuehler, 2009). In our study, participants who reported experiencing more discrimination expected more rejection and stereotyping from others (stigma consciousness), felt more socially isolated, and had more difficulty talking to others about their sexual identity. Stigma consciousness was also directly related to social isolation and social constraints. According to the social-cognitive processing model (SCPM; Lepore, 2001), those who have difficulty talking with others about stressful events (i.e., social constraints) are unlikely to garner the benefits of social support which would assist in processing their emotional responses to these stressors, resulting in increased distress. In our model, both social isolation and social constraints were associated with more depressive symptoms.
Also, consistent with the motivational model of alcohol use (Cooper, 1994; Cox & Klinger, 1988), social constraints and depressive symptoms were associated with negative reinforcement drinking motives (i.e., drinking to cope and drinking to conform) that were in turn associated alcohol-related problems. Interestingly, while both coping and conformity motives were associated with alcohol-related problems, only coping motives was associated with alcohol use. The lack of a significant relationship between conformity motives and drinking may reflect that coping motives accounts for more variance in drinking, which is consistent with prior literature suggesting the salience of coping motives over other motive types (for review, see Kuntsche et al., 2005).
Although drinking motives have been examined extensively among heterosexual individuals, relatively little is known about reasons for drinking among lesbian women. Our results support the application of the motivational model of alcohol use to lesbian women’s alcohol use. In addition to offering insight regarding underlying mechanisms, drinking motives may also yield helpful information regarding alcohol use disparities. In fact, a recent study of college drinking reported lesbian/bisexual women engaged in more drinking to conform compared to heterosexual women and young women searching for sexual identity (i.e., “questioning”) engaged in more drinking to cope than other groups (Talley, Sher, Steinley, Wood, & Littlefield, 2012).
The final model also suggests the possibility of two distinguishable pathways to drinking problems among lesbian women. Social isolation links only to coping motives and not conformity motives but coping motives were associated with both drinking quantity and drinking problems, while social constraints link to both coping and conformity motives but conformity motives were associated only with drinking problems and not drinking quantity. While we did not measure drinking context, the literature on lesbian women has noted that they are more likely than heterosexual women to spend time at bars and parties (Trocki, Drabble, & Midanik, 2005) and that they experience, among other things, safety, support, and reduction of stress in lesbian bars (Gruskin, Byrne, Kools, & Altschuler, 2007). The social constraints to conformity motives to drinking problems pathway may represent a drinking pattern associated with lesbian bar culture. Individuals experiencing social constraints may drink to fit in and experience negative drinking consequences. There may also be those lesbians, experiencing social isolation, who generally drink alone or at home with a partner. The pathway here is not through conformity motives, but through coping; and drinking in this context may represent drinking to deal with internal, more than external, negative states. While this description is highly speculative, it does suggest that future research might focus not only on reasons for drinking but also drinking contexts in our ongoing effort to understand mechanisms leading to alcohol use and abuse among lesbian women.
Although we measured discrimination at the individual level, emerging research also demonstrates that structural stigma defined as “societal-level conditions, cultural norms, institutional policies that constrain the opportunities, resources, and well-being of the stigmatized” (Hatzenbuehler & Link, 2014, p. 2) plays a significant role in the health outcomes of sexual minorities (Hatzenbuehler, 2014; Hatzenbuehler, Flores, & Gates, in press). Our results reinforce the growing body of research that illustrates the power of discrimination to produce health and mental health problems for stigmatized groups. Policy and law that normalize and protect the lives and relationships of sexual minority women (and men) can potentially ease the burden of stigma and stigma-related stress.
Limitations
Limitations of our study include a relatively out, well-educated, partnered, mostly Caucasian sample recruited online in the United States. Also, we cannot know how our results would generalize to an older sample of lesbian women of those without partners. In addition, our sample, by design, reflected a range of alcohol use with one third engaged in binge drinking at least once in a typical week. The occurrence of significant alcohol-related problems was relatively low suggesting that the consequences of alcohol use in this sample were relatively minor. Thus, we cannot determine if our model would work similarly among those with more severe alcohol-related consequences without replication using a sample with more problematic alcohol use. We did, however, compare binge drinkers with non-binge drinkers and although the models were different the paths were largely similar in direction and strength except for depressive symptoms which were associated with alcohol-related problems for binge drinkers only.
We also relied on a single item to assess discrimination. Although this approach allows participants to interpret discrimination due to sexual identity broadly, it is important to replicate these findings with established multi-item measures of discrimination. As mentioned above, we do believe that further investigation of drinking context, i.e., in a bar, at home, with a partner, alone, etc., is a potentially important aspect of understanding drinking in this population. In addition, it is important to consider multiple identities in seeking a greater understanding of coping and outcomes. In previous analyses of these data looking specifically at race and SES we found that race was not, but SES was, related to increased perceptions of sexual minority discrimination. Among lesbian women, being Black was indirectly linked to more hazardous drinking but directly linked to less hazardous drinking (Lewis, Mason, Winstead, Gaskins, & Irons, 2016). Investigating the interplay of sexual identity, ethnicity, social class, ability status, and other statuses will increase our understanding of the paths from stigma-related stress to alcohol problems and other health outcomes. The degree to which this model applies to lesbian women cross-culturally and internationally awaits empirical investigation as well.
This study is also limited by its cross-sectional nature and reliance on self-reports. Although we generated the direction of the paths in our model based on our theoretical conceptualization, the design of the study precludes our ability to confirm the direction of effects. Although our model fared better than two other alternative models we tested, support for this model does not rule out the possibility that other models may do as well or better in predicting drinking and alcohol-related problems. Nevertheless, this demonstration of sequential mediation from discrimination and stigma consciousness to drinking problems reinforces the view that progressive changes in policies and social attitudes may have real consequences for lesbian women’s health and well-being.
Conclusions
Our conceptual model demonstrates the potential impact of stigma-related stressors on alcohol misuse (problems and quantity) mediated by social factors, depressive symptoms, and drinking motives. Our model also highlights the benefit of integrating a sexual minority specific framework (i.e., minority stress theory) with a general process framework (i.e., motivational model of alcohol use) to gain a more complete understanding of the underlying mechanisms of lesbian women’s alcohol use and related problems. Reducing binge drinking is a high priority health issue of the Healthy People 2020 initiative that is particularly applicable to lesbian health (Healthypeople.gov) given the alcohol-related health disparities suffered by sexual minority women. Alcohol misuse contributes to numerous individual and community/social problems including poor physical health, injury, violence, crime, and risky sexual behavior (CDC, 2016, WHO, 2004). Understanding the mechanisms by which discrimination and stigma “get under the skin” (Hatzenbuehler, 2009, p. 708) can inform efforts to intervene (e.g., Chaudoir, Wang, & Pachankis, in press) to reduce health disparities, improve lesbian health and well-being, and reduce social harms as well as illuminate our view of the negative consequences of prejudice against sexual minorities as a social issue.
Acknowledgments
Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R15AA020424 to Robin Lewis (PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The Harris Interactive Service Bureau (HISB) was responsible solely for the data collection in this study. The authors were responsible for the study’s design, data analysis, reporting the data, and data interpretation.
Biographies
Robin J. Lewis, Ph.D. is a Professor of Psychology at Old Dominion University and Director of Clinical Training for Virginia Consortium Ph. D. Program in Clinical Psychology. Her research focuses on sexual minority health and reducing health disparities for sexual minority women. She has funding from the National Institute of Alcohol Abuse and Alcoholism to study minority stress, alcohol use, and intimate partner violence among lesbian women.
Barbara A. Winstead, Ph.D. is a professor of Psychology at Old Dominion University and a faculty member with the Virginia Consortium Program in Clinical Psychology. Her research focuses on gender and relationships, with recent publications on unwanted pursuit and stalking. She is co-editor with Dr. James Maddux of Psychopathology: Foundations for a Contemporary Understanding, 3rd edition and co-author with Professor Janis Sanchez of “The Role of Gender, Race, and Class in Psychopathology.” She is co-PI with Robin Lewis (PI) on an NIAAA grant to study minority stress, alcohol use, and intimate partner violence among lesbian women.
Tyler Mason, Ph.D., is a National Institute of Mental Health postdoctoral fellow at the Neuropsychiatric Research Institute. His research interests focus on the cause, course, and treatment of eating disorders and obesity.
Cathy Lau-Barraco, Ph.D., is an Associate Professor in the Department of Psychology at Old Dominion University. Her research focuses on psychosocial determinants and consequences of alcohol use and brief interventions with at-risk populations. She is Principal Investigator of an Early Career (K01) Award from the National Institute of Alcohol Abuse and Alcoholism focused on evaluating a brief drinking intervention for nonstudent young adults.
References
- Adams R, Winger J, Mosher C. A meta-analysis of the relationship between social constraints and distress in cancer patients. Journal of Behavioral Medicine. 2015;38:294–305. doi: 10.1007/s10865-014-9601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Alterman AI, Cacciola JS, Ivey MA, Habing B, Lynch KG. Reliability and validity of the alcohol short index of problems and a newly constructed drug short index of problems. Journal of Studies on Alcohol and Drugs. 2009;70:304–307. doi: 10.15288/jsad.2009.70.304. doi:2009-06143-017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Fact sheets - Alcohol use and your health. 2016 Retrieved from: https://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm.
- Chaudoir SR, Wang K, Pachankis JE. What reduces sexual minority stress? A review of the intervention toolkit. Journal of Social Issues. doi: 10.1111/josi.12233. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Lapp WM. The Temptation and Restraint Inventory for measuring drinking restraint. Addiction. 1992;87:625–633. doi: 10.1111/j.1360-0443.1992.tb01964.x. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. doi: 10.1037/1040-3590.6.2.117. [DOI] [Google Scholar]
- Cox WM, Klinger E. A motivational model of alcohol use. Journal of Abnormal Psychology. 1988;97:168–180. doi: 10.1037//0021-843x.97.2.168. [DOI] [PubMed] [Google Scholar]
- Goldsmith AA, Tran GQ, Smith JP, Howe SR. Alcohol expectancies and drinking motives in college drinkers: Mediating effects on the relationship between generalized anxiety and heavy drinking in negative-affect situations. Addictive Behaviors. 2009;34:505–513. doi: 10.1016/j.addbeh.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, Reynolds B, Skewes MC. Role of impulsivity in the relationship between depression and alcohol problems among emerging adult college drinkers. Experimental and Clinical Psychopharmacololgy. 2011;19:303–313. doi: 10.1037/a0022720. [DOI] [PubMed] [Google Scholar]
- Gruskin E, Byrne K, Kools S, Altschuler A. Consequence of frequenting the lesbian bar. Women & Health. 2007;44:103–120. doi: 10.1300/J013v44n02_06. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin. 2009;135:707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. Structural stigma and the health of lesbian, gay, and bisexual populations. Current Directions in Psychological Science. 2014;23:127–132. doi: 10.1177/0963721414523775. [DOI] [Google Scholar]
- Hatzenbuehler ML, Flores AL, Gates GJ. Social attitudes regarding same-sex marriage and LGBT health disparities: Results from a national probability sample. Journal of Social Issues (in press) [Google Scholar]
- Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Social Science & Medicine. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, Dovidio J. How does stigma “get under the skin”?: The mediating role of emotion regulation. Psychological Science. 2009;20:1282–1289. doi: 10.1111/j.1467-9280.2009.02441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103:813–821. doi: 10.2105/Ajph.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawthorne G. Measuring social isolation in older adults: Development and initial validation of the friendship scale. Social Indicators Research. 2006;77:521–548. [Google Scholar]
- HealthyPeople.gov. Lesbian, gay, bisexual, and transgender health. n.d. Retreived from: http://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health/objectives.
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Juth V, Smyth JM, Carey MP, Lepore SJ. Social constraints are associated with negative psychological and physical adjustment in bereavement. Applied Psychology Health And Well-Being. 2015 doi: 10.1111/aphw.12041. [DOI] [PubMed] [Google Scholar]
- Keough MT, O’Connor RM, Sherry SB, Stewart SH. Context counts: Solitary drinking explains the association between depressive symptoms and alcohol-related problems in undergraduates. Addictive Behavior. 2015;42:216–221. doi: 10.1016/j.addbeh.2014.11.031. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1995;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Lehavot K, Simoni JM. The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology. 2011;79:159–170. doi: 10.1037/a0022839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepore SJ. A social–cognitive processing model of emotional adjustment to cancer. In: Baum A, Anderson BL, editors. Psychosocial interventions for cancer. Washington, DC: American Psychological Association; 2001. pp. 99–116. [Google Scholar]
- Lepore SJ, Silver RC, Wortman CB, Wayment HA. Social constraints, intrusive thoughts, and depressive symptoms among bereaved mothers. Journal of Personality and Social Psychology. 1996;70:271–282. doi: 10.1037/0022-3514.70.2.271. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Hove MC, Whiteside U, Lee CM, Kirkeby BS, Oster-Aaland L, Larimer ME. Fitting in and feeling fine: Conformity and coping motives as mediators of the relationship between social anxiety and problematic drinking. Psychology of Addictive Behaviors. 2008;22:58–67. doi: 10.1037/0893-164X.22.1.58. [DOI] [PubMed] [Google Scholar]
- Lewis RJ, Derlega VJ, Clarke EG, Kuang JC. Stigma consciousness, social constraints, and lesbian well-being. Journal of Counseling Psychology. 2006;53:48–56. doi: 10.1037/0022-0167.53.1.48. [DOI] [Google Scholar]
- Lewis RJ, Mason TB, Winstead BA, Gaskins M, Irons LB. Pathways to hazardous drinking among racially and socioeconomically diverse lesbian women. Psychology of Women Quarterly. 2016;40:584–581. doi: 10.1177/0361684316662603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis RJ, Milletich RJ, Mason TB, Derlega VJ. Pathways connecting sexual minority stressors and psychological distress among lesbian women. Journal of Gay & Lesbian Social Services. 2014;26:147–167. doi: 10.1080/10538720.2014.891452. [DOI] [Google Scholar]
- Mason TB, Lewis RJ. Minority stress and binge eating among lesbian and bisexual women. Journal of Homosexuality. 2015;62:971–992. doi: 10.1080/00918369.2015.1008285. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ. Sexual orientation, substance use behaviors and substance dependence in the united states. Addiction. 2009;104:1333–1345. doi: 10.1111/j.1360-0443.2009.02596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the united states. American Journal of Public Health. 2010;100:1946–1952. doi: 10.2105/ajph.2009.163147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Wardell JD, Read JP. Drinking motives in the prospective prediction of unique alcohol-related consequences in college students. Journal of Studies on Alcohol and Drugs. 2014;75:93–102. doi: 10.15288/jsad.2014.75.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Test manual. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism (NIAAA); 1995. The drinker inventory of consequences (drinc): An instrument for assessing adverse consequences of alcohol abuse; pp. 95–3911. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- National Institute for Alcohol Abuse and Alcoholism [NIAAA] What’s low risk drinking? n.d. Retrived from https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-Your-Drinking-Pattern-Risky/Whats-Low-Risk-Drinking.aspx.
- Pinel EC. Stigma consciousness: The psychological legacy of social stereotypes. Journal of Personality and Social Psychology. 1999;76:114–128. doi: 10.1037/0022-3514.76.1.114. [DOI] [PubMed] [Google Scholar]
- Roos CR, Pearson MR, Brown DB. Drinking motives mediate the negative associations between mindfulness facets and alcohol outcomes among college students. Psychology of Addictive Behaviors. 2015;29:176–183. doi: 10.1037/a0038529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences. 2001;31:157–171. doi: 10.1016/S0191-8869(00)002130. [DOI] [Google Scholar]
- Talley AE, Littlefield AK. Pathways between concealable stigmatized identities and substance misuse. Social & Personality Psychology Compass. 2014;8:569–582. doi: 10.1111/spc3.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley AE, Sher KJ, Steinley D, Wood PK, Littlefield AK. Patterns of alcohol use and consequences among empirically derived sexual minority subgroups. Journal of Studies on Alcohol & Drugs. 2012;73:290–302. doi: 10.15288/jsad.2012.73.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trocki KF, Drabble L, Midanik L. Use of heavier drinking contexts among heterosexual, homosexuals and bisexuals: Results from a nation household probability survey. Journal of Studies of Alcohol. 2005;66:105–110. doi: 10.15288/jsa.2005.66.105. [DOI] [PubMed] [Google Scholar]
- World Health Organization [WHO] Global Status Report on Alcohol 2004. Geneva: World Health Organization, Department of Mental Health and Substance Abuse; 2004. Retrieved from: http://www.who.int/substance_abuse/publications/globalstatusreportalcohol2004_healtheffects.pdf. [Google Scholar]
- Williams SL, Mann AK. Sexual and gender minority health disparities as a social issue: How stigma and intergroup relations can explain and reduce health disparities. Journal of Social Issues (in press) [Google Scholar]
- Williams SL, Mann AK, Fredrick EG. Proximal minority stress, psychosocial resources and health among sexual minorities. Journal of Social Issues (in press) [Google Scholar]
- Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, Lima VD. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7:e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]


