Abstract
Background:
Individuals with multiple sclerosis (MS) face a range of barriers to accessing and using health-care services. The aim of this review was to identify specific barriers to accessing and using health-care services based on a continuum of the health-care delivery system.
Methods:
Literature searches were conducted in the PubMed, PsycINFO, CINAHL, and Web of Science databases. The following terms were searched as subject headings, key words, or abstracts: health care, access, barriers, physical disability, and multiple sclerosis. The literature search produced 361 potentially relevant citations. After screening titles, abstracts, and citations, eight citations were selected for full-text review.
Results:
Health-care barriers were divided into three continuous phases of receiving health care. In the before-visit phase, the most commonly identified barrier was transportation. In the during-visit phase, communication quality was the major concern. In the after-visit phase, discontinued referral was the major barrier encountered.
Conclusions:
There are multiple interrelated barriers to accessing and using health-care services along the health-care delivery continuum for people with MS and its associated physical disabilities, ranging from complex and long-recognized barriers that will likely require extended advocacy to create policy changes to issues that can and should be addressed through relatively minor changes in health-care delivery practices, improved care coordination, and increased provider awareness, education, and responsiveness to patients' needs.
Multiple sclerosis (MS) is the second most common neurologic disorder leading to disability in young adults, exceeded only by trauma.1 With a prevalence rate between 10 and 216 per 100,000 people,2 there are approximately 450,000 individuals with MS in the United States and 2.5 million worldwide, and most were diagnosed between the ages of 20 and 50 years.3,4 MS is a chronic, debilitating, immune-mediated disease affecting the central nervous system.5 MS symptoms are associated with motor and cognitive impairments and emotional changes. Common symptoms include fatigue, pain, numbness and tingling, weakness, muscle stiffness or spasms, tremors, bladder and bowel dysfunction, visual problems, cognitive dysfunction, emotional changes, depression, slurring speech, difficulty walking and problems with balance, and difficulties tolerating heat.6 These impairments can create further physical, mental, and social disabilities that threaten quality of life7 and increase limitations in community participation in such areas as working, learning, socializing, and nurturing. For MS symptom management and disability rehabilitation, people with MS generally require comprehensive lifelong health care to support and maintain their health, social function, and well-being across the life span.
MS is one of the most costly neurologic diseases.8 Individuals with MS pay twice the out-of-pocket health-care expenditures of the general population.9 Among direct all-cause medical costs for chronic conditions, MS has the second highest cost, after congestive heart failure.10 In the United States, all-cause health-care costs for an individual with MS, including direct and indirect costs, range from $8528 to $54,244 per year.10 On average, direct and indirect costs constitute 77% and 23% of total costs, respectively. Such costs do not include those related to disability and early retirement.10 However, individuals with MS do not receive equally corresponding health-care services. In a population-based study, which included 2156 people with MS who are representative of the MS population in the United States, Minden et al.9 analyzed access to health care. Although only 3.8% (approximately 7000 US citizens with MS) did not have health insurance, 17.5% of insured participants reported that their plans did not cover prescription medication, 9.5% found it somewhat or very difficult to obtain a referral to a specialist, and 53.4% and 40.5% could not choose any physician or hospital they wanted, respectively.9 Furthermore, 10.5% of insured participants had difficulty obtaining prescription medication, 4.1% had obstacles accessing medical care, and 2.4% could not obtain mental health services. This population-based survey showed that there is a need to systematically review the barriers to access and use of extended health care in individuals with MS.
In addition, in a recent analysis of 8983 individuals with MS, approximately 77.1% had one or more physical and mental comorbidities, such as hyperlipidemia, hypertension, depression, and anxiety.11 Comorbidities worsen MS symptoms and progression.11 These secondary health conditions and their associated increased disability require multiple health-care services, which are needed across the life span. However, health-care systems and patient education do not currently address the range of concurrent health and psychosocial issues related to MS and comorbidities sufficiently or effectively.12 Limited health care leads to negative effects on social (eg, social roles and participation), psychological (eg, depression, frustration, and stress), physical (eg, health deterioration), economic (eg, absence from work, additional health expenditures), and independence (eg, increased dependency on others) issues.
It is important to recognize and address barriers encountered by individuals with MS during the process of health-care delivery to constantly improve quality and outcomes. The fact that people with MS encounter numerous physical, programmatic, and social barriers to accessing health care has been well established.9–15 These barriers create and contribute to health disparities, which further exacerbate illness and disability. Learning about patients' experiences and perceptions of health care throughout the health-care continuum is an important step in improving person-centered health-care service delivery systems and promoting the health of individuals with MS.16 In the present literature review, we contribute to this process by detailing specific barriers to accessing and using health-care services reported by people with MS across the continuum of the health-care delivery system.
Methods
Search Strategy
We searched the following databases: PubMed, PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Web of Science. The search was updated periodically between November 2014 and February 2016. We used the following search terms in subject headings, abstracts, and key words: health care, access, barriers, physical disability, and multiple sclerosis. We applied the Boolean operator “OR.” We used the search term physical disability because the primary and early disability of MS is physical disability. We searched all available years for the databases.
Selection Criteria
In addition to meeting the search criteria, the selection criteria included that studies must concern health-care use in the United States, be written in English, and be published in peer-reviewed journals. In addition, we focused this review on access and continuous-use barriers in the health-care delivery process from adult patients' perspectives rather than from health-care providers' perspectives. If the studies did not clearly report the diagnoses of participants, the studies had to report the physical disability situations of participants. If the reported disability conditions could be experienced by people with MS, we included the studies for further review. Furthermore, the study participants had to have provided detailed and concrete experiences with barriers to accessing health-care services or to using health-care services after visiting a health-care provider in a clinic. Therefore, if only general barriers were reported without an interview to inquire about detailed experiences (such as noting only geographic distance, financial constraints, and inadequate care without detailed interpretations with the specific details of such barriers), the study was excluded. We did not include other publication types, such as abstracts, review articles, conference presentations, editorials, book chapters, or dissertations. The initial search and the citation search identified 361 citations. Two of us (C.C. and M.B.) independently assessed eligibility and specificity by reviewing titles, abstracts, and results. When there were discrepancies on selected citations, the authors jointly reviewed the articles against the selection criteria to reach a consensus.
Results
Study Selection and Characteristics
We agreed on eight studies that provided specific barriers to access to and use of health-care services. We reviewed the full text of these eight citations and elected to exclude one study involving 9643 veterans with MS17 because the study did not use interviews to inquire about specific barriers. Of the seven remaining studies,9,18–23 four used focus group interviews, two used telephone interviews and surveys, and one used a survey with questions generated from a focus group interview. Five studies clearly recruited participants with MS. Two studies included participants with MS-related physical disabilities. In the reviewed studies, participants had used a broad range of health-care services, including primary-care physicians, specialists, rehabilitation services, and mental health services. The present review also included specific barriers related to medical equipment.18
Barriers in Health-Care Delivery Process
We divided health-care barriers into three phases of the health-care continuum, namely, before, during, and after the clinical visit. In the following paragraphs we present the findings according to these phases.
Before Health-Care Visit
In the before-visit phase, common and lasting barriers included the limits experienced in, and complications associated with, dealing with health-care systems. These barriers included not being eligible for some health-care services or plan changes, limits in quantity or quality by a health plan benefit package, rejection of insurance coverage, long waiting times for health plan approval, not being covered for functional maintenance and/or mental health services (eg, psychotherapy sessions), and limited sessions for rehabilitation.9,19,20 These initial barriers may trigger the subsequent hurdle of not being able to make an appointment as the patient's needs dictate. In addition, individuals with MS found that the office hours were too short or limited for making an appointment, and they frequently found telephone contact difficult.19,21 Other difficulties in making an appointment included being declined or delayed without continuous assistance, being unable to be referred, and lack of available appointments in a short period, especially when patients needed to accommodate the time of a person or service that offers them physical assistance (eg, transportation, mobility or transfer/support, pushing a wheelchair, reading instructions) during a health-care provider visit.9,19–21
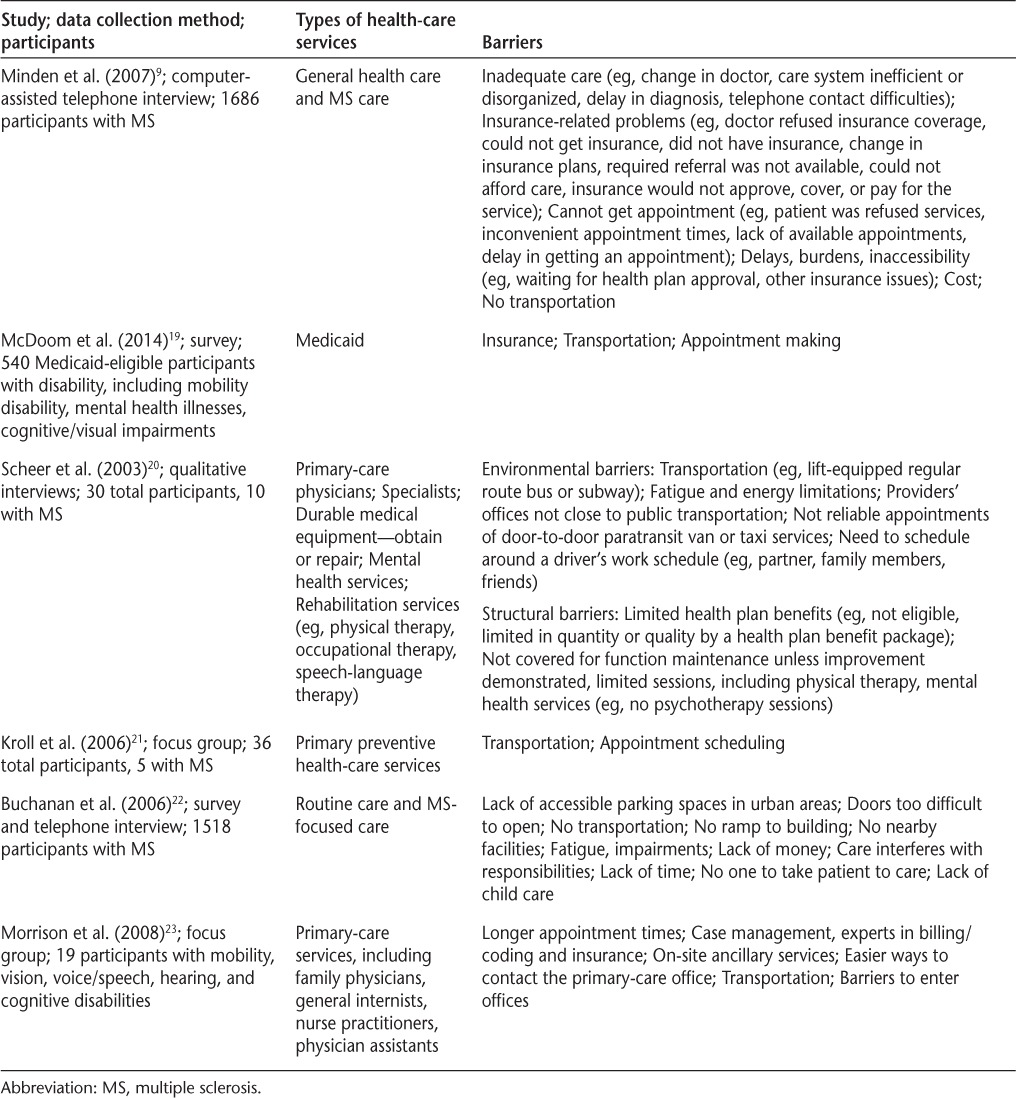
Geographic distance and transportation were frequently identified barriers. The reviewed studies suggested that long distances from health-care service facilities and living in a rural area are still problematic for many patients in terms of health-care accessibility.22 In addition, many individuals reported that fatigue makes long-distance travel a challenge.20,22 Moreover, door-to-door paratransit transportation service is neither reliable nor sufficient, and lifting equipment is not standard for all transportation services.9,19–21,23 A shortage of transportation assistance results in the need to ask family members or friends to provide a ride. In this latter scenario, individuals need to schedule their appointment around a driver's available time, increasing the likelihood of delaying visits to health-care providers and creating additional challenges in making an appointment.20,22 A related issue involves making health-care appointments during the patient's or driver's family or working hours.20,22 For example, if no one is available to help take care of their children, other family care/responsibilities, or work duties, individuals with MS, especially women with MS, may end up not visiting health-care providers (Table 1).
Table 1.
A summary of barriers to access and utilization of health-care services: the before-visit phase
During Health-Care Visit
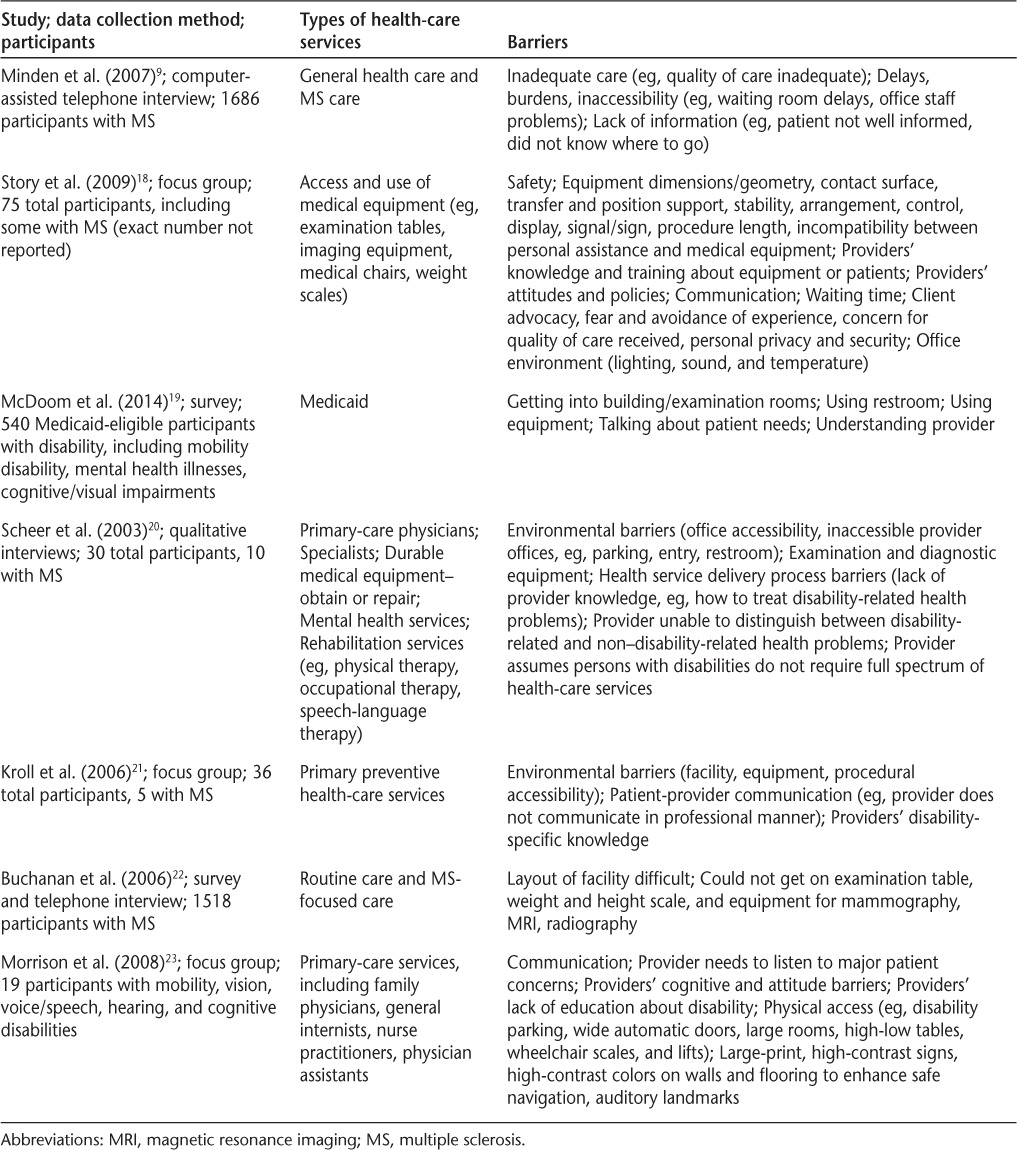
When individuals with MS arrive at health-care appointments, they frequently report encountering accessibility barriers in the physical environment, such as a shortage or absence of accessible parking spots, no ramp to the building, hard-to-open doors, and no space for a wheelchair user moving around in an office (eg, hallway, restroom).19–23 There is often incompatibility between the patients and the medical equipment. For example, patients with MS may be unable to get on the examination table, weight and height scale, and equipment for mammography, magnetic resonance imaging, and radiography.18–23 In addition, there is a lack of transfer and position support.18,23 Assistance for visual impairments (eg, large-print, high-contrast signs and auditory landmarks) is often overlooked.18,23
When individuals with MS communicated with health-care providers, they felt that the health-care providers were hurried and not listening to their needs.9,19,21,23 Patients reported being concerned about the education, knowledge, and attitude of health-care providers who are caring for people with disabilities. For example, health-care providers were seen as having a lack of knowledge about disability, disability-related, or non–disability-specific health problems.18,20,21,23 In attending to a focal condition only, rather than treating a patient as a whole person, health-care providers may neglect health-care needs that are prioritized by patients or unintentionally miss cues for addressing other care needs, such as those related to productivity or sexuality. An additional communication discrepancy between patients and health-care providers, with implications for professional ethics, was that patients expressed worries about their advocacy, privacy, and security while receiving health care (Table 2).9,18
Table 2.
A summary of barriers to access and utilization of health-care services: the during-visit phase
After Health-Care Visit
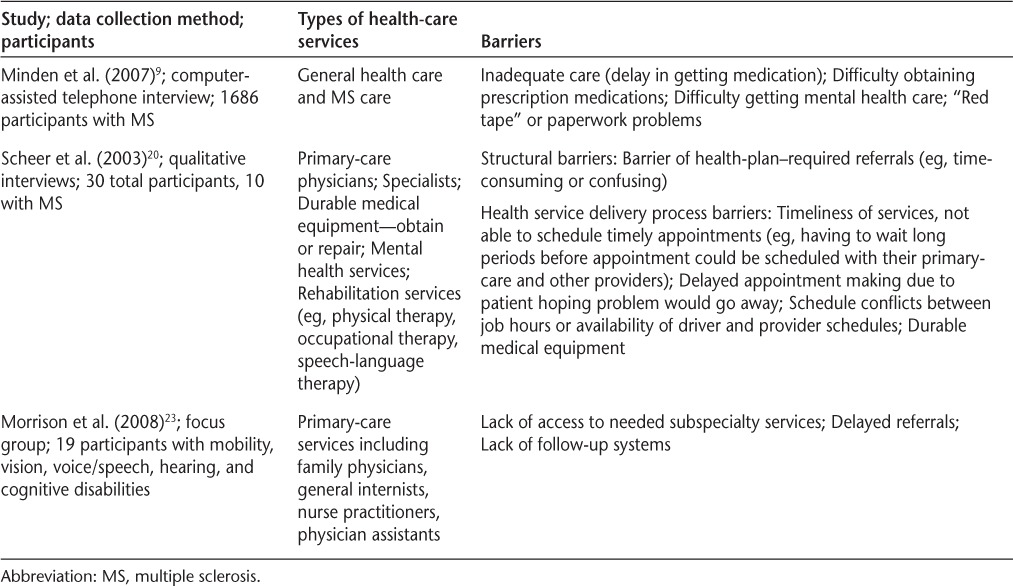
After visiting their health-care providers, patients reported barriers in connecting to referral appointments for further health-care needs.9,20,23 These referrals can be confusing and time-consuming, especially for subspecialty services.23 Such referral barriers may be due to a lack of a follow-up system.23 In addition, the previously identified barriers to making an appointment in the before-visit phase were also reported to be related to this phase. Patients also reported having difficulties in getting medications or reading the instructions on the labels (Table 3).9
Table 3.
A summary of barriers to access and utilization of health-care services: the after-visit phase
Discussion
Although there is a fairly large body of research exploring the health-care priorities, preferences, and experiences of general health-care consumers, the number of studies specific to patients with MS is considerably limited. The existing research on health-care–related needs and satisfaction in people with MS is characterized by several limitations. First, this research is generally based on relatively small and localized samples. Second, needs assessments are often very broad in scope, incorporating a wide range of psychosocial and environmental domains and, therefore, having limited health-care–specific content. Third, studies that do evaluate the health-care needs and experiences of people with MS are frequently based on frameworks established by researchers and health-care professionals and are, thus, limited in their capacity to identify the consumer's perspective.13–15,24–26 The present review focused explicitly on studies that incorporated the patient's perceptions about their health care and, specifically, on studies in which detailed interview-based information was provided. The review framework, based on three temporal phases of health care, provided a person-centered perspective on barriers to access and utilization of health-care services.
Barriers during the period before the health-care visit were grouped in terms of health insurance barriers, including primarily issues with eligibility for health insurance coverage and coverage for adjunct or subspecialty services; scheduling barriers, related to limited appointment times, difficulty scheduling by telephone, co-scheduling with support persons and services, and arranging child or family care; and transportation-related barriers, including geographic distance from health-care facilities and inaccessible paratransit transportation. Barriers identified during the health-care visit included accessibility barriers in the physical environment and issues associated with the interaction with health-care providers related to communication, knowledge of and attention to nonfocal health issues, and concerns about privacy and security. In the period after the health-care visit, the primary barriers were related to follow-up and referrals and issues related to obtaining and adhering to medications. The following discussion addresses implications and recommendations in the context of these phases.
Characteristics of effective health-care plans include affordable health insurance with coverage for all necessary services, a usual source of care, access to specialty care as needed, choice of providers, an absence of physical access barriers, and feeling respected, informed, and well cared for.9 However, in the present review we found that these characteristics are frequently absent in the health-care delivery system for individuals with MS. The nondiscrimination provisions of the Patient Protection and Affordable Care Act (Public Law 111-148) are designed to enable people with disabilities and preexisting conditions to access private health insurance in addition to public health insurance, which limits choices of health-care providers. However, both health-care providers and consumers need comprehensive knowledge about what health services are covered and operated by the new policy.
Although the Americans with Disabilities Act of 1990 (ADA) established requirements for health-care facilities to be free of physical and environmental barriers for individuals living with disabilities, these remain the most commonly identified barriers in the present review. To address these physical barriers, health-care providers may benefit from further education and training on these requirements and on applying the 2010 ADA Standards for Accessible Design. The New Construction and Alterations section of the ADA specifies the standards for medical care facilities, in addition to indoor and outdoor environments.
Patients often reported delays in accessing and receiving needed health care and follow-up services, contributing to worsening health outcomes. To address these issues, health-care providers may need to consider implementing more flexible service hours, educating staff, and implementing processes to be more responsive to patient needs. Pritchard et al.27 recently noted that access to high-quality care can be improved through staff knowledge of the clinical population and specific patient needs, including awareness of patients who require extra time for appointments and scheduling accordingly and developing a method of tracking or documenting patients' special needs.27 Although financial and practical considerations may not allow for child and family care in many health-care facilities, the peer-navigator approach may be used to work with patients to explore their health-care service needs and assist with planning for child care and transportation issues.
Access to, and insurance coverage for, extended rehabilitation and subspecialty services are legitimately needed by individuals with MS due to the chronic and progressive nature of the condition. The frequency with which barriers to access and coverage were identified in this and previous research suggests the need for advocacy for health insurance policy revision. However, providing individuals in the early stages of MS with self-management counseling and increased provider attention to wellness have been identified as an intermediate solution.28
Individuals with MS often need multiple specialty-care services and often receive numerous subspecialty or allied health referrals, including for radiology; occupational, physical, speech, and vocational therapies; nutrition; and pain specialists. However, delayed or discontinued referrals are not uncommon for individuals with MS.9,17,20,23 Furthermore, as was identified in the present review, primary-care providers often address only one focal condition rather than taking a comprehensive view, including consideration of comorbid conditions and secondary health problems. A care coordination service by a professional specialized in disability and life span care is a critical component of care for many patients with MS. A professional case manager or life span coach specialized in disability can integrate a client's needed health-care services and health-care coverage across an individual's life stages.23 Some individuals with MS have also suggested that independent living centers and rehabilitation facilities could be used as a “one-stop shop” for integrating all health-care needs for treating MS and MS-related disabilities.21
Brief and hurried interactions with health-care providers are commonly reported by individuals with MS.29 Individuals with MS have recommended that health professional training can better prepare providers to adequately meet the needs of patients by strengthening listening and communication skills with individuals with disabilities. Brandes et al.30 found three kinds of communication barriers between health-care providers and patients with chronic disease. The first kind of barrier is related to the provider's behavior, such as not responding with empathy when patients express a concern, not explicitly inviting patients to discuss their concerns, and not facilitating interactions where patients feel they are stupid when expressing their concerns.30 The second kind of barrier is related to the provider's environment, such as not having enough time to listen to patients' concerns; not paying attention to patients and instead constantly looking at his or her computer screen; and patients being unable to choose a provider.30 The third kind of barrier affects the patient's attitude and empowerment: for example, patients being afraid they are wasting their provider's time when they express their concerns, patients feeling ashamed when they express their concerns, and patients being afraid that expressing their concerns will damage their relationship with their provider.30 The provider's paternalistic or patronizing attitude along with a medical-model practice will insult, segmentalize, and reduce the consumer's choice.31
Finally, transportation barriers have proved to be perhaps the most intransigent and irresolvable health-care barrier for many health-care consumers, and particularly those with the most significant mobility and health issues, including many patients with MS. According to Syed et al.,32 as many as 67% of patients have reported that transportation barriers affect health-care access across a range of studies. When patients cannot get to health-care appointments, they miss the opportunity for evaluation and treatment and changes in treatment regimens and are at increased risk for delayed interventions that may reduce or prevent complications.32 Beyond longer-term solutions, including better collaboration between policy makers, urban planners, and advocates, shorter-term solutions include reimbursement for travel, home medication delivery, and home visits by providers.32 Individuals with MS have benefited from telecare,33 or the use of telecommunications to provide health-care services in an individual's residence or an accessible alternative facility.33
Conclusion
The Institute of Medicine has defined high-quality health care as the provision of appropriate services in a technically competent manner and as including good communication, shared decision making, and consistency with patient values and preferences.34 Optimizing the structure, processes, and interactions between health-care providers and patients is crucial to achieving high-quality care.35 Access to and active participation in health care are directly and inherently linked to health outcomes, making the awareness and understanding of health-care barriers for people with MS a critical area of focus. In the present study, we summarized key barriers as identified and explicated by patients with MS. Although many of these barriers may ultimately require sustained advocacy before needed policy changes are implemented, others are more amenable to redress through increased health-care provider awareness of and responsiveness to patients' needs.
PracticePoints
Learning about patients' experiences and perceptions of health care throughout the health-care continuum is an important step in improving person-centered health-care service delivery systems and promoting the health of people with MS.
Health-care barriers were identified across three phases of health care, including the before-visit phase, where the major barrier was transportation; the during-visit phase, in which communication quality was the major concern; and the after-visit phase, wherein continuity of care and referrals were the major barriers.
Clinicians can help reduce barriers to access and continuity in MS health care by ensuring the accessibility of the physical health-care environment and becoming familiar with legislation and guidelines concerning accessibility for patients with disabilities, attending to patients' needs through effective listening and communication skills, and ensuring that staff are aware of patients' needs for scheduling, transportation, and mobility assistance. Clinicians are encouraged to view patients' health comprehensively and attend to co-occuring conditions and secondary health concerns and to ensure care coordination for patients with MS who require multiple specialty-care services. Finally, clinicians should explore creative individualized solutions with patients who face transportation barriers to care, including reimbursement for travel, home medication delivery, and home-based health-care options.
Financial Disclosures
The authors have no conflicts of interest to disclose.
Funding/Support
This study was supported by the Health Care Delivery and Policy Research program (contract HC 0168) from the National Multiple Sclerosis Society.
References
- 1. National Institute of Neurological Disorders and Stroke. . Multiple sclerosis information page. https://www.ninds.nih.gov/Disorders/All-Disorders/Multiple-Sclerosis-Information-Page. Accessed September 23, 2017.
- 2. World Health Organization. . Atlas: Multiple Sclerosis Resources in the World. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 3. Compston A, Coles A.. Multiple sclerosis. Lancet. 2002; 359: 1221– 1231. [DOI] [PubMed] [Google Scholar]
- 4. National Multiple Sclerosis Society. . What is MS? http://www.nationalmssociety.org/What-is-MS. Accessed February 25, 2016.
- 5. National Multiple Sclerosis Society. . What is an immune-mediated disease? http://www.nationalmssociety.org/What-is-MS/Definition-of-MS/Immune-mediated-disease#section-0. Accessed February 25, 2016.
- 6. Compston A, Coles A.. Multiple sclerosis. Lancet. 2008; 372: 25– 31. [DOI] [PubMed] [Google Scholar]
- 7. Mitchell AJ, Benito-Leon J, Gonzalez JMM, . et al. Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of well-being. Lancet Neurol. 2005; 4: 556– 566. [DOI] [PubMed] [Google Scholar]
- 8. Gustavsson A, Svensson M, Jacobi F, . et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011; 21: 718– 779. [DOI] [PubMed] [Google Scholar]
- 9. Minden SL, Frankel D, Hadden L, . et al. Access to health care for people with multiple sclerosis. Mult Scler. 2007; 13: 547– 558. [DOI] [PubMed] [Google Scholar]
- 10. Adelman G, Rane SG, Villa KF.. The cost burden of multiple sclerosis in the United States: a systematic review of the literature. J Med Econ. 2013; 16: 639– 647. [DOI] [PubMed] [Google Scholar]
- 11. Marrie RA, Hanwell H.. General health issues in multiple sclerosis: comorbidities, secondary conditions, and health behaviors. Continuum (Minneap Minn). 2013; 19: 1046– 1057. [DOI] [PubMed] [Google Scholar]
- 12. Barnett K, Mercer SW, Norbury M, . et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012; 380: 37– 43. [DOI] [PubMed] [Google Scholar]
- 13. Forbes A, While A, Taylor M.. What people with multiple sclerosis perceive to be important to meeting their needs. J Adv Nurs. 2007; 58: 11– 22. [DOI] [PubMed] [Google Scholar]
- 14. Defriez M, Griffiths D, Millett C, . et al. The perception of the current provision of care for multiple sclerosis sufferers in the community. Prim Health Care Res Dev. 2003; 4: 233– 243. [Google Scholar]
- 15. Freeman A, Thompson AJ.. Community services in multiple sclerosis: still a matter of chance. J Neurol Neurosurg Psychiatry. 2000; 69: 728– 732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Institute of Medicine, Committee on Quality of Health Care in America. . Crossing the Quality Chasm. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 17. Turner AP, Chapko MK, Yanez D, . et al. Access to multiple sclerosis specialty care. PM R. 2013; 5: 1044– 1050. [DOI] [PubMed] [Google Scholar]
- 18. Story MF, Schwier E, Kailes JI.. Perspectives of patients with disabilities on the accessibility of medical equipment: examination tables, imaging equipment, medical chairs, and weight scales. Disabil Health J. 2009; 2: 169– 179. [DOI] [PubMed] [Google Scholar]
- 19. McDoom MM, Koppelman E, Drainoni ML.. Barriers to accessible health care for Medicaid eligible people with disabilities: a comparative analysis. J Disabil Policy Stud. 2014; 25: 154– 163. [Google Scholar]
- 20. Scheer JM, Kroll T, Neri MT, . et al. Access barriers for persons with disabilities: the consumer's perspective. J Disabil Policy Stud. 2003; 14: 221– 230. [Google Scholar]
- 21. Kroll T, Jones GC, Kehn M, . et al. Barriers and strategies affecting the utilisation of primary preventive services for people with physical disabilities: a qualitative inquiry. Health Soc Care Community. 2006; 14: 284– 293. [DOI] [PubMed] [Google Scholar]
- 22. Buchanan RJ, Stuifbergen A, Chakravorty BJ, . et al. Urban/rural differences in access and barriers to health care for people with multiple sclerosis. J Health Hum Serv Adm. 2006; 29: 360– 375. [PubMed] [Google Scholar]
- 23. Morrison EH, George V, Mosqueda L.. Primary care for adults with physical disabilities: perceptions from consumer and provider focus groups. Fam Med. 2008; 40: 645– 651. [PubMed] [Google Scholar]
- 24. Gottberg K, Einarsson U, Ytterberg C, . et al. Use of health care services and satisfaction with care in people with multiple sclerosis in Stockholm County: a population-based study. Mult Scler. 2008; 14: 962– 971. [DOI] [PubMed] [Google Scholar]
- 25. MS Society. . Measuring Up: Experiences of Health Services of People with MS. London, UK: MS Society; 2003. [Google Scholar]
- 26. Somerset M, Campbell R, Sharp DJ, . et al. What do people with MS want and expect from health-care services? Health Expect. 2001; 4: 29– 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pritchard S, Milligan J, Lee J.. Making your office accessible for patients with mobility impairments. Can Fam Physician. 2014; 60: 253– 254. [PMC free article] [PubMed] [Google Scholar]
- 28. Bandura A. The primacy of self-regulation in health promotion. Appl Psychol. 2005; 54: 245– 254. [Google Scholar]
- 29. World Health Organization. . Disability and Health: Fact Sheet No. 352. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 30. Brandes K, Linn AJ, Smit EG, . et al. Patients' reports of barriers to expressing concerns during cancer consultations. Patient Educ Couns. 2015; 98: 317– 322. [DOI] [PubMed] [Google Scholar]
- 31. Yee S, Breslin ML.. Achieving accessible health care for people with disabilities: why the ADA is only part of the solution. Disabil Health J. 2010; 3: 253– 261. [DOI] [PubMed] [Google Scholar]
- 32. Syed ST, Gerber BS, Sharp LK.. Traveling towards disease: transportation barriers to health care access. J Commun Health. 2013; 38: 976– 993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zissman K, Lejbkowicz I, Miller A.. Telemedicine for multiple sclerosis patients: assessment using Health Value Compass. Mult Scler J. 2012; 18: 472– 480. [DOI] [PubMed] [Google Scholar]
- 34. Institute of Medicine. . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 35. Tzelepis F, Rose SK, Sanson-Fisher RW, . et al. Are we missing the Institute of Medicine's mark? a systematic review of patient-reported outcome measures assessing quality of patient-centered cancer care. BMC Cancer. 2014; 14: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]


