Abstract
Cardiomyopathies might lead to end-stage heart disease with the requirement of drastic treatments like bridging up to transplant or heart transplantation. A not precisely known proportion of these diseases are genetically determined. We genotyped 43 index-patients (30 DCM, 10 ARVC, 3 RCM) with advanced or end stage cardiomyopathy using a gene panel which covered 46 known cardiomyopathy disease genes. Fifty-three variants with possible impact on disease in 33 patients were identified. Of these 27 (51%) were classified as likely pathogenic or pathogenic in the MYH7, MYL2, MYL3, NEXN, TNNC1, TNNI3, DES, LMNA, PKP2, PLN, RBM20, TTN, and CRYAB genes. Fifty-six percent (n = 24) of index-patients carried a likely pathogenic or pathogenic mutation. Of these 75% (n = 18) were familial and 25% (n = 6) sporadic cases. However, severe cardiomyopathy seemed to be not characterized by a specific mutation profile. Remarkably, we identified a novel homozygous PKP2-missense variant in a large consanguineous family with sudden death in early childhood and several members with heart transplantation in adolescent age.
Introduction
Although multiple studies on genetics of cardiomyopathies [1–7] indicated a notable proportion of genetic cases, the genotyping of end-stage heart failure patients is not well established in clinical practice. The Human Gene Mutation Database (HGMD, [8]) lists 156 genes related to cardiomyopathies that can all necessitate heart transplantation (HTx) in the end-stage of the disease. The genes that are most commonly affected are desmosomal genes in case of arrhythmogenic right ventricular cardiomyopathy (ARVC) [9] and genes coding for components of the sarcomere, Z-disk, intercalated disk, cell membrane, ion channel, and nucleus in case of dilated cardiomyopathy (DCM), respectively [2, 4, 5, 7, 10]. Genotyping of patients evaluated for HTx, bridged to transplantation by ventricular assist device implantation (VAD) or already transplanted is still not routinely performed although this contributes to early family management [11]. Both HTx and VAD implantation may cause a considerable psychological burden for the patients and their relatives. Therefore, especially in these families a possible genetic cause of the disease is a pressing question. The knowledge of the disease-causing mutation supports the early identification of family members with asymptomatic disease or at risk for developing disease. An early patient management might prevent sudden cardiac death and might prevent or at least delay HTx or VAD implantation [11]. However, at present there are no specific guidelines available on how to treat genotype positive yet phenotype negative individuals.
The goal of this study was to evaluate whether genotyping of patients with end-stage cardiomyopathy might provide the chance to identify characteristic genes or mutations that are associated with the most severe course of this disease. Furthermore, we speculate that a notable proportion of sporadic cases are genetically determined. Therefore, we analysed 46 disease genes in 43 index-patients with end-stage cardiomyopathy by next generation sequencing (NGS). We found that the majority of DCM-cases (60%) and 40% of ARVC-cases were carriers of an at least likely pathogenic (class 4 or 5) mutation following the American College of Medical Genetics and Genomics (ACMG) guidelines for variant classification [12]. Of note, we identified a novel homozygous PKP2-gene mutation, which is associated with dilated cardiomyopathy.
Material and methods
Study population
We included patients with no-ischemic severe heart failure with need of HTx or mechanical circulatory support. We also included patients transferred to our center for the evaluation to list for HTx. A positive family history for cardiomyopathy or in case of presumed sporadic cases age at diagnosis ≤ 40 years were defined as additional study criteria. This led to the inclusion of 30 DCM (21 familial, 9 sporadic) and 3 RCM index-patients (1 familial, 2 sporadic). Additionally, for ARVC-cases an at least possible diagnosis of ARVC according the revised Task Force Criteria [13] and the modified criteria [14] in case of pediatric patients (ARVC-01 and ARVC-08) was a prerequisite. Ten ARVC index-patients (6 familial, 4 sporadic cases) met the criteria and were included in the study. Of these 4 patients had ARVC with left ventricular dilation and had been treated by HTx, and total artificial heart implantation, respectively. The remaining 6 cases were diagnosed with arrhythmias and right ventricle enlargement/failure. Four of them underwent HTx, two cases were evaluated for HTx and treated with an ICD. All patients (n = 43) were genotyped in 46 cardiomyopathy-associated genes (see below).
DCM and RCM were diagnosed according to established criteria [15, 16]. Clinical characteristics of the index-patients are summarised in Table 1, S1 and S2 Tables. All patients were of European/Caucasian origin. The written informed consent of all patients was obtained. In case of minors patient written informed consent of the parents were obtained. The study was approved by the local ethics committee (Ruhr University Bochum, Bad Oeynhausen, Germany, Reg.-No.27.1/2011). This study was complied with the Declaration of Helsinki.
Table 1. Clinical, familial and genetic data of 50 patients with advanced or end stage cardiomyopathy.
| Patient ID | Gender | Age at diagnosis (Years) |
Treatment | NYHA*/Task Force classification† | Age at HTxa/VADb | Family history‡ | Affected Genes (ACMG class) |
|---|---|---|---|---|---|---|---|
| DCM-01 | m | 1 | VAD, HTx | IV | 13a | Sporadic§ | MYH7 (4), MYL2 (4) |
| DCM-02 | m | 31 | pre HTxII | III | - | Sporadic | TTN (3) |
| DCM-03 | m | 68 | ICD, VAD | III | 69b | Son with DCM | TTN (4), DSC2 (2), TTN (3) |
| DCM-04 | m | 30 | HTx | IV | 62a | Mother (61y) died from DCM | TTN (4), DSP (3) |
| DCM-05 | m | 11 | HTx | IV | 14 | Older brother with DCM and HTx | TNNC1 (4), TNNC1 (3) |
| DCM-06 | m | < 1 | VAD, HTx | IV | <1a | Sporadic | TTN (3) |
| DCM-07 | m | 35 | ICD, VAD, HTx | IV | 47a | Cousin with HTx, sister with suspicion of DCM, father and brother died from heart disease, sister with heart disease | LMNA (5) |
| DCM-08 | m | 23 | VAD, HTx | IV | 23a | Father with DCM | TTN (3) |
| DCM-09 | f | 41 | ICD, AMB | II#,** | - | SCD of father (40y), brother died from heart disease (23y) | DES (5), TTN (3) |
| DCM-10 | m | 33 | ICD, HTX | IV | 37 | Mother and aunt with HTx, brother and niece with DCM | DSP (2) |
| DCM-11 | m | 36 | ICD, HTx | III-IV | 48a | Two cousins died from SCD | DES (4) |
| DCM-12 | m | 18 | ICD, VAD | III-IV | 29b | Sporadic | TTN (4), TNNT2 (3) |
| DCM-13 | m | 39 | pre HTxII | I#,** | - | Father with DCM and HTx | LMNA (4), TTN (4) |
| DCM-14 | m | 60 | ICD, HTx | III | 63a | Mother and two brothers died from heart disease, sister with DCM and HTx | RBM20 (4), DSP (3) |
| DCM-15 | m | 32 | HTx | III | 40a | Son with DCM and HTx, sister with DCM | RBM20 (5), TTN (3) |
| DCM-16 | f | 20 | ICD, VAD | III-IV | 32b | Sporadic | TTN (4), TTN (3) |
| DCM-17 | m | 14 | ICD,HTx | III | 59 | Father and paternal uncle with SCD | DES (5) |
| DCM-18 | f | n.a | ICD, HTx | IV | 52a | Monozygotic twin sister (45y) died from heart disease | LMNA (5) |
| DCM-19 | m | 5 | ICD, VAD | IV | 22b | Sporadic | NEXN (4), MYH7 (4) |
| DCM-20 | m | 35 | ICD, pre HTx | II-III | - | Father with DCM | TTN (4), DSP (3) |
| DCM-21 | f | n.a | ICD, pre HTx | II#,** | - | Father died from DCM, deceased brother with VAD, son and daughter with heart disease | TTN (3) |
| DCM-22 | f | 59 | pre HTxII | II#,** | - | Brother with HTx, another brother with VAD | TTN (4) |
| DCM-23 | f | n.a. | HTx | IV | 14a | SCD of 2 brothers in childhood, 2 siblings with DCM and HTx in adolescent age | PKP2 (4), LAMA4 (2) |
| DCM-24 | f | 30 | VAD | IV | 31b | Sporadic | TTN (3) |
| DCM-25 | m | 40 | ICD, pre HTx | II-III | - | SCD of 3 maternal uncles, son with DCM | Unknown |
| DCM-26 | f | n.a | HTx | IV | 16a | Sporadic | Unknown |
| DCM-27 | m | 38 | VAD, HTx | IV | 53a | Father died from DCM (43y), brother and sister with heart disease | Unknown |
| DCM-28 | m | 37 | ICD, VAD, HTx | IV | 52a | SCD of maternal grandmother (60y) | Unknown |
| DCM-29 | m | 31 | HTx | IV | 42a | Paternal grandfather (51y) and father (46y) deceased from heart disease | Unknown |
| DCM-30 | m | 36 | ICD, pre HTx | II** | - | Sporadic | Unknown |
| RCM-01 | f | 12 | VAD, HTx | IV | 13a | Sporadic | MYL3 (3) |
| RCM-02 | m | < 1 | VAD | IV | <1b | Sporadic | TNNI3 (4) |
| RCM-03 | m | 19 | HTx | IV | 12a | Mother (42y) with muscular dystrophy died from heart disease | CRYAB (5) |
| ARVC-01 | m | 14 | ICD | DD††** | Sporadic | PKP2 (5) | |
| ARVC-02 | m | 35 | ICD, HTx | DD | 36a | SCD of father, brother with heart disease | MYH7 (3) |
| ARVC-03 | m | 67 | ICD | PD | Sporadic | PRKAG2 (3) | |
| ARVC-04 | f | 35 | ICD, TAH | DD | 55b | SCD of maternal grandmother and uncle, sister with DCM | PLN (5), MYH6 (3), TTN (2) |
| ARVC-05 | f | 45 | ICD, HTx | DD | 47a | Maternal grandfather with SCD | LMNA (4), PKP2 (3) |
| ARVC-06 | f | 21 | ICD, HTx | DD | 32a | ARVC with SCD of father and brother | PKP2 (5), PKP2 (3), RYR2 (3), TTN (3) |
| ARVC-07 | m | 40 | ICD, HTx | BL | 62a | Paternal great-grandfather and father with heart disease and premature death | DES (3) |
| ARVC-08 | m | 16 | ICD, HTx | BL†† | 21a | Sporadic | Unknown |
| ARVC-09 | f | 42 | VAD | PD | 45b | Sporadic | Unknown |
| ARVC-10 | f | n.a | ICD, HTx | DD | 46a | Two maternal great-uncles with SCD | Unknown |
Abbreviations
a = age at HTx, ACMG class 2 = likely benign, ACMG class 3 = variant of uncertain significance, ACMG class 4 = likely pathogenic, ACMG class 5 = pathogenic, AMB = ambulatory, ARVC = arrhythmogenic right ventricular cardiomyopathy
b = age at VAD, DCM = dilated cardiomyopathy; f = female, FS = fractional shortening, HTx = heart transplantation, ICD = implantable cardioverter defibrillator, ID = identification, m = male, n.a. = not available, RCM = restrictive cardiomyopathy, SCD = sudden cardiac death, TAH = total artificial heart, VAD = ventricular assist device; y = year(s).
*New York Heart Association functional classification of heart failure before VAD or HTx, respectively.
†Classification according Task Force Criteria [13].
‡Familial disposition for cardiomyopathy due to pedigree analysis and anecdotal evidence.
§Sporadic = isolated cases without family history.
IITreated medically.
#Progressive cardiomyopathy with familial disposition due to pedigree analysis or anecdotal evidence, respectively.
**Not yet listed for HTx but in the long term surveillance program.
DNA analysis
DNA was isolated from white blood cells using standard techniques (High Pure PCR Template Preparation Kit®, Roche Diagnostics GmbH, Mannheim, Germany) and prepared for cardiac gene enrichment re-sequencing on a MiSeq® next generation sequencing system according to manufactures instructions (TruSight™ Rapid Capture Sample Preparation Kit). All patients were screened for variants in 46 cardiomyopathy genes using the TruSight™ Cardiomyopathy gene panel. The evidence linking these genes to cardiomyopathy has been published previously [17] (for gene list see S3 Table). Enrichment, sequencing kits and sequencing system were supplied by Illumina Inc, San Diego, CA, USA. For reads alignment and base calling Illumina´s automated work flow was used (BWA [18], GATK [19], and SAMtools [20]).
A minimum read depth of ≥ 20 reads was set as quality cut-off (quality data see S4 Table). For variant annotation the VariantStudio™ v2.1 software provided by Illumina Inc with the UCSC Genome Build hg19 as reference was used. We filtered variants located in exon- and consensus splice-sequences (± 1 and 2 position) with a global minor allele frequency (MAF) ≤0.0005 according to the data provided by the Exome Aggregation Consortium (Version 0.3, ExAC data and browser (beta) Version) [21]. Synonymous variants were not taken into account. Variants of interest were verified by Sanger sequencing (BigDye® Terminator v1.1 Cycle Sequencing Kit, ABI PRISM® 3100 genetic analyzer, Applied Biosystems, Foster City, CA, USA).
Variant classification
This study was primarily designed to identify dominant single gene mutations with clear clinical impact on ARVC or other cardiomyopathy subtypes. Therefore the guidelines [12] of the American College of Medical Genetics and Genomics (ACMG) were considered for variant classification. The ACMG defined five variant classes: class 5, pathogenic; class 4, likely pathogenic; class 3, variant of uncertain significance (VUS); class 2, likely benign; class 1, benign. For use on mainly private variants the criteria and rules for classification have been adjusted (for details see S1 Methods). The cut-off for the minor allele frequency (MAF) of variants of interest was set to a value ≤0.0005 and thus within the range of the respective disease prevalence (http://www.orpha.net) [22]. The ExAC browser [21] was used as reference for allele frequencies. Only frequencies of the non-Finnish European population were taken into account. Original reports listed in the Human Mutation Database Professional 2015.1 (HGMD®) [8] and the ARVC Genetic Variants Database [23, 24] were reviewed concerning variant classification. Deleterious effect of a variant was considered when ≥3 prediction tools forecasted the variant to be deleterious (MutPred [25], SNP&GO [26, 27], Fathmm [28], and PolyPhen-2 (Polymorphism Phenotyping v2, humVar) [29]). In case of the TTN-gene only variants affecting the cardiac titin isoforms N2B and/or N2BA were further investigated. In this manuscript only (likely) pathogenic gene variations are referred to as ‘mutation’ while (likely) benign variants, variants of uncertain significance and gene variations in a general context are called ‘variant’.
Gene and variant nomenclature
The nomenclature of sequence variants based on the rules of the Human Genome Variation Society (HGVS, www.hgvs.org). Nucleotide and amino acid numbering refers to the reference sequences given by the National Center of Biotechnology Information (NCBI, http://www.ncbi.nlm.nih.gov) (S3 Table). In case of TTN the nomenclature refers to the longest predicted isoform (NM_001267550.1, NP_001254479.1). All variations listed in this manuscript were submitted to ClinVar (http://www.ncbi.nlm.nih.gov/clinvar) using the submission name HDZNRW. An already existing listing of the study variants in the ClinVar database was checked. Some of them have been reported by others, a few with conflicting interpretation of pathogenicity. The listing of TTN variants was only partially verified because of inconsistent nomenclature based on different isoforms.
Results
Patient cohort
The study cohort comprised 43 unrelated index-patients (29 male, 14 female) with cardiomyopathy of different types (Fig 1). Of these, 33 patients presented with end-stage disease and already underwent implantation of VAD and/or HTx. Ten patients were evaluated for HTx due to clinical signs of advanced cardiomyopathy. Seventy-nine percent of DCM- and RCM-patients were in New York Heart Association (NYHA) classification III or IV (Table 1). Six ARVC-patients were classified with definite diagnosis (DD), 2 patients with possible (PD), and 2 patients with borderline diagnosis (BL) (Table 1). The mean age at diagnosis was not significantly different in DCM- (0031±17 years) and ARVC-cases (35±17 years) (S1 Fig). Due to the small number statistical evaluations for RCM-cases were not possible in this study (Table 1). Familial disposition for the cardiomyopathy due to pedigree analysis and anecdotal evidence was suspected in 21of 30 DCM, 6 of 10 ARVC and once in RCM (n = 3) cases (Table 1). Sporadic cardiomyopathy was suspected in 15 patients. Where available the pedigrees illustrating heart disease within the families and variant co-segregation/penetrance are shown in S2 Fig.
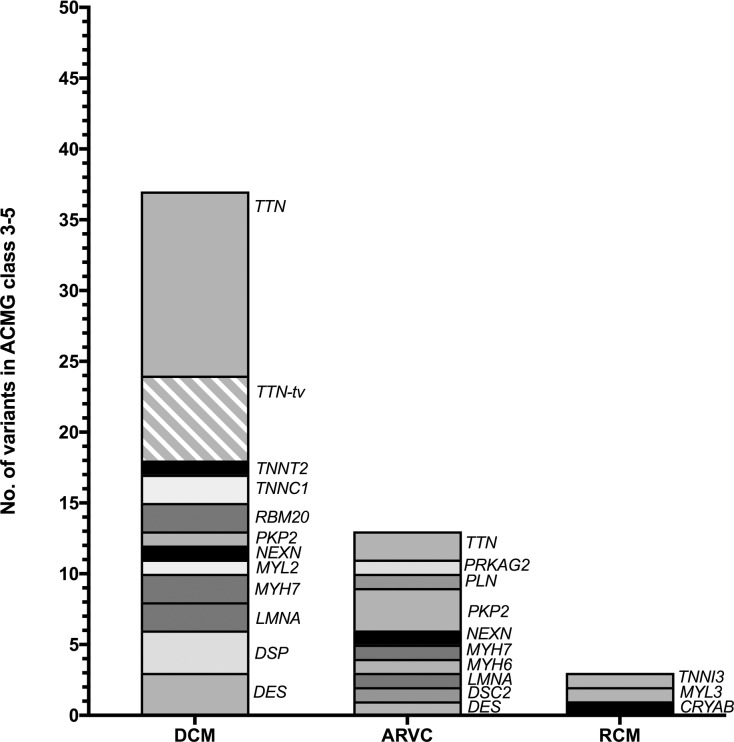
Fig 1. Variant carrying genes.
In DCM-cases TTN carried the most variants. Of 19 TTN-variants in DCM-cases, 6 were truncating variants. The other affected genes were TNNT2, TNNC1, RBM20, PKP2, NEXN, MYL2, MYH7, LMNA, DSP, and DES. In ARVC-cases predominantly PKP2- and TTN-variants were identified. Further variants were found in the genes PRKAG2, PLN, MYH7, MYH6, LMNA, and DES. In the cohort of the RCM-cases variants in 3 different genes were identified: TNNI3, MYL3, and CRYAB. ACMG class 3–5 = variant of uncertain significance, likely pathogenic, pathogenic, respectively.
Genotyping results
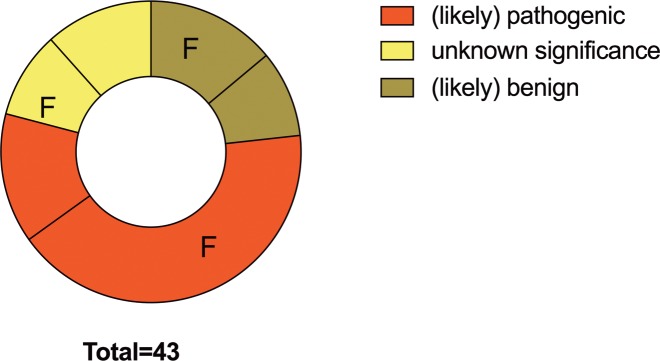
In the entire study population we identified (likely) pathogenic mutations in 56% of index-patients (18 familial, 6 sporadic cases). Nine patients were carriers of a pathogenic and 15 carried a likely pathogenic mutation. VUS were found in 21% of cases (4 familial, 5 sporadic cases). An only likely benign variant was identified in one patient and variants with an allele frequency exceeding the disease prevalence and therefore not further investigated were identified in 9 patients. This means that in total in 23% (n = 10, 6 familial, 4 sporadic cases) of patients no disease associated variants were identified (Fig 2).
Fig 2. Distribution of variant classes.
We genotyped 43 index-patients. Of these 18 familial and 6 sporadic cases carried (likely) pathogenic mutations. At least variants of uncertain significance were found in 4 familial and 5 sporadic cases. Only likely benign variants or variants with an allele frequency exceeding the disease prevalence were identified in 10 patients (6 familial, 4 sporadic cases). Familial disposition for the cardiomyopathy is based on pedigree analysis and family reports. Abbreviations: F = familial cases, no label = sporadic cases.
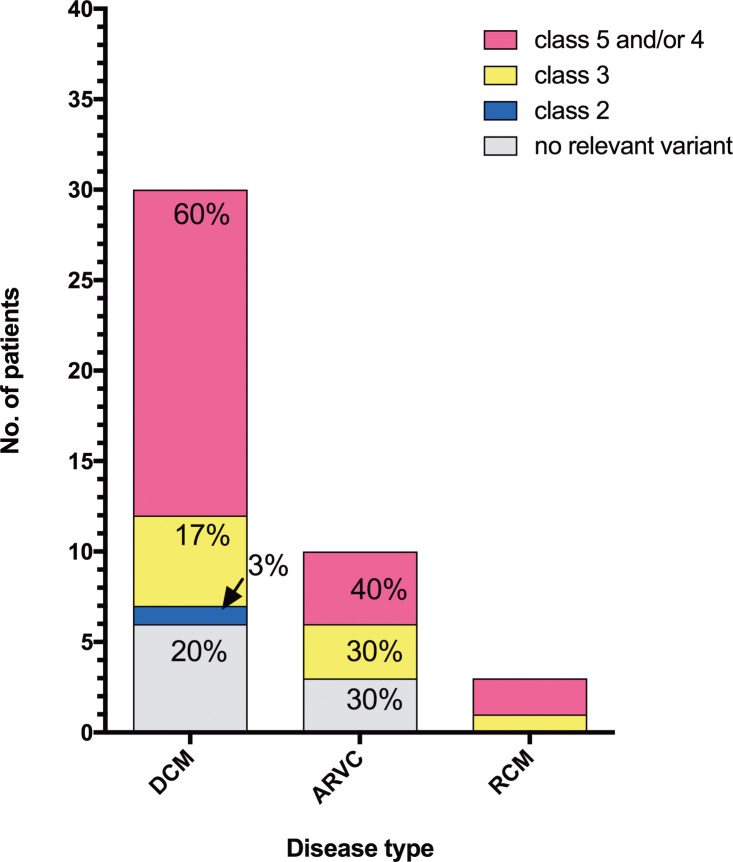
Of the DCM-patients, 60% (n = 18) had pathogenic or likely pathogenic mutations, respectively, while 17% (n = 5) were at least carriers of VUS. One DCM-case (DCM-10) had only a likely benign variant. In DCM-patients 25–30 only polymorphisms were identified (Fig 3). The proportion of pathogenic or likely pathogenic mutations was 66% in familial DCM and 44% in sporadic DCM-cases. In 40% (n = 4; 3 familial, 1 sporadic case) of ARVC-cases pathogenic or likely pathogenic mutations were found (Fig 3). In the entire ARVC-cohort (likely) pathogenic mutations were identified in 50% of familial cases (n = 6). In sporadic cases (n = 4) one pathogenic mutation was identified. Three ARVC-patients each were carriers of VUS or polymorphisms, respectively (Fig 3). In the RCM-cases (n = 3) two patients with pathogenic or likely pathogenic mutations (1 familial, 1 sporadic case), respectively, were identified (Fig 3).
Fig 3. Classification of the variants.
In 60% of DCM- and 40% of ARVC-cases pathogenic and/or likely pathogenic mutations were identified. At least variants with uncertain significance were found in 17% DCM- and 30% ARVC-cases. No relevant variants (MAF >0.0005 in etiological matching controls) were found in 22% and 30% of DCM-, and ARVC-cases, respectively. In RCM-cases, 2 pathogenic and/or likely pathogenic mutations and 1 variant with uncertain significance were identified. Abbreviations: class 2 = likely benign, class 3 = variant of uncertain significance, class 4 = likely pathogenic, class 5 = pathogenic.
Variant classification
In 19 of 46 genes, a total of 57 variants were found (Fig 1). We identified 41 missense variants in addition to 3 nonsense, 7 frameshift, 3 in frame insertion/deletion, and 3 canonical splice-site variants. Out of these, 15 had entries in the mutation-databases [8, 24], whereas 42 variants were previously not described in context with a disease. We evaluated the pathogenic evidence of all variants (S5 and S6 Tables) and classified four variants likely benign, whereas fifty-three variants were classified (likely) pathogenic or VUS, respectively. The potentially disease related variants affected 18 genes. In total, we identified 9 pathogenic mutations in 9 index-patients (8 familial cases, 1 sporadic case) in 6 different genes (LMNA, DES, RBM20, CRYAB, PKP2, PLN). We identified two or more variants in 14 DCM- and 3 ARVC-cases.
In DCM-patients TTN was the most frequently affected gene (51% of variants; Fig 1). In the DCM-cohort, pathogenic mutations were identified in DES, LMNA, and RBM20 (Table 1, S5 Table), whereas likely pathogenic mutations were found in MYL2, MYH7, TTN, TNNC1, DES, LMNA, RBM20, NEXN, and PKP2. Remarkably, a homozygous PKP2-gene mutation (c.2035C>T, p.His679Tyr) was identified in a large Turkish family (DCM-23). As expected, PKP2 was the most frequently affected gene in ARVC-patients. Pathogenic mutations in the ARVC-cohort were found in PKP2 and PLN, a likely pathogenic mutation was found in LMNA (Table 1, S5 Table). Surprisingly, no further desmosomal genes were affected in ARVC-cases. In the RCM-cases two patients with pathogenic or likely pathogenic mutations in TNNI3 and CRYAB, respectively, were identified (Table 1, S5 Table). The median age at diagnosis in DCM- and ARVC-cases (33 and 36 years, respectively) was not significantly different in dependence of variant classification (S3 Fig).
Twenty-one TTN variants (7 TTN-tv (premature stop codon with/without preceded frameshift, and canonical ± 1 or 2 splice site variants), 13 missense, 1 in-frame insertion) were identified in 16 (37%) of 43 index-patients (Table 1, S5 Table). In DCM-patients TTN-variants were more frequent (p<0.05; S4 Fig), whereas TTN-tv were increased by trend (p = 0.05, data not shown) when compared to the other cardiomyopathies. Most of the TTN-variants (5 TTN-tv, 7 missense) affected the titin domains spanning the A-band of the sarcomere. But also variants in the I-band (3x missense, 2x TTN-tv), M-line (2x missense, 1x in frame insertion), and Z-band (1x missense) region of the protein were identified (S7 Table). All but one TTN-variant were located within exons that are estimated to be incorporated in 100% of the cardiac TTN-transcripts (PSI 100%, [6], http://cardiodb.org/titin) and might be expressed to a notable amount. The TTN-variant found in patient DCM-2 is located within the I-band and is estimated to be expressed only in 8% of the transcripts and is therefore believed to be of low disease relevance [6]. Seven (21%) of the 34 variant carriers of the present study had only TTN-variant(s). Of these four patients had a single TTN missense variant affecting the I-, A, and Z-band of titin, respectively. One patient was carrier of a single TTN-tv in the A-band of the protein. DCM-16 had a splice and a missense TTN-variant in the A- and I-band, respectively. DCM-24 is carrier of one in-frame duplication and two missense variants affecting the M-line and the A-band, respectively (S5 and S7 Tables).
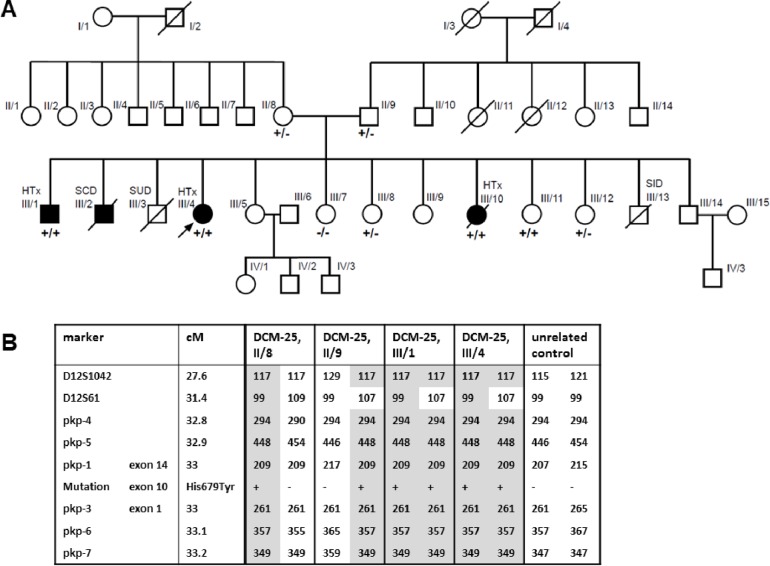
Family with a novel homozygous PKP2-gene mutation
We identified a novel homozygous PKP2-mutation c.2035C>T, p.His679Tyr in index-patient DCM-23 (III/4, Fig 4A) who is a member of a large non-consanguineous Yezidi family. The affected family members did not fulfill the ARVC Task Force criteria although PKP2 is generally associated with ARVC. Three genetically untested brothers died suddenly in childhood (III/2, III/3, III/13; 11 years, 2 years, 7 days, respectively). She and two siblings (male (III/1), female (III/10)) who are also homozygous for the PKP2-mutation underwent HTx in adolescent age (14, 13 and 17 years, respectively) because of DCM (ECGs shown in S5 Fig.). The 57 years old mother (II/8), the 66 years old father (II/9) and two other siblings (III/8, III/12) who are heterozygous mutation carriers have no signs of cardiac disease at all, suggesting a variant co-segregation in an autosomal recessive mode. Surprisingly, the youngest sister (III/11, 18 years old) who is also a homozygous mutation carrier has currently no detectable signs of cardiomyopathy as examined by ECG, TTE and MRI (data not shown). The suspected pathogenic impact of PKP2 c.2035C>T was verified by analyzing whole exome data of the parents, an unaffected sister (III/8), and the index-patient (III/4) (S1 Methods, S6 Fig). No other co-segregating variant with an allele frequency ≤0.0005 was found in cardiomyopathy genes listed in HGMD (n = 156, S8 Table). A further indication of pathogenicity is the absence of PKP2 c.2035C>T in the ExAc browser with sufficient coverage of the gene region (read depth of 50 in 80% of the alleles). Analysis of the PKP2 locus (Fig 4B, S1 Methods) of the index-patient (III/4) and her transplanted brother (III/1) revealed that they are homozygous for a haplotype surrounding the PKP2-gene which largely overlaps between father (II/9) and mother (II/8), suggesting that they are probably (distantly) related and the mutation might be inherited from a common ancestor. In order to study the pathogenic mechanism of the mutation we investigated plakophilin-2 mRNA and protein levels in explanted myocardium, but no differences compared to controls were detected (S1 Methods, S7 and S8 Figs). Immunofluorescence staining of myocardial sections of the explanted heart of individual III/10 showed normal localization of PKP2 at the intercalated disc (S1 Methods, S9 Fig). Thus, the mutation appears to have no influence on the stability or subcellular localization of PKP2 within the myocardium. No segregation with disease was observed for the nonsense variant in LAMA4 (S5 Table).
Fig 4. Pedigree of DCM-23 family and PKP2 c.2035C>T co-segregation.
A. Family members with HTx were homozygous carriers of PKP2 c.2035C>T, p.His679Tyr whereas heterozygous carriers and the homozygous carrier III/11 had no signs of cardiomyopathy. The LAMA4 variant did not co-segregate with disease (data not shown). Squares = males, circles = females. Deceased individuals are indicated by slashes. Filled symbols indicate individuals with DCM. The index-patient is marked with an arrow. Genotypes are shown by present (+) or by absent (-) of the gene variant. Abbreviations: SCD = sudden cardiac death, SID = sudden infant death, SUD = unexplained sudden death. B. Haplotype analyses of PKP2 c.2035C>T mutation carriers from family DCM-23. Haplotypes associated with the PKP2 mutation are shown in grey shaded areas. These haplotypes are identical in both parents (II/8, II/9) with the exception of marker D12S61. Abbreviation: cM = centimorgan.
Discussion
This study focused on the genotyping of patients with advanced cardiomyopathy. Our inclusion criteria lead to a study cohort mainly composed of patients who have been bridged for heart transplantation and those already transplanted. The study design was set for the identification of highly penetrant monogenic causes of cardiomyopathies.
In total 57 variants were identified of which a high proportion were classified (likely) pathogenic (51%). Surprisingly, (likely) pathogenic mutations were more frequently present in DCM- than in ARVC-cases (60% versus 40%) although the majority of currently known ARVC-genes with the exception of the minor disease genes TGFB3, CTNNA3 (see www.arvcdatabase.info), [4], FLNC [30], and SCN5A [31] were analyzed. No variants were identified even in one definite and one familial ARVC-case. This strongly suggests that other currently unknown genes and/or genotypes are involved in the development of ARVC. Especially future screening of the FLNC-gene could increase the variant detection because a prevalence of 1% of truncating FLNC-mutations was reported in dilated and arrhythmic cardiomyopathies [30].
The mutation rate and profile in ARVC patients is in discrepancy to what have been expected and published before by others. For example Groeneweg et al. [32] found a mutation rate of 63% in a large ARVC-cohort, and in desmosomal genes a mutation rate of 40% was reported [33]. The high mutation rate in our DCM-cohort is in the upper range of values reported so far [2, 4, 5], in case of familial DCM it is in agreement with the findings of Cuenca et al. [7]. Apparently, the mutation profiles differ notably between the different studies. As expected, screening for gene variants is more successful in familial cases, but also in presumably sporadic cases (likely) pathogenic mutations were identified in a noteworthy high number (25%). In previous studies the prevalence of (potentially) pathogenic mutations in sporadic DCM-cases was 8% and 68%, respectively [4, 5]. Our study cohort includes 12 patients with disease onset at ≤20 years of age assuming a genetic cause of disease although familial cardiomyopathy was reported only for four cases. In eight patients an at least likely pathogenic gene mutation was identified. These findings underscore the relevance to perform genetic testing not only in suspected familial or sporadic cases with clinical clues suggestive of a particular/rare genetic disease as recommended by the European Society of Cardiology [11] but in all index-patients with an unknown etiology of the disease. Nevertheless, a characteristic mutation profile for severe cardiomyopathy could not be defined.
Twenty five percent of our DCM cohort carried a TTN-tv mutation as reported for end-stage DCM patients by Roberts et al. [6]. All TTN-tv mutations were classified as likely pathogenic considering a high prevalence of TTN-tv in DCM-cohorts. TTN alternative splicing, position-independent nonsense-mediated mRNA decay, an internal promoter, allele-specific expression, structural and functional effects on sarcomere formation and force generation as well as negative effects by incorporation of truncated titin into the sarcomere were discussed as pathomechanisms for truncated titin [34–39]. Nevertheless, many additional data are required for a better understanding of the mechanisms. Because of the background noise in the general population TTN missense variants were classified as VUS although recent large-scale sequencing and functional analysis indicated strong impact on cardiomyopathies [40–42]. Protein unfolding and domain destabilization was shown and/or predicted for TTN missense mutations located in the Z-disk [42], A/I junction region [43], and in the I-band [41] of the protein, respectively. Decreased contractile force generation of a missense mutation located in the Z/I-band junction was reported by Hinson et al. [35]. We identified 7 index-patients with only TTN variants of different types affecting different protein regions. But although functional data are available a final classification of TTN variants is not possible. Classification still based mostly on populations genetic data and one should keep in mind that new functional data could lead to variant re-classification. Two patients carried multiple TTN variants. We did not investigate whether the gene was affected in a compound heterozygous or homozygous way. Regardless, no data are available about patients with several TTN variants and about a possibly increasing impact on disease. In agreement with recent data [6, 40] most TTN-variants affected the inextensible A-band of titin and are incorporated in 100% of the cardiac TTN-transcripts. [44, 45]. Patient DCM-16 is carrier of a TTN-tv and missense variant, had disease onset at the age of 20 years and VAD implantation when she was 32 years old. Therefore, we suggest that TTN associated cardiomyopathy is present also in young adults even though mostly it has its onset in the mid-late life period [40].
We identified a non-synonymous PKP2-mutation that in homozygous carriers led to manifestation of end-stage DCM at young age. This mutation might be characterized by a reduced penetrance [46–48] since at present a homozygous 18 years old mutation carrier has no signs of cardiac disease. We cannot rule out additional genetic factor(s) underlying the disease of the family, although screening of all known cardiomyopathy associated genes gave no indication for this. For PKP2 truncating mutations and interestingly, also for missense mutations haploinsufficiency was indicated as a possible pathomechanism. Functional data to support this assumption are limited. Kirchner et al. [49] reported decreased in vivo and in vitro protein expression, impairment of protein structure and stability, and mislocation of plakophilin 2 in the cytoplasm in case of PKP2 missense mutations. In addition for other PKP2 missense mutations impairment of in vitro de novo desmosome assembly was described [50] and influence on the expression of heat shock protein 90 was observed in case of two PKP2 truncating mutations [51]. In our study the investigation of heart tissue of a homozygous mutation carrier revealed no impact of PKP2 p.His679Tyr on plakophilin expression, stability and cell localization. This might indicate a different pathomechanism as described above, although it must clearly be pointed out, that in contrast to our in vivo data the characteristics of the mutations described by Kirchner et al. based mainly on cell culture experiments. To our knowledge, this is the first report of a PKP2-missense mutation causing recessively inherited DCM. No signs of hair or skin abnormalities that were reported with other recessive desmosomal gene mutations [52, 53] were observed.
We detected a missense mutation in the Z-disk protein NEXN that was already described to have a disruptive effect on the cardiac sarcomere in a DCM patient and a dominant negative effect on Z-disk stability in zebrafish [54]. In accordance, we found this mutation in a male DCM patient (DCM-19) who underwent VAD implantation at the age of 22 years. Based on the functional studies described by Hassel et al. [54], an allele frequency clearly below the prevalence of DCM, and multiple computational evidence for a deleterious effect on the protein this NEXN mutation must be classified as likely pathogenic according to ACMG guidelines. Our study is the second report that links the NEXN gene to DCM and thereby strengthens the importance of NEXN as a (minor) disease gene.
In our study, the usage of a sequencing panel with a comparatively small number of myopathy associated genes for genotyping patients has historical reasons. But despite the limited gene number it is important to point out that the majority of variants identified here were novel variants in known major disease genes which are listed in the Mendelian Inheritance in Man (MIM) compendium and which are covered by the 46-gene panel used here. As expected besides these also variants in minor disease genes were identified.
Extensive variation screening in other (minor) disease genes in the whole exome and genome, respectively, might provide further insights. However, variant classification with respect to the impact on disease development and clinical course still remains the real challenge [12]. Due to limited availability of case reports, small families with limited co-segregation data, and rarely available functional data, some ACMG [12] criteria were not applicable and others had to be adjusted. But apart from this limitation, the ACMG guidelines were a suitable tool for a uniform and differentiated variant classification. At present there are no guidelines available how to treat non-symptomatic mutation carriers, due to the heterogeneous genetic background of cardiomyopathies and the lack of pharmacological evidence for preventive treatment. In order to overcome this limitation in the future more studies like the recent trials that investigate the effect of drug treatment of pre-symptomatic PLN and LMNA mutation carriers are of impact (Clinical trials identifier: NCT01857856 and European Society of Cardiology Congress 2016, Rome, Poster P4981, respectively).
Limitation
We excluded variants with an allele frequency above the disease prevalence. Therefore, this study is not suited for the identification of a complex genotype or modifiers as well as variants with reduced penetrance. Copy number variants and large DNA-rearrangements have not been investigated. Only allele frequencies of the ethnically narrow non-Finnish European population provided by the Exome Aggregation Consortium were taken into account to define variants of further interest. Variant screening was limited to 46 myopathy associated genes covered by the TruSight™ Cardiomyopathy gene panel of Illumina. The recently described ARVC and DCM disease gene FLNC and the ARVC disease gene SCN5A were not screened for variants.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The authors gratefully thank all participating patients and the staff of the transplantation unit of the HDZ-NRW for their continuous help and support of this research project. We thank Désirée Gerdes, Daniela Baurichter, Ramona Cebulla and Ludolf Boven for excellent technical assistance. The authors would like to thank the Exome Aggregation Consortium and the groups that provided exome variant data for comparison.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by a grant of the Erich and Hanna Klessmann Foundation, Gütersloh, Germany to HM; the Deutsche Forschungsgemeinschaft (DFG) [grant No. MI 1146/2-1 to HM]; and The Netherlands Cardiovascular Research Initiative: An initiative with support of the Dutch Heart Foundation [CVON2012-10 PREDICT and CVON2014-40 DOSIS to JPvT]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ng D, Johnston JJ, Teer JK, Singh LN, Peller LC, Wynter JS, et al. Interpreting secondary cardiac disease variants in an exome cohort. Circ Cardiovasc Genet. 2013;6(4):337–46. Epub 2013/07/19. doi: 10.1161/CIRCGENETICS.113.000039 CIRCGENETICS.113.000039 [pii]. ; PubMed Central PMCID: PMC3887521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pugh TJ, Kelly MA, Gowrisankar S, Hynes E, Seidman MA, Baxter SM, et al. The landscape of genetic variation in dilated cardiomyopathy as surveyed by clinical DNA sequencing. Genet Med. 2014;16(8):601–8. Epub 2014/02/08. doi: 10.1038/gim.2013.204 gim2013204 [pii]. . [DOI] [PubMed] [Google Scholar]
- 3.Golbus JR, Puckelwartz MJ, Dellefave-Castillo L, Fahrenbach JP, Nelakuditi V, Pesce LL, et al. Targeted Analysis of Whole Genome Sequence Data to Diagnose Genetic Cardiomyopathy. Circulation: Cardiovascular Genetics. 2014;7(6):751–9. doi: 10.1161/circgenetics.113.000578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haas J, Frese KS, Peil B, Kloos W, Keller A, Nietsch R, et al. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur Heart J. 2014. Epub 2014/08/29. doi: ehu301 [pii] doi: 10.1093/eurheartj/ehu301 . [DOI] [PubMed] [Google Scholar]
- 5.van Spaendonck-Zwarts KY, van Rijsingen IA, van den Berg MP, Lekanne Deprez RH, Post JG, van Mil AM, et al. Genetic analysis in 418 index patients with idiopathic dilated cardiomyopathy: overview of 10 years' experience. Eur J Heart Fail. 2013;15(6):628–36. Epub 2013/01/26. doi: 10.1093/eurjhf/hft013 hft013 [pii]. . [DOI] [PubMed] [Google Scholar]
- 6.Roberts AM, Ware JS, Herman DS, Schafer S, Baksi J, Bick AG, et al. Integrated allelic, transcriptional, and phenomic dissection of the cardiac effects of titin truncations in health and disease. Sci Transl Med. 2015;7(270):270ra6 Epub 2015/01/16. doi: 10.1126/scitranslmed.3010134 7/270/270ra6 [pii]. ; PubMed Central PMCID: PMC4560092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cuenca S, Ruiz-Cano MJ, Gimeno-Blanes JR, Jurado A, Salas C, Gomez-Diaz I, et al. Genetic basis of familial dilated cardiomyopathy patients undergoing heart transplantation. J Heart Lung Transplant. 2016. Epub 2016/02/24. doi: S1053-2498(16)00009-7 [pii] doi: 10.1016/j.healun.2015.12.014 . [DOI] [PubMed] [Google Scholar]
- 8.Stenson PD, Mort M, Ball EV, Shaw K, Phillips A, Cooper DN. The Human Gene Mutation Database: building a comprehensive mutation repository for clinical and molecular genetics, diagnostic testing and personalized genomic medicine. Hum Genet. 2014;133(1):1–9. Epub 2013/10/01. doi: 10.1007/s00439-013-1358-4 ; PubMed Central PMCID: PMC3898141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ackerman MJ, Priori SG, Willems S, Berul C, Brugada R, Calkins H, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies: this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Europace. 2011;13(8):1077–109. Epub 2011/08/04. doi: 10.1093/europace/eur245 eur245 [pii]. . [DOI] [PubMed] [Google Scholar]
- 10.Hershberger RE, Siegfried JD. Update 2011: clinical and genetic issues in familial dilated cardiomyopathy. J Am Coll Cardiol. 2011;57(16):1641–9. Epub 2011/04/16. doi: 10.1016/j.jacc.2011.01.015 S0735-1097(11)00520-1 [pii]. ; PubMed Central PMCID: PMC3088091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pinto YM, Elliott PM, Arbustini E, Adler Y, Anastasakis A, Bohm M, et al. Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J. 2016;37(23):1850–8. Epub 2016/01/23. doi: 10.1093/eurheartj/ehv727 ehv727 [pii]. . [DOI] [PubMed] [Google Scholar]
- 12.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24. Epub 2015/03/06. doi: 10.1038/gim.2015.30 gim201530 [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010;31(7):806–14. Epub 2010/02/23. doi: 10.1093/eurheartj/ehq025 ehq025 [pii]. ; PubMed Central PMCID: PMC2848326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deshpande SR, Herman HK, Quigley PC, Shinnick JK, Cundiff CA, Caltharp S, et al. Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia (ARVC/D): Review of 16 Pediatric Cases and a Proposal of Modified Pediatric Criteria. Pediatr Cardiol. 2016;37(4):646–55. Epub 2016/01/09. doi: 10.1007/s00246-015-1327-x 10.1007/s00246-015-1327-x [pii]. . [DOI] [PubMed] [Google Scholar]
- 15.Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O'Connell J, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation. 1996;93(5):841–2. Epub 1996/03/01. . [DOI] [PubMed] [Google Scholar]
- 16.Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29(2):270–6. Epub 2007/10/06. doi: ehm342 [pii] doi: 10.1093/eurheartj/ehm342 . [DOI] [PubMed] [Google Scholar]
- 17.Teekakirikul P, Kelly MA, Rehm HL, Lakdawala NK, Funke BH. Inherited cardiomyopathies: molecular genetics and clinical genetic testing in the postgenomic era. J Mol Diagn. 2013;15(2):158–70. Epub 2013/01/01. doi: 10.1016/j.jmoldx.2012.09.002 S1525-1578(12)00304-2 [pii]. . [DOI] [PubMed] [Google Scholar]
- 18.Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25(14):1754–60. Epub 2009/05/20. doi: 10.1093/bioinformatics/btp324 btp324 [pii]. ; PubMed Central PMCID: PMC2705234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20(9):1297–303. Epub 2010/07/21. doi: 10.1101/gr.107524.110 gr.107524.110 [pii]. ; PubMed Central PMCID: PMC2928508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics. 2009;25(16):2078–9. Epub 2009/06/10. doi: 10.1093/bioinformatics/btp352 btp352 [pii]. ; PubMed Central PMCID: PMC2723002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Exome Aggregation Consortium (ExAC) C, MA. http://exacbroadinstituteorg, Version 03, January 2015
- 22.Towbin JA, Lorts A, Jefferies JL. Left ventricular non-compaction cardiomyopathy. Lancet. 2015. Epub 2015/04/14. doi: S0140-6736(14)61282-4 [pii] doi: 10.1016/S0140-6736(14)61282-4 . [DOI] [PubMed] [Google Scholar]
- 23.van der Zwaag PA, Jongbloed JD, van den Berg MP, van der Smagt JJ, Jongbloed R, Bikker H, et al. A genetic variants database for arrhythmogenic right ventricular dysplasia/cardiomyopathy. Hum Mutat. 2009;30(9):1278–83. Epub 2009/07/02. doi: 10.1002/humu.21064 . [DOI] [PubMed] [Google Scholar]
- 24.Lazzarini E, Jongbloed JD, Pilichou K, Thiene G, Basso C, Bikker H, et al. The ARVD/C genetic variants database: 2014 update. Hum Mutat. 2015;36(4):403–10. Epub 2015/02/14. doi: 10.1002/humu.22765 . [DOI] [PubMed] [Google Scholar]
- 25.Li B, Krishnan VG, Mort ME, Xin F, Kamati KK, Cooper DN, et al. Automated inference of molecular mechanisms of disease from amino acid substitutions. Bioinformatics. 2009;25(21):2744–50. Epub 2009/09/08. doi: 10.1093/bioinformatics/btp528 btp528 [pii]. ; PubMed Central PMCID: PMC3140805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calabrese R, Capriotti E, Fariselli P, Martelli PL, Casadio R. Functional annotations improve the predictive score of human disease-related mutations in proteins. Hum Mutat. 2009;30(8):1237–44. Epub 2009/06/11. doi: 10.1002/humu.21047 . [DOI] [PubMed] [Google Scholar]
- 27.Capriotti E, Altman RB. Improving the prediction of disease-related variants using protein three-dimensional structure. BMC Bioinformatics. 2011;12 Suppl 4:S3 Epub 2011/10/26. doi: 10.1186/1471-2105-12-S4-S3 1471-2105-12-S4-S3 [pii]. ; PubMed Central PMCID: PMC3194195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shihab HA, Gough J, Cooper DN, Stenson PD, Barker GL, Edwards KJ, et al. Predicting the functional, molecular, and phenotypic consequences of amino acid substitutions using hidden Markov models. Hum Mutat. 2013;34(1):57–65. Epub 2012/10/04. doi: 10.1002/humu.22225 ; PubMed Central PMCID: PMC3558800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7(4):248–9. Epub 2010/04/01. doi: 10.1038/nmeth0410-248 nmeth0410-248 [pii]. ; PubMed Central PMCID: PMC2855889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ortiz-Genga MF, Cuenca S, Dal Ferro M, Zorio E, Salgado-Aranda R, Climent V, et al. Truncating FLNC Mutations Are Associated With High-Risk Dilated and Arrhythmogenic Cardiomyopathies. J Am Coll Cardiol. 2016;68(22):2440–51. Epub 2016/12/03. doi: S0735-1097(16)36416-6 [pii] doi: 10.1016/j.jacc.2016.09.927 . [DOI] [PubMed] [Google Scholar]
- 31.Te Riele AS, Agullo-Pascual E, James CA, Leo-Macias A, Cerrone M, Zhang M, et al. Multilevel analyses of SCN5A mutations in arrhythmogenic right ventricular dysplasia/cardiomyopathy suggest non-canonical mechanisms for disease pathogenesis. Cardiovasc Res. 2017;113(1):102–11. Epub 2017/01/11. doi: 10.1093/cvr/cvw234 cvw234 [pii]. ; PubMed Central PMCID: PMC5220677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Groeneweg JA, Bhonsale A, James CA, Te Riele AS, Dooijes D, Tichnell C, et al. Clinical Presentation, Long-Term Follow-Up, and Outcomes of 1001 Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy Patients and Family Members. Circ Cardiovasc Genet. 2015. Epub 2015/03/31. doi: CIRCGENETICS.114.001003 [pii] doi: 10.1161/CIRCGENETICS.114.001003 . [DOI] [PubMed] [Google Scholar]
- 33.Pilichou K, Nava A, Basso C, Beffagna G, Bauce B, Lorenzon A, et al. Mutations in desmoglein-2 gene are associated with arrhythmogenic right ventricular cardiomyopathy. Circulation. 2006;113(9):1171–9. doi: 10.1161/CIRCULATIONAHA.105.583674 . [DOI] [PubMed] [Google Scholar]
- 34.Gramlich M, Michely B, Krohne C, Heuser A, Erdmann B, Klaassen S, et al. Stress-induced dilated cardiomyopathy in a knock-in mouse model mimicking human titin-based disease. J Mol Cell Cardiol. 2009;47(3):352–8. Epub 2009/05/02. doi: 10.1016/j.yjmcc.2009.04.014 S0022-2828(09)00182-5 [pii]. ; PubMed Central PMCID: PMC2764556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hinson JT, Chopra A, Nafissi N, Polacheck WJ, Benson CC, Swist S, et al. HEART DISEASE. Titin mutations in iPS cells define sarcomere insufficiency as a cause of dilated cardiomyopathy. Science. 2015;349(6251):982–6. Epub 2015/09/01. doi: 10.1126/science.aaa5458 349/6251/982 [pii]. ; PubMed Central PMCID: PMC4618316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schafer S, de Marvao A, Adami E, Fiedler LR, Ng B, Khin E, et al. Titin-truncating variants affect heart function in disease cohorts and the general population. Nat Genet. 2017;49(1):46–53. Epub 2016/11/22. doi: 10.1038/ng.3719 ng.3719 [pii]. ; PubMed Central PMCID: PMC5201198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carmignac V, Salih MA, Quijano-Roy S, Marchand S, Al Rayess MM, Mukhtar MM, et al. C-terminal titin deletions cause a novel early-onset myopathy with fatal cardiomyopathy. Ann Neurol. 2007;61(4):340–51. Epub 2007/04/21. doi: 10.1002/ana.21089 . [DOI] [PubMed] [Google Scholar]
- 38.Zou J, Tran D, Baalbaki M, Tang LF, Poon A, Pelonero A, et al. An internal promoter underlies the difference in disease severity between N- and C-terminal truncation mutations of Titin in zebrafish. Elife. 2015;4:e09406 Epub 2015/10/17. doi: 10.7554/eLife.09406 e09406 [pii]. ; PubMed Central PMCID: PMC4720518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deo RC. Alternative Splicing, Internal Promoter, Nonsense-Mediated Decay, or All Three: Explaining the Distribution of Truncation Variants in Titin. Circ Cardiovasc Genet. 2016;9(5):419–25. Epub 2016/10/21. doi: CIRCGENETICS.116.001513 [pii] doi: 10.1161/CIRCGENETICS.116.001513 ; PubMed Central PMCID: PMC5068190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Begay RL, Graw S, Sinagra G, Merlo M, Slavov D, Gowan K, et al. Role of Titin Missense Variants in Dilated Cardiomyopathy. J Am Heart Assoc. 2015;4(11). Epub 2015/11/15. doi: 10.1161/JAHA.115.002645 e002645 [pii] JAHA.115.002645 [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bogomolovas J, Fleming JR, Anderson BR, Williams R, Lange S, Simon B, et al. Exploration of pathomechanisms triggered by a single-nucleotide polymorphism in titin's I-band: the cardiomyopathy-linked mutation T2580I. Open Biol. 2016;6(9). Epub 2016/09/30. doi: 160114 [pii] rsob.160114 [pii] doi: 10.1098/rsob.160114 ; PubMed Central PMCID: PMC5043576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hastings R, de Villiers CP, Hooper C, Ormondroyd L, Pagnamenta A, Lise S, et al. Combination of Whole Genome Sequencing, Linkage, and Functional Studies Implicates a Missense Mutation in Titin as a Cause of Autosomal Dominant Cardiomyopathy With Features of Left Ventricular Noncompaction. Circ Cardiovasc Genet. 2016;9(5):426–35. Epub 2016/10/21. doi: CIRCGENETICS.116.001431 [pii] doi: 10.1161/CIRCGENETICS.116.001431 ; PubMed Central PMCID: PMC5068189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peled Y, Gramlich M, Yoskovitz G, Feinberg MS, Afek A, Polak-Charcon S, et al. Titin mutation in familial restrictive cardiomyopathy. Int J Cardiol. 2014;171(1):24–30. Epub 2013/12/10. doi: 10.1016/j.ijcard.2013.11.037 S0167-5273(13)02055-X [pii]. . [DOI] [PubMed] [Google Scholar]
- 44.Herman DS, Lam L, Taylor MR, Wang L, Teekakirikul P, Christodoulou D, et al. Truncations of titin causing dilated cardiomyopathy. N Engl J Med. 2012;366(7):619–28. Epub 2012/02/18. doi: 10.1056/NEJMoa1110186 ; PubMed Central PMCID: PMC3660031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jansweijer JA, Nieuwhof K, Russo F, Hoorntje ET, Jongbloed JD, Lekanne Deprez RH, et al. Truncating titin mutations are associated with a mild and treatable form of dilated cardiomyopathy. Eur J Heart Fail. 2016. Epub 2016/11/05. doi: 10.1002/ejhf.673 . [DOI] [PubMed] [Google Scholar]
- 46.Rigato I, Bauce B, Rampazzo A, Zorzi A, Pilichou K, Mazzotti E, et al. Compound and digenic heterozygosity predicts lifetime arrhythmic outcome and sudden cardiac death in desmosomal gene-related arrhythmogenic right ventricular cardiomyopathy. Circ Cardiovasc Genet. 2013;6(6):533–42. Epub 2013/09/28. doi: 10.1161/CIRCGENETICS.113.000288 CIRCGENETICS.113.000288 [pii]. . [DOI] [PubMed] [Google Scholar]
- 47.Quarta G, Muir A, Pantazis A, Syrris P, Gehmlich K, Garcia-Pavia P, et al. Familial evaluation in arrhythmogenic right ventricular cardiomyopathy: impact of genetics and revised task force criteria. Circulation. 2011;123(23):2701–9. Epub 2011/05/25. doi: 10.1161/CIRCULATIONAHA.110.976936 CIRCULATIONAHA.110.976936 [pii]. . [DOI] [PubMed] [Google Scholar]
- 48.Xu T, Yang Z, Vatta M, Rampazzo A, Beffagna G, Pilichou K, et al. Compound and digenic heterozygosity contributes to arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2010;55(6):587–97. Epub 2010/02/16. doi: 10.1016/j.jacc.2009.11.020 S0735-1097(09)03813-3 [pii]. ; PubMed Central PMCID: PMC2852685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kirchner F, Schuetz A, Boldt LH, Martens K, Dittmar G, Haverkamp W, et al. Molecular insights into arrhythmogenic right ventricular cardiomyopathy caused by plakophilin-2 missense mutations. Circ Cardiovasc Genet. 2012;5(4):400–11. Epub 2012/07/12. doi: 10.1161/CIRCGENETICS.111.961854 CIRCGENETICS.111.961854 [pii]. . [DOI] [PubMed] [Google Scholar]
- 50.Hall C, Li S, Li H, Creason V, Wahl JK 3rd. Arrhythmogenic right ventricular cardiomyopathy plakophilin-2 mutations disrupt desmosome assembly and stability. Cell Commun Adhes. 2009;16(1–3):15–27. Epub 2009/06/18. doi: 10.1080/15419060903009329 912444287 [pii]. . [DOI] [PubMed] [Google Scholar]
- 51.Joshi-Mukherjee R, Coombs W, Musa H, Oxford E, Taffet S, Delmar M. Characterization of the molecular phenotype of two arrhythmogenic right ventricular cardiomyopathy (ARVC)-related plakophilin-2 (PKP2) mutations. Heart Rhythm. 2008;5(12):1715–23. doi: 10.1016/j.hrthm.2008.09.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McKoy G, Protonotarios N, Crosby A, Tsatsopoulou A, Anastasakis A, Coonar A, et al. Identification of a deletion in plakoglobin in arrhythmogenic right ventricular cardiomyopathy with palmoplantar keratoderma and woolly hair (Naxos disease). Lancet. 2000;355(9221):2119–24. doi: 10.1016/S0140-6736(00)02379-5 . [DOI] [PubMed] [Google Scholar]
- 53.Alcalai R, Metzger S, Rosenheck S, Meiner V, Chajek-Shaul T. A recessive mutation in desmoplakin causes arrhythmogenic right ventricular dysplasia, skin disorder, and woolly hair. J Am Coll Cardiol. 2003;42(2):319–27. . [DOI] [PubMed] [Google Scholar]
- 54.Hassel D, Dahme T, Erdmann J, Meder B, Huge A, Stoll M, et al. Nexilin mutations destabilize cardiac Z-disks and lead to dilated cardiomyopathy. Nat Med. 2009;15(11):1281–8. Epub 2009/11/03. doi: 10.1038/nm.2037 nm.2037 [pii]. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.