Abstract
This study aims to determine the stability of palatal rugae before and after orthodontic treatment. 50 orthodontic cases were selected with pre- and posttreatment casts and 50 casts were randomly selected as variables. Landmarks on the palatal raphe and rugae were marked on the maxillary casts. Points were made on medial and lateral ends of first, second and third rugae. Each cast was photographed, measured and then trimmed leaving only the rugae area of the hard palate. In the pre and post-treatment group, changes in transverse measurements were significantly different for lateral points of first rugae and anteroposterior changes were significant for the distances between first and second rugae. All inter-point measurements of third rugae were stable in post-treatment casts. Thirty blinded examiners compared 50 trimmed preorthodontic casts to similarly prepared one hundred casts for possible matches based on pattern of rugae. The percentages of correct matches for examiners had a median of 90%. The matching of pre-operative and post-operative orthodontic casts demonstrated that although some changes do occur in the rugae during orthodontic treatment, the morphology of palatal rugae remains stable throughout life. Hence carefully assessed rugae pattern may have a definite role in forensic identification. Further, points associated with the third palatal ruage were the most immutable over a person's life and hence could be used as a reference to evaluate the changes in teeth positions during orthodontic treatment.
Keywords: Palatal rugae, stability, forensic identification
INTRODUCTION
Transverse palatine folds or palatal rugae (PR), are asymmetrical and irregular elevations of the mucosa in the anterior third of the palate, arranged in a transverse direction from the palatine raphe located in the mid-sagittal plane. (1-3) The rugae play an important role in forensics, as they are protected from trauma and high temperatures due to their internal position in the oral cavity, surrounded and protected by lips, cheeks, tongue, teeth and bone.
Studies undertaken to determine the thermal effects and the decomposition changes on the palatal rugae have concluded that most burn victims with panfacial third degree burns did not sustain any palatal rugae pattern changes, and when changes were noted, they were less pronounced than the generalized body state. (4) Rugae have been used in medico-legal identification processes because their individual morphological characteristics are stable over time. (1-3) Palatal rugae appear during the third month of intrauterine life from the connective tissue covering the palatine process of the maxillary bone. The growth and development is controlled by epithelialmesenchymal interactions, where specific extracellular matrix molecules are spatiotemporally expressed during development. (5)
Various investigators have implied that palatal rugae are unique to each individual and they can be used successfully in human identification. However, researchers have disagreed as to whether or not legal identification could be based solely on palatal rugae. Controversy also exists about the stability of quantitative and qualitative characteristics of rugae during growth. English et al (2) and Peavy and Kendrick (6) noted that the characteristic pattern of the palatal rugae did not change as a result of growth, remaining stable from the time of development until the oral mucosa degenerated at death. Van der Linden proved that the anterior rugae do not increase in length after 10 years of age. (7) Also qualitative characteristics such as shape, direction and unification remain stable throughout life. (2) However, Hauser et al have suggested that the mean ruga count changes moderately in adolescence and then increases markedly from the age of 35 to 40 years. (8) In contrast, Lysell considered that the number of ruga decreased from 23 years of age onwards. (9) Some events can contribute to changes in rugae pattern, including trauma, extreme finger sucking in infancy, and persistent pressure with orthodontic treatment and dentures. (9) It has been suggested that changes in the length of rugae with age result from underlying palatal growth. (8-10)
Furthermore, Bailey et al, Almeida et al and Abdel-Aziz et al concluded that movement of teeth may change the position of the rugae points. (11-13)
Very few studies have been undertaken to establish the reliability of palatal rugae pattern in individual identification which could play a very important role in forensic sciences. However, rugoscopy can be applicable for forensic identification only when there is available antemortem information for comparison such as dental casts, tracings or digitized rugae patterns. Previous studies may not have considered the effects of growth, extractions, palatal expansion, or some combination of these. The inadvertent use of other features of the cast, such as teeth, edentulous ridge morphology, muscle attachments, vestibular depth, or some combination of these, to aid in the identification, may have influenced their results. Thus the present study will evaluate accuracy of identification by comparing the rugae patterns on pre-operative and postoperative orthodontic casts overcoming these limitations. The purpose of this investigation is to determine if palatal rugae can be relied upon for identification of the individual and whether it can play a definite role in forensic science.
MATERIAL AND METHODS
To determine whether the pattern of the palatal rugae were affected by orthodontic therapy, one hundred and fifty maxillary casts were collected from various private Orthodontist practitioners, out of which 50 orthodontic cases were selected with pre- and post-treatment maxillary dental casts of patients (21 males and 29 females) ranging from 18 to 27 years. All patients had permanent dentitions at the beginning of treatment. 40 patients had extraction of two maxillary premolars and were treated with fixed orthodontic appliances with subsequent retraction of the maxillary anterior teeth into the extraction spaces. 10 patients had no history of extraction and were treated by conventional edgewise techniques. The duration of treatment varied from 8-30 months. All the initial impressions, which were taken from the orthodontic patients, were made from alginate impression materials and the casts were made from hard dental stone at each of the dental clinics and laboratories.
Cast analysis:
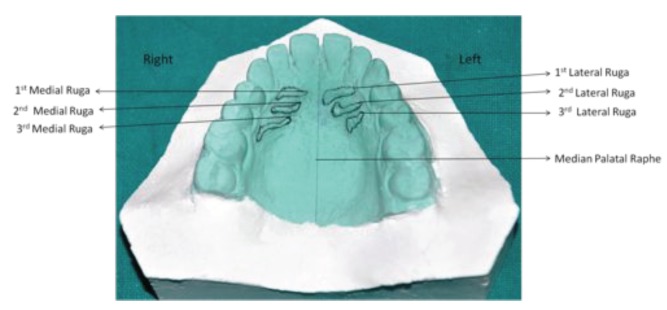
Landmarks on the palatal raphe and palatal rugae were marked on the maxillary casts using a 0.3 mm graphite pencil under adequate light and magnification according to the classification given by Kapali et al (14) (Fig.1). Medial and lateral points were marked on medial and lateral ends of first, second and third rugae. Each cast was photographed by a standardized technique using a tripod mounted SLR digital camera (Nikon D90) with uniform settings and measurements were made using the UTHSCSA Image Tool version 2.0 computer program. The median palatal plane was constructed on the median palatal raphe (MPP). Perpendicular distances from MPP to the rugae points were calculated on each cast. Additionally, transverse linear distances between medial points and between lateral points of the right and left rugae of the first, second and third rugae were calculated. Further, the linear antero-posterior (AP) distances between the medial and between lateral points of all these three rugae types were also individually evaluated. These measurements were compared between the initial (pre-treatment casts) and final records (post-treatment casts).
Fig. 1.
Landmarks on a dental cast, showing 1st, 2nd and 3rd rugae with their medial and lateral points.
Palatal rugae for forensic identification; collection of data:
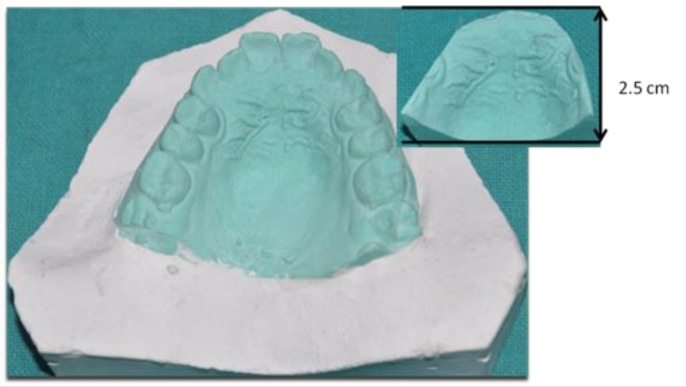
Fifty post-orthodontic casts were dispersed with 50 randomly selected casts which acted as variables. All casts were trimmed so that all areas except for the rugae area of the hard palate are removed. All one hundred and fifty maxillary casts were trimmed utilizing modification of a manner originally described by English et al. (2) The posterior of the cast was trimmed perpendicular to the base until the cast measured 2.5 cm from the incisive papilla to the posterior. The remaining borders were trimmed to shape the arch form until the teeth and vestibule areas had been removed (Fig.2). These one hundred and fifty casts were divided into two groups. The first group of preorthodontic casts were given a random number; the second group consisted of postoperative casts and randomly selected casts mixed together and numbered randomly. The case numbers of the pre-operative casts with that of matching post-operative dental casts were recorded but were not revealed to the evaluators. Thirty examiners including 5 oral pathologists, 5 orthodontists and 20 dental students were selected as evaluators who were given 50 pre-orthodontic casts and were asked to compare them to the other one hundred casts for possible matches based on rugae pattern.
Fig. 2.
Maxillary cast and trimmed cast. The maxillary casts were trimmed until the casts measured 2.5 cm from the incisive papilla to the posterior, and until the teeth and vestibule region had been removed.
The case numbers that matched correctly were recorded. The percentages of correct matches for each examiner were analyzed. Moreover, we focused on the percentages of correct matches for each case and compared the shapes and patterns of those rugae to find the differences between the cases with low percentages and those with high percentages of correct matches.
Statistical analysis:
The correctness of the match for each examiner was calculated as the percentage of correct matches. The collected data were further analysed using paired t-test to detect any significant differences between the pre- and post-treatment records for the three different groups of measurements. Statistical analysis was performed using SPSS software version 16.
RESULTS
To verify an accuracy of identification based on rugae pattern, we performed the examination of comparing rugae patterns to identify the pairs of pre- and post-treated orthodontic casts (Fig.3). The percentages of correct matches for each examiner ranged from 74-98%. The median percentage was 90%, and the interquartile range was 86–93% (Fig.4).
Fig. 3.

Matching of pre-operative and post-operative casts based on palatal rugae patterns.
Fig. 4.
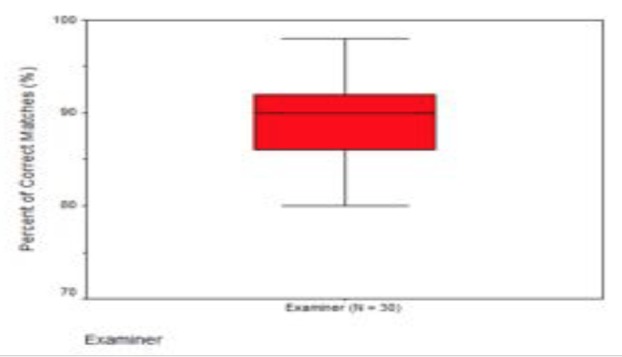
Distribution of the percentage of correct matches for each examiner. The median is indicated with horizontal bar, while the horizontal boundaries of the boxes represent the interquartile ranges and the vertical bar indicates the range. The median (interquartile range) of all examiners was 90% (86–93%).
To examine the indication and the limitations of this method, we analyzed the percentages of correct matches for each case which ranged from 73% to 100%. The median percentage was 90%, and the interquartile range was 87– 93% (Fig.5). We also investigated the morphological features which affected the accuracy of the identification.
Fig. 5.
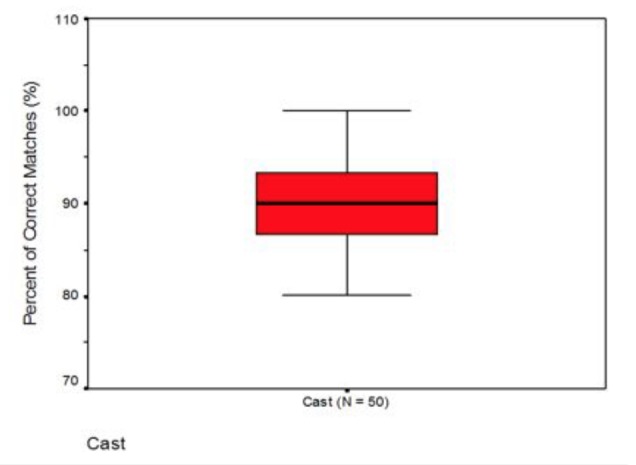
Distribution of the percentage of correct matches for each case. The bars and box indicate the same in Fig. 4. The median (interquartile range) of all cases was 90% (87–93%).
When the pre- and post- transverse linear changes of the rugae points were compared, average change observed over time was statistically significant for the distance between the lateral points of the first rugae (Table 1). The changes observed in the remaining points in the transverse direction were not significantly different between the two groups. Comparison between the pre- and posttreatment changes in the position of palatal rugae points in relation to the median palatal plane also showed a similar result, with significant observable difference regarding lateral points of first left rugae and lateral points of second left rugae (Table 2). When the anteroposterior changes of the rugae points were compared between the pre- and post treatment casts, the average changes were significant for the distances between the lateral points of the first and second left rugae, medial points of first and second right rugae and lateral points of second and third left rugae (Table 3).
Table 1. Descriptive statistics for the transverse changes between bilateral rugae points for pre- and post-treated orthodontic patients.
| VARIABLE | MEAN | SD | MAXIMUM | MINIMUM | ||
|---|---|---|---|---|---|---|
| 1st lateral ruga | Pre | 233.623 | 58.151 | 328 | 108.44 | P<0.05 |
| Post | 250.965 | 42.240 | 307 | 151.2 | ||
| 1st medial ruga | Pre | 57.588 | 27.098 | 110.07 | 16.16 | P>0.05 |
| Post | 58.556 | 20.473 | 88.77 | 26.83 | ||
| 2nd lateral ruga | Pre | 276.434 | 39.220 | 333.49 | 226.04 | P>0.05 |
| Post | 276.296 | 36.177 | 330.49 | 232.31 | ||
| 2nd medial ruga | Pre | 73.533 | 41.89 | 153.69 | 22 | P>0.05 |
| Post | 78.59 | 31.65 | 146.51 | 36.89 | ||
| 3rd lateral ruga | Pre | 297.47 | 69.98 | 401.17 | 143.07 | P>0.05 |
| Post | 318.71 | 32.23 | 383.54 | 273.09 | ||
| 3rd medial ruga | Pre | 140.18 | 57.87 | 214.22 | 66.31 | P>0.05 |
| Post | 149.98 | 55.83 | 222.14 | 75.18 |
Values are expressed in pixels. SD= standard deviation.
Table 2. Descriptive statistics for the transverse changes between bilateral rugae points in relation to the median palatal plane for pre- and post-treated orthodontic patients.
| VARIABLE | MEAN | SD | MAXIMUM | MINIMUM | ||
|---|---|---|---|---|---|---|
| 1st lateral left ruga | Pre | 120.56 | 8.85 | 166.01 | 106.92 | P<0.05 |
| Post | 139.51 | 18.26 | 150.12 | 74.73 | ||
| 1st medial left ruga | Pre | 23.70 | 14.69 | 58.14 | 7.07 | P>0.05 |
| Post | 26.04 | 14.02 | 56.47 | 11 | ||
| 1st lateral right ruga | Pre | 122.33 | 13.35 | 136.53 | 110.03 | P>0.05 |
| Post | 144.52 | 17.28 | 155.08 | 124.58 | ||
| 1st medial right ruga | Pre | 33.49 | 15.43 | 50.36 | 20.1 | P>0.05 |
| Post | 24.75 | 3.05 | 28.07 | 22.09 | ||
| 2nd lateral left ruga | Pre | 142.83 | 24.81 | 171.42 | 127.01 | P<0.05 |
| Post | 131.95 | 22.82 | 158.2 | 116.84 | ||
| 2nd medial left ruga | Pre | 49.05 | 20.07 | 64.28 | 26.31 | P>0.05 |
| Post | 46.01 | 16 | 62 | 30 | ||
| 2nd lateral right ruga | Pre | 121.47 | 34.32 | 160.05 | 94.34 | P>0.05 |
| Post | 136.7 | 27.57 | 168.01 | 116.07 | ||
| 2nd medial right ruga | Pre | 46.86 | 46.99 | 100.3 | 12 | P>0.05 |
| Post | 44.70 | 40.98 | 92 | 20 | ||
| 3rd lateral left ruga | Pre | 177.06 | 22.43 | 202.16 | 159 | P>0.05 |
| Post | 157.49 | 30.29 | 192.17 | 136.24 | ||
| 3rd medial left ruga | Pre | 91.46 | 6.19 | 98.18 | 86 | P>0.05 |
| Post | 94.13 | 3.37 | 98.02 | 82.02 | ||
| 3rd lateral right ruga | Pre | 169.38 | 12.99 | 162.01 | 122.07 | P>0.05 |
| Post | 173.43 | 15.98 | 190 | 158.11 | ||
| 3rd medial right ruga | Pre | 79.38 | 54.29 | 130.06 | 22.09 | P>0.05 |
| Post | 75.54 | 46.44 | 106.02 | 22.09 |
Values are expressed in pixels. SD= standard deviation.
Table 3. Descriptive statistics for the anteroposterior changes between rugae points for pre- and post-treated orthodontic patients.
| VARIABLE | MEAN | SD | MAXIMUM | MINIMUM | ||
|---|---|---|---|---|---|---|
| 1st -2nd lateral left ruga | Pre | 72.42 | 24.85 | 103.48 | 25.5 | P<0.05 |
| Post | 54.25 | 22.53 | 117.38 | 41.23 | ||
| 1st -2nd medial left ruga | Pre | 60.85 | 22.41 | 94.11 | 23.6 | P>0.05 |
| Post | 57.41 | 18.50 | 81.86 | 25.52 | ||
| 1st -2nd lateral right ruga | Pre | 51.57 | 13.31 | 59.93 | 36.22 | P>0.05 |
| Post | 52.99 | 10.21 | 59.61 | 41.23 | ||
| 1st -2nd medial right ruga | Pre | 53.14 | 27.76 | 75.29 | 22 | P<0.05 |
| Post | 71.18 | 30.77 | 96.04 | 36.77 | ||
| 2nd-3rd lateral left ruga | Pre | 80.25 | 34.52 | 137.36 | 27.66 | P<0.05 |
| Post | 59.70 | 36.92 | 151.94 | 23.32 | ||
| 2nd-3rd medial left ruga | Pre | 66.53 | 13.95 | 90.44 | 42.43 | P>0.05 |
| Post | 64.71 | 10.92 | 82.61 | 45.61 | ||
| 2nd-3rd lateral right ruga | Pre | 70.24 | 31.52 | 91.76 | 34.06 | P>0.05 |
| Post | 61.69 | 15.02 | 71.69 | 44.41 | ||
| 2nd-3rd medial right ruga | Pre | 72.34 | 11.58 | 82.37 | 59.67 | P>0.05 |
| Post | 88.82 | 36.82 | 130.3 | 60 |
Values are expressed in pixels. SD= standard deviation.
DISCUSSION
In the present study, the rugae points were unstable in the transverse direction with respect to the lateral points of the first rugae. These results concurred with Bailey et al (12) who believed that extraction of the first premolars creates a large space for distal retraction of the maxillary anterior teeth, which affect the positions of the lateral points of the first rugae thus changing the transverse distance between them. These features were first noticed, by Peavy and Kendrick, (6, 9, 12, 15) who said "the closer the rugae are to the teeth, the more prone they are to stretch in the direction that their associated teeth move". These findings were also consistent with those of Van der Linden (7) and Almeida et al (11) who also observed the influence of orthodontic treatment on the positions of the lateral rugae points. None of the medial points of the first rugae were affected for the transverse values. This finding is in congruence with previous studies by Housser, (16, 17) who concluded that lateral edges of the rugae move forward with the migration of teeth in extraction cases but felt that the medial ruga points were unaffected. There were no significant changes in transverse values for the medial and lateral points of the second and third rugae. This may be due to a decrease in arch circumference, which primarily affects the anterior part of the palate. (12)
It was also found in the present study that anteroposterior changes were significantly different for distances between lateral points of the first and second left rugae, between second and third left rugae and between the medial points of first and second right rugae, thus suggesting that that space closure has some effect on the stability of the rugae. These findings concur with Bailey et al (12) who concluded that the extraction of two premolars creates space for distal retraction of the maxillary anterior teeth, which could lead to these changes in anteroposterior values.
Another interesting finding which was found in the present study was the stability of all the measurements of third rugae which could be due to their position near the molar region away from the distal retraction of anterior teeth. Therefore, these points might serve as stable references when evaluating orthodontic treatment as they did not depend on retraction of anterior teeth. These results were consistent with those of Schwarze, (18) who advocated the use of posterior medial rugae points in the evaluation of anteroposterior changes of buccal teeth and Paevy and Kendrick (6) who concluded that these rugae were not appreciably altered after orthodontic treatment. It has been said that the more posterior rugae are less susceptible to changes with tooth movement: the third palatal rugae pair in particular being the most stable reference. (9, 13)
On matching of preoperative and post operative casts based on palatal rugae patterns, 30 examiners achieved 90% correct matches as the median in the present study and percentage of correct matches ranged from 74-98% which is in congruence with the results of the following published reports. English et al, (2) who examined the accuracy of identification using essentially the same method as used in the current study, reported that the percentage of correct matches was 100% based on four investigators and two teams, the exception being 88% for one investigator. Limsons and Julian, (4) who compared some points of the rugae patterns using computer software, reported that the percentage of correct matches ranged from 92 to 97% based on four computer operators. Maki Ohtani et al (19) explored the accuracy of using the palatal rugae pattern in forensic practice for personal identification in edentulous cases, and suggested 94% correct matches. Furthermore, in the present study, most of the examiners matched the casts with a high accuracy, in spite of variations in their knowledge regarding oral anatomy and in their experience with forensic identification. With regard to the indication and the limitations of this method, the median of the percentages correctly matched for each case was found to be 90%. These results suggest the usefulness and easy reproducibility of comparing palatal rugae patterns for personal identification of cases. In cases where post-mortem dental identification is difficult as in edentulous patients, rugae pattern can be used as a supplement. Limitations of palatoscopy are that post-mortem identification is not possible without antemortem data. Additionally, complex rugae patterns can cause intra and interobserver errors. Kapali et al have stated that dentures, malpositioned teeth and palatal pathologies can cause alterations in rugae patterns. (14) The matching of pre-operative and post-operative orthodontic casts demonstrated that the changes occurring following extractions and tooth movement did not significantly alter the pattern of rugae. Although some changes do occur in the rugae during orthodontic treatment, the morphology of palatal rugae remains stable throughout life. Hence the pattern of palatal rugae is unique to each individual and that it can therefore be used in establishing identity.
CONCLUSION
Orthodontic treatment and tooth movement have a significant effect on the stability of first and second palatal rugae as concluded by previous investigators. The most reliable points which remain stable over a person's life were the medial and lateral third rugae points and these could be used as reference points to evaluate the dental movements. For future studies it would be beneficial to use a larger sample size and wider age range. Although some changes do occur in the rugae during orthodontic treatment the morphology of palatal rugae remains stable throughout life and may be important for identification where there is antemortem information available for comparison.
REFERENCES
- 1.Patil MS, Patil SB, Acharya AB. Palatine rugae and their significance in clinical dentistry: a review of the literature. J Am Dent Assoc. 2008;139:1471–8. 10.14219/jada.archive.2008.0072 [DOI] [PubMed] [Google Scholar]
- 2.English WR, Robison SF, Summitt JB, Oesterle LJ, Brannon RB, Morlang WM. Individuality of human palatal rugae. J Forensic Sci. 1988;33:718–26. 10.1520/JFS12479J [DOI] [PubMed] [Google Scholar]
- 3.Caldas IM, Magalhaes T, Afonso A. Establishing identity using cheiloscopy and palatoscopy. Forensic Sci Int. 2007;165:1. 10.1016/j.forsciint.2006.04.010 [DOI] [PubMed] [Google Scholar]
- 4.Limson KS, Julian R. Computerized recording of the palatal rugae pattern and an evaluation of its application in forensic identification. J Forensic Odontostomatol. 2004;22:1–4. [PubMed] [Google Scholar]
- 5.Amasaki H, Ogawa M, Nagasao J, Mutoh K, Ichihara N, Asari M, et al. Distributional changes of BrdU, PCNA, E2F1 and PAL31 molecules in developing murine palatal rugae. Ann Anat. 2003;185:517–23. 10.1016/S0940-9602(03)80116-4 [DOI] [PubMed] [Google Scholar]
- 6.Peavy DC, Jr, Kendrick GS. The effects of tooth movement on the palatine rugae. J Prosthet Dent. 1967;18:536–42. 10.1016/0022-3913(67)90219-3 [DOI] [PubMed] [Google Scholar]
- 7.van der Linden FP. Changes in the position of posterior teeth in relation to ruga points. Am J Orthod. 1978;74:142. 10.1016/0002-9416(78)90081-7 [DOI] [PubMed] [Google Scholar]
- 8.Hauser G, Daponte A, Roberts MJ. Palatal rugae. J Anat. 1989;165:237–49. [PMC free article] [PubMed] [Google Scholar]
- 9.Lysell L. Plicae palatinae transversae and papilla incisiva in man; a morphologic and genetic study. Acta Odontol Scand. 1955;13:5–137. [PubMed] [Google Scholar]
- 10.Simmons JD, Moore RN, Erickson LC. A longitudinal study of anteroposterior growth changes in the palatine rugae. J Dent Res. 1987;66:1512–5. 10.1177/00220345870660092001 [DOI] [PubMed] [Google Scholar]
- 11.Almeida MA, Phillips C, Kula K, Tulloch C. Stability of the palatal rugae as landmarks for analysis of dental casts. Angle Orthod. 1995;65:43–8. [DOI] [PubMed] [Google Scholar]
- 12.Bailey LT, Esmailnejad A, Almeida MA. Stability of the palatal rugae as landmarks for analysis of dental casts in extraction and nonextraction cases. Angle Orthod. 1996;66:73–8. [DOI] [PubMed] [Google Scholar]
- 13.Abdel-Aziz HM, Sabet NE. Palatal rugae area: a landmark for analysis of pre- and post-orthodontically treated adult Egyptian patients. East Mediterr Health J. 2001;7:60–6. [PubMed] [Google Scholar]
- 14.Kapali S, Townsend G, Richards L, Parish T. Palatal rugae patterns in Australian aborigines and Caucasians. Aust Dent J. 1997;42:129–33. 10.1111/j.1834-7819.1997.tb00110.x [DOI] [PubMed] [Google Scholar]
- 15.Hoggan BR, Sadowsky C. The use of palatal rugae for the assessment of anteroposterior tooth movements. Am J Orthod Dentofacial Orthop. 2001;119:482–8. 10.1067/mod.2001.113001 [DOI] [PubMed] [Google Scholar]
- 16.Hausser E. Relation between the palatine ridges and the teeth. Dtsch Zahnarztl Z. 1950;5:879–84. [contd.] [PubMed] [Google Scholar]
- 17.Hausser E. The palatal ridges in man; their significances and their modifications. Stoma (Heidelb). 1951;4:3–26. [PubMed] [Google Scholar]
- 18.Schwarze CW. Long-time study on the sagittal position of the 1st molars. Fortschr Kieferorthop. 1972;33:93–102. 10.1007/BF02170669 [DOI] [PubMed] [Google Scholar]
- 19.Ohtani M, Nishida N, Chiba T, Fukuda M, Miyamoto Y, Yoshioka N. Indication and limitations of using palatal rugae for personal identification in edentulous cases. Forensic Sci Int. 2008;176:178–82. 10.1016/j.forsciint.2007.09.002 [DOI] [PubMed] [Google Scholar]