Highlights
-
•
Airway management during surgical repair of iatrogenic tracheal injury can be difficult.
-
•
ECMO has emerged as a valid tool to maintain adequate oxygenation during tracheal surgery.
-
•
Veno-venous ECMO allows a safer peri and intraoperative management of iatrogenic tracheal injuries.
Keywords: ECMO, Tracheal perforation, Case report
Abstract
Introduction
Extracorporeal membrane oxygenation (ECMO) is used extensively in cardiothoracic surgery both for hemodynamic and respiratory support. It has proven to be a valuable tool to maintain adequate oxygenation during tracheal surgery. Airway lesion may be an indication for veno-venous ECMO both in case of conservative management and in case of surgical repair. Here we report the case of a patient with a iatrogenic tracheal injury, successfully operated with the support of veno-venous extracorporeal oxygenation.
Presentation of case
A 39-year-old female underwent an elective laparoscopic adhesiolysis. At the end of the procedure, the patient had developed subcutaneous emphysema. A CT-scan showed mediastinal and subcutaneous emphysema and left pneumothorax with a laceration of the membranous portion of the middle third of the trachea.
A left pleural drain was inserted and a bronchoscopy showed a 2-cm long tear of the membranous portion in the middle third of the trachea.
Veno-venous ECMO was established and surgical repair of the tracheal lesion was performed. Post-operative recovery was uneventful and the patient was discharged on 8th postoperative day.
Discussion
The use of Veno-venous ECMO allowed a safe intubation with optimal oxygenation. A selective intubation with a small tube was performed to prevent further tracheal injury and allow an adequate surgical space for tracheal repair.
Conclusion
The use of ECMO support represents a safe and effective way to manage patients with ITI when surgical repair with minimally invasive ventilation is needed.
Since this is a case report larger studies are needed to validate the technique.
1. Introduction
Iatrogenic tracheobronchial injuries (ITI) are rare events but they are associated with high morbidity if not promptly diagnosed and treated. The incidence rate of ITI is 1 event every 20.000–75.000 elective orotracheal intubations, while in the emergency setting the occurrence of ITI increases up to 15% [1]. Management of ITI can be conservative or surgical. Although the conservative approach may be successful in selected patients, complications such as mediastinitis, sepsis or sudden tracheal obstruction can occur, as well as a higher risk of tracheal stenosis in the late phase. In case of tracheal lesions longer than 1 cm and located in the lower trachea, a surgical approach is recommended [2]. Currently, veno-venous extracorporeal membrane oxygenation (VV-ECMO) is recognized as an effective supportive therapy in patients with respiratory failure which is refractory to conventional ventilation [3]. In the setting of ITI, VV-ECMO could be used to minimize the adverse effects of positive pressure ventilation on tracheal leakage and/or allow surgical repair by providing a constant and adequate oxygenation [3], [4]. Thus, we report the case of a patient with a lower ITI which was surgically treated under VV-ECMO support.
The work has been reported in line with the SCARE criteria. [5]
2. Presentation of case
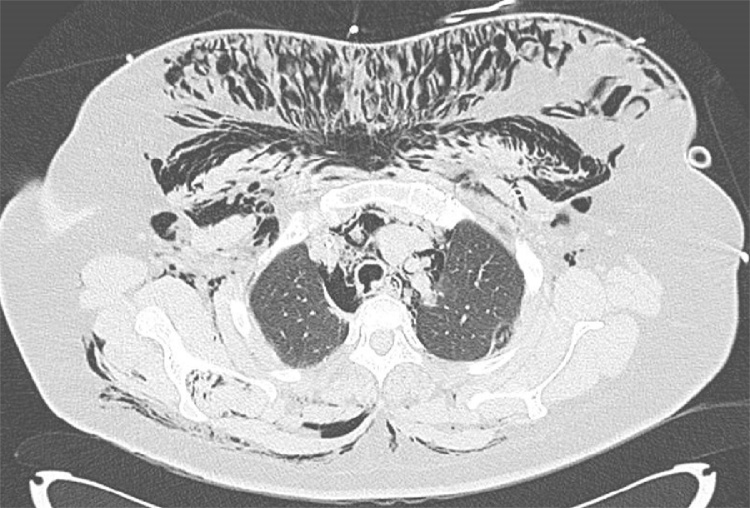
A 39-year-old female with a history of obesity, hypertension, gastro-esophageal reflux disease and Hashimoto’s thyroiditis underwent an elective laparoscopic adhesiolysis. At the end of the procedure, the patient was extubated and subcutaneous emphysema at the trunk and face was observed. A CT-scan showed mediastinal and subcutaneous emphysema and left pneumothorax with a laceration of the membranous portion of the middle third of the trachea (Fig. 1). The patient was then referred to our hospital (academic institution) for further treatment.
Fig. 1.
Pre-operative chest CT-scan showing the perforation of the posterior wall of the trachea, mediastinal emphysema and subcutaneous emphysema.
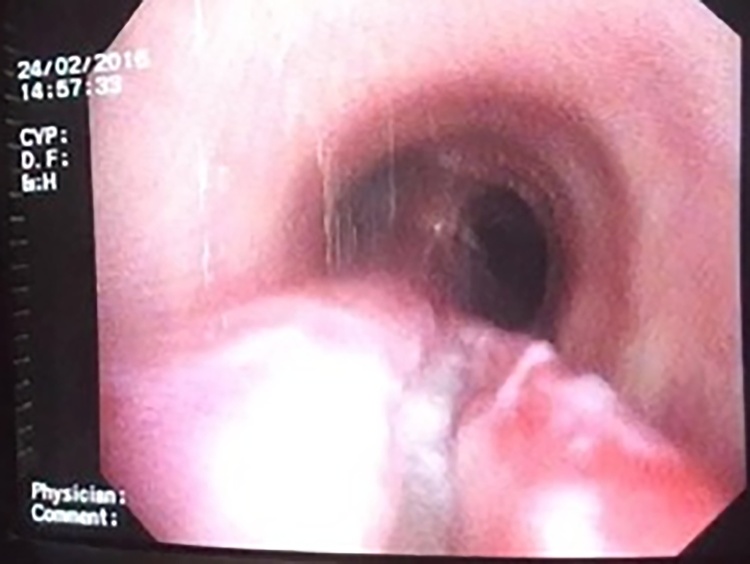
On Intensive Care (ICU) arrival, the patient was on spontaneous breathing, with an oxygen saturation of 95% under nasal oxygen therapy (8 L/min). A left pleural drain was inserted and a bronchoscopy showed a 2-cm long tear of the membranous portion in the middle third of the trachea; through the injury, mediastinal fatty tissue was visible (Fig. 2). Surgical repair was then indicated. However, considering the difficult airway management during surgery, the patients was put on VV-ECMO. No anticoagulation was required, since a short-time ECMO was planned and a heparin-coated circuit was used. The right jugular and right femoral veins were cannulated using the Seldinger technique under ultrasound guidance, using a 20-Fr and 25-Fr cannula, respectively. VV-ECMO was started before orotracheal intubation with a blood flow of 4 L/min and FiO2 of 70%. Afterward, selective intubation of the left bronchus with a single lumen 5-mm tube was performed in order to allow an easier surgical procedure.
Fig. 2.
Bronchoscopy showing the 2-cm tear lesion of the posterior wall of the trachea and mediastinal fatty tissue visible through the laceration.
A right posterolateral thoracotomy was performed and an intercostal vascularized muscular flap was prepared. After ligation of the azygous vein, the mediastinal pleura was opened and the ITI of the membranous portion in the middle third identified. The lesion was repaired and the suture protected with the muscular flap. At the end of the procedure the patient was extubated and gradually weaned from VV-ECMO within 5 h. The procedure was performed by two trained thoracic surgeons (G.O. and F. A.) and by a trained cardiac surgeon (C.P.).
Post-operative recovery was uneventful, a bronchoscopy done on the seventh postoperative day and a chest CT-scan performed done on the eleventh post-operative day showed good healing of the lesion without remarkable tracheal narrowing (Fig. 3).
Fig. 3.
Post-operative chest CT-scan showing the intercostal vascularized muscular flap transposed to protect the suture of the trachea.
3. Discussion
There is limited literature reporting the use of VV-ECMO during surgical repair of ITI. Son et al. [3] reported a case of conservatively managed ITI in a patient on spontaneous breathing and concomitant VV-ECMO for 28 days, while two other studies reported cases of surgical repair of tracheal and bronchial injuries under VV-ECMO therapy [6], [7]. Compared to our experience, the two cases urgently required VV-ECMO because of severe hypoxemia and ineffective mechanical ventilation. Literature regarding VV-ECMO implementation in case of at-risk thoracic surgery is limited and mainly concerns neonatal population rather than adults [7], [8].
The most common technique to maintain intraoperative oxygenation during tracheal surgery is cross-table ventilation. Anyway tubes and lines in the operation field may impair surgical access and visibility. Moreover extended retraction manoeuvres of the mediastinum, leading to haemodynamic stability, can be necessary in order to obtain better exposure. An established alternative to ventilation in such situation are cardiopulmonary bypass or ECMO [8].
Common complication of cardiopulmonary bypass following complex thoracic surgery procedures are bleeding due to systemic anticoagulation and intraoperative pulmonary edema [8], [9].
The use of ECMO instead of standard cardio-pulmonary bypass technique in tracheal surgery is supported by the lack of full anticoagulation therapy and less fluid overload due to haemodilution.
Tomasko and Bharat have reported cases of patients on ECMO as a bridge to lung transplantation managed without full anticoagulation [10], [11].
In our case, the choice of VV-ECMO allowed a safer intubation with optimal oxygenation, as a selective intubation with a small 5-mm tube was performed to prevent further tracheal injury and allow an adequate surgical space for tracheal repair. Moreover heparin was not administered since we planned to keep the VV-ECMO for the time of surgery.
Of course, considering the invasiveness of the procedure, future alternatives, including extracorporeal carbon dioxide removal (ECCO2R) systems, should also be tested in those patients with minimal oxygenation problems and a more complete assessment of potential side effects, such as post-ECMO venous thrombosis or vascular injuries, need to be evaluated in larger cohorts.
4. Conclusion
The advantage of using VV-ECMO compared to conventional ventilation during tracheal surgery was the use of a selective small ventilation catheter allowing better surgical access and visibility.
Though this is a single case experience, the use of ECMO support showed to be a safe and effective way to manage patients with ITI when surgical repair with minimally invasive ventilation is needed.
ECMO can be a valid tool in similar situations but larger studies are needed to confirm these promising results.
Conflicts of interest
Nothing to declare.
Sources of funding
Nothing to declare.
Ethical approval
In our institution we are exempted to require ethical approval for publication of clinical case/series.
Our ethic committee only require written informed consent for publication.
Consent
Written informed consent was obtained from the patient for publication of data and images.
Author contribution
Filippo Antonacci and Mirko Belliato designed the study, interpreted data, wrote the paper.
Chiara De Tisi and Ilaria Donadoni collected data and wrote the paper.
Fabio Silvio Taccone interpreted data and wrote the paper.
Giorgio Iotti, Marco Maurelli, Giulio Orlandoni and Carlo Pellegrini designed the study.
Guarantor
ppo Antonacci, Mirko Belliato.
References
- 1.Prokakis C., Koletsis E.N., Dedeilias P., Fligou F., Filos K., Dougenis D. Airway trauma: a review on epidemiology, mechanisms of injury, diagnosis and treatment. J. Cardiothorac. Surg. 2014;9:117. doi: 10.1186/1749-8090-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deja M., Menk M., Heidenhain C. Strategies for diagnosis and treatment of iatrogenic tracheal ruptures. Minerva Anestesiol. 2011;77:1155–1166. [PubMed] [Google Scholar]
- 3.Son B.S., Cho W.H., Kim C.W. Conservative extracorporeal membrane oxygenation treatment in a tracheal injury: a case report. J. Cardiothorac. Surg. 2015;10:48. doi: 10.1186/s13019-015-0252-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasegawa T., Oshima Y., Matsuhisa H., Okata Y., Yokoi A., Yokoyama S., Maeda K. Clinical equivalency of cardiopulmonary bypass and extracorporeal membrane oxygenation support for pediatric tracheal reconstruction. Pediatr. Surg. Int. 2016;32:1029–1036. doi: 10.1007/s00383-016-3921-2. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill and the SCARE Group D.P. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Sian K., McAllister B., Brady P. The use of extracorporeal membrane oxygenation therapy in the delayed surgical repair of a tracheal injury. Ann. Thorac. Surg. 2014;97:338–340. doi: 10.1016/j.athoracsur.2013.04.126. [DOI] [PubMed] [Google Scholar]
- 7.Walker J.L., Wiersch J., Benson C., Young H.a., Dearmond D.T., Johnson S.B. The successful use of cardiopulmonary support for a transected bronchus. Perfusion. 2012;27:34–38. doi: 10.1177/0267659111420321. [DOI] [PubMed] [Google Scholar]
- 8.Lang G., Ghanim B., Hotzenecker K., Klikovits T., Matilla J.R., Aigner C., Taghavi S., Klepetko W. Extracorporeal membrane oxygenation support for complex trachea-bronchial procedures. Eur. J. Cardio-Thorac. Surg. 2015;47:250–256. doi: 10.1093/ejcts/ezu162. [DOI] [PubMed] [Google Scholar]
- 9.Wiebe K., Baraki H., Macchiarini P., Haverich A. Extended pulmonary resections of advanced thoracic malignancies with support of cardiopulmonary bypass. Eur. J. Cardiothorac. Surg. 2006;29(April (4)):571–578. doi: 10.1016/j.ejcts.2005.10.041. (discussion 577–8) [DOI] [PubMed] [Google Scholar]
- 10.Tomasko J., Prasad S.M., Dell D.O., DeCamp M.M., Bharat A. Therapeutic anticoagulation-free extracorporeal membrane oxygenation as a bridge to lung transplantation. J. Heart Lung Transplant. 2016;35(July (7)):947–948. doi: 10.1016/j.healun.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Bharat A., DeCamp M.M. Veno-arterial extracorporeal membrane oxygenation without therapeutic anticoagulation for intra-operative cardiopulmonary support during lung transplantation. J. Thorac. Dis. 2017;9(July (7)):E629–E631. doi: 10.21037/jtd.2017.06.11. [DOI] [PMC free article] [PubMed] [Google Scholar]