Abstract
Study Objectives:
The aim of this study was to investigate the predictors of dental changes associated with long-term treatment with oral appliances (OAs) in patients with obstructive sleep apnea (OSA).
Methods:
This was a retrospective study to investigate Japanese patients with OSA receiving long-term treatment with OAs. Comparisons of cephalometric analysis were carried out between the initial and follow-up assessments of dental and skeletal changes. Based on dental changes, predictors that may cause side effects were investigated.
Results:
A total of 64 patients (average age at start of treatment: 57.7 ± 14.2 years, 44 males) were included in this study. The average duration of treatment was 4.3 ± 2.1 years. Over the total treatment period, there was a significant reduction in overjet (OJ) (1.5 ± 1.3 mm) and overbite (0.90 ± 1.5 mm), and an increase in the lower incisor line to the mandibular plane (3.1 ± 5.4°). A larger reduction in OJ of ≥ 1 mm was associated with treatment duration, use frequency, and mandibular advancement of the OAs. In addition to these predictive factors, the number of teeth was correlated with the amount of OJ reduction.
Conclusions:
For long-term treatment with OAs, the risk of dental side effects should be considered, such as a reduction in OJ. A small number of maxillary teeth, as well as the factors associated with OAs, including treatment duration, use frequency, and mandibular advancement of the OAs, was correlated with an increased rate of OJ reduction.
Commentary:
A commentary on this article appears in this issue on page 7.
Citation:
Minagi HO, Okuno K, Nohara K, Sakai T. Predictors of side effects with long-term oral appliance therapy for obstructive sleep apnea. J Clin Sleep Med. 2018;14(1):119–125.
Keywords: cephalometric analysis, dental side effects, long-term treatment, mandibular advancement devices, oral appliance, sleep apnea, snoring
BRIEF SUMMARY
Current Knowledge/Study Rationale: Oral appliances are an effective treatment option for patients with obstructive sleep apnea, although dental changes may occur. To prevent the side effects of long-term oral appliance treatment, an investigation of the predictors of dental changes is needed.
Study Impact: To more safely and effectively administer long-term oral appliance treatment to patients with obstructive sleep apnea, clarifying the predictors for side effects is important. Our study found several factors that may predict overjet reduction for patients undergoing long-term oral appliance treatment.
INTRODUCTION
Obstructive sleep apnea (OSA) is characterized by recurrent upper airway obstruction during sleep.1 OSA often leads to poor sleep quality and daytime sleepiness, and increases the risk of motor vehicle accidents, stroke, and hypertension.2,3 Oral appliances (OAs), which function to hold the mandible in a forward position and enlarge the airway during sleep, are indicated as a primary treatment option for snoring and mild/ moderate OSA.4 Many studies have indicated a short-term benefit of using OAs for OSA.5 However, past studies suggested that OAs have short-term and long-term side effects such as excess salivation or mouth dryness, and temporomandibular joint and dental discomfort.6–9 Of the side effects, skeletal and dental changes are a serious problem because they are irreversible.10–12
Studies have demonstrated that the dental changes that occur will continue to progress over the duration of treatment.13 For long-term treatment of OAs, changes in overjet (OJ) and overbite (OB), retroclination of the upper incisors, and a proclination of the lower incisors have also been described.14,15 Although not all occlusal changes should be interpreted as unfavorable, dental changes are serious problems for dentists.16 In previous studies, some predictors of side effects with long-term use of OAs were investigated.17,18 For example, a deep bite and the use of a soft elastomeric device provided protection from large reductions in OJ. However, previous studies that reveal predictors used study models that are susceptible to larger random errors than measurements on X-rays. In this study, we investigate dental changes by cephalometric analysis. This is a standard approach to investigate dental and skeletal changes. It is known that patients treated with OAs should be monitored for at least 1 year or longer.19 To prevent the dental side effects of long-term OA treatment, establishing a prediction method and diagnosing indications of side effects are needed. Furthermore, the identification of these side effects may contribute to the development of better devices in the future.
In this study, we have investigated some factors that cause orthodontic changes during the treatment of OSA with OAs by cephalometric analysis. To start, cephalometric changes were analyzed after long-term use of the OAs. Next, to prevent side effects, we evaluated the predictors of dental changes after long-term use of the OAs. Then, we analyzed correlations of predictive factors and OJ reduction. The specific aims of this study were to clarify the magnitude and progression of orthodontic changes associated with long-term OA treatment, as well as to investigate the relationship between the observed changes and the predictors.
METHODS
Study Design
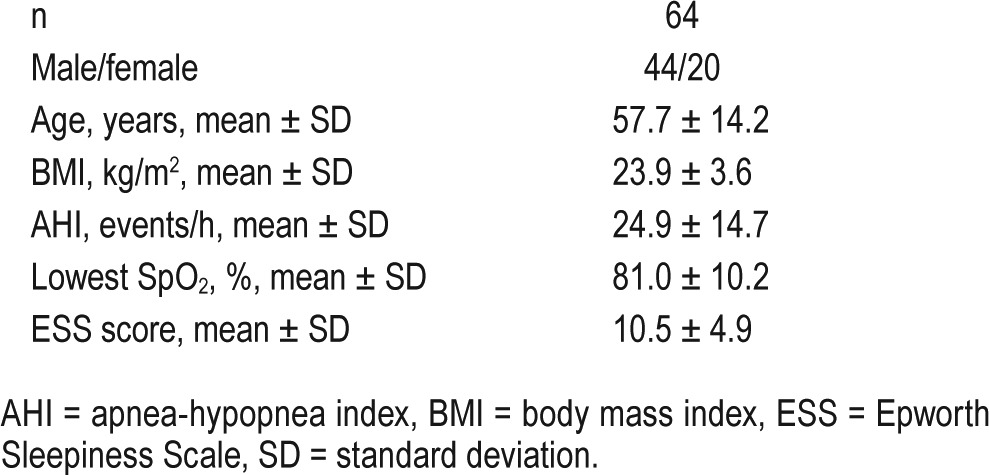
Sixty-four adult patients with OSA were recruited from Osaka University Dental Hospital, Japan, between June 2006 and April 2015. All patients had OSA symptoms (snoring, apnea, and sleepiness), the diagnosis was made by nocturnal polysomnography, used OAs for therapy, and came to Osaka University Dental Hospital for regular follow-ups. Age, body mass index, apnea-hypopnea index (AHI), lowest SpO2, Epworth Sleepiness Scale score, and the number of teeth were obtained from clinical records. The number of teeth included wisdom teeth. The inclusion criteria were as follows: (1) patients had undergone overnight polysomnography as a pretreatment baseline (AHI > 5.0 events/h) in a sleep laboratory at a sleep center; (2) patients were instructed to wear an OA during sleep for more than 5 hours per night and more than 5 nights per week; and (3) patients had worn an OA for at least 1 year. The patients' clinical characteristics are shown in Table 1.
Table 1.
Patients' baseline characteristics.
The design of all OAs is acrylic monoblock. The OAs used in this study are made of two separate parts comprising polyethylene terephthalate glycol modified plates (ERKODRNT, Pfalzgrafenweiler, Germany), fixing the patient's mandible in a forward position. The mandibular protruded positions were titrated as previously described.20 Initially, mandible advancement was set at 60% to 70% of the maximum mandibular protruded position. OAs were incrementally titrated according to either a maximal comfortable protruded position of the mandible or a resolution of snoring and daytime symptoms. Increased advancement of OAs was facilitated by the separation of upper and lower components of OAs, and then repositioning at a more advanced mandibular position. The mandibular advancement was measured with a caliper with a resolution of 0.1 mm by a single investigator. The movement rates were calculated from movement quantity for the quantity of their max forward movement. This research was performed under the approval of the Osaka University Ethics Committee (Osaka University Dental Hospital, No.H28-E20).
Data Analysis
In this study, lateral cephalometric radiographs CX150WT (Asahi, Kyoto, Japan) were obtained to analyze the orthodontic side effects. The film was taken when the patient sat upright with the Frankfort plane parallel to the ground, naturally closed lips, and the bite in intercuspal occlusion with relaxation of the tongue and perioral muscles. Demographic data used in the correlations were collected before OA placement from medical records. The period of OA use was calculated as the interval between the date of appliance placement and the new cephalogram. To analyze the cephalograms, all distances and angles were manually measured by Dolphin Imaging Version 8.0 Software (Dolphin Imaging & Management Solutions, Chatsworth, California, United States). This software uses the indirect digitization of multiple dental and skeletal landmarks of the scanned cephalogram (Figure 1). To minimize identification error, all measurements were performed blindly such that the investigator could not identify names of patients or whether the data was baseline or follow-up. Cephalometric analysis was carried out as previously described.21
Figure 1. Cephalometric landmarks.
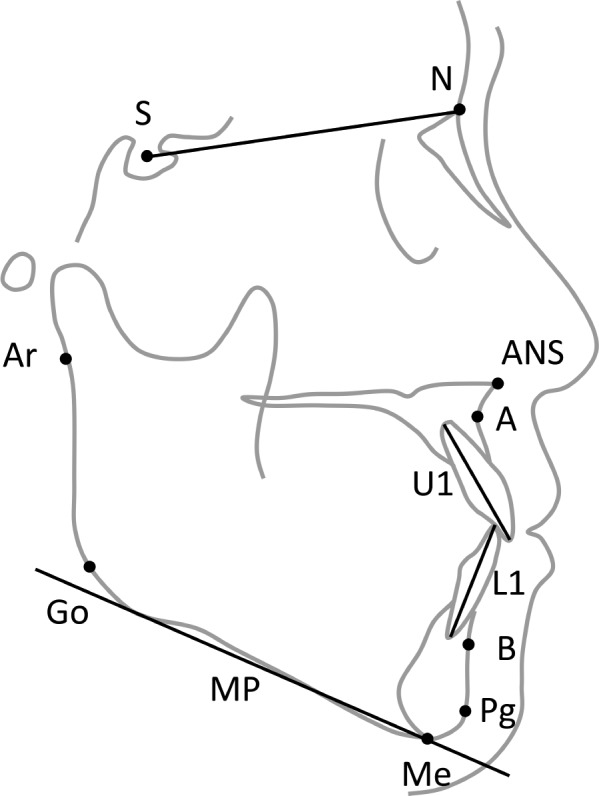
The following points were identified on lateral cephalograms. Points: S (sella) = the midpoint of the pituitary fossa), N (nasion) = the most anterior point on the frontonasal suture, ANS (anterior nasal spine) = the tip of the median, sharp bony process of the maxilla at the lower margin of the anterior nasal opening, A (Point A) = the deepest midline concavity on the anterior maxilla, B (Point B) = the deepest midline concavity on the mandibular symphysis, Pg (pogonion) = the most anterior point on the contour of the bony chin determined by a tangent through the nasion, Me (menton) = the intersection of the bony inferior symphysis with the inferior margin of the mandibular body, Go (gonion) = the constructed point of the intersection of the ramus plane and the tangent to the body of the mandible, Ar (articulare) = the point of intersection of the inferior cranial base surface and the averaged posterior surfaces of the mandibular condyles. Planes: SN (sella-nasion line) = the line through the sella and nasion, MP (mandibular plane according to Steiner) = the line through the gonion and gnathion, U1 (upper incisor line) = the line through the upper incisor apex and the upper incisor incisal edge, L1 (lower incisor line) = the line through the lower incisor apex and the lower incisor incisal edge. Linear measurements: OJ (overjet) = horizontal projection of maxillary teeth beyond the mandibular anterior teeth, usually measured parallel to the occlusal plane, OB (overbite) = vertical overlap of maxillary teeth over mandibular anterior teeth, usually measured perpendicular to the occlusal plane.
Statistical Analysis
The software package SPSS Version 23 (IBM Corp., Armonk, New York, United States) was used for statistical analysis. The data are presented as the mean values and standard deviations. We used the paired t test to compare the averages of continuous variables (such as age) and chi-square tests to compare the proportions of categorical variables (such as sex) between the groups. Spearman rank correlations were used to determine the relationship between the amount of OJ reduction and predictors.
RESULTS
Sixty-four patients were recruited, and had a mean age of 57.7 years (Table 1). The mean follow-up period was 4.3 ± 2.1 years (range 1.0–9.3 years). Patients with mild to severe OSA (range AHI 5.5–66.7 events/h) were included in analysis.
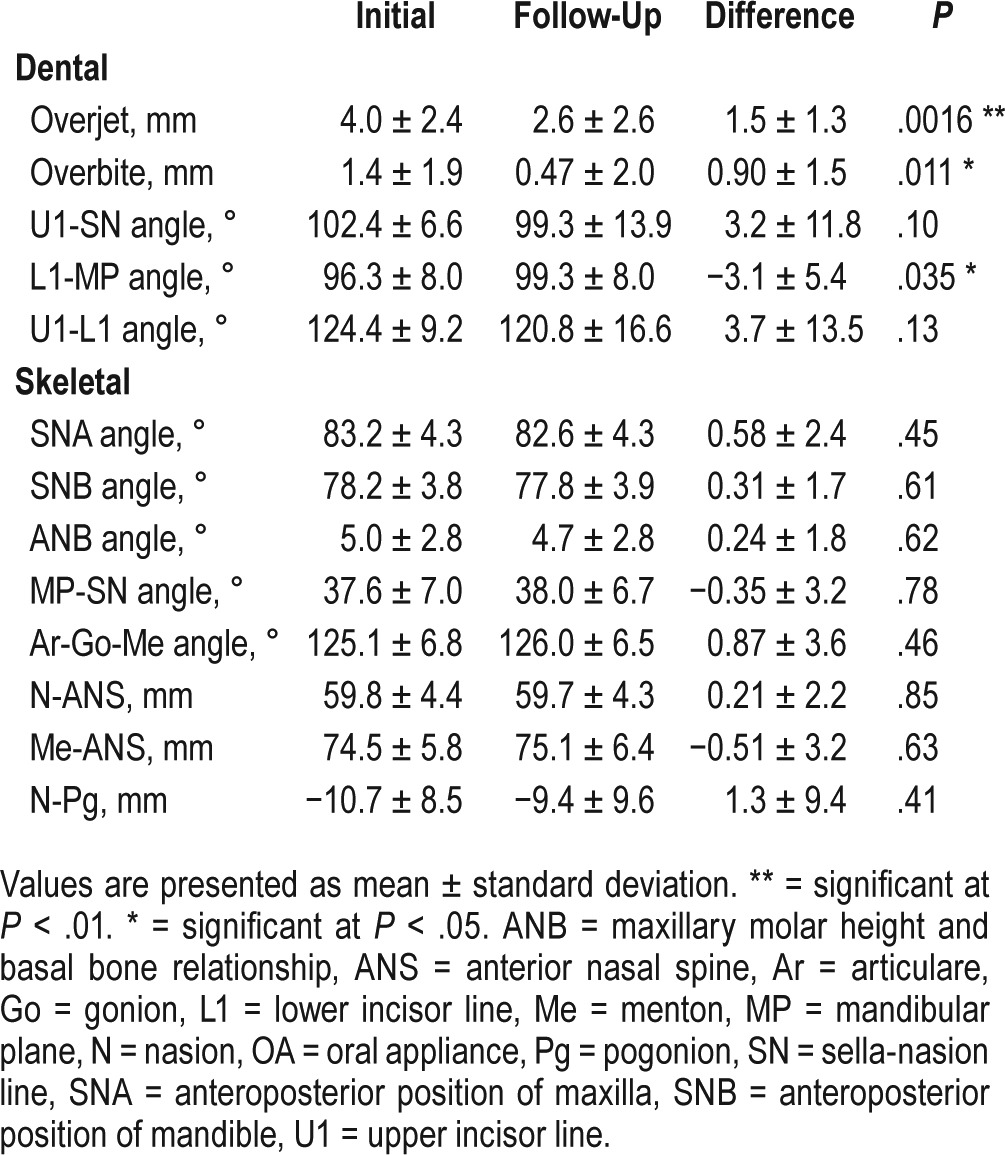
Cephalometric Changes
Dental and skeletal changes after long-term use of the OAs are shown in Table 2. After long-term treatment with OAs, signifi-cant dental changes were observed with decreases in the OJ and OB and increases in the lower incisor line to mandibular plane (L1-MP) angle. The maxillary incisors exhibited significant retroclinations (L1-MP angle difference; 3.1 ± 5.4°). Although it was not significant, the maxilla showed a cetroclination of the incisors (upper incisor line to sella-nasion line [U1-SN] angle difference; 3.2 ± 11.8°). With retroclinations of upper incisors and lower cetroclination, the relationship between maxillary and mandibular incisors statistically differed (OJ difference; 1.5 ± 1.3 mm and OB difference; 0.90 ± 1.5 mm). However, no significant skeletal changes were found after long-term treatment.
Table 2.
Cephalometric changes after long-term treatment with OAs.
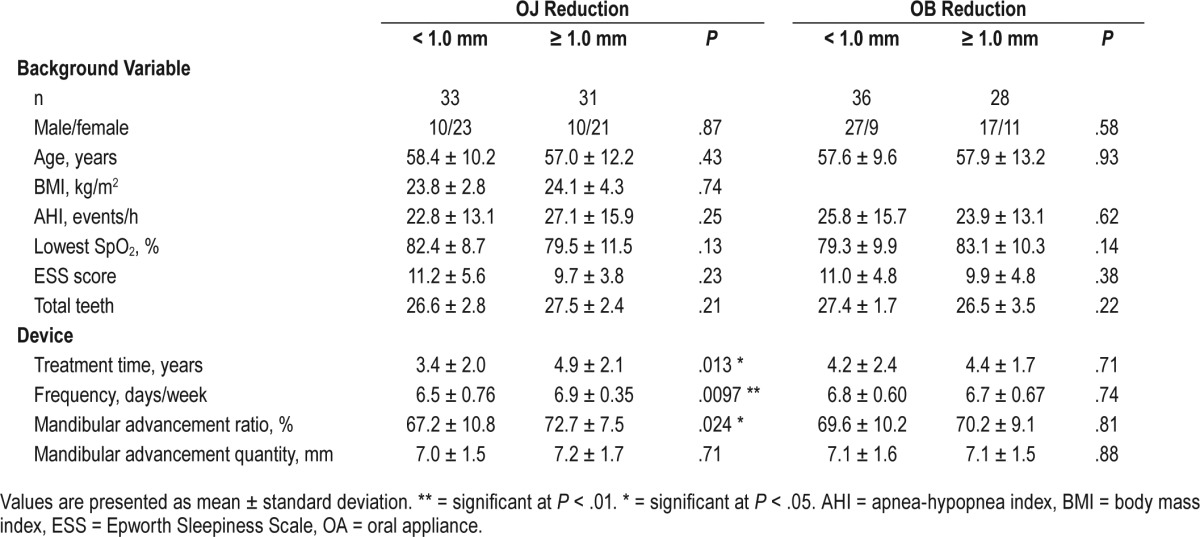
Predictors of Bite Changes
To analyze the predictors of bite changes, we divided subjects into two groups based on amount of change in OJ and OB reductions—no bite change group (< 1.0 mm) and bite change group (≥ 1.0 mm).17 The comparison between the two groups and predictors of bite changes after use of OAs are presented in Table 3. For the background variables of patients, the paired comparisons were not different. In the OJ bite change groups, paired comparisons between the groups demonstrated a meaningful difference for the treatment duration, use frequency, and mandibular advancement rate (%) of OAs. On analysis between the two groups, the mandibular advancement rate was significantly different from the mandibular advancement quantity (mm). In addition, based on OB reduction, there were no predictors that were different between the two groups after long-term use of the OAs.
Table 3.
Predictors of dental changes after long-term treatment of OAs.
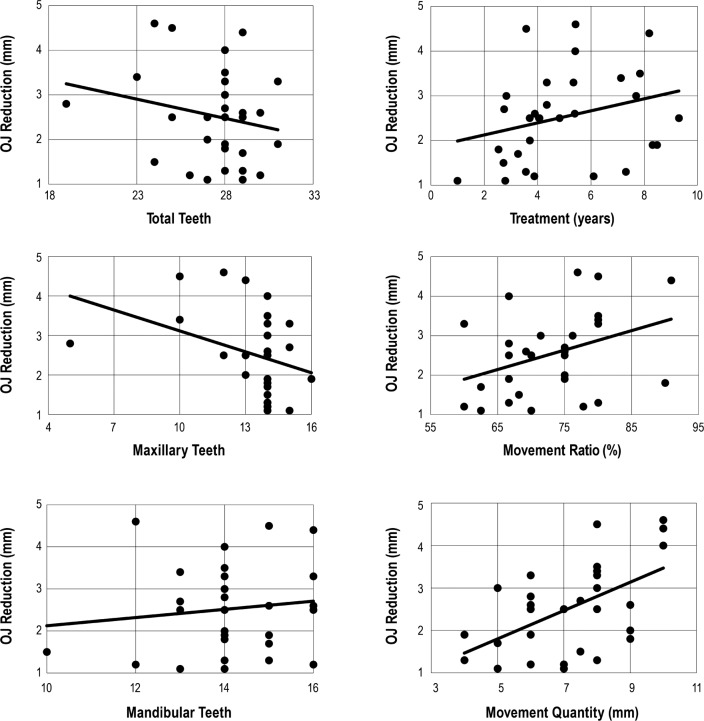
Correlation of OJ Reduction and Predictive Factors
To clarify the relationship between the amount of OJ reduction and predictive factors, we used the Pearson correlation coefficient (Table 4). There was a slight correlation between the treatment duration and mandibular advancement rate and quantity. The amount of mandibular advancement quantity (mm) was higher than the rate of mandibular advancement. The usage frequency demonstrated no correlation because 31 of 32 patients used the OAs every day. There was weak negative correlation regarding the number of teeth, and a negative correlation was found between maxillary teeth and OJ reductions. Figure 2 shows the relationships between OJ reduction and predictors that were correlated.
Table 4.
Correlation of predictive factors and OJ reduction in bite change group.
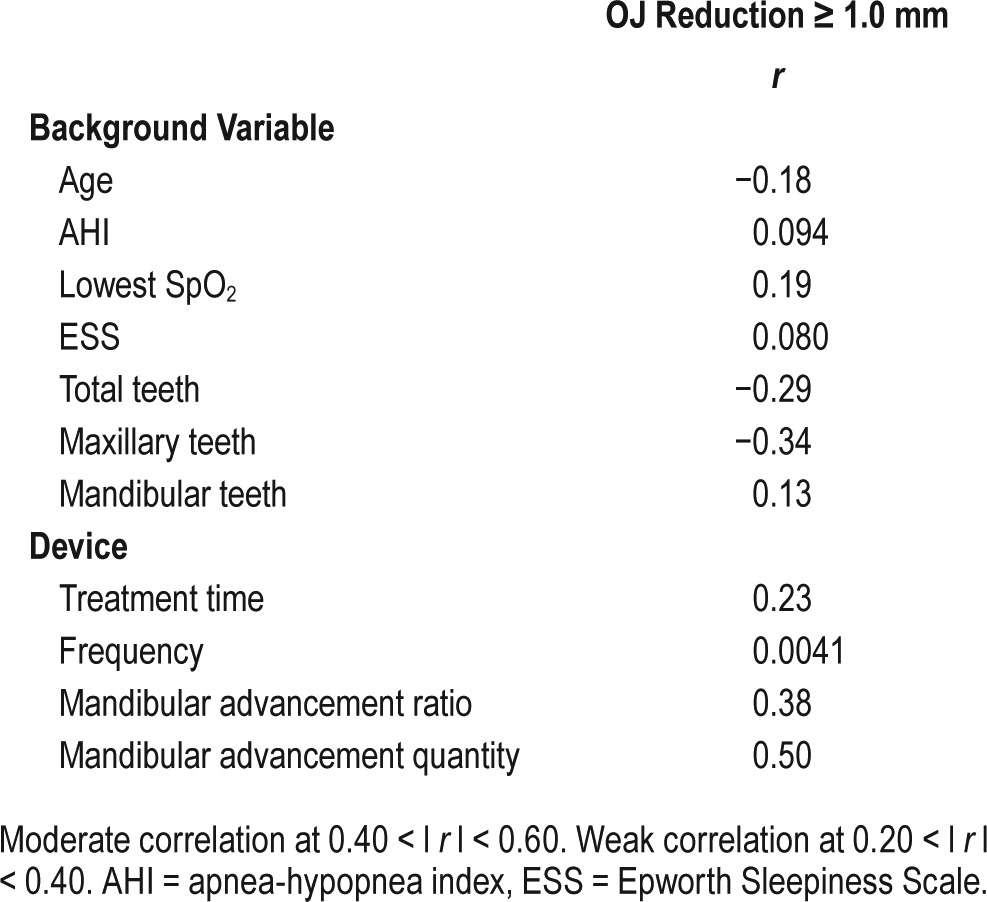
Figure 2. Correlation graphs of predictive factors and OJ reduction in bite changes.
The graphs show the correlation of reduction of OJ (mm) and each predictable factor. OJ = overjet.
DISCUSSION
This study examined patients with OSA who had undergone long-term treatment with OAs in order to find predictive factors of side effects. After long-term treatment with OAs, clinically significant cephalographical changes in occlusion were observed. This study demonstrates that the factors that caused occlusion changes included treatment period, use frequency, and mandibular advancement of OAs. Furthermore, these advancement factors and number of teeth were related to the amount of OJ reduction. To our knowledge, this is the first study reporting that a smaller number of teeth is correlated with an increased rate of change in the OJ.
There are many ways to investigate dental side effects of OAs. Some researchers identified changes in cephalometric analysis, dental model analysis, and occlusal function by a dental prescale occluser system.18,22,23 All analyses are used in many fields of dentistry, but cephalometric analysis is able to reveal skeletal and dental side effects and shows less random errors than analysis by dental casts. Changes in OJ and OB, retroclination of the upper incisors, and a proclination of the lower incisors have also been described in previous studies.24 Using objective cephalometric measurements, OJ and OB were analyzed in previous studies as well.18,25,26 Our results for the devices and the patients were similar to previous study results, and demonstrate that the relationship between maxillary and mandibular incisors changed with retroclinations of upper incisors (U1-SN angle difference; 3.2 ± 11.8°) and cetroclinations of lower incisors (L1-MP angle difference; 3.1 ± 5.4°). The reductions of OJ and OB were also observed (OJ difference; 1.5 ± 1.3 mm and OB difference; 0.90 ± 1.5 mm). These changes have been attributed to a labially directed force to the mandibular incisors and a palatally directed force to the maxillary incisors while the appliance is in place, and the mandible attempts to return to a less constrained position.14,17,18,27 OA mechanisms of action on the dentition may be similar with functional appliances,28 but for only 6 to 8 hours a day. OJ changes were caused by increasing the extent of mandibular advancement. The marked changes we found are opposite to the findings with a Herbst appliance in growing children.28,29 In this study, there were no cephalometric changes in skeletal analysis after long-term treatment with OAs. The OAs for OSA used in adults induced teeth movements but not craniofacial skeletal changes. These findings indicate that OJ and OB were decreased as a result of teeth axis changes.
Although past examinations demonstrated dental changes from OAs in patients with OSA,19,23 there are few studies that report on patients who exhibit dental movement. It is useful to determine the predictors of OA side effects in patients who snore and patients with OSA. To prevent dental side effects, establishment of a method to diagnose indication is needed for patients who undergo long-term OA therapy. Pliska et al. found that reductions of OJ and OB and a long period of treatment caused mandibular intermolar distance changes after an average observation period of over 11 years.13 In our study, a larger reduction in OJ was also associated with treatment duration, usage frequency, and the mandibular advancement rate of OAs by comparison between the bite change and no bite change groups. In the bite change group, most patients used OAs every day. Using OAs every day is beneficial to improve sleep, but regarding side effects, the frequency is an important risk factor. Marklund et al. found that deep bite provided protection against bite change.30 Although differences were observed for OJ, OB showed no statistically significant differences. We found some correlations, none of which were very strong, but we hypothesize that several characteristics are involved, each with a different weight of influence on OB. Although reversed occlusion is expected for patients on OB analysis, there were statistical differences in some predictors (treatment days, frequency). These results suggest that the predictors were masked in OB analysis, and the tendency in OB was considered to be the same as for OJ analysis. Furthermore, as previously demonstrated, OB does not constantly change,23 whereas there are previous studies that supported that OB tended to continue as long as OAs were used.23 We examined predictors in patients who used OAs for a long time, but it is thought that more meaningful results may be provided by longer-term treatment. These findings support our results. We also found that excessive mandibular advancement caused dental changes and became a risk factor for side effects. Marklund et al. also demonstrated that the use of soft elastomeric devices provided protection from large reductions in OJ with comparison of the odds ratio.30 This research using study models has also indicated that orthodontic side effects may be predictable based on initial characteristics in dental occlusion and the factors associated with OAs. By measuring forces created by progressive mandibular advancement with OAs, regular dose-dependent increases of force values with increasing mandibular advancement were determined to reach 1.18 N per millimeter of advancement.31 This also supports that mandibular advancement is an important predictive factor. As for this result, to predict side effects, the device factors are more important than the background of patients. In addition to these predictive factors, the number of teeth is correlated with the amount of OJ reduction. Patients with OSA and deep bites did not show reductions in OJ.17 However, the number of teeth had a negative correlation with OJ reduction. According to type of teeth and total number of teeth, OJ reduction was associated with the total number of teeth and number of maxillary teeth. Thus, we found that a smaller number of teeth, especially maxillary teeth, was related to the change in the OJ. OAs have full-arch occlusal coverage, and therefore the mechanical loading force is applied to all teeth. Thus, fewer teeth must carry more burden. Interestingly, OJ reduction and mandibular advancement quantity exhibited stronger correlations than other predictors in the bite change group. This suggests that both mandibular advancement rate and quantity are important to prevent side effects. Moreover, significant differences were observed between the two groups, but there was no correlation regarding the frequency. This is because in the bite change group, all patients used OAs every day except one.
There are a number of potential limitations in this study. The main limitation was that there was a patient selection bias. All patients in this study have teeth that can use OAs to treat OSA (range; 17–31, average; 27.0 ± 2.6). Moreover, this was a retrospective case series and our data only included follow-up patients who were controlled before and after the study. As was mentioned before, there are some side effects resulting from long-term treatment of OAs. This study includes patients who have tolerable side effects, and not those who dropped out due to problems. Although this was a retrospective study, it provides important insights into OAs treatment. Another limitation is methodology. Previous studies showed that OAs have the potential to move anterior teeth and molars by analysis of a study model.18 Ideally, more detailed consideration of occlusion changes may be possible by concurrent studies of cephalometric and study model analysis. However, the prediction of treatment outcome was good and it may be related to the OAs used for patients with OSA.
This study suggests some important factors for patients before treatment and follow-up. The dentists who prescribe OAs should follow long-term OA treatment of OSA. For patients before treatment, in terms of OA treatment success, it is important to predict side effects. Moreover, to identify high-risk patients, it is necessary to consider other appropriate treatment options before treatment with OAs. In some cases, poor convalescence is predicted and treatment options, such as continuous positive airway pressure treatment and surgery, are considered. For example, patients who are only concerned about snoring should be advised to not use OAs every night. In addition, some patients who have few maxillary teeth should be advised about the high risk of dental changes. Thus, managing cases on an individual basis may decrease the extent of changes in high-risk patients. However, most patients neither recognize nor have problems with bite changes. There were no patients who had serious damage to the teeth or temporomandibular joints in this study. Similarly, for follow-up patients, medical staff must note device adjustments as well as side effects. It is thought that assessing changes in OJ is the most important because measurement of OJ is easy for dentists. Therefore, OJ is a useful index to determine dental changes with long-term oral appliance therapy. Particularly high-risk patients are those who frequently use OAs for a long time and those who use OAs that greatly advance the mandible forward.
The treatment of OSA often continues throughout life. In this study, we revealed the predictors of dental changes in order to prevent side effects of long-term OA treatment. This study demonstrates new predictable factors that may cause an occlusion change. Moreover, it may be possible to adjust the mandibular position of OAs and treatment schedule or to suggest other treatments for high-risk patients. With better knowledge of predictive factors for side effects of long-term OA treatment for OSA, clinicians can develop treatment options in the future that will increase patient satisfaction and enhance follow-up treatment for patients.
DISCLOSURE STATEMENT
Work for this study was performed at the Osaka University Graduate School of Dentistry. All authors have seen and approved this manuscript. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Dr. Hiroshi Kurosaka and Dr. Safiye Esra Sarper, Department of Orthodontics and Dentofacial Orthopedics, Osaka University Graduate School of Dentistry Osaka Japan, for their helpful advice on cephalometric analysis.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- ESS
Epworth Sleepiness Scale
- L1-MP
lower incisor line to mandibular plane
- OA
oral appliance
- OB
overbite
- OJ
overjet
- OSA
obstructive sleep apnea
- U1-SN
upper incisor line to sella-nasion line
REFERENCES
- 1.Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976;27:465–484. doi: 10.1146/annurev.me.27.020176.002341. [DOI] [PubMed] [Google Scholar]
- 2.Christensen AS, Clark A, Salo P, et al. Symptoms of sleep disordered breathing and risk of cancer: a prospective cohort study. Sleep. 2013;36(10):1429–1435. doi: 10.5665/sleep.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flemons WW. Clinical practice. Obstructive sleep apnea. N Engl J Med. 2002;347(7):498–504. doi: 10.1056/NEJMcp012849. [DOI] [PubMed] [Google Scholar]
- 4.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29(3):375–380. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson KA, Cartwright R, Rogers R, Schmidt-Nowara W. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29(2):244–262. doi: 10.1093/sleep/29.2.244. [DOI] [PubMed] [Google Scholar]
- 6.Chan AS, Cistulli PA. Oral appliance treatment of obstructive sleep apnea: an update. Curr Opin Pulm Med. 2009;15(6):591–596. doi: 10.1097/MCP.0b013e3283319b12. [DOI] [PubMed] [Google Scholar]
- 7.Ferguson KA, Ono T, Lowe AA, Keenan SP, Fleetham JA. A randomized crossover study of an oral appliance vs nasal-continuous positive airway pressure in the treatment of mild-moderate obstructive sleep apnea. Chest. 1996;109(5):1269–1275. doi: 10.1378/chest.109.5.1269. [DOI] [PubMed] [Google Scholar]
- 8.Pancer J, Al-Faifi S, Al-Faifi M, Hoffstein V. Evaluation of variable mandibular advancement appliance for treatment of snoring and sleep apnea. Chest. 1999;116(6):1511–1518. doi: 10.1378/chest.116.6.1511. [DOI] [PubMed] [Google Scholar]
- 9.Pantin CC, Hillman DR, Tennant M. Dental side effects of an oral device to treat snoring and obstructive sleep apnea. Sleep. 1999;22(2):237–240. doi: 10.1093/sleep/22.2.237. [DOI] [PubMed] [Google Scholar]
- 10.Lawton HM, Battagel JM, Kotecha B. A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: a prospective study. Eur J Orthod. 2005;27(1):82–90. doi: 10.1093/ejo/cjh067. [DOI] [PubMed] [Google Scholar]
- 11.Vezina JP, Blumen MB, Buchet I, Hausser-Hauw C, Chabolle F. Does propulsion mechanism influence the long-term side effects of oral appliances in the treatment of sleep-disordered breathing? Chest. 2011;140(5):1184–1191. doi: 10.1378/chest.10-3123. [DOI] [PubMed] [Google Scholar]
- 12.Doff MHJ, Finnema KJ, Hoekema A, Wijkstra PJ, de Bont LGM, Stegenga B. Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on dental side effects. Clin Oral Investig. 2013;17(2):475–482. doi: 10.1007/s00784-012-0737-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pliska BT, Nam H, Chen H, Lowe AA, Almeida FR. Obstructive sleep apnea and mandibular advancement splints: occlusal effects and progression of changes associated with a decade of treatment. J Clin Sleep Med. 2014;10(2):1285–1291. doi: 10.5664/jcsm.4278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robertson C, Herbison P, Harkness M. Dental and occlusal changes during mandibular advancement splint therapy in sleep disordered patients. Eur J Orthod. 2003;25(4):371–376. doi: 10.1093/ejo/25.4.371. [DOI] [PubMed] [Google Scholar]
- 15.Gong X, Zhang J, Zhao Y, Gao X. Long-term therapeutic efficacy of oral appliances in treatment of obstructive sleep apnea-hypopnea syndrome. Angle Orthod. 2013;83(4):653–658. doi: 10.2319/060412-463.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Almeida FR, Bittencourt LR, de Almeida CI, Tsuiki S, Lowe AA, Tufik S. Effects of mandibular posture on obstructive sleep apnea severity and the temporomandibular joint in patients fitted with an oral appliance. Sleep. 2002;25(5):507–513. [PubMed] [Google Scholar]
- 17.Marklund M. Predictors of long-term orthodontic side effects from mandibular advancement devices in patients with snoring and obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2006;129(2):214–221. doi: 10.1016/j.ajodo.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Almeida FR, Lowe AA, Otsuka R, Fastlicht S, Farbood M, Tsuiki S. Long-term sequellae of oral appliance therapy in obstructive sleep apnea patients: part 2. Study-model analysis. Am J Orthod Dentofacial Orthop. 2006;129(2):205–213. doi: 10.1016/j.ajodo.2005.04.034. [DOI] [PubMed] [Google Scholar]
- 19.Fritsch KM, Iseli A, Russi EW, Bloch KE. Side effects of mandibular advancement devices for sleep apnea treatment. Am J Repir Crit Care Med. 2001;164(5):813–818. doi: 10.1164/ajrccm.164.5.2003078. [DOI] [PubMed] [Google Scholar]
- 20.Okuno K, Sasao Y, Nohara K, et al. Endoscopy evaluation to predict oral appliance outcomes in obstructive sleep apnoea. Eur Respir J. 2016;47(5):1410–1419. doi: 10.1183/13993003.01088-2015. [DOI] [PubMed] [Google Scholar]
- 21.Tsuda H, Almeida FR, Tsuda T, Moritsuchi Y, Lowe AA. Craniofacial changes after 2 years of nasal continuous positive airway pressure use in patients with obstructive sleep apnea. Chest. 2010;138(4):870–874. doi: 10.1378/chest.10-0678. [DOI] [PubMed] [Google Scholar]
- 22.Otsuka R, de Almeida FR, Lowe AA. The effects of oral appliance therapy on occlusal function in patients with obstructive sleep apnea: a short-term prospective study. Am J Orthod Dentofacial Orthop. 2007;131(2):176–183. doi: 10.1016/j.ajodo.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 23.Almeida FR, Lowe AA, Sung JO, Tsuiki S, Otsuka R. Long-term sequellae of oral appliance therapy in obstructive sleep apnea patients: part 1. Cephalometric analysis. Am J Orthod Dentofacial Orthop. 2006;129(2):195–204. doi: 10.1016/j.ajodo.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Rose EC, Staats R, Virchow C, Jr, Jonas IE. Occlusal and skeletal effects of an oral appliance in the treatment of obstructive sleep apnea. Chest. 2002;122(3):871–877. doi: 10.1378/chest.122.3.871. [DOI] [PubMed] [Google Scholar]
- 25.Bondemark L. Does 2 years' nocturnal treatment with a mandibular advancement splint in adult patients with snoring and OSAS cause a change in the posture of the mandible? Am J Orthod Dentofacial Orthop. 1999;116(6):621–628. doi: 10.1016/s0889-5406(99)70196-4. [DOI] [PubMed] [Google Scholar]
- 26.Tsuiki S, Hiyama S, Ono T, et al. Effects of a titratable oral appliance on supine airway size in awake non-apneic individuals. Sleep. 2001;24(5):554–560. doi: 10.1093/sleep/24.5.554. [DOI] [PubMed] [Google Scholar]
- 27.Hammond RJ, Gotsopoulos H, Shen G, Petocz P, Cistulli PA, Darendeliler MA. A follow-up study of dental and skeletal changes associated with mandibular advancement splint use in obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2007;132(6):806–814. doi: 10.1016/j.ajodo.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 28.Zymperdikas VF, Koretsi V, Papageorgiou SN, Papadopoulos MA. Treatment effects of fixed functional appliances in patients with Class II malocclusion: a systematic review and meta-analysis. Eur J Orthod. 2016;38(2):113–126. doi: 10.1093/ejo/cjv034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pancherz H, Fackel U. The skeletofacial growth pattern pre- and post-dentofacial orthopaedics. A long-term study of Class II malocclusions treated with the Herbst appliance. Eur J Orthod. 1990;12(2):209–218. doi: 10.1093/ejo/12.2.209. [DOI] [PubMed] [Google Scholar]
- 30.Marklund M, Franklin KA, Persson M. Orthodontic side-effects of mandibular advancement devices during treatment of snoring and sleep apnoea. Eur J Orthod. 2001;23(2):135–144. doi: 10.1093/ejo/23.2.135. [DOI] [PubMed] [Google Scholar]
- 31.Cohen-Levy J, Petelle B, Pinguet J, Limerat E, Fleury B. Forces created by mandibular advancement devices in OSAS patients: a pilot study during sleep. Sleep Breath. 2013;17(2):781–789. doi: 10.1007/s11325-012-0765-4. [DOI] [PubMed] [Google Scholar]