Abstract
Care for children as they near the end of life is difficult and very complex. More difficult still are the decisions regarding what interventions are and are not indicated during these trying times. Occasionally, families of children who are nearing the end of life disagree with the assessment of the medical team regarding these interventions. In rare cases, the medical team can be moved to enact a do not attempt resuscitation (DNAR) order against the wishes of the patient’s parents. This manuscript presents one such illustrative case and discusses the ethical issues relevant to such challenging clinical scenarios. The authors posit that such a unilateral do not attempt resuscitation order is only appropriate in very limited circumstances in pediatric care. Instead, focus should be placed on open discussion between parents and members of the clinical team, shared decision-making, and maintenance of the clinician-parent relationship while simultaneously supporting members of the clinical team who express discomfort with parental decisions. The authors propose an alternative framework for approaching such a conflict based on clinician-parent collaboration and open communication.
Keywords: Ethics, Decision-making, Do not attempt resuscitation, Do not resuscitate, Pediatrics, Futility
INTRODUCTION
Care for children at the end of life is complex, requiring medical knowledge, interpersonal skills, and the involvement of numerous subspecialists. Decisions about which interventions are warranted at the end of life can be even more complicated, bringing into question medical facts as well as individual values and biases. Complicating matters further are cases in which the child’s parents and medical team are in disagreement. Many hospitals have guidelines for management of such situations, but these cases remain highly charged for all involved. Several recent policy statements highlight the complexity of these contentious scenarios and the strong reactions they elicit.1,2 One particularly challenging disagreement involves cardiopulmonary resuscitation (CPR) of a child with a terminal illness and no known curative options.
We present the case of one such patient and propose a framework for an approach based in tenets of clinical ethics and palliative care.
CASE PRESENTATION
Baby G is seven months old and has advanced liver failure. He was born full-term and developed jaundice shortly after birth. Despite evaluation at several medical facilities, a unifying diagnosis could not be found. He is now severely malnourished, with significant ascites and poor liver function. He is irritable, likely due to hepatic encephalopathy, and is becoming increasingly inconsolable. Despite his condition, he is on room air with stable vital signs.
Supportive therapies are initiated to correct his metabolic derangements and improve his nutritional status. Although the etiology of G’s liver failure is unclear, liver transplantation is the only curative option. Baby G, however, is ineligible for transplant evaluation due to complex social factors.1 His mother is resolved to get him a transplant and is uninterested in discussing alternative hopes or goals of care.
The medical team is at an impasse – they are faced with a critically ill child for whom curative options are not available but for whom the mother will not consider non-curative goals of care. Some distressed members of the care team feel that intensive care for G is futile; they wish to override the mother’s wishes and enter into Baby G’s chart a unilateral do not attempt resuscitation (DNAR) order.
FUTILITY
Cases like this can cause angst among members of the medical team, a condition referred to as “moral distress.” First defined as a circumstance in which one “knows the right thing to do, but institutional constraints make it nearly impossible to pursue the right course of action,”3 moral distress may also describe a situation in which a provider’s sense of “right” is in conflict with the wishes of a patient/surrogate.4,5 This often is related to the belief that an intervention is “futile,” a term that has gone in and out of favor in recent years. Over the past 30 years, researchers have attempted to delineate the concept of futile (or non-beneficial) interventions.6–8 An intervention has been described as quantitatively futile if it has been successful in <1% of cases or qualitatively futile if it portends an extremely poor post-intervention quality of life.9,10 Most now draw distinction between ineffective interventions (physiological futility) and those that would not be of sufficient benefit to the child. The first is a medical assessment – antimicrobial therapy, for instance, would not be medically effective to treat a respiratory virus. The second is a value judgment. What is deemed sufficiently beneficial to one party might not be to another. Determinations of benefit typically are based on an individual’s experiences, cultural and religious beliefs, and future goals. While healthcare professionals decide what is physiologically futile, determinations of benefit for an individual child are far more nuanced but, with few exceptions, should ultimately lie in the hands of the child’s parents.
Inherent in weighing risks and benefits of any intervention is the expectation that providers can reliably predict the intervention’s outcome. Unfortunately, healthcare providers are rather inaccurate in prognosticating when patients will die and which interventions will or will not prolong life.11–13 Definitions of “futility” vary greatly, equating to estimated survival rates anywhere from 0 to 60%.14,15 If clinicians cannot agree on how futility is defined or what will happen to a patient with or without a given intervention, it becomes very difficult to call any particular intervention futile, even in the physiologic sense. Recent movements to replace “futile” with “potentially inappropriate” or “likely non-beneficial” do little to rectify this problem.1,2
One illustrative case study of the role of the futility determination is the Texas Advance Directives Act, legislation aimed at providing an extrajudicial means of resolving conflicts about end-of-life decisions between patients/surrogates and medical providers.16 Some have argued that this law provides a legal and moral “safe harbor” for resolving futility disputes and aids in conservation of scarce medical resources.17–19 Others have called the statute biased and unfair, as committees reviewing the cases sided with the clinicians in >90% of cases,20,21 and in the only published report of pediatric patients for whom the law was applied, all patients were either Hispanic or African-American.22,23 Such findings raise significant concerns about justice and equity, two considerations of great importance in modern medical care.
THE UNIQUE CASE OF PEDIATRICS
In modern medical practice, adults have the autonomous right to make “poor” decisions about their medical care. While the medical team may disagree with a competent adult’s decision to forgo treatment for a curable disease with non-morbid treatment, for instance, the team must respect the patient’s autonomy and cannot override such a decision. In pediatrics, parents are generally accepted to have the right to make medical decisions for their children, but these rights are not without limit.24
Various frameworks have been proposed to determine when healthcare professionals are justified in superseding individuals’ wishes, but the bar is quite high for overruling parents’ decisions regarding the care of their children.24–26 Pediatricians generally do not favor overriding parents’ medical decisions for their children, typically doing so only in the setting of clear and present harm. Diekema’s “harm principle” is one oft-cited threshold for state intervention in the setting of parent-physician conflicts,27 further operationalized by Gillam’s “zone of parental discretion.”28 For conflicts around pediatric end-of-life resuscitation, we favor Ross’ construct of constrained parental autonomy, wherein parents have “a presumptive right to non-interference” that is restricted only if parents fail to provide for their child’s basic needs or disrespect his/her developing personhood.29
This model calls for healthcare professionals to override parents’ wishes only when 1) parents refuse an efficacious, likely successful treatment, thus threatening the child’s life or putting him/her at great risk for serious/significant morbidity; or 2) parents request treatments that are “virtually futile and inhumane.”29 Though we have addressed the hazards of calling an intervention “futile,” we feel this model is an appropriately stringent standard for considering parent preferences regarding end-of-life resuscitation in the setting of terminal illness.
We posit that the decision to override parent preferences regarding interventions at a child’s end of life should be limited to cases in which the parents’ request is clearly malicious and/or an obvious violation of the child’s well-being. As in the model of constrained parental autonomy, this bar intentionally is set quite high, as allowing a child’s life to end without attempting CPR over parental objections is a decision not to be taken lightly. Only extreme actions such as overt child abuse meet these stringent requirements. For example, parent belief in the sanctity of life is a common reason for parent-clinician conflict in end-of-life decision-making.30,31 Temporarily keeping a child with terminal cancer and respiratory failure on a ventilator because continued life is the parents’ highest value supports this belief and should not be grounds for unilateral action. It is immaterial whether parent preference is based on religion or other sociocultural leanings; rather, what matters is that the parents feel each moment of life has meaning unto itself. This value is assigned by the family, not the healthcare team.
Parental motivations certainly matter: in contrast with the prior example, parents who wish to keep their child on a ventilator to continue receiving dependent tax or supplemental security benefits can (and likely should) be questioned. Only if parents clearly are being malicious and/or are in obvious violation of a child’s well-being (such as cases of medical child abuse, Munchausen-by-proxy, or keeping the child alive solely to continue to receive governmental benefits) should the right to decide what is or is not done for a child be wrested from them. While conceptualizations of “well-being” vary by individual, that is not to say that this is a purely subjective standard. Nonetheless, parents’ preferences regarding end-of-life resuscitation should be fulfilled in all but exceedingly rare circumstances.
Clearly, the healthcare team is not obligated to provide all interventions requested by parents to prolonging the child’s life. For example, extracorporeal membrane oxygenation (ECMO) or surgical intervention need not be performed if requested by parents when there is team consensus that these are not medically indicated (i.e., would be physiologically futile). Unlike other medical interventions, current practice – whether by policy or law – requires that CPR be attempted by default in the event of cardiopulmonary arrest or to be discussed with patients/families – even when not recommended – and that decisions about resuscitative efforts (and limits thereof) be made together.
DO NOT ATTEMPT RESUSCITATION ORDERS
The complexity of these issues becomes apparent when discussing initiation of DNAR orders, particularly unilateral DNAR orders. Most commonly utilized for adults with terminal illnesses, DNAR orders are used in a similar fashion and with similar goals in pediatric care. The primary difference is that for adults, the competent patient or his/her designated surrogate is the individual who decides to forgo resuscitative efforts, whereas in pediatrics, the child’s parent is the usual decision-maker.
Though this difference is relatively small in the setting of a standard DNAR order, its significance becomes greater when the patient/parents do not agree with the healthcare team’s plans to withhold resuscitative measures. In such cases, the team sometimes will opt to enter a DNAR order in the patient’s chart without consent from the patient or surrogate, an act known as a unilateral DNAR order. Some have argued that a DNAR order should never be placed without explicit assent/consent.32 In placing a unilateral DNAR order, the clinician implicitly takes on the role of surrogate decision-maker and states his/her belief that attempts at resuscitation would not be in the patient’s best interest.
In recent years, however, many have questioned whether the best interest standard is appropriate in pediatrics.29,33–39 Parents’ decisions for their child need not be the “best” decision but rather must be above a certain level of acceptability. Additionally, parsing the interests of a child from those of the parents/family can be difficult, further limiting the utility of the best interest standard in pediatrics. As discussed above, constrained parental autonomy is a more appropriate and forgiving approach. This model fits what usually is done in standard pediatric practice: though healthcare providers may not always agree with parents’ choices, they only intervene if those choices are clearly malicious and/or an obvious violation of the child’s well-being. This gives parents the benefit of the doubt and acknowledges that unless there is convincing evidence otherwise, parents are assumed to be looking out for what they believe to be best for their children.
SOCIOCULTURAL DIVERSITY
With important issues such as these, we must also consider the diversity of our patient population. Today, pediatric patients are of many different races, ethnicities, and nations of origin, and their families have widely varying sociocultural beliefs. While disagreement remains regarding how to consider differential standards of care in areas of differing socioeconomic status (e.g., developing versus developed nation),40,41 the same does not apply to patients of different financial means or backgrounds treated at a single institution. When faced with disagreements over medical interventions, we must ensure that our patients are offered treatments justly and equitably. Research has shown, however, that those of low socioeconomic status, low health literacy, and different racial, ethnic, and religious backgrounds may both think differently about choices at the end of life and be given different options.20,42–45 It is not difficult to imagine that unilateral DNAR orders would be ordered more commonly for patients with different beliefs than their healthcare team and for those who do not have the means or wherewithal to object. A recent policy statement put forth by the Society of Critical Care Medicine minimizes the significance of these differential beliefs,2 and experience with the Texas Advance Directives Act has done little to assuage these concerns.23,46
CASE PRESENTATION, CONTINUED
Baby G is at risk of death from a range of causes including acute bleeding, infection, electrolyte imbalance, and respiratory failure. Presently, however, he is clinically stable without signs or symptoms of imminent decompensation. His mother’s stated goal is to provide any therapies that will keep him alive, and she continues to express hope for a miracle.
Providers agree that Baby G may die very soon due to an acute event but also may live for many months. The team expresses moral distress – if he were to have an acute event, should CPR be performed as his mother wishes, even though some members of the team feel that CPR would not be in G’s best interest? To declare that CPR would be unconditionally futile (non-beneficial) for Baby G is a value judgment that the only worthwhile goal is long-term survival. Recovery from an acute arrhythmia, opioid side effect, or septic episode to return to the chronic state of living with advanced liver disease without an option for transplantation might be a poor outcome for some but a good outcome for others.
COMMUNICATION AND GOALS OF CARE
In any assessment of the potential benefits and burdens of resuscitative measures, there is an inherent judgment regarding what constitutes a “good” outcome. For some, prolongation of life itself is the goal; others may define quality of life differently. This dictates that parents’ voices be included in any decision about their child’s end-of-life care. Providers must assess the risks and potential benefits of treatment options, but to determine if a given outcome is good, we must understand parents’ goals and values.
Establishment of goals of care can best be achieved through open-ended questioning in a setting of trust and collaborative communication (Table 1).47 Clinicians can query parents about their hopes, worries, and next steps in treatment based on their understanding of their child’s status. This collaborative paradigm shifts the interaction from a delivery of information, debate, and oversimplification to one of learning, exploration, and understanding of complexity.48 It is empowering to bring parents into the decision-making process by asking them to help the medical team understand their perspectives. Challenging the hopes of parents should be avoided, even if these hopes seem physiologically impossible. Unrealistic expectations are problematic; unrealistic hopes are not.
TABLE 1.
Open-ended phrases to facilitate collaborative communication and shared decision-making
| Beginning the conversation |
|
|
| “Tell us about your child before he/she became sick. What was important to him/her and his/her quality of life?” |
| “What is your understanding of your child’s illness/condition?” |
|
|
| Eliciting goals of care |
|
|
| “As you think about your child’s illness/condition, what are your hopes?” |
| “As you think about your child’s illness/condition, what are your worries?” |
| “You mentioned that what is most important to you is that your child be cured. We are hoping for that too. However, if the time comes when a cure isn’t possible, what would be most important to your child and your family?” |
|
|
| Talking about the possibility of death |
|
|
| “We hope that your child will get better, but I am very worried that our treatments will not be successful” |
| “Although no one knows for certain what will happen for your child, most children who are in this situation do not survive” |
|
|
| Talking about what to expect |
|
|
| “Would it be helpful to talk about what to expect if your child’s illness/condition gets worse?” |
| “Have you experienced anything like this before in your family?” |
Adapted from Mack and Wolfe.45
Utilizing shared decision-making, the medical team can present parents with a clear recommendation based on knowledge of the medical facts and the parents’ value system and ask if they agree with these plans.49 This directed approach may be interpreted by some as paternalistic, but the recommendation is central to truly shared decision-making.50,51 Support from the palliative care and/or ethics teams may be beneficial in such situations, both to support parent-clinician discussions and to help alleviate provider moral distress that may arise.52
Making a recommendation about resuscitation status and seeking parental agreement is very different than initiating a unilateral DNAR order. Offering a recommendation acknowledges differences in views while still attempting to lead parents toward interventions that the healthcare team feels to be most appropriate for the child. In contrast, the unilateral DNAR simply supersedes parental decisions. Though subtle, this distinction is important. The former empowers parents while still enabling the team to professionally guide the family, while the latter takes advantage of the clinician-parent power imbalance to throw parents’ disagreements aside. Furthermore, while a unilateral DNAR abruptly and aggressively ends the conversation, a recommendation maintains the clinician-parent relationship and invites further discussion. If the parents do not agree with the recommendation, the discussion can begin again later with further inquiry into the parents’ reasoning and subsequent reevaluation of the child’s status, the parents’ goals of care, and the treatment plan. In the interim, any moral distress that is expressed by providers should be acknowledged, supported, and addressed. Recognition of this distress and provision of support for the healthcare team is integral to the care of the patient and to the morale and well-being of the team. Provider distress alone, however, is insufficient grounds to supersede parental decision-making.
CHALLENGING THE “ALL OR NOTHING” DICHOTOMY
A common misconception that further complicates communication about resuscitation status is the belief that CPR is an “all or nothing” phenomenon.53 Classically, the belief existed that CPR was ineffective after 10–20 minutes, but recent work indicates that individuals may survive with favorable neurologic outcomes following resuscitations of much longer duration.54,55 This has led to recognition that both initiation of CPR and ending a code are complex decisions that require significant individual clinician judgment and tailoring to each clinical scenario.56 Such personalization of care – delivery of care in a medically appropriate manner – is common in medical practice. It is absolutely vital when considering if and how to resuscitate a pediatric patient at the end of life. Such a process allows for consideration of situational factors and context far more than could be accomplished by simply checking “yes” or “no” on a DNAR order in advance of an arrest.
A “medically appropriate” code should not be confused with a “slow code,” however.57–59 We support provision of a tailored, appropriate period of high-quality CPR while investigating possible acute, reversible causes for the patient’s arrest. If no such cause is found, the resuscitation leader can stop resuscitative measures following an individually-defined appropriate duration. An “appropriate” code might last only a few minutes for one patient but much longer and with more invasive interventions for another, when considering the parents’ goals of care, the patient’s clinical circumstances, and other contextual features. Individualization imparts variability in practice, but all care, including at the end of life, should be malleable and individualized. This individualization gives providers – some of whom may question the appropriateness of CPR – input into what an appropriate code should entail for each patient, thereby minimizing provider discomfort/distress and maximizing expert engagement. A growing literature considers what an appropriate code might entail (and for how long),56–58,60–62 but a comprehensive discussion of this is beyond the scope of this manuscript.
This blended, flexible approach requires that providers accept a degree of uncertainty. Education and support are needed to ensure all team members share a common understanding of how practice can and should be tailored for each individual patient, particularly when not all members of the team agree regarding the appropriateness of resuscitative measures. Again, ethics and/or palliative care teams can assist with such endeavors.
AN ALTERNATIVE MODEL
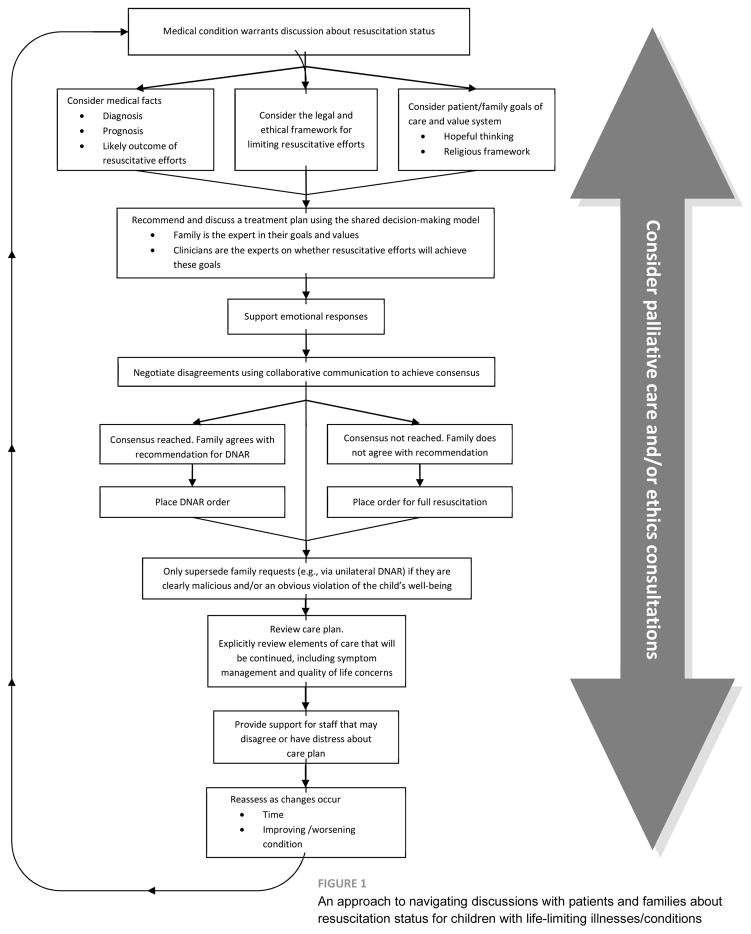
Most often, the medical team and parents agree about initiation of a DNAR order; occasionally the team does not explicitly agree with the parents but is willing to defer to parental wishes. Though uncommon, entrenched disagreements are highly charged and distressing for all involved. We propose a model (Figure 1) that includes active solicitation of the input of parents and significant effort to defer to parental wishes, only overruling those wishes when they or the reasons for them are clearly malicious and/or an obvious violation of the child’s well-being. This model engages parents and the medical team in active communication in attempt to come to consensus about what to do in the case of a child’s arrest. All parties are encouraged to voice their perspectives in a respectful and collaborative fashion.
FIGURE 1.
An approach to navigating discussions with patients and families about resuscitation status for children with life-limiting illnesses/conditions
Imposing a unilateral DNAR order can irreparably fracture the clinician-parent relationship at a time when that relationship is needed more than ever. Though potentially time-intensive and complicated, this approach gives parents a strong voice in their child’s care at the end of life, provides the healthcare team the opportunity to impart its clinical expertise, maintains or even strengthens the clinician-parent relationship, and hopefully provides the child in question with an elusive “good death.”63 The time has come for clinicians to take to heart the words from Robert Truog’s landmark piece from 2010: “providing non-beneficial CPR can be an act of sincere caring and compassion” and has “a limited but legitimate place in the practice of medicine.”64
CASE CONCLUSION
With excellent supportive care in the intensive care unit, Baby G stabilizes, and, after many discussions between the medical team and Baby G’s mother, he is transferred to a chronic care floor with orders for full resuscitative efforts. Due to the unwavering advocacy of his mother, G is reevaluated and listed for liver transplantation. He lives in the hospital for three months, during which time he grows his first tooth, takes many smiling photos, and wins the hearts of nurses and staff. Unfortunately, while awaiting transplant, Baby G dies from gastrointestinal bleeding that could not be controlled with intensive care and surgical efforts.
Since his death, his mother has expressed extreme gratitude not only for the time she had with him, but also for the valiant efforts of the healthcare team as they provided CPR in his final moments.
Acknowledgments
Funding: This work was supported by the National Institutes of Health (T32 CA136432), Pedals for Pediatrics, and the Harvard Medical School Center for Bioethics (JMM)
Baby G’s name and several details of his case have been changed to maintain confidentiality. The authors would like to thank the members of the Ethics Advisory Committee and the DNR Subcommittee at Boston Children’s Hospital for their invaluable discussions and insights on this topic.
Abbreviations
- DNAR
do not attempt resuscitation
- CPR
cardiopulmonary resuscitation
- ECMO
extracorporeal membrane oxygenation
Footnotes
Baby G was ineligible for transplant evaluation because he did not have health insurance or means of payment as a result of recent immigration to the United States. This eligibility criterion itself is ethically charged, but a full discussion of this issue is beyond the scope of this manuscript.
Contributor Statement:
Drs. Marron, Wolfe, and Jones each participated in project design, drafted and critically reviewed the manuscript, and approved the final manuscript as submitted.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
None of the authors have any financial or personal conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bosslet GT, Pope TM, Rubenfeld GD, et al. An Official ATS/AACN/ACCP/ESICM/SCCM Policy Statement: Responding to Requests for Potentially Inappropriate Treatments in Intensive Care Units. American journal of respiratory and critical care medicine. 2015;191(11):1318–1330. doi: 10.1164/rccm.201505-0924ST. [DOI] [PubMed] [Google Scholar]
- 2.Kon AA, Shepard EK, Sederstrom NO, et al. Defining Futile and Potentially Inappropriate Interventions: A Policy Statement From the Society of Critical Care Medicine Ethics Committee. Critical care medicine. 2016;44(9):1769–1774. doi: 10.1097/CCM.0000000000001965. [DOI] [PubMed] [Google Scholar]
- 3.Jameton A. Nursing practice : the ethical issues. Englewood Cliffs, N.J: Prentice-Hall; 1984. [Google Scholar]
- 4.Hamric AB. Empirical research on moral distress: issues, challenges, and opportunities. HEC forum : an interdisciplinary journal on hospitals’ ethical and legal issues. 2012;24(1):39–49. doi: 10.1007/s10730-012-9177-x. [DOI] [PubMed] [Google Scholar]
- 5.Campbell SM, Ulrich CM, Grady C. A Broader Understanding of Moral Distress. The American journal of bioethics : AJOB. 2016;16(12):2–9. doi: 10.1080/15265161.2016.1239782. [DOI] [PubMed] [Google Scholar]
- 6.Waisel DB, Truog RD. The cardiopulmonary resuscitation-not-indicated order: futility revisited. Annals of internal medicine. 1995;122(4):304–308. doi: 10.7326/0003-4819-122-4-199502150-00011. [DOI] [PubMed] [Google Scholar]
- 7.Helft PR, Siegler M, Lantos J. The rise and fall of the futility movement. The New England journal of medicine. 2000;343(4):293–296. doi: 10.1056/NEJM200007273430411. [DOI] [PubMed] [Google Scholar]
- 8.Burns JP, Truog RD. Futility: a concept in evolution. Chest. 2007;132(6):1987–1993. doi: 10.1378/chest.07-1441. [DOI] [PubMed] [Google Scholar]
- 9.Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Annals of internal medicine. 1990;112(12):949–954. doi: 10.7326/0003-4819-112-12-949. [DOI] [PubMed] [Google Scholar]
- 10.Murphy DJ, Finucane TE. New do-not-resuscitate policies. A first step in cost control. Archives of internal medicine. 1993;153(14):1641–1648. [PubMed] [Google Scholar]
- 11.Meadow W, Lagatta J, Andrews B, et al. Just, in time: ethical implications of serial predictions of death and morbidity for ventilated premature infants. Pediatrics. 2008;121(4):732–740. doi: 10.1542/peds.2006-2797. [DOI] [PubMed] [Google Scholar]
- 12.Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ (Clinical research ed) 2000;320(7233):469–472. doi: 10.1136/bmj.320.7233.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poses RM, Bekes C, Copare FJ, Scott WE. The answer to “What are my chances, doctor?” depends on whom is asked: prognostic disagreement and inaccuracy for critically ill patients. Critical care medicine. 1989;17(8):827–833. doi: 10.1097/00003246-198908000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Curtis JR, Park DR, Krone MR, Pearlman RA. Use of the medical futility rationale in do-not-attempt-resuscitation orders. JAMA. 1995;273(2):124–128. [PubMed] [Google Scholar]
- 15.McCrary SV, Swanson JW, Youngner SJ, Perkins HS, Winslade WJ. Physicians’ quantitative assessments of medical futility. The Journal of clinical ethics. 1994;5(2):100–105. [PubMed] [Google Scholar]
- 16.Texas Health and Safety Code Section 166.001: Advance Directives Act, 1999.
- 17.Fine RL, Mayo TW. Resolution of futility by due process: early experience with the Texas Advance Directives Act. Annals of internal medicine. 2003;138(9):743–746. doi: 10.7326/0003-4819-138-9-200305060-00011. [DOI] [PubMed] [Google Scholar]
- 18.McCullough LB. Professionally Responsible Clinical Ethical Judgments of Futility. The American journal of bioethics : AJOB. 2015;15(8):54–56. doi: 10.1080/15265161.2015.1045096. [DOI] [PubMed] [Google Scholar]
- 19.Fine RL. Point: The Texas Advance Directives Act effectively and ethically resolves disputes about medical futility. Chest. 2009;136(4):963–967. doi: 10.1378/chest.09-1267. [DOI] [PubMed] [Google Scholar]
- 20.Rosoff PM. Institutional futility policies are inherently unfair. HEC forum : an interdisciplinary journal on hospitals’ ethical and legal issues. 2013;25(3):191–209. doi: 10.1007/s10730-012-9194-9. [DOI] [PubMed] [Google Scholar]
- 21.Truog RD. Counterpoint: The Texas Advance Directives Act is ethically flawed: medical futility disputes must be resolved by a fair process. Chest. 2009;136(4):968–971. doi: 10.1378/chest.09-1269. discussion 971–963. [DOI] [PubMed] [Google Scholar]
- 22.Eason EB, Castriotta RJ, Gremillion V, Sparks JW. Withdrawal of life sustaining treatment in children in the first year of life. Journal of perinatology : official journal of the California Perinatal Association. 2008;28(9):641–645. doi: 10.1038/jp.2008.58. [DOI] [PubMed] [Google Scholar]
- 23.Bosslet G, Helft PR. In response to: Withdrawal of life-sustaining treatment in the first year of life. Journal of perinatology : official journal of the California Perinatal Association. 2009;29(4):327–328. doi: 10.1038/jp.2009.6. author reply 328–329. [DOI] [PubMed] [Google Scholar]
- 24.Buchanan AE, Brock DW. Deciding for others : the ethics of surrogate decision making. Cambridge England ; New York: Cambridge University Press; 1989. [Google Scholar]
- 25.McDougall RJ, Notini L. Overriding parents’ medical decisions for their children: a systematic review of normative literature. Journal of medical ethics. 2014;40(7):448–452. doi: 10.1136/medethics-2013-101446. [DOI] [PubMed] [Google Scholar]
- 26.Mercurio MR, Murray PD, Gross I. Unilateral pediatric “do not attempt resuscitation” orders: the pros, the cons, and a proposed approach. Pediatrics. 2014;133(Suppl 1):S37–43. doi: 10.1542/peds.2013-3608G. [DOI] [PubMed] [Google Scholar]
- 27.Diekema DS. Parental refusals of medical treatment: the harm principle as threshold for state intervention. Theoretical medicine and bioethics. 2004;25(4):243–264. doi: 10.1007/s11017-004-3146-6. [DOI] [PubMed] [Google Scholar]
- 28.Gillam L. The zone of parental discretion: An ethical tool for dealing with disagreement between parents and doctors about medical treatment for a child. Clinical Ethics. 2016;11(1):1–8. [Google Scholar]
- 29.Ross LF. Children, families, and health care decision making. Oxford ; New York: Clarendon Press; 1998. [Google Scholar]
- 30.Kopelman AE. Understanding, avoiding, and resolving end-of-life conflicts in the NICU. The Mount Sinai journal of medicine, New York. 2006;73(3):580–586. [PubMed] [Google Scholar]
- 31.Hamric AB, Borchers CT, Epstein EG. Development and Testing of an Instrument to Measure Moral Distress in Healthcare Professionals. AJOB Primary Research. 2012;3(2):1–9. [Google Scholar]
- 32.Biegler P. Should patient consent be required to write a do not resuscitate order? Journal of medical ethics. 2003;29(6):359–363. doi: 10.1136/jme.29.6.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brudney D, Lantos JD. Whose interests count? Pediatrics. 2014;134(Suppl 2):S78–80. doi: 10.1542/peds.2014-1394B. [DOI] [PubMed] [Google Scholar]
- 34.Groll D. Four models of family interests. Pediatrics. 2014;134(Suppl 2):S81–86. doi: 10.1542/peds.2014-1394C. [DOI] [PubMed] [Google Scholar]
- 35.Martin C. Deception and the death of Ilyusha: truth and the best interest of a dying child in The Brothers Karamazov. Pediatrics. 2014;134(Suppl 2):S87–96. doi: 10.1542/peds.2014-1394D. [DOI] [PubMed] [Google Scholar]
- 36.Lindemann H. Why families matter. Pediatrics. 2014;134(Suppl 2):S97–103. doi: 10.1542/peds.2014-1394E. [DOI] [PubMed] [Google Scholar]
- 37.Hardart GE, Chung WK. Genetic testing of children for diseases that have onset in adulthood: the limits of family interests. Pediatrics. 2014;134(Suppl 2):S104–110. doi: 10.1542/peds.2014-1394F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carbone J. Legal applications of the “best interest of the child” standard: judicial rationalization or a measure of institutional competence? Pediatrics. 2014;134(Suppl 2):S111–120. doi: 10.1542/peds.2014-1394G. [DOI] [PubMed] [Google Scholar]
- 39.Rhodes R, Holzman IR. Is the best interest standard good for pediatrics? Pediatrics. 2014;134(Suppl 2):S121–129. doi: 10.1542/peds.2014-1394H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Angell M. The Ethics of Clinical Research in the Third World. New England Journal of Medicine. 1997;337(12):847–849. doi: 10.1056/NEJM199709183371209. [DOI] [PubMed] [Google Scholar]
- 41.Wendler D, Emanuel EJ, Lie RK. The standard of care debate: can research in developing countries be both ethical and responsive to those countries’ health needs? American journal of public health. 2004;94(6):923–928. doi: 10.2105/ajph.94.6.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee KJ, Tieves K, Scanlon MC. Alterations in end-of-life support in the pediatric intensive care unit. Pediatrics. 2010;126(4):e859–864. doi: 10.1542/peds.2010-0420. [DOI] [PubMed] [Google Scholar]
- 43.Blackhall LJ, Frank G, Murphy ST, Michel V, Palmer JM, Azen SP. Ethnicity and attitudes towards life sustaining technology. Social science & medicine (1982) 1999;48(12):1779–1789. doi: 10.1016/s0277-9536(99)00077-5. [DOI] [PubMed] [Google Scholar]
- 44.Brierley J, Linthicum J, Petros A. Should religious beliefs be allowed to stonewall a secular approach to withdrawing and withholding treatment in children? Journal of medical ethics. 2013;39(9):573–577. doi: 10.1136/medethics-2011-100104. [DOI] [PubMed] [Google Scholar]
- 45.Kapo J, MacMoran H, Casarett D. “Lost to follow-up”: ethnic disparities in continuity of hospice care at the end of life. Journal of palliative medicine. 2005;8(3):603–608. doi: 10.1089/jpm.2005.8.603. [DOI] [PubMed] [Google Scholar]
- 46.Truog RD. Tackling medical futility in Texas. The New England journal of medicine. 2007;357(1):1–3. doi: 10.1056/NEJMp078109. [DOI] [PubMed] [Google Scholar]
- 47.Mack JW, Wolfe J. Early integration of pediatric palliative care: for some children, palliative care starts at diagnosis. Current opinion in pediatrics. 2006;18(1):10–14. doi: 10.1097/01.mop.0000193266.86129.47. [DOI] [PubMed] [Google Scholar]
- 48.Feudtner C. Collaborative communication in pediatric palliative care: a foundation for problem-solving and decision-making. Pediatric clinics of North America. 2007;54(5):583–607. ix. doi: 10.1016/j.pcl.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Social science & medicine (1982) 1997;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 50.Marron JM, Truog RD. Against “Healthy Paternalism” at the End of Life. JAMA oncology. 2016;2(6):832. doi: 10.1001/jamaoncol.2016.1390. [DOI] [PubMed] [Google Scholar]
- 51.Blumenthal-Barby JS, Naik AD. In Defense of Nudge-Autonomy Compatibility. The American journal of bioethics : AJOB. 2015;15(10):45–47. doi: 10.1080/15265161.2015.1074304. [DOI] [PubMed] [Google Scholar]
- 52.Casarett D, Siegler M. Unilateral do-not-attempt-resuscitation orders and ethics consultation: a case series. Critical care medicine. 1999;27(6):1116–1120. doi: 10.1097/00003246-199906000-00031. [DOI] [PubMed] [Google Scholar]
- 53.Clark JD, Dudzinski DM. The false dichotomy: do “everything” or give up. The American journal of bioethics : AJOB. 2011;11(11):26–27. doi: 10.1080/15265161.2011.603807. [DOI] [PubMed] [Google Scholar]
- 54.Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380(9852):1473–1481. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nagao K, Nonogi H, Yonemoto N, et al. Duration of Prehospital Resuscitation Efforts After Out-of-Hospital Cardiac Arrest. Circulation. 2016;133(14):1386–1396. doi: 10.1161/CIRCULATIONAHA.115.018788. [DOI] [PubMed] [Google Scholar]
- 56.Ranola PA, Merchant RM, Perman SM, et al. How long is long enough, and have we done everything we should?--Ethics of calling codes. Journal of medical ethics. 2015;41(8):663–666. doi: 10.1136/medethics-2013-101949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Morrison W, Feudtner C. Quick and limited is better than slow, sloppy, or sly. The American journal of bioethics : AJOB. 2011;11(11):15–16. doi: 10.1080/15265161.2011.603804. [DOI] [PubMed] [Google Scholar]
- 58.Janvier A, Barrington K. What is an “appropriate code”? The American journal of bioethics : AJOB. 2011;11(11):18–20. doi: 10.1080/15265161.2011.603798. [DOI] [PubMed] [Google Scholar]
- 59.Lantos JD, Meadow WL. Should the “slow code” be resuscitated? The American journal of bioethics : AJOB. 2011;11(11):8–12. doi: 10.1080/15265161.2011.603793. [DOI] [PubMed] [Google Scholar]
- 60.Petty K, DeGarmo N, Aitchison R, Aitchison P, Wang E, Kharasch M. Ethical considerations in resuscitation. Disease-a-month : DM. 2013;59(5):217–220. doi: 10.1016/j.disamonth.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 61.Mancini ME, Diekema DS, Hoadley TA, et al. Part 3: Ethical Issues: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S383–396. doi: 10.1161/CIR.0000000000000254. [DOI] [PubMed] [Google Scholar]
- 62.Yoon JC, Kim WY. What should we consider when applying termination of resuscitation rules? Journal of thoracic disease. 2016;8(7):1377–1380. doi: 10.21037/jtd.2016.05.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Powell T, Hulkower A. A Good Death. The Hastings Center report. 2017;47(1):28–29. doi: 10.1002/hast.669. [DOI] [PubMed] [Google Scholar]
- 64.Truog RD. Is it always wrong to perform futile CPR? The New England journal of medicine. 2010;362(6):477–479. doi: 10.1056/NEJMp0908464. [DOI] [PubMed] [Google Scholar]