Abstract
Purpose
To report removal of retained subfoveal perfluorocarbon liquid (PFCL) after vitrectomy for retinal detachment.
Methods
Three patients underwent 3-port 23-gauge vitrectomy in an attempt to remove retained subfoveal PFCL bubble secondary to retinal detachment surgery. In two patients, removal was achieved via a 23-G needle whereas the third patient with multiple small subfoveal droplets, multiple punctures were required and in that case a small 40-G needle was used.
We assessed best corrected visual acuity (BCVA), fundus imaging, and spectral domain optical coherence tomography (SD-OCT) of all patients before and after surgery.
Results
The subfoveal PFCL was successfully removed in all 3 eyes and although a functional improvement was documented, outer retinal atrophy and photoreceptor loss was observed in all our cases.
Conclusions
SD-OCT allows early recognition of retained subfoveal PFCL. Surgical removal may lead to retinal morphologic restoration and functional improvement. While we achieved complete removal of PFCL with both 23-G and 40-G instrumentation, we believe the versatility and ease justifies the universal usage of 40-G retinotomy needles.
Keywords: Subfoveal perfluorocarbon, PFCL, PFCL removal
Introduction
The advantages of perfluorocarbon liquids (PFCLs) have been widely reported in vitreoretinal surgery. However, its use is associated with some complications including the risk of PFCL retention which range between 0.9 and 11%.1, 2, 3 Subretinal retention of PFCL is thought to cause retinal damage as a consequence of mechanical compression of the retina, and secondly from chemical toxicity due to high oxygen carrying capacity of this tamponade which causes vasoconstriction of retinal blood vessels.4, 5, 6, 7 When this retention occurs in the subfoveal area, the consequent deterioration of the central vision justifies early surgical removal of PFCL. Spectral domain optical coherence tomography (SD-OCT) is indispensable in differentiating retained PFCL from subretinal fluid which is managed only with patient follow-up after surgery. We present three patients who had retained subfoveal PFCL after pars plana vitrectomy for retinal detachment. Surgical removal of PFCL was performed in all three patients with three different methods. The anatomical and visual outcomes are discussed below.
Case report
Patient 1
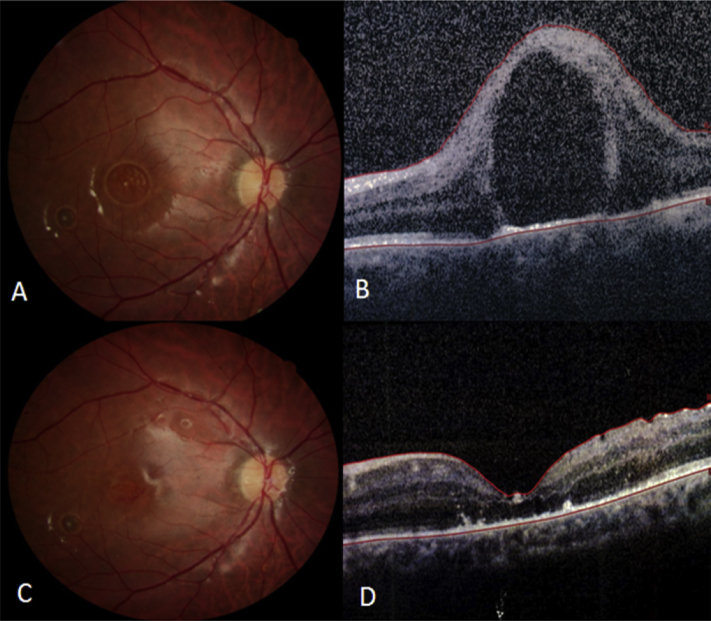
A 55-year-old man presented with a macular threatening rhegmatogenous retinal detachment secondary to a large superotemporal horseshoe tear. The patient underwent PFCL assisted pars plana vitrectomy with silicone oil tamponade. On the first postoperative day, the patient's vision was counting finger (CF) at 4 m and the retina totally attached. However, a large subfoveal and multiple extrafoveal PFCL bubbles were noted clinically, and this was confirmed with OCT imaging (Fig. 1). Five days after the first operation, we re-operated and using a 23-G needle performed a retinotomy at the supranasal edge of the subfoveal bubble. The initial approach was to perform a passive removal while maintaining the intraocular pressure with a silicone oil overfill, but this was unsuccessful so we connected a 27-G cannula to the vitrector and used active aspiration to remove the PFCL. The postoperative examination confirmed there was complete removal of the bubble, and this was recorded with the OCT (Fig. 1). Three months later, the patient's vision improved to 20/50, but there was evidence of outer retinal atrophy and photoreceptor loss in the region of the retinotomy.
Fig. 1.
First patient fundus photograph and optical coherence tomography (OCT) the day after surgery (A, B) and after removal of perfluorocarbon liquid (PFCL) bubble (C, D). Atrophy of outer retinal layers and photoreceptor loss is evident in follow-up OCT (D).
Patient 2
A 37-year-old man who was bilaterally pseudophakic presented with a recent visual loss in his left eye. He was found to have a total retinal detachment with a superotemporal break. He underwent a 23-G PFCL-assisted pars plana vitrectomy with silicone oil injection. On day one, the retina was completely attached, but a large subfoveal PFCL was present (Fig. 2a). The acuity was CF. A further procedure was planned for 3 days hence to remove the subfoveal PFCL using 23-G vitrectomy. On this occasion a retinotomy was made with a 23-G needle adjacent to the subfoveal bubble and by means of a soft tip needle, the PFCL was removed. Again, the intraocular pressure was maintained by simultaneous injection of silicone oil.
Fig. 2.
Second patient fundus photograph and optical coherence tomography (OCT) the day after surgery (A, B) and after removal of perfluorocarbon liquid (PFCL) bubble (C, D). Again atrophy of outer retinal layers and photoreceptor loss is evident in follow-up OCT (D).
Postoperative fundus examination and OCT confirmed complete removal of the bubble (Fig. 2b). Visual acuity improved to 2/10 at 3 months follow-up. A subsequent OCT scan showed outer retinal layer atrophy with photoreceptor loss (Fig. 2c).
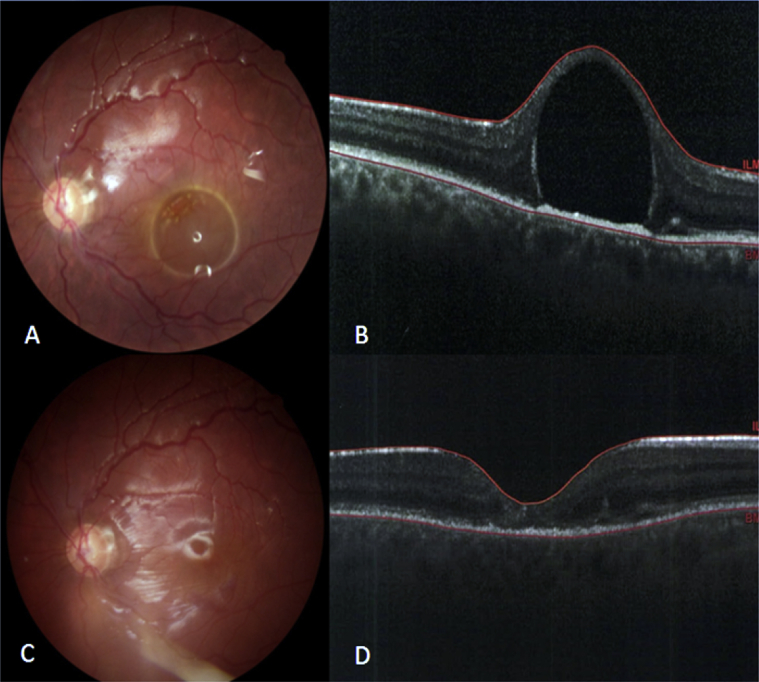
Patient 3
A 30-year-old woman underwent scleral buckling for total rhegmatogenous retinal detachment in her right eye 3 weeks prior to presentation which was unsuccessful. Subsequent to this, a 23-G vitrectomy with oil tamponade was performed which achieved anatomical success, but postoperatively, multiple small PFCL bubbles were noted at the macula and fovea (Fig. 3a). OCT images confirmed the presence of multiple subfoveal PFCL bubbles (Fig. 3b). Four days later, we performed 23-G vitrectomy to remove the bubbles. We also peeled the internal limiting membrane (ILM) prior to removal of the bubbles to reduce the risk of macular hole formation. In this case, the silicone oil was removed, the ILM stained with Brilliant Blue G (BBG) dye, and subsequently peeled from the posterior pole including the location containing the PFCL bubbles. The bubbles were removed by passive aspiration via multiple tiny retinotomies created by the 40-gauge needle. Silicone oil was injected into the eye at the end of surgery. Postoperative OCT confirmed removal of all bubbles. Two months later, the patient's best corrected visual acuity (BCVA) improved to 2/10, but we noticed the formation of a full thickness macular hole and atrophy of outer retinal layers and photoreceptor loss on OCT images (Fig. 3).
Fig. 3.
Third patient fundus photograph and optical coherence tomography (OCT) the day after surgery (A, B) and after removal of perfluorocarbon liquid (PFCL) bubble (C, D). Full-thickness macular hole is evident in follow-up OCT (D).
Discussion
A recognised risk of using PFCL during vitrectomy surgery is that some bubbles may be trapped under the retina and become positioned under or near the macula. This complication is more commonly reported following surgeries for giant retinal tears, in cases where there is incomplete removal of tractional membranes and when multiple small PFCL bubbles form during surgery.7
Retained PFCL causes retinal toxicity through presumed mechanical compression and chemical toxicity.4, 5, 6, 7 The presence of subretinal PFCL does not seem to affect visual and anatomic success when located outside the macula, but deterioration of the central vision will occur when it involves the macular area, especially the fovea.7
An important factor in removing subfoveal PFCL is timely operation before irreversible retinal damage and atrophy. In some cases, differentiation of subretinal PFCL from subretinal fluid may pose a problem. The latter usually resolves without intervention. SD-OCT is quite helpful in this regard. Some distinguishing features have been described, as well.8 On OCT of subretinal PFCL, the retinal contour has the shape of the Greek letter Ω and the angle between the retinal pigment epithelium (RPE), and the neurosensory retina at the base of the PFCL droplet is always acute, while subretinal fluid leads to a retinal contour resembling a hat, with an obtuse angle between the RPE and the neurosensory retina at the base. The retinal layers above the subretinal PFCL droplets are undefined, but in persistent subretinal fluid, the overlying retinal layers are clearly differentiable. Other distinguishing features are elevation of the RPE hyper-reflective band and a hyper-reflective shadow at the choroid in the cases of retained PFCL.8 The observed macular hole after PFCL removal could be due to the local shrinkage of the retina due to glial cells toxicity, surgical trauma, or the retention of cyst-like material around the bubble.
This series demonstrates small bubbles of PFCL removal can either be achieved with a small retinotomy adjacent to the PFCL bubble using a small gauge cannula (39–50 gauges) and active aspiration. Larger bubbles may require a peripheral retinotomy, induction of a localized detachment of the retina, and the insertion of a flute needle under the retina.7, 9, 10 In two of our cases, we used a 23-G needle with success as the size of the bubble permitted that approach whereas the case with multiple and small collections a 40-G aspiration was necessary. In retrospect, it may have been prudent to use a 40-G needle in all 3 cases to reduce the degree of retinal trauma.
We believe some of the adverse changes seen on OCTs of patients 1 and 2 were caused by the harsh surgical technique induced by the large gauge needle used for retinotomy.
In conclusion, subfoveal PFCL causes outer retinal atrophy and photoreceptor loss, probably because of mechanical compression and chemical injury. New imaging modalities such as SD-OCT allow early recognition of retained subfoveal PFCL. Surgical removal leads to retinal morphologic restoration and functional improvement. Where possible, we would now advocate the use of a 40-G needle to remove subretinal PFCL in the first instance.
Footnotes
Conflicts of interest: No conflicts of interest.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Roth D.B., Sears J.E., Lewis H. Removal of retained subfoveal perfluoro-n-octane liquid. Am J Ophthalmol. 2004;138:287–289. doi: 10.1016/j.ajo.2004.02.077. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Valenzuela E., Ito Y., Abrams G.W. Risk factors for retention of subretinal perfluorocarbon liquid in vitreoretinal surgery. Retina. 2004;24:746–752. doi: 10.1097/00006982-200410000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Bourke R.D., Simpson R.N., Cooling R.J., Sparrow J.R. The stability of perfluoro-N-octane during vitreoretinal procedures. Arch Ophthalmol. 1996;114:537–544. doi: 10.1001/archopht.1996.01100130529005. [DOI] [PubMed] [Google Scholar]
- 4.Kobuch K., Menz D.H., Hoerauf H., Dresp J.H., Gabel V.-P. New substances for intraocular tamponades: perfluorocarbon liquids, hydrofluorocarbon liquids and hydrofluorocarbon-oligomers in vitreoretinal surgery. Graefe's Arch Clin Exp Ophthalmol. 2001;239:635–642. doi: 10.1007/s004170100330. [DOI] [PubMed] [Google Scholar]
- 5.Kobuch K., Fuchs B., Tomi A., Roider J., Gabel V.P. The influence of O2 and CO2 concentrations in perfluorocarbon liquid as vitreous substitutes on the retinal perfusion. Invest Ophthalmol Vis Sci. 1999;40:4052. [Google Scholar]
- 6.Kobuch K., El Batarny A., Ueda N. Perfluorophenanthrene causes vascular and neural damage in the rabbit eye. Invest Ophthalmol Vis Sci. 1997;38:3111. [Google Scholar]
- 7.Rayan S.J. 5th ed. vol. 3. 2013. p. 1753. (Retina). [Google Scholar]
- 8.Lois N., Wong D. Lippincot Williams & Wilkins, a Wolters Kluwer busineu; 2013. Complications of vitreo-retinal surgery; pp. 212–217. [Chapter 19c] [Google Scholar]
- 9.Le Tien V., Pierre-Kahn V., Azan F., Renard G., Chauvaud D. Displacement of retained subfoveal perfluorocarbon liquid after vitreoretinal surgery. Arch Ophthalmol. 2008;126:98–101. doi: 10.1001/archophthalmol.2007.2. [DOI] [PubMed] [Google Scholar]
- 10.Kim J.M., Woo S.J., Park K.H., Chung H. Surgical removal of retained subfoveal perfluorocarbon liquid through a therapeutic macular hole with intravitreal PFCL injection and gas tamponade. Korean J Ophthalmol. 2013;27(5):392–395. doi: 10.3341/kjo.2013.27.5.392. [DOI] [PMC free article] [PubMed] [Google Scholar]