SUMMARY
Objectives
To define the possible complications of oral surgery in childhood in patients affected by type 1 Osteogenesis imperfecta (OI) and treated with bisphosphonates (BP).
Methods
The study was conducted among 20 patients in childhood with an age range 8–14 (12 ♂ e 8 ♀) affected by OI. Patients were initially evaluated at the Policlinico Umberto I, University Hospital of Rome, Rare Disease Center Skeletal Dysplasia-Bone Metabolic Pathologies and after at the Policlinico Umberto I, University Hospital of Rome, Head and Neck Department, UOC Pediatric Dentistry.
Results
From this experience, we showed that a proper patient management from the medical and dental point of view can protect these patients from the risk of post-operative problems, such as onj, soft tissue flogos, intraoral and extraoral fistulas, failure to heal the post-extractive alveolus, infections, post-operative pain and pathological fractures. The follow-up, ranging from a minimum of 2 years to a maximum of 5 years, have not demonstrated the presence of particular complications or healing defects.
Conclusions
The clinical experiences observed in these patients are encouraging because no postoperative complications have been observed compared to patients non-affected by OI.
Keywords: osteogenesis imperfecta, bisphosphonates, children, oral surgery
Introduction
Osteogenesis imperfecta (OI) is a rare disease, hereditary connective tissue whose main peculiarities are bone fragility responsible for multiple recurrent fractures that can occur for minimal traumas and low bone density (1).
Clinically it can detect: low stature, blue sclera, loss of hearing in adulthood, imperfect dentinogenesis, scoliosis and ligament laxity; regarding the OI classification, nowadays we refer to the one proposed by Sillence et al. (2) in 1979, who classified patients with OI in four groups based on clinical criteria and on severity of the disease.
The 90% of OI types are characterized by COLIA1 and COLIA2 gene mutations, which encoding the chains α1 e α2 of the type I collagen, which is the principal component of the bone matrix (3).
The diagnosis (3) is mainly of clinical and radiological type. The pathological monitoring examination of OI is the MOC (DXA) that is performed annually for the control of bone density. The MOC is evaluated by the pediatric specialist: if this exam presents bone stability values, the drug therapy may be interrupted.
There is currently no causal type therapy (4). Elective therapy is the administration of bisphosphonates (BP), that are drugs classified as bone-suppressors acting by blocking osteoclastic activity, hence the bone remodeling and increasing bone resistance to fractures. Depending on the presence of an amine group, it can be distinguished in aminoBP and non-aminoBP. These drugs are known and feared because of the risk of developing osteonecrosis (onj) (5, 6).
The literature review shows a lack of sufficient data for provide scientifically validated protocols that defines the management pre- and postoperative management of the patients in childhood with OI that has to perform oral surgery.
Hennedige et al. (7) conducted a literature review showing that no patients under the age of 24 presented onj associated with the use of BP.
Bhatt et al. (8–11) described the absence of bronj cases in children, and the low incidence in adult oncology patients treated with high doses of BPs. Antoniazzi et al. (12) described the absence of onj cases in a pediatric sample affected by OI treated with neridronate.
Objective of the study
In the UOC of Pediatric Dentistry of Umberto I, University Hospital of Rome, patients with “special needs” problems, with systemic pathologies and with dental anomalies are visited and treated (13–15).
Of these patients, the need for surgical and orthodontic treatment and customer satisfaction is assessed (16–18).
The objective of the study was to describe the clinical experience of 20 patients in childhood recruited at the Umberto I, University Hospital of Rome, Head and Neck Department, UOC Pediatric Dentistry. The possible complications of oral surgery in childhood age in patients with OI and treated with bisphosphonates were studied (19, 20). We focused our observation from simpler procedures such as abt of the tartar in which it is expected to have gingival bleeding, or the simple extraction, to the most complex and invasive procedures as complicated extractions such as germectomy or the application of orthodontic mini-implants.
With this experience, we aim to increase the information published on these patients in order to have real protocols in the future for pre- and postoperative management in oral surgery.
Possible complications monitored in the sample:
- Onj
- Soft tissue flogues
- Intraoral and extraoral fistula
- Failure to heal the post extraction vessel
- Post-operative pain
- Edema and trism
- Pathological fracture.
Material and methods
The study was conducted among 20 patients in childhood with an age range 8–14 (12 ♂ e 8 ♀) affected by type I OI. Patients were initially evaluated at the Umberto I, University Hospital of Rome, Rare Disease Center Skeletal Dysplasia-Bone Metabolic Pathologies and after at the Umberto I, University Hospital of Rome, Head and Neck Department, UOC Pediatric Dentistry. Patients underwent specialist examination, first and second radiographic investigations were prescribed based on clinical need and hence dental care plans were drawn up in collaboration with the pediatric specialist.
On the sample of 20 patients were carried out the following:
- 35 tartar ablations
- 20 germectomies of thirds molar
- 15 simple extracts of deciduous teeth
- 5 surgical operations for canines included
- 8 frenulectomies
- 3 extractions of second molar deciluted anchilosate.
Pharmacological management of the patient in childhood evolutionary age with OI
The therapeutic use of BP in compliance with a scientifically validated protocol is evaluated in relation to a clinical history that has one of the following conditions occurring in the two years prior to observation:
- 3 long bone fractures
- 1 vertebral fracture
- 1 long bones fracture and 1 or more vertebral fractures
- 2 long bones fracture and 1 or more vertebral fractures.
With one long bone fracture therapy is not initiated and the patient is kept under control. The BP certificated in Italy is neridronate (Nerixia®) (21), administered intravenously to quarterly cycles.
Pre-and postoperative management
For the surgical management of interventions that affect the oral cavity of the childhood patient with OI we followed the recommendations of the Consensus Conference 2010 held in Rome on the Management of the Lower Third Molar (22).
In patients with OI, antibiotic prophylaxis is performed not for the risk of developing onj but for the risk of getting into a bacterial endocarditis (EB).
In support of the recommendations outlined by the Consensus Conference we also followed the guidelines of the European Society of Cardiology (ESC) 2015 for the management of infectious endocarditis (Table 1) (23).
Table 1.
Guidelines of the European Society of Cardiology 2015.
| Single-dose 30–60 minutes before the procedure | |||
|---|---|---|---|
| Situation | Antibiotic | Adults | Children |
| No allergy to penicillin or ampicillin | Amoxicillin or ampicillin | 2 g p os o i.v. | 50 mg/kg p os o i.v. |
|
| |||
| Allergy to penicillin or ampicillin | Clindamycin | 600 mg p os o i.v. | 20 mg/kg p os o i.v. |
Clinical examples
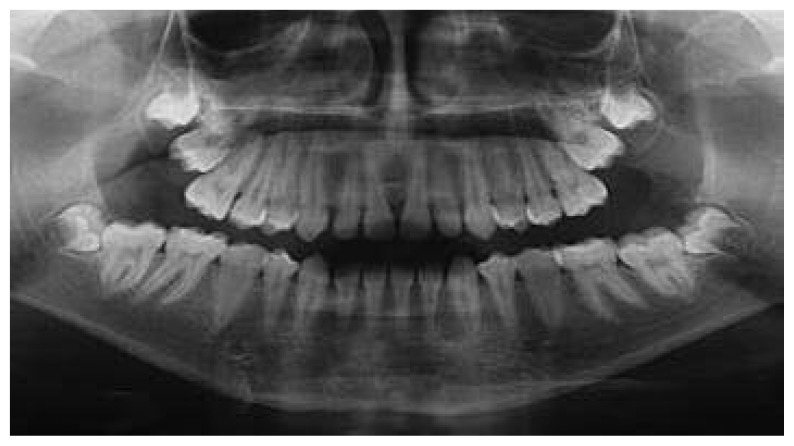
Patient of 14 years old, affected by OI and in treatment with nerhydrate since 2007, in which it was necessary to program the extraction of all four gemstones of thirds molar, 1.8, 2.8, 3.8, 4.8 in order to allow the correct eruption of the sevens (Figure 1). The patient suspended the BP during the period of the surgery and performed antibiotic prophylaxis. The patient was subjected to semi-annual checks. A control Rx opt was performed at two years, in which it is possible to observe the correct eruption of the permanent molar seconds and the normal alveolar bone architecture (Figure 2).
Figure 1.
Rx OPT case 1 initial.
Figure 2.
Rx OPT case 1 after 2 years.
Patients of 12 years old with type I OI, affected by Imperfect Dentinogenesis, has been treated with neridronate since 2006 and has undergone orthodontic treatment initiated at the age of 9 years, it was necessary to perform the germectomy of 3.8 (Figure 3). The patient suspended BP and performed antibiotic prophylaxis. The patient was subjected to semi-annual inspections, performed a first two-year control Rx opt and another one at 5 years old, in which the normal architecture of the alveolar bone is highlighted, the correct eruption of the sevens and the need to program the surgical extraction of 4.8 (Figure 4) in the future.
Figure 3.
Rx OPT case 2 initial.
Figure 4.
Rx OPT case 1 after 5 years.
Results and conclusions
Based on the clinical experiences of the patients recruited at the Umberto I, University Hospital of Rome, Head and Neck Department, UOC Pediatric Dentistry, and based on the literature review, it is not yet possible to define scientifically validated protocols or guidelines for the management of the developing age patient with OI that needs oral surgery.
However, to date, experience had on these patients are encouraging as they have not encountered particular post-operative complications compared to patients with OI.
The procedures performed on this sample are summarized in Table 2.
Table 2.
Procedures performed by UOC Pediatric Dentistry.
| Therapeutic procedures | BP Suspension | Prophylactic Antibiotic | Type of Intervention | Post-operative Management |
|---|---|---|---|---|
| Germectomy | YES | YES | COMPLEX | YES Analgesic therapy and/or FANS |
| Simple extraction | NO | NO | SIMPLE | NO |
| Anchilotic tooth extraction | NO | YES | COMPLEX | YES |
| Frenulectomy | NO | NO | SIMPLE | NO |
| Operculum | NO | NO | SIMPLE | YES |
| Abt | NO | NO | SIMPLE | NO |
| Orthodontic mini-implants | NO | YES | COMPLEX | YES |
With this experience, we showed that a proper patient management from the medical and dental point of view can protect these patients from the risk of post-operative problems, such as onj, soft tissue flogos, intraoral and extraoral fistulas, failure to heal the post-extractive alveolus, infections, post-operative pain and pathological fractures. The follow-up, ranging from a minimum of 2 years to a maximum of 5 years, have not demonstrated the presence of particular complications or healing defects.
In the management of these patients, it must be constant the collaboration with the pediatric specialist in order to optimize the response time according to drug therapy, monitor healing with close controls, assess the actual need for some interventions, assess the risks of complications, (24) perform remote follow-up.
References
- 1.Ben Amor M, Rauch F, Monti E, et al. Osteogenesis imperfecta. Pediatr Endocrinol Rev. 2013;10:397–405. [PubMed] [Google Scholar]
- 2.Sillence DO. Osteogenesis imperfecta: an expanding panorama of variants. Clin Orthop. 1981;159:11–25. [PubMed] [Google Scholar]
- 3.Greggio NA, Rigon F, Zacchello F. Osteogenesi Imperfetta. Osteopatie Pediatriche Emergenti. 2003;5:139–52. [Google Scholar]
- 4.Monti E, Mottes M, Fraschini P, et al. Current and emerging treatments for the management of osteogenesis imperfect. Ther Clin Risk Manag. 2010;6:367–381. doi: 10.2147/tcrm.s5932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Russell RGG, Watts NB, Ebetino FH, et al. Mechanism of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int. 2008;19:733–759. doi: 10.1007/s00198-007-0540-8. [DOI] [PubMed] [Google Scholar]
- 6.Bedogni, Campisi, Fusco, Agrillo . Raccomandazioni clinico-terapeutiche sull’osteonecrosi delle ossa mascellari associata a bisfosfonati e sua prevenzione. SICMF-SIPMO; 2013. [Google Scholar]
- 7.Hennedige AA, Jayasinghe J, Khajeh J, Macfarlane TV. Systematic Review on the Incidence of Bisphosphonate Related Osteonecrosis of the Jaw in Children Diagnosed with Osteogenesis Imperfecta. J Oral Maxillofac Res. 2013 doi: 10.5037/jomr.2013.4401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malmgren B, Astrom E, Soderhall S. No osteonecrosis in jaws of young patients with osteogenesis imperfecta treated with bisphosphonates. J Oral Pathol Med. 2008;37:196–200. doi: 10.1111/j.1600-0714.2007.00607.x. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz S, Joseph C, Iera D, Vu DD. Bisphosphonates, Osteonecrosis, Osteogenesis Imperfecta and Dental Extractions: A Case Series. J Can Dent Assoc. 2008 Jul-Aug;74(6):537–42. [PubMed] [Google Scholar]
- 10.Chahine C, Cheung MS, Head TW, Schwartz S, Glorieux FH, Rauch F. Tooth Extraction Socket Healing in Pediatric Patients Treated with Intravenous Pamidronate. J Pediatr. 2008;153:719–20. doi: 10.1016/j.jpeds.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Bhatt RN, Hibbert SA, Munns CF. The use of bisphosphonates in children: review of the literature and guidelines for dental management. Aust Dent J. 2014;59(1):9–19. doi: 10.1111/adj.12140. [DOI] [PubMed] [Google Scholar]
- 12.Maines E, Monti E, Doro F, Morandi G, Cavarzere P, Antoniazzi F. Children and adolescents treated with neridronate for osteogenesis imperfecta show no evidence of any osteonecrosis of the jaw. J Bone Miner Metab. 2012;30:434–438. doi: 10.1007/s00774-011-0331-3. [DOI] [PubMed] [Google Scholar]
- 13.Capasso F, Panetta F, Ierardo G, Parisella V, Polimeni A. Klinefelter syndrome: Case report. Oral Implantol (Rome) 2009 Jul;2(3):27–36. Epub 2010 Apr 20. [PMC free article] [PubMed] [Google Scholar]
- 14.Ierardo G, Luzzi V, Panetta F, Sfasciotti GL, Polimeni A. Noonan syndrome: A case report. Eur J Paediatr Dent. 2010 Jun;11(2):97–100. [PubMed] [Google Scholar]
- 15.Fadda MT, Ierardo G, Ladniak B, Di Giorgio G, Caporlingua A, Raponi I, Silvestri A. Treatment timing and multidisciplinary approach in Apert syndrome. Group of Apert syndrome, Policlinico Umberto I, “Sapienza” University of Rome, Italy. Ann Stomatol (Roma) 2015 Jul 28;6(2):58–63. eCollection 2015 Apr–Jun. [PMC free article] [PubMed] [Google Scholar]
- 16.Ierardo G, Luzzi V, Nardacci G, Vozza I, Polimeni A. Minimally invasive orthodontics: elastodontic therapy in a growing patient affected by Dentinogenesis Imperfecta. Ann Stomatol (Roma) 2017 Jul 3;8(1):34–38. doi: 10.11138/ads/2017.8.1.034. eCollection 2017 Jan–Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ierardo G, Calcagnile F, Luzzi V, Ladniak B, Bossu M, Celli M, Zambrano A, Franchi L, Polimeni A. Osteogenesis imperfecta and rapid maxillary expansion: Report of 3 patients. Am J Orthod Dentofacial Orthop. 2015 Jul;148(1):130–7. doi: 10.1016/j.ajodo.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 18.Ierardo G, Luzzi V, Vestri A, Sfasciotti GL, Polimeni A. Evaluation of customer satisfaction at the Department of Paediatric Dentistry of “Sapienza” University of Rome. Eur J Paediatr Dent. 2008 Mar;9(1):30–6. [PubMed] [Google Scholar]
- 19.Annibali S, Pippi R, Sfasciotti GL. Chirurgia orale a scopo ortodontico. Elsevier - Masson; 2007. [Google Scholar]
- 20.Panzoni E. Chirurgia Estrattiva: Masson; 1986. [Google Scholar]
- 21.Bibliografia Nerixia® Abiogen Pharma. Foglietto illustrativo. Aprile. 2002. [Google Scholar]
- 22.Annibali S, De biase A, Pippi R, Sfasciotti GL. A Consensus Conference on management of the lower third molar. Reviews Minerva Stomatologica. 2011;60:509–527. [PubMed] [Google Scholar]
- 23.European Heart Journal Advance Access published August 29, 2015
- 24.Saccucci M, Ierardo G, Protano C, Vitali M, Polimeni A. How to manage the biological risk in a dental clinic: state of the art and future perspectives. Minerva Stomatol. 2017 Jun 23; doi: 10.23736/S0026-4970.17.04087-0. [DOI] [PubMed] [Google Scholar]