Abstract
Background:
Despite multiple benefits, laparoscopic surgery always poses anesthetic challenge due to significant alteration of hemodynamics. Various pharmacological agents have been used for the same with variable response. Dexmedetomidine, in addition to sympatholytic effect, diminishes intraoperative requirement of anesthetics including propofol. The present study was conducted to evaluate the effects of intravenous dexmedetomidine on intraoperative hemodynamics and propofol requirement using bispectral index (BIS) in laparoscopic cholecystectomy.
Methods:
Forty patients undergoing laparoscopic cholecystectomy were randomly allocated to receive either dexmedetomidine (Group A; n = 20) or normal saline (Group B; n = 20). In Group A, dexmedetomidine was loaded (1 μg/kg) before anesthesia induction and infused (0.6 μg/kg/h) during surgery. Anesthesia was induced with propofol, and maintenance infusion rate was adjusted to a BIS of 55–60 in both groups. Mean arterial pressure (MAP) and heart rate (HR) were recorded at baseline and at various time points from loading of drugs to just after tracheal extubation. All infusions were stopped with removal of scope from abdominal cavity. Recovery time (time from end of all infusions to BIS = 80) and extubation time (time from end of all infusions to extubation) were noted.
Results:
After intubation, MAP and HR values in Group A were significantly lower than Group B at various time points of study. To achieve similar BIS values, significantly low doses of propofol were required in Group A during induction and intraoperatively. Doses were reduced by 36% and 31%, respectively. Mean recovery time and mean extubation time in Group A were also significantly less.
Conclusion:
During propofol-based anesthesia for laparoscopic cholecystectomy, dexmedetomidine provides stable intraoperative hemodynamics and reduces propofol requirement for induction as well as maintenance, without compromising recovery profile.
Keywords: Dexmedetomidine, hemodynamics, laparoscopic cholecystectomy, propofol
INTRODUCTION
Laparoscopic cholecystectomy is one of the most frequently performed laparoscopic surgeries nowadays. Since the introduction of diagnostic laparoscopic procedures in the early 1970s and the first laparoscopic cholecystectomy procedures in the late 1980s,[1] laparoscopy has expanded impressively both in scope and volume. Increasing success of laparoscopic surgery can be attributed to the fact that it results in multiple benefits compared with open procedures, such as reduced trauma to patient, disturbance of homeostasis, morbidity, mortality, recovery time and hospital stay, with consequent reductions in healthcare costs.[2,3] Efforts have been made to use the laparoscopic approach for gastrointestinal (e.g., colonic, gastric, splenic, hepatic surgery), gynecologic (e.g., hysterectomy), urologic (e.g., nephrectomy, prostatectomy), and vascular (e.g., aortic) procedures.
Despite multiple benefits, any laparoscopic surgery always poses a challenge to its successful anesthetic management, mainly due to significant alteration of hemodynamics, resulting from the combined effects of pneumoperitoneum, patient position, anesthesia, and hypercapnia from the absorbed CO2 that is used to produce pneumoperitoneum. Pneumoperitoneum creation (increased intra-abdominal pressure) is immediately followed by an increased plasma renin activity and increase in plasma levels of norepinephrine and epinephrine.[4] The renin–angiotensin–aldosterone system is also activated. All these changes collectively lead to an elevated arterial pressure, increased systemic and pulmonary vascular resistance, and decreased cardiac output.[5]
Various agents such as isoflurane,[4] propofol, β-blockers,[6] and antihypertensives[7,8] have been used to reduce hemodynamic changes associated with laparoscopic surgery with variable response. Effects of α2-adrenergic agonist clonidine have also been studied widely.[9,10] These may reduce anesthetic and analgesic requirements, promote perioperative hemodynamic stability, reduce myocardial ischemia, improve renal function, provide sedation and anxiolysis, and attenuate neurohumoral “stress response” of major surgery.[11] These may reduce circulating catecholamines level during surgery.
Dexmedetomidine, which is the pharmacologically active dextro-isomer of medetomidine, is a newer highly selective α2-adrenergic agonist, approved by Food and Drug Administration (FDA) in 1999.[12] It has a ten-fold greater α2:α1 receptor selectivity and has a shorter duration of action than clonidine.[11] It possesses hypnotic, sedative, anxiolytic, sympatholytic, and analgesic properties without producing significant respiratory depression.[13] It also diminishes intraoperative requirement of analgesics[14] and anesthetics (including propofol).[15,16,17,18,19] These properties make it theoretically a suitable agent for use as a part of an anesthetic regimen.[11] However, fewer studies are available on the propofol-sparing effect of dexmedetomidine during laparoscopic cholecystectomy.
In October 1996, bispectral index (BIS) achieved approval by the FDA as the first electroencephalogram (EEG)-based monitor of anesthetic effect. BIS reduces complex EEG processing to a simple number ranging from 100 to 0. BIS decreases with increasing depth of anesthesia, and adequate level of anesthesia is achieved with BIS ranging from 40 to 60. BIS monitoring allows reduction in the total amount of anesthetic that patients are exposed to and appears to decrease time for emergence and recovery.[20]
The primary aim of this study was to evaluate the effect of intravenous (i.v.) dexmedetomidine on intraoperative hemodynamic response to critical incidences such as laryngoscopy, endotracheal intubation, pneumoperitoneum creation, and extubation in patients undergoing laparoscopic cholecystectomy. The secondary aims were to observe the effect on BIS-guided propofol requirement, extubation time, and occurrence of adverse effects.
METHODS
The present study was conducted from May 2012 to September 2012, with due permission and approval of Local Ethical Committee and after obtaining informed written consent from all the patients. It was a prospective, randomized, double-blind, placebo-controlled clinical study. Forty patients of American Society of Anesthesiologists (ASA) physical status classes I and II between 40 and 50 years of age with body weight 60–70 kg of either sex and posted for laparoscopic cholecystectomy under general anesthesia were included in the study. Patients with decreased autonomic control such as the elderly, diabetic patients, patients with preoperative hypotension or bradycardia or dysrhythmia, patients with chronic hypertension or severe cardiac disease or heart block, patients on drugs such as beta blockers or calcium channel blockers, patients with anticipated difficult intubation, obese patients, patients with history of sleep apnea, anemic patients, patients with impaired renal or hepatic function, pregnant or lactating women, patients with history of alcohol or drug abuse, and patients with history of allergy to egg proteins and drugs were not considered for the study.
The patients were randomly allocated by chit and box method into two groups of twenty patients each, Group A (patients receiving dexmedetomidine preloading 1 μg/kg followed by infusion 0.6 μg/kg/hr) and Group B (patients receiving normal saline 0.9% preloading followed by infusion at similar rates).
Infusion was prepared by a separate anesthetist in a separate room according to the group allotted. To prepare the infusion, dexmedetomidine 2 mL containing 200 μg of the drug was withdrawn in a 50 mL syringe and was diluted up to 50 mL with normal saline resulting in the final concentration of 4 μg/mL. Dexmedetomidine or normal saline infusion was given through a syringe infusion pump. Depending on the weight of the patient, the pump was set so as to deliver the targeted infusion rate. Thus, the syringe and volume of prepared solution were similar in both groups, and the assessor as well as the patient was unaware of the group. Decoding of blinding to the assessor was done only at the time of tabulation and result analysis.
After taking the patient on the operation table, a multipara monitor with BIS module was attached, and the baseline pulse rate (PR) and mean arterial pressure (MAP) were noted down (T – Ctrl). A wide bore i.v. cannula was inserted for giving the i.v. fluids, and another line was taken up for the infusion pump. Test drug preloading was done over 10 min, and then, infusion pump was set to deliver targeted intraoperative infusion rate which was continued till removal of scope from the abdominal cavity. PR and MAP were noted down after drug preloading (T – Load). Premedication was administered before induction of anesthesia to all the patients in the form of injection glycopyrrolate 0.005 mg/kg i.v., injection fentanyl citrate 2 μg/kg i.v., injection ranitidine 50 mg i.v., and injection ondansetron 4 mg i.v. as per the institutional protocol. Injection diclofenac (aqueous) 75 mg was added to i.v. fluid drip.
Five minutes after starting the drug infusion at targeted intraoperative rate, preoxygenation was performed for 3 min. Patients were induced with injection propofol i.v. infused slowly 20 mg (2 mL) every 5 s till BIS value reached below 60 followed by i.v. injection atracurium besylate 0.5 mg/kg. Patient was ventilated with 100% O2 for 150 s. PR and MAP were recorded just before intubation (T – Ind). Trachea was intubated with appropriate size-cuffed endotracheal tube after direct laryngoscopy. Tube position was confirmed by auscultation and ETCO2. PR and MAP were recorded just after intubation (T – Int). Anesthesia was maintained with O2:N2O (50:50), injection propofol i.v. infusion titrated to maintain BIS value 55–60 and injection atracurium besylate i.v. as a muscle relaxant. Intra-abdominal pressure was maintained between 12 and 14 mm Hg throughout the laparoscopic procedure. The patients were mechanically ventilated using circle system to keep the ETCO2 between 35 and 45 mm Hg. Drug infusion and anesthetic agents were stopped as soon as the scope was taken out of the abdominal cavity. Reversal and extubation were carried out by conventional methods.
All patients were monitored intraoperatively for vital parameters at regular intervals. PR and MAP were recorded at surgical incision (T – Inc), just after insufflation (T – Ins), 15 min after insufflation (T – Ins15), 30 min after insufflation (T – Ins30), at exsufflation (T – Exs), just after reversal (T – Rev), and just after extubation (T – Ext). Extubation was considered end point of our study. Patients were also observed for time to achieve BIS value 80 (recovery time) and time to extubate trachea (extubation time) from stoppage of anesthetic agents. Mean propofol maintenance infusion rate was calculated. Finally, the patient was shifted to the recovery room.
The results were tabulated and statistically analyzed using SPSS (Statistical Package for Social Sciences) Software version 17.0.0 (SPSS Inc., Chicago, Illinois, USA). The normality of the data distributions was evaluated using the Shapiro–Wilk test. Groups were compared for demographic data (age, weight), duration of surgery, volume of intravascular fluids administered intraoperatively, propofol required for induction, propofol maintenance infusion rate, recovery time, and extubation time by a Student's t-test. Categorical data, i.e., sex and ASA physical status class were compared between groups using Chi-square test. Intergroup differences in the data collected at each measured time point were determined using a Student's t-test and intragroup differences from baseline within each group were determined by a paired t-test. Results were expressed as mean ± standard deviation. P < 0.05 was considered statistically significant.
RESULTS
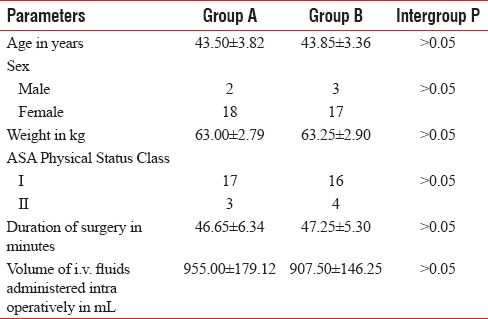
Both groups under study were comparable to each other with respect to age, sex, weight, ASA physical status class, duration of surgery, and volume of i.v. fluids administered intraoperatively [Table 1]. The mean age of the patients was 43.68 years (range - 40–50 years). The mean weight of the patients was 63.13 kg (range - 60–70 kg). There was no significant difference between the groups in reference to the baseline PR and the MAP.
Table 1.
Demographic characteristics, duration of surgery, and volume of intravenous fluids administered intraoperatively
The mean PR in Group B increased significantly just after intubation and thereafter remained above baseline throughout, with significant differences just after insufflation, 15 min after insufflation, and just after extubation. In Group A, the mean PR decreased significantly from baseline just after test drug preloading and remained significantly low at all time points till exsufflation; after which, it gradually increased and returned to baseline just after extubation. When the mean PRs at different time points were compared in both groups, values in Group A were lower than in Group B, and significant differences were found at all time points [Table 2 and Figure 1].
Table 2.
Mean pulse rate (beats per minute) at different time – points of study
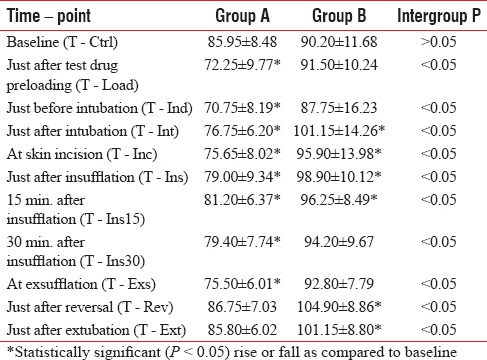
Figure 1.
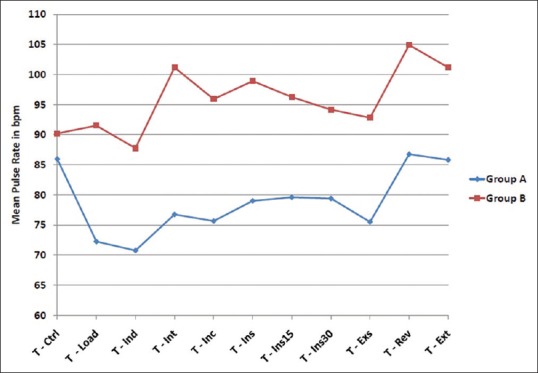
Trends of mean pulse rates at different time points of study in both groups
There was a significant fall in the average of MAP in Group B just before intubation, but it increased significantly above baseline after intubation, and thereafter, it remained above baseline at all time points, with significant differences just after insufflation, 15 and 30 min after insufflation, after exsufflation, and just after extubation. In Group A, the average of MAP decreased significantly below baseline just before intubation, but it gradually increased and crossed baseline just after insufflation. It decreased after exsufflation, but it again increased and crossed baseline just after extubation. No significant difference was seen at any time point except just after induction. When the averages of MAP at different time points were compared in both groups, values in Group A were lower than in Group B, and significant differences were found just after intubation, just after insufflation, 30 min after insufflation, after exsufflation, and just after extubation [Table 3 and Figure 2].
Table 3.
Average of mean arterial pressure (mm Hg) at different time – points of study
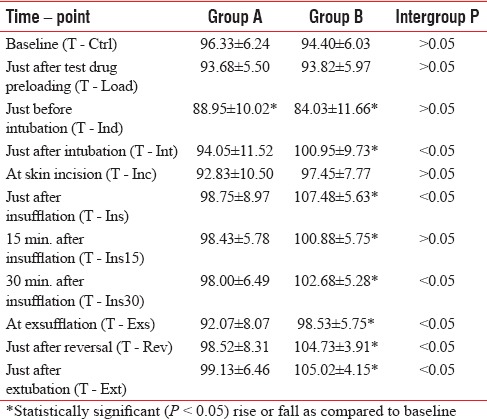
Figure 2.
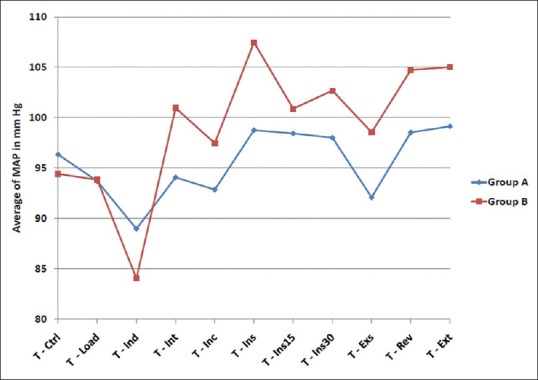
Trends of average of mean arterial pressure at different time points of study in both groups
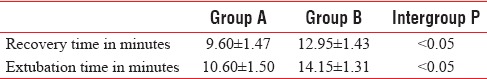
The mean recovery time in Group A was significantly less than that in Group B (9.60 ± 1.47 vs. 12.95 ± 1.43 min). Similarly, the mean extubation time in Group A was significantly less than that in Group B (10.60 ± 1.50 vs. 14.15 ± 1.31 min) [Table 4].
Table 4.
Recovery time and extubation time
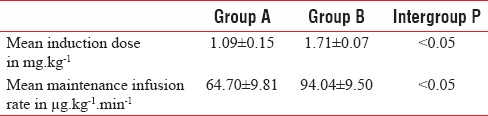
To achieve similar BIS values, significantly low doses of propofol were required in Group A as compared to Group B during induction (1.09 ± 0.15 vs. 1.71 ± 0.07 mg/kg) and intraoperatively (64.70 ± 9.81 vs. 94.04 ± 9.50 μg/kg/min). The induction and intraoperative maintenance doses were reduced by 36% and 31%, respectively [Table 5].
Table 5.
Propofol required for induction and maintenance of anaesthesia
DISCUSSION
The hemodynamic alterations due to intense sympathetic stimulation accompanying laparoscopic surgery comprising of elevation in heart rate and rise in mean arterial pressure are well known. The potential for life-threatening complications associated with such a response is also well documented. There exists a strong relationship of both perioperative myocardial ischemia and postoperative myocardial infarction with anesthetic and surgical events known to produce intense sympathetic stimulation, with or without hemodynamic abnormalities.[21] Thus, it is logical to look for methods to reduce sympathetic stimulation per se.
Various drugs and methods had been studied to prevent hemodynamic alterations due to stress of surgery and anesthesia. Dexmedetomidine, a highly selective α2-agonist, has also been evaluated in the past for attenuation of hemodynamic responses in various doses and along with various anesthetic regimens for various types of surgeries.[11,15,19] Gynecologic diagnostic laparoscopy was the first laparoscopic procedure in which the effects of dexmedetomidine were studied with encouraging results.[22] Since then, the molecule has been widely used to assess its effect on hemodynamic responses in patients undergoing various types of laparoscopic surgeries, including laparoscopic cholecystectomy.[14,23,24,25,26,27,28,29,30,31]
Our study confirms the fact that stressful events such as laryngoscopy and endotracheal intubation, pneumoperitoneum, and extubation do lead to significant increase in PR and MAP in patients undergoing laparoscopic cholecystectomy[4,26,29,30,31,32] as seen in normal saline group. This sympathoadrenal response is effectively attenuated by used doses of dexmedetomidine providing intraoperative hemodynamic stability[14,26,29,30,31,32] as seen in dexmedetomidine group. Although there was significant decrease in PR from baseline in dexmedetomidine group, significant bradycardia was not noted in any case.
It may be hypothesized that dexmedetomidine, due to its sedative effect, can delay patients’ response to verbal command leading to prolongation of extubation time. Ohtani et al., based on their findings that sevoflurane produced a shorter time to eye opening than propofol when coadministered with dexmedetomidine, suggested that dexmedetomidine may delay recovery when given as an adjuvant to propofol during total i.v. anesthesia.[33] However, in our study, recovery time as well as extubation time was found to be significantly less in dexmedetomidine group. This could be explained to some degree by the decreased requirement of propofol because of dexmedetomidine. It also might be because of the ability of dexmedetomidine to provide sedation without affecting respiratory function. Afanador et al.[34] and Bajwa et al.[35] also, in their respective studies, observed significantly reduced extubation time in patients who were given dexmedetomidine. Bhattacharjee et al.[14] and Kang et al.[19] observed no significant effect of dexmedetomidine on response to verbal command and extubation time; however, the extubation time in dexmedetomidine group was less than in placebo in both studies.
Propofol is a frequently used i.v. anesthetic agent for induction and maintenance of anesthesia during laparoscopic surgery. Although known for its remarkable safety, various recent literatures and evidences have suggested about the potential for intraoperative complications even with short-term infusions.[36,37,38,39] Hence, there is tendency to use another adjuvant having sedative properties that could reduce the requirement of propofol.
With the use of dexmedetomidine, the induction and intraoperative maintenance doses in our study were reduced by 36% and 31%, respectively. This could be explained by the sedative effect of dexmedetomidine, which could allow inducing hypnosis with a reduction in anesthetic drug doses. Our findings substantiate those of previous researchers who also observed significant dose-sparing effect of dexmedetomidine on various anesthetics in their respective studies.[19,31,34,35]
One of the limitations of our study was the use of BIS, which provides minimum information regarding analgesia, for measuring depth of anesthesia. Furthermore, the administration of muscle relaxants was in the form of time-bound boluses and not guided by neuromuscular monitoring.
CONCLUSION
During propofol-based anesthesia for laparoscopic cholecystectomy, dexmedetomidine provides more stable intraoperative hemodynamics and reduces the requirement of propofol for induction as well as maintenance, without compromising the recovery profile.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Dubois F, Icard P, Berthelot G, Levard H. Coelioscopic cholecystectomy. Preliminary report of 36 cases. Ann Surg. 1990;211:60–2. doi: 10.1097/00000658-199001000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grace PA, Quereshi A, Coleman J, Keane R, McEntee G, Broe P, et al. Reduced postoperative hospitalization after laparoscopic cholecystectomy. Br J Surg. 1991;78:160–2. doi: 10.1002/bjs.1800780209. [DOI] [PubMed] [Google Scholar]
- 3.Joris J, Cigarini I, Legrand M, Jacquet N, De Groote D, Franchimont P, et al. Metabolic and respiratory changes after cholecystectomy performed via laparotomy or laparoscopy. Br J Anaesth. 1992;69:341–5. doi: 10.1093/bja/69.4.341. [DOI] [PubMed] [Google Scholar]
- 4.Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg. 1993;76:1067–71. doi: 10.1213/00000539-199305000-00027. [DOI] [PubMed] [Google Scholar]
- 5.Lenz RJ, Thomas TA, Wilkins DG. Cardiovascular changes during laparoscopy. Studies of stroke volume and cardiac output using impedance cardiography. Anaesthesia. 1976;31:4–12. doi: 10.1111/j.1365-2044.1976.tb11738.x. [DOI] [PubMed] [Google Scholar]
- 6.Koivusalo AM, Scheinin M, Tikkanen I, Yli-Suomu T, Ristkari S, Laakso J, et al. Effects of esmolol on haemodynamic response to CO2 pneumoperitoneum for laparoscopic surgery. Acta Anaesthesiol Scand. 1998;42:510–7. doi: 10.1111/j.1399-6576.1998.tb05159.x. [DOI] [PubMed] [Google Scholar]
- 7.Feig BW, Berger DH, Dougherty TB, Dupuis JF, Hsi B, Hickey RC, et al. Pharmacologic intervention can reestablish baseline hemodynamic parameters during laparoscopy. Surgery. 1994;116:733–9. [PubMed] [Google Scholar]
- 8.Joris JL, Hamoir EE, Hartstein GM, Meurisse MR, Hubert BM, Charlier CJ, et al. Hemodynamic changes and catecholamine release during laparoscopic adrenalectomy for pheochromocytoma. Anesth Analg. 1999;88:16–21. doi: 10.1097/00000539-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Joris JL, Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML. Hemodynamic changes induced by laparoscopy and their endocrine correlates: Effects of clonidine. J Am Coll Cardiol. 1998;32:1389–96. doi: 10.1016/s0735-1097(98)00406-9. [DOI] [PubMed] [Google Scholar]
- 10.Laisalmi M, Koivusalo AM, Valta P, Tikkanen I, Lindgren L. Clonidine provides opioid-sparing effect, stable hemodynamics, and renal integrity during laparoscopic cholecystectomy. Surg Endosc. 2001;15:1331–5. doi: 10.1007/s004640090126. [DOI] [PubMed] [Google Scholar]
- 11.Jalonen J, Hynynen M, Kuitunen A, Heikkilä H, Perttilä J, Salmenperä M, et al. Dexmedetomidine as an anesthetic adjunct in coronary artery bypass grafting. Anesthesiology. 1997;86:331–45. doi: 10.1097/00000542-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Yazbek-Karam VG, Aouad MM. Perioperative uses of dexmedetomidine. Middle East J Anaesthesiol. 2006;18:1043–58. [PubMed] [Google Scholar]
- 13.Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000;90:699–705. doi: 10.1097/00000539-200003000-00035. [DOI] [PubMed] [Google Scholar]
- 14.Bhattacharjee DP, Nayek SK, Dawn S, Bandopadhyay G, Gupta K. Effects of dexmedetomidine on hemodynamics in patients undergoing laparoscopic cholecystectomy – A comparative study. J Anaesth Clin Pharmacol. 2010;26:45–8. [Google Scholar]
- 15.Aantaa R, Kanto J, Scheinin M, Kallio A, Scheinin H. Dexmedetomidine, an alpha 2-adrenoceptor agonist, reduces anesthetic requirements for patients undergoing minor gynecologic surgery. Anesthesiology. 1990;73:230–5. doi: 10.1097/00000542-199008000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Khan ZP, Munday IT, Jones RM, Thornton C, Mant TG, Amin D. Effects of dexmedetomidine on isoflurane requirements in healthy volunteers 1: Pharmacodynamic and pharmacokinetic interactions. Br J Anaesth. 1999;83:372–80. doi: 10.1093/bja/83.3.372. [DOI] [PubMed] [Google Scholar]
- 17.Dutta S, Karol MD, Cohen T, Jones RM, Mant T. Effect of dexmedetomidine on propofol requirements in healthy subjects. J Pharm Sci. 2001;90:172–81. doi: 10.1002/1520-6017(200102)90:2<172::aid-jps8>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 18.Ngwenyama NE, Anderson J, Hoernschemeyer DG, Tobias JD. Effects of dexmedetomidine on propofol and remifentanil infusion rates during total intravenous anesthesia for spine surgery in adolescents. Paediatr Anaesth. 2008;18:1190–5. doi: 10.1111/j.1460-9592.2008.02787.x. [DOI] [PubMed] [Google Scholar]
- 19.Kang WS, Kim SY, Son JC, Kim JD, Muhammad HB, Kim SH, et al. The effect of dexmedetomidine on the adjuvant propofol requirement and intra operative hemodynamics during remifentanil-based anesthesia. Korean J Anesthesiol. 2012;62:113–8. doi: 10.4097/kjae.2012.62.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mansour EE. BIS-guided evaluation of dexmedetomidine vs. midazolam as anaesthetic adjuncts in off-pump coronary artery bypass surgery (OPCAB) Saudi J Anaesth. 2009;3:7–14. [Google Scholar]
- 21.Slogoff S, Keats AS. Does perioperative myocardial ischemia lead to postoperative myocardial infarction? Anesthesiology. 1985;62:107–14. doi: 10.1097/00000542-198502000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Aho M, Scheinin M, Lehtinen AM, Erkola O, Vuorinen J, Korttila K. Intramuscularly administered dexmedetomidine attenuates hemodynamic and stress hormone responses to gynecologic laparoscopy. Anesth Analg. 1992;75:932–9. [PubMed] [Google Scholar]
- 23.Feld JM, Hoffman WE, Stechert MM, Hoffman IW, Ananda RC. Fentanyl or dexmedetomidine combined with desflurane for bariatric surgery. J Clin Anesth. 2006;18:24–8. doi: 10.1016/j.jclinane.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 24.Ramsay MA, Saha D, Hebeler RF. Tracheal resection in the morbidly obese patient: The role of dexmedetomidine. J Clin Anesth. 2006;18:452–4. doi: 10.1016/j.jclinane.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Tufanogullari B, White PF, Peixoto MP, Kianpour D, Lacour T, Griffin J, et al. Dexmedetomidine infusion during laparoscopic bariatric surgery: The effect on recovery outcome variables. Anesth Analg. 2008;106:1741–8. doi: 10.1213/ane.0b013e318172c47c. [DOI] [PubMed] [Google Scholar]
- 26.Manne GR, Upadhyay MR, Swadia V. Effects of low dose dexmedetomidine infusion on haemodynamic stress response, sedation and post-operative analgesia requirement in patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2014;58:726–31. doi: 10.4103/0019-5049.147164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chauhan Y, Parikh H. Effects of dexmedetomidine on hemodynamics in patients undergoing laproscopic surgeries under general anaesthesia – A comparative study. Indian J Appl Res. 2014;4:70–2. [Google Scholar]
- 28.Vora KS, Baranda U, Shah VR, Modi M, Parikh GP, Butala BP. The effects of dexmedetomidine on attenuation of hemodynamic changes and there effects as adjuvant in anesthesia during laparoscopic surgeries. Saudi J Anaesth. 2015;9:386–92. doi: 10.4103/1658-354X.159461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Laxmi Narsaiah G, Murali CH, Srinivasa Rao B, Praveeen Kumar D, Saravan Kumar G. Haemodynamic effects of low dose dexmedetomidine infusion in patients undergoing laparoscopic cholecystectomy – A randomized study. Sch J App Med Sci. 2016;4:1736–40. [Google Scholar]
- 30.Chavan SG, Shinde GP, Adivarekar SP, Gujar SH, Mandhyan S. Effects of dexmedetomidine on perioperative monitoring parameters and recovery in patients undergoing laparoscopic cholecystectomy. Anesth Essays Res. 2016;10:278–83. doi: 10.4103/0259-1162.171460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anjum N, Tabish H, Debdas S, Bani HP, Rajat C, Anjana Basu GD. Effects of dexmedetomidine and clonidine as propofol adjuvants on intra-operative hemodynamics and recovery profiles in patients undergoing laparoscopic cholecystectomy: A prospective randomized comparative study. Avicenna J Med. 2015;5:67–73. doi: 10.4103/2231-0770.160231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Indian J Anaesth. 2011;55:352–7. doi: 10.4103/0019-5049.84846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ohtani N, Kida K, Shoji K, Yasui Y, Masaki E. Recovery profiles from dexmedetomidine as a general anesthetic adjuvant in patients undergoing lower abdominal surgery. Anesth Analg. 2008;107:1871–4. doi: 10.1213/ane.0b013e3181887fcc. [DOI] [PubMed] [Google Scholar]
- 34.Afanador C, Marulanda L, Torres G, Marín A, Vidal C, Silva G. Effect of intraoperative use of dexmedetomidine on anesthetic requirements and time to tracheal extubation in elective adult heart surgery patients. A retrospective cohort study. Internet J Anesthesiol. 2009;22:2. [Google Scholar]
- 35.Bajwa SJ, Kaur J, Singh A, Parmar S, Singh G, Kulshrestha A, et al. Attenuation of pressor response and dose sparing of opioids and anaesthetics with pre-operative dexmedetomidine. Indian J Anaesth. 2012;56:123–8. doi: 10.4103/0019-5049.96303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burow BK, Johnson ME, Packer DL. Metabolic acidosis associated with propofol in the absence of other causative factors. Anesthesiology. 2004;101:239–41. doi: 10.1097/00000542-200407000-00035. [DOI] [PubMed] [Google Scholar]
- 37.Salengros JC, Velghe-Lenelle CE, Bollens R, Engelman E, Barvais L. Lactic acidosis during propofol-remifentanil anesthesia in an adult. Anesthesiology. 2004;101:241–3. doi: 10.1097/00000542-200407000-00036. [DOI] [PubMed] [Google Scholar]
- 38.Hatch DJ. Propofol-infusion syndrome in children. Lancet. 1999;353:1117–8. doi: 10.1016/S0140-6736(99)90018-1. [DOI] [PubMed] [Google Scholar]
- 39.Bray RJ. Propofol infusion syndrome in children. Paediatr Anaesth. 1998;8:491–9. doi: 10.1046/j.1460-9592.1998.00282.x. [DOI] [PubMed] [Google Scholar]


