Abstract
Nonalcoholic fatty liver disease (NAFLD) is rapidly becoming a major cause of chronic liver disease worldwide. Concurrent to an increase in NAFLD prevalence, there is an increase in the obesity epidemic and the correlated insulin-resistant state. It is a challenge to diagnose NAFLD because many patients are asymptomatic until the later stages of disease. The most common symptoms include fatigue, malaise, and discomfort in the right upper quadrant. The major and most accurate tool to clinically diagnose NAFLD is a liver biopsy, followed by histological analysis. However, this procedure is invasive and often carries a high risk of complications. Currently, there are no officially approved medications for the treatment of NAFLD. Although lifestyle modifications with proper diet and exercise have been shown to be beneficial, this has been difficult to achieve and sustain for many patients. Effective pharmacological treatments are still lacking; therefore, additional research to identify novel drugs is clearly warranted. PPARs are promising drug targets for the management of NAFLD and its related conditions of type 2 diabetes mellitus and cardiovascular disease. In this review, we provide an overview of recent studies on the association of PPARs and NAFLD.
1. Introduction
Nonalcoholic fatty liver disease (NAFLD) has been defined as hepatic steatosis without significant alcohol intake or other diseases [1]. It also has been defined as the hepatic manifestation of metabolic syndrome (MS), whose main symptoms include insulin resistance state, atherogenic dyslipidemia, abdominal obesity, and hypertension [1]. Currently, there is growing evidence that NAFLD is a multisystem disease, affecting extrahepatic organs [2]. NAFLD increases the risk of type 2 diabetes mellitus (T2DM), chronic kidney disease (CKD), and cardiac diseases, including cardiovascular disease (CVD) [2]. The pathological state of NAFLD results from high levels of circulating free fatty acids (FFAs), leading to accumulation of lipid deposits within hepatocytes that triggers steatosis. The clinical spectrum of NAFLD ranges from simple steatosis to steatohepatitis, bridging fibrosis, and cirrhosis [3]. The primary step in NAFLD is triglyceride accumulation in hepatocytes, which appears to be dependent on IR [4]. The second state involves hepatocellular injury, namely, nonalcoholic steatohepatitis (NASH), which includes many factors, including oxidative stress, increased proinflammatory cytokines, mitochondrial dysfunction, iron overload, bacterial overgrowth, and genetic predisposition [5]. Many NAFLD patients ultimately progress to liver cirrhosis and hepatocellular carcinoma [6, 7]. In recent studies, the pathophysiology of NAFLD was reported, including the theories of “two-hit” and “multiple parallel hit” [8, 9]. However, the precise mechanism involved in the development and progression of NAFLD is not completely understood.
2. Peroxisome Proliferator-Activated Receptors
2.1. PPARs Overview
Peroxisome proliferator-activated receptors (PPARs) are an important group of receptors that play a role in mediating the pleiotropic effects of diverse environmental contaminants, food components, and drugs [10]. PPARs are members of the nuclear receptor superfamily and induce the expression of numerous genes by functioning as ligand-activated transcription factors. The ligands of several PPARs include serial compounds and endogenous lipids, such as FFAs and eicosanoids [11]. Once a ligand binds to the promoter of the target gene, a heterodimer is formed with the retinoid X receptor (RXR). This heterodimer subsequently binds response elements that regulate the expression of genes encoding enzymes or proteins involved in beta oxidation, fatty acid (FA) uptake, adipogenesis, adipocyte differentiation, ketogenesis, bile acid synthesis, triglyceride turnover, and IR [12, 13].
In mammals, three PPAR isoforms have been identified: alpha (α), beta/delta (β/δ), and gamma (γ), which are differentially distributed in various tissues [11]. PPARα is ubiquitously expressed and is primary found in the liver, heart, and kidneys. In addition, PPARβ/δ is also ubiquitously expressed in muscle, adipose tissue, and the liver. PPARγ has three isoforms (γ1, γ2, and γ3) that display differences in tissue localization for each isoform; for example, γ1 has a ubiquitous tissue localization, γ2 is primarily localized in adipose tissue, and γ3 is localized in macrophages, colon, and adipose tissue [11, 14–17]. PPARs function as transcription factors that regulate the expression of genes involved in adipose metabolism, glucose metabolism, and cellular proliferation and differentiation (Table 1) [11, 15–17].
Table 1.
PPARs expression and respective ligands.
| Types | Major distribution | Targets |
|---|---|---|
| Agonist | ||
|
| ||
| PPARα | Liver, heart, kidney | Fenofibrate |
| Clofibrate | ||
| (FGF21) | ||
| (G0S2) | ||
|
| ||
| PPARβ/δ | Skeletal muscle, liver | GW0742 |
| GW501516 | ||
| MBX-8025 | ||
|
| ||
| PPARγ | Adipose tissue | TZDs |
| (rosiglitazone, pioglitazone) | ||
| Palmitate | ||
| PGC1 | ||
|
| ||
| PPARα/δ | GFT505 (elafibranor) | |
|
| ||
| PPARα/γ | Tesaglitazar | |
| Glitazars (saroglitazar) | ||
|
| ||
| Antagonist | ||
|
| ||
| PPARγ | Isorhamnetin (quercetin) | |
|
| ||
| PPARα/γ | Z-551 | |
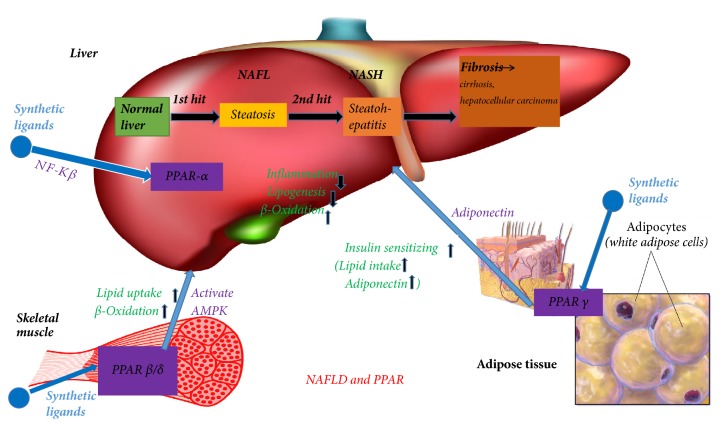
Previous studies have identified various roles for PPARδ in inflammation, lipid metabolism, and cancer [18]. Because of its intrinsic expression and diverse cellular actions, no single descriptor appropriately describes the biological function of PPARδP. PPARγ is known as the critical transcriptional regulator of the induction of adipogenesis [19]. This process occurs in fat cells that differentiate from preadipocytes into mature adipose cells. In addition to adipocytes, PPARγ is also expressed with a limited number of other cell types to cause anti-inflammatory actions and promotes lipid storage [20]. PPARγ is the molecular target of the insulin-sensitizing drugs pioglitazone and rosiglitazone, so PPARγ has been recognized as one of the key receptors in the pharmacological treatment of T2DM [21]. PPARα has an important role in the liver and acts as the main regulator of lipid metabolism, particularly during fasting [22–24]. Fasting is associated with lipid homeostasis in the liver, which is coordinated by PPARα. Previous studies using low and high throughput gene expression analysis have demonstrated that PPARα modulates the expression of numerous genes involved in virtually every profile of lipid metabolism, including FFA uptake, mitochondrial and peroxisome fatty acid oxidation (FAO), cytogenesis, and the formation and breakdown of triglycerides and lipid droplets [25]. Therefore, in this review, we aimed to summarize recent advancements that have been reported on PPAR-related genes and target drugs, thereby promoting the molecular mechanism of action of NAFLD (Figure 1).
Figure 1.
The relation between PPAR and NAFLD.
2.2. PPAR Gene Polymorphisms
Three distinct forms of the PPAR family exist in humans and rodents and all are encoded by different genes that have been identified and well characterized. The gene for PPARα is NR1C1, the gene for PPAR(β/δ) is NP1C2, and the gene for PPARγ is NR1C3 [14]. All three PPARs are heterodimers that bind to DNA using retinoid X receptors (RXR:NR2B subgroup). They preferentially bind to direct repeats of the nuclear receptor half site AGGTCA separated by 1 nucleotide (DR1).
Each subtype has unique functions. PPAR binds to direct repeats of the nuclear receptor half site AGGTCA separated by 1 nucleotide (DR1) independently. The PPARs gene is located on chromosome 3 and is linked to NAFLD. The C/G polymorphism (rs1801282) results in a Pro-to-Ala change, which represents a substitution of proline (Pro) with alanine (Ala) at codon 12. It was found that this substitution is related to a decrease in both DNA binding and transcriptional activity, and as a result, the encoded Ala allele form is reduced. The Pro12Ala variant is associated with increased insulin sensitivity, a lower body mass, and protection from T2DM. Carriers of the PPARγ Ala allele demonstrate increased resistance to NAFLD development and progression by inhibiting oxidative stress [26, 27]. Additionally, a meta-analysis study revealed a protective role against NAFLD for the Ala allele of the PPARγ Pro12 Ala (rs1801282) polymorphism [28]. Moreover, the rs1801282 polymorphism was associated with NAFLD susceptibility in East Asians but not in European populations [28]. Domenici et al. (2013) showed that the 12 Ala allele of PPARγ was less prevalent among NASH patients compared to the healthy volunteers group. No associations were found among PPARγ single nucleotide polymorphisms (SNPs) (rs1801282) and clinical, laboratory, and histological parameters in NAFLD patients. However, it was shown that the rs1801282 SNP may lead to protection against liver injuries [29]. The PPARα SNP Leu162Val (rs1800206) may be involved in the progression of NAFLD because carriers of this SNP have more advanced fibrosis [29]. However, Wang et al. suggested that the rs1801282 polymorphism of PPARγ was not associated with NAFLD risk in both Asian and Caucasian descents based on a meta-analysis study [30]. However, the rs1800206 polymorphism of PPARα showed to be associated with lipoprotein (a) (Lp(a)). Lp(a) is a low density lipoprotein- (LDL-) like particle that is associated with increased risk of atherosclerosis and CVD [31, 32]. Thus, it provides evidence that PPARα/γ may influence the risk of dyslipidemia and CVD via Lp (a) [31, 32]. The Ala12Ala genotype of PPARγ2 may decrease the number of diseased vessels and the severity of CVD. This may be due to a direct antiatherogenic effect of this polymorphism, as well as an indirect effect through its association with reduced inflammatory parameters and IR [33]. The SNP rs3856806 (also termed C161T or C1431T) in PPARγ was significantly associated with a fasted serum lipid profile [34]. Wan et al. suggested that the PPARγ SNP rs3856806 may reduce the risk of severe atherogenesis by modulation of the adipose metabolism in Chinese patients with CVD [35]. Previous studies have shown that the SNP rs3856806 increased NAFLD susceptibility through the adiponectin pathway [36, 37].
Moreover, recent studies indicated that fibroblast growth factor 21 (FGF21) functions as an endocrine hormone that mediates many of the effects of PPARα. PPARα directly induced the gene encoding FGF21 during fasting via a binding site in the promoter. Subsequently, FGF21 stimulated lipolysis in adipose tissue and cytogenesis in the liver. In vitro studies demonstrated that fatty acids act as ligands that can bind PPARα.
G0/G1 switch gene 2 (G0S2) plays a significant role in controlling lipolysis in adipocytes and serves as a target gene of PPARs. It was first found to be differentially expressed in lymphocytes during the lectin-induced switch from the G0 to G1 phase of the cell cycle [38, 39]. The highest levels of G0S2 mRNA are found in brown and white adipose tissue and are largely upregulated during adipogenesis in mouse 3T3-L1 cells [40]. These data indicate that G0S2 may participate in lipid metabolism. Recently, Yang et al. reported that G0S2 localizes to lipid droplets and prevented adipose triglyceride lipase- (ATGL-) mediated turnover occurrence in HeLa cells and adipocytes [41]. Both human and mouse G0S2 genes encode a protein of 103 amino acids and have 78% sequence homology [42]. Additional studies have revealed that G0S2 mRNA is highly expressed in brown and white adipose tissue and is upregulated during growth arrest in 3T3-L1 fibroblasts [40]. The activation of PPARγ and PPARα [40], PPARβ/δ [43], retinoic acid [42, 44], and IR can upregulate G0S2 expression in 3T3-L1 cells and human acute promyelocytic leukemia cells [41]. Furthermore, Ong et al. reported that G0S2 inhibits the triglyceride hydrolase activity of ATGL, which is a major regulator of the lipid metabolism in mammals [45]. ATGL is also a major lipase in the liver, which indicated that G0S2 may have a significant role in regulating lipolysis in adipocytes [41].
3. PPARα
PPARα is important in the regulation of lipid transport and metabolism chiefly through the activation of mitochondrial and peroxisomal fatty acid β-oxidation pathways. PPARα regulates the transcription of constitutive genes encoding fatty acid-metabolizing enzymes and mitochondrial FA oxidation (FAO) activity, primarily in the liver [46]. PPARα directly inhibits inflammatory genes induced by NF-κB [47] and reduces IL-1-induced expression of C-reactive protein in human primary hepatocytes [48]. Moreover, fenofibrate treatment decreased the IL-6-induced expression of acute phase response genes in the livers of wild type mice but not PPARα-deficient mice. Fenofibrate treatment also reduced plasma concentrations of the acute phase proteins fibrinogen, C-reactive protein, serum amyloid A, plasminogen, and alpha 2-macroglobulin in human subjects [49–51]. PPARα activators, such as the widely prescribed fibrate drugs, ameliorate hepatic steatosis by enhancing mitochondrial FAO in mice [52]. Furthermore, PPARα has an anti-inflammatory role after being fed with a high-fat diet (HFD) [53]. PPARα is a transcriptional regulator of the lipid pathway and a direct target of a microRNA (miRNA or miR) in the liver (miR-34a). The miR-34a-PPARα has recently been identified and provides a novel clue to the pathogenesis of steatosis in NAFLD [54]. In fact, miR-34a may become a target for the treatment of NAFLD.
Currently, it is suggested that microRNAs contribute to the pathogenesis of NAFLD. MicroRNAs act as potent posttranscriptional regulators of gene expression [55, 56]. MiR-21 is increased in the liver of NASH patients [49] and in animal models of NASH [54, 57–59]. In hepatocytes, miR-21 is induced by unsaturated fatty acids in an mTOR/NF-κB-dependent manner [60]. In addition, recent studies have demonstrated that hepatic miR-21 plays an active role in NASH pathogenesis by inhibiting PPARα, which is a key target of miR-21 [54]. The miR-21/PPARα axis regulates PPARα in muscle tissue of NAFLD patients, which may be important in disease development and progression.
Similarly, PPARα is activated by a wide range of different fatty acids and eicosanoids [61–65]. Moreover, PPARα served as a receptor for various synthetic compounds, collectively referred to as peroxisome proliferators [12]. This includes phthalates, insecticides, herbicides, surfactants, organic solvents, and hypolipidemic fibrate drugs. For decades, fibrates have been used by divers primarily because of their ability to decrease circulating triglycerides [66]. The first generation of PPARα agonists Clofibrate and Fenofibrate have been thought to primarily activate PPARα in the liver, resulting in improvements in the plasma lipid profile. However, it is concerning that the World Health Organization conducted a clinical trial in which increased coronary and overall mortality rates in the Clofibrate treatment groups were detected [67]. Bezafibrate is a low potency compound that activates all three PPAR isoforms. It has been shown to decrease the risk of cardiovascular events and prevent the onset of diabetes in patients with metabolic syndrome [68]. It has also been reported to be safe and well tolerated [69]. Thus, pharmacological targeting of PPARα has been considered as a promising treatment of NAFLD.
A dual PPARα/δ agonist called GFT505 has been indicated to promote markers of liver dysfunction, reduce hepatic lipid accumulation, and decrease hepatic inflammatory gene expression in liver in numerous animal models of NAFLD [60]. Moreover, GFT505 treatment reduced liver dysfunction markers and enhanced hepatic and peripheral insulin sensitivity in humans [60, 61].
4. PPARδ
Pharmacological targets of PPARα and PPARγ are relatively well-known in the therapies of dyslipidemia and diabetes [70]. However, PPARδ also has a significant role in the regulation of metabolism since its activation augments fatty acid oxidation, alleviates glucose homeostasis, and reduces macrophage inflammatory responses [15, 70]. According to a current study, the PPARδ agonist GW0742 was suggested to reduce the renal dysfunction and inflammation caused by chronic high-fructose corn syrup (HFCS-55) exposure by preventing the activation of the NLRP3 inflammasome in the nephridium [71]. In a recent study, it was suggested that GW501516 decreased activation of the inflammasome and overproduction of proinflammatory cytokines in HepG2 cells and mouse livers [72]. Furthermore, GW501516 alleviated hepatic steatosis in vivo.
Due to its ability to maintain metabolic homeostasis, AMPK is an important metabolic regulator in cellular and organismal survival and an essential mediator for fatty acid metabolism [72–74]. Numerous studies have demonstrated that PPARδ prevented the downregulation of AMPK [72, 73]. PPARδ agonist GW501516 inhibited activation of the inflammasome and reduced IL-1β levels. Additionally, GW501516 potentially modulated AMPK phosphorylation and reduced the production of reactive oxygen species. This anti-inflammatory effect may be related to the amelioration of hepatic steatosis in mice. The target of the inflammasome by the PPARδ agonist might be related to the therapeutic implications for the treatment of NAFLD.
Lastly, a novel PPARδ agonist, MBX-8025, was evaluated in a small, randomized, double-blind, placebo-controlled study. This study included overweight subjects with dyslipidemia and found that treatment with MBX-8025 resulted in favorable lipid profiles and decreased gamma-glutamyl transpeptidase (GGT) [75]. However, other markers of NAFLD or liver injury were not measured in this study, which has limited the interpretation of the treatment effectiveness of NAFLD.
5. PPARγ
The PPARγ coactivator 1 (PGC1) is a group of transcriptional coactivators that include PGC1α, PGC1β, and the PGC related coactivator (PRC) [76]. PGC1α is related to transcriptional factors such as PPARα, PPARγ, estrogen-related receptor, liver X receptor, and hepatocyte nuclear factor-4α. Furthermore, PGC1α regulates the mitochondrial metabolism [77] and modulates energy, glucose, and adipose metabolism. These characteristics are recognized as key therapeutic targets for diabetes and obesity. A recent study in humans also suggested that the mRNA expression of PPARγ was markedly higher in obese patients (n = 22, NAFLD) when compared to controls. Moreover, PPARγ expression in the liver was suggested to have a positive correlation with sterol regulatory element binding protein 1c mRNA levels, serum insulin levels, and homeostasis model assessment-insulin resistance and has a negative correlation with total adiponectin levels [78]. Thus, it was determined that the peroxisome proliferator-like effects of rosiglitazone in fat mice might be due to the activation of PPARγ. In a recent study, it was suggested that palmitate (not oleate) upregulates PPARγ via PGC1s in Huh7 cells. Moreover, both PGC1α and PPARγ are similarly upregulated and palmitate constituent was increased in the liver in the NAFLD mouse model, indicating a positive correlation with the triglyceride content. This suggested an explicit effect on the lipid metabolism that causes intrahepatic triglyceride accumulation.
It is well established that PPARγ is the primary regulator of adipose tissue development and function and is more abundant in adipose tissue than in any other cell type. Thiazolidinediones (TZDs) play a key role in stimulating progenitor stem cells to differentiate in adipocytes and influence mature adipocytes [79]. Current reports have also shown that TZDs enhance FGF21 expression in adipose tissue. TZDs also increase PPARγ transcriptional activity in an autocrine or paracrine manner and target PPARγ by posttranslational modification. TZDs represent a class of clinically used insulin-sensitizing drugs, which currently includes rosiglitazone and pioglitazone that exert many other pleiotropic effects [79]. Pioglitazone has shown to improve endothelial dysfunction, reduces blood pressure, corrects diabetic dyslipidemia, and reduced circulating levels of inflammatory cytokines and prothrombotic factors [79]. Consistent with these antiatherogenic effects, pioglitazone reduced major adverse cardiac endpoints such as mortality, myocardial infarction, and stroke [80].
Most studies on PPARγ ligands have focused on agonists. Here, we identified that isorhamnetin, a natural and novel identified compound in fruits, vegetables, and the metabolite of quercetin, ameliorated MS induced by diet or leptin deficiency [81]. Isorhamnetin treatment inhibited 3T3-L1 adipocyte differentiation induced by PPARγ agonists such as rosiglitazone [81, 82]. It can reduce the expression of genes downstream of PPARs and antagonize PPARγ transactivity. Moreover, it also reduced the onset of obesity and ameliorated hepatic steatosis induced by both high-fat diet treatment and leptin deficiency [83–85]. In addition, it was also indicated that gypenoside treatment significantly reduced levels of PPARγ, thereby having potential hepatoprotective effects [86]. These results suggested that dietary supplements of isorhamnetin may be beneficial for the prevention of obesity and steatosis. In addition, PPARi antagonists may be a promising therapy for hepatic steatosis.
6. Conclusions
In this review, several molecular pathways have been outlined, contributing to therapies for NAFLD. However, the precise details of these pathways are still being elucidated, but they provide targets for future therapeutic strategies in NAFLD treatment. In addition, the efficacy and safety of NAFLD management should be considered. Additional clinical evidence is required before their clinical application, and further large-scale clinical trials and practice are warranted to verify drug treatment effects.
Acknowledgments
The authors would like to sincerely thank Dr. Jie Lu, Dr. Xiaorong Xu, and the staff of the Central Laboratory of Shanghai Tenth People's Hospital for their assistance. This study was supported by grants from National Natural Science Foundation of China (81300340; 81770518) and Chinese Foundation for Hepatitis Prevention and Control (CFHPC2013101).
Contributor Information
Xiaorong Xu, Email: xuxr@tongji.edu.cn.
Jie Lu, Email: kennisren@hotmail.com.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Alberti K. G., Eckel R. H., Grundy S. M., Zimmet P. Z., Cleeman J. I., Donato K. A., et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; american heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16) doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 2.Armstrong M. J., Adams L. A., Canbay A., Syn W.-K. Extrahepatic complications of nonalcoholic fatty liver disease. Hepatology. 2014;59(3):1174–1197. doi: 10.1002/hep.26717. [DOI] [PubMed] [Google Scholar]
- 3.Green R. M. NASH - Hepatic metabolism and not simply the metabolic syndrome. Hepatology. 2003;38(1):14–17. doi: 10.1053/jhep.2003.50325. [DOI] [PubMed] [Google Scholar]
- 4.Angulo P. Nonalcoholic fatty liver disease. The New England Journal of Medicine. 2002;346(16):1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 5.Tamura S., Shimomura I. Contribution of adipose tissue and de novo lipogenesis to nonalcoholic fatty liver disease. The Journal of Clinical Investigation. 2005;115(5):1139–1142. doi: 10.1172/JCI200524930. doi: 10.1172/JCI200524930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vernon G., Baranova A., Younossi Z. M. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Alimentary Pharmacology & Therapeutics. 2011;34(3):274–285. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 7.Musso G., Gambino R., Cassader M., Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Annals of Medicine. 2011;43(8):617–649. doi: 10.3109/07853890.2010.518623. [DOI] [PubMed] [Google Scholar]
- 8.Day C. P., James O. F. W. Steatohepatitis: a tale of two “Hits”? Gastroenterology. 1998;114(4):842–845. doi: 10.1016/S0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 9.Angulo P. Nonalcoholic fatty liver disease. The New England Journal of Medicine. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 10.Kersten S., Desvergne B., Wahli W. Roles of PPARS in health and disease. Nature. 2000;405(6785):421–424. doi: 10.1038/35013000. [DOI] [PubMed] [Google Scholar]
- 11.Cave M. C., Clair H. B., Hardesty J. E., et al. Nuclear receptors and nonalcoholic fatty liver disease. Biochimica et Biophysica Acta (BBA)-Gene Regulatory Mechanisms. 2016;1859(9):1083–1099. doi: 10.1016/j.bbagrm.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Issemann I., Green S. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature. 1990;347(6294):645–650. doi: 10.1038/347645a0. [DOI] [PubMed] [Google Scholar]
- 13.Desvergne B., Wahli W. Peroxisome proliferator-activated receptors: nuclear control of metabolism. Endocrine Reviews. 1999;20(5):649–688. doi: 10.1210/edrv.20.5.0380. [DOI] [PubMed] [Google Scholar]
- 14.Evans R. M., Mangelsdorf D. J. Nuclear receptors, RXR, and the big bang. Cell. 2014;157(1):255–266. doi: 10.1016/j.cell.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tailleux A., Wouters K., Staels B. Roles of PPARs in NAFLD: potential therapeutic targets. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2012;1821(5):809–818. doi: 10.1016/j.bbalip.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 16.Pawlak M., Lefebvre P., Staels B. Molecular mechanism of PPARα action and its impact on lipid metabolism, inflammation and fibrosis in non-alcoholic fatty liver disease. Journal of Hepatology. 2015;62(3):720–733. doi: 10.1016/j.jhep.2014.10.039. [DOI] [PubMed] [Google Scholar]
- 17.Motojima K., Passilly P., Peters J. M., Gonzalez F. J., Latruffe N. Expression of putative fatty acid transporter genes are regulated by peroxisome proliferator-activated receptor α and γ activators in a tissue- and inducer-specific manner. The Journal of Biological Chemistry. 1998;273(27):16710–16714. doi: 10.1074/jbc.273.27.16710. [DOI] [PubMed] [Google Scholar]
- 18.Wagner K.-D., Wagner N. Peroxisome proliferator-activated receptor beta/delta (PPARβ/δ) acts as regulator of metabolism linked to multiple cellular functions. Pharmacology & Therapeutics. 2010;125(3):423–435. doi: 10.1016/j.pharmthera.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Tontonoz P., Hu E., Spiegelman B. M. Stimulation of adipogenesis in fibroblasts by PPARγ2, a lipid-activated transcription factor. Cell. 1994;79(7):1147–1156. doi: 10.1016/0092-8674(94)90006-X. [DOI] [PubMed] [Google Scholar]
- 20.Tontonoz P., Spiegelman B. M. Fat and beyond: the diverse biology of PPARγ. Annual Review of Biochemistry. 2008;77:289–312. doi: 10.1146/annurev.biochem.77.061307.091829. [DOI] [PubMed] [Google Scholar]
- 21.Lehmann J. M., Moore L. B., Smith-Oliver T. A., Wilkison W. O., Willson T. M., Kliewer S. A. An antidiabetic thiazolidinedione is a high affinity ligand for peroxisome proliferator-activated receptor γ (PPARγ) The Journal of Biological Chemistry. 1995;270(22):12953–12956. doi: 10.1074/jbc.270.22.12953. [DOI] [PubMed] [Google Scholar]
- 22.Hashimoto T., Cook W. S., Qi C., Yeldandi A. V., Reddy J. K., Rao M. S. Defect in peroxisome proliferator-activated receptor α-inducible fatty acid oxidation determines the severity of hepatic steatosis in response to fasting. The Journal of Biological Chemistry. 2000;275(37):28918–28928. doi: 10.1074/jbc.M910350199. [DOI] [PubMed] [Google Scholar]
- 23.Kersten S., Seydoux J., Peters J. M., Gonzalez F. J., Desvergne B., Wahli W. Peroxisome proliferator-activated receptor α mediates the adaptive response to fasting. The Journal of Clinical Investigation. 1999;103(11):1489–1498. doi: 10.1172/jci6223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leone T. C., Weinheimer C. J., Kelly D. P. A critical role for the peroxisome proliferator-activated receptor alpha (PPARalpha) in the cellular fasting response: the PPARalpha-null mouse as a model of fatty acid oxidation disorders. Proceedings of the National Acadamy of Sciences of the United States of America. 1999;96(13):7473–7478. doi: 10.1073/pnas.96.13.7473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kersten S. Integrated physiology and systems biology of PPARalpha. Molecular Metabolism. 2014;3(4):354–371. doi: 10.1016/j.molmet.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dimitrova-Shumkovska J., Veenman L., Ristoski T., Leschiner S., Gavish M. Chronic high fat, high cholesterol supplementation decreases 18 kDa Translocator Protein binding capacity in association with increased oxidative stress in rat liver and aorta. Food and Chemical Toxicology. 2010;48(3):910–921. doi: 10.1016/j.fct.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 27.Thamer C., Haap M., Volk A., et al. Evidence for greater oxidative substrate flexibility in male carriers of the Pro 12 Ala polymorphism in PPARγ2. Hormone and Metabolic Research. 2002;34(3):132–136. doi: 10.1055/s-2002-23196. [DOI] [PubMed] [Google Scholar]
- 28.Lee Y. H., Bae S.-C., Song G. G. Meta-analysis of associations between the peroxisome proliferator-activated receptor-γ Pro12Ala polymorphism and susceptibility to nonalcoholic fatty liver disease, rheumatoid arthritis, and psoriatic arthritis. Genetic Testing and Molecular Biomarkers. 2014;18(5):341–348. doi: 10.1089/gtmb.2013.0503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Domenici F. A., Brochado M. J. F., Martinelli A. D. L. C., Zucoloto S., da Cunha S. F. D. C., Vannucchi H. Peroxisome proliferator-activated receptors alpha and gamma2 polymorphisms in nonalcoholic fatty liver disease: A study in Brazilian patients. Gene. 2013;529(2):326–331. doi: 10.1016/j.gene.2013.06.091. [DOI] [PubMed] [Google Scholar]
- 30.Wang J., Guo X., Wu P., et al. Association between the Pro12Ala polymorphism of PPAR-γ gene and the non-alcoholic fatty liver disease: A meta-analysis. Gene. 2013;528(2):328–334. doi: 10.1016/j.gene.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 31.Danesh J., Collins R., Peto R. Lipoprotein(a) and coronary heart disease: meta-analysis of prospective studies. Circulation. 2000;102(10):1082–1085. doi: 10.1161/01.cir.102.10.1082. [DOI] [PubMed] [Google Scholar]
- 32.Xie H., Hai B., Wu M., et al. Analysis on the association between PPARα/γ polymorphisms and lipoprotein(a) in a Chinese Han population. Molecular Genetics and Genomics. 2014;289(5):981–987. doi: 10.1007/s00438-014-0866-9. [DOI] [PubMed] [Google Scholar]
- 33.Youssef S. M., Mohamed N., Afef S., et al. A Pro 12 Ala substitution in the PPARγ2 polymorphism may decrease the number of diseased vessels and the severity of angiographic coronary artery. Coronary Artery Disease. 2013;24(5):347–351. doi: 10.1097/MCA.0b013e328361a95e. [DOI] [PubMed] [Google Scholar]
- 34.Oladi M., Nohtani M., Avan A., et al. Impact of the C1431T polymorphism of the peroxisome proliferator activated receptor-gamma (PPAR-γ) gene on fasted serum lipid levels in patients with coronary artery disease. Annals of Nutrition and Metabolism. 2015;66(2-3):149–154. doi: 10.1159/000381358. [DOI] [PubMed] [Google Scholar]
- 35.Wan J., Xiong S., Chao S., et al. PPARγ gene C161T substitution alters lipid profile in Chinese patients with coronary artery disease and type 2 diabetes mellitus. Cardiovascular Diabetology. 2010;9, article no. 13 doi: 10.1186/1475-2840-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hui Y., Yu-yuan L., Yu-qiang N., et al. Effect of peroxisome proliferator-activated receptors-γ and co-activator-1α genetic polymorphisms on plasma adiponectin levels and susceptibility of non-alcoholic fatty liver disease in Chinese people. Liver International. 2008;28(3):385–392. doi: 10.1111/j.1478-3231.2007.01623.x. [DOI] [PubMed] [Google Scholar]
- 37.Zhou Y., Li Y., Nie Y., et al. Influence of polygenetic polymorphisms on the susceptibility to non-alcoholic fatty liver disease of Chinese people. Journal of Gastroenterology and Hepatology. 2010;25(4):772–777. doi: 10.1111/j.1440-1746.2009.06144.x. [DOI] [PubMed] [Google Scholar]
- 38.Nakamura N., Shimaoka Y., Tougan T., et al. Isolation and expression profiling of genes upregulated in bone marrow-derived mononuclear cells of rheumatoid arthritis patients. DNA Research. 2006;13(4):169–183. doi: 10.1093/dnares/dsl006. [DOI] [PubMed] [Google Scholar]
- 39.Russell L., Forsdyke D. R. A human putative lymphocyte G0/G1 switch gene containing a CpG-rich island encodes a small basic protein with the potential to be phosphorylated. DNA and Cell Biology. 1991;10(8):581–591. doi: 10.1089/dna.1991.10.581. [DOI] [PubMed] [Google Scholar]
- 40.Zandbergen F., Mandard S., Escher P., et al. The G0/G1 switch gene 2 is a novel PPAR target gene. Biochemical Journal. 2005;392(2):313–324. doi: 10.1042/BJ20050636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang X., Lu X., Lombès M., et al. The G0/G1 Switch Gene 2 Regulates Adipose Lipolysis through Association with Adipose Triglyceride Lipase. Cell Metabolism. 2010;11(3):194–205. doi: 10.1016/j.cmet.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kitareewan S., Blumen S., Sekula D., et al. G0S2 is an all-trans-retinoic acid target gene. International Journal of Oncology. 2008;33(2):397–404. doi: 10.3892/ijo_00000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teunissen B. E. J., Smeets P. J. H., Willemsen P. H. M., de Windt L. J., van der Vusse G. J., van Bilsen M. Activation of PPARdelta inhibits cardiac fibroblast proliferation and the transdifferentiation into myofibroblasts. Cardiovascular Research. 2007;75(3):519–529. doi: 10.1016/j.cardiores.2007.04.026. [DOI] [PubMed] [Google Scholar]
- 44.Cheng Y.-H., Utsunomiya H., Pavone M. E., Yin P., Bulun S. E. Retinoic acid inhibits endometrial cancer cell growth via multiple genomic mechanisms. Molecular Endocrinology. 2011;46(2):139–153. doi: 10.1530/JME-10-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ong K. T., Mashek M. T., Bu S. Y., Greenberg A. S., Mashek D. G. Adipose triglyceride lipase is a major hepatic lipase that regulates triacylglycerol turnover and fatty acid signaling and partitioning. Hepatology. 2011;53(1):116–126. doi: 10.1002/hep.24006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aoyama T., Peters J. M., Iritani N., et al. Altered constitutive expression of fatty acid-metabolizing enzymes in mice lacking the peroxisome proliferator-activated receptor α (PPARα) The Journal of Biological Chemistry. 1998;273(10):5678–5684. doi: 10.1074/jbc.273.10.5678. [DOI] [PubMed] [Google Scholar]
- 47.Staels B., Koenig W., Habib A., et al. Activation of human aortic smooth-muscle cells is inhibited by PPARα but not by PPARγ activators. Nature. 1998;393(6687):790–793. doi: 10.1038/31701. [DOI] [PubMed] [Google Scholar]
- 48.Kleemann R., Gervois P. P., Verschuren L., Staels B., Princen H. M. G., Kooistra T. Fibrates down-regulate IL-1-stimulated C-reactive protein gene expression in hepatocytes by reducing nuclear p50-NFκB-C/EBP-β complex formation. Blood. 2003;101(2):545–551. doi: 10.1182/blood-2002-06-1762. [DOI] [PubMed] [Google Scholar]
- 49.Gervois P., Kleemann R., Pilon A., et al. Global suppression of IL-6-induced acute phase response gene expression after chronic in vivo treatment with the peroxisome proliferator-activated receptor-alpha activator fenofibrate. The Journal of Biological Chemistry. 2004;279(16):16154–16160. doi: 10.1074/jbc.M400346200. [DOI] [PubMed] [Google Scholar]
- 50.Lefebvre P., Chinetti G., Fruchart J. C., Staels B. Sorting out the roles of PPARα in energy metabolism and vascular homeostasis. The Journal of Clinical Investigation. 2006;116(3):571–580. doi: 10.1172/jci27989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Staels B., Maes M., Zambon A. Fibrates and future PPARα agonists in the treatment of cardiovascular disease. Nature Clinical Practice Cardiovascular Medicine. 2008;5(9):542–553. doi: 10.1038/ncpcardio1278. [DOI] [PubMed] [Google Scholar]
- 52.Nakajima T., Tanaka N., Kanbe H., et al. Bezafibrate at clinically relevant doses decreases serum/liver triglycerides via down-regulation of sterol regulatory element-binding protein-1c in mice: A novel peroxisome proliferator-activated receptor α-independent mechanism. Molecular Pharmacology. 2009;75(4):782–792. doi: 10.1124/mol.108.052928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stienstra R., Mandard S., Patsouris D., Maass C., Kersten S., Müller M. Peroxisome proliferator-activated receptor α protects against obesity-induced hepatic inflammation. Endocrinology. 2007;148(6):2753–2763. doi: 10.1210/en.2007-0014. [DOI] [PubMed] [Google Scholar]
- 54.Loyer X., Paradis V., Hénique C., et al. Liver microRNA-21 is overexpressed in non-alcoholic steatohepatitis and contributes to the disease in experimental models by inhibiting PPARa expression. Gut. 2015;65(11):1882–1894. doi: 10.1136/gutjnl-2014-308883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bartel D. P. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pereira D. M., Rodrigues P. M., Borralho P. M., Rodrigues C. M. P. Delivering the promise of miRNA cancer therapeutics. Drug Discovery Therapy. 2013;18(5-6):282–289. doi: 10.1016/j.drudis.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 57.Wang B., Majumder S., Nuovo G., et al. Role of microRNA-155 at early stages of hepatocarcinogenesis induced by choline-deficient and amino acid-defined diet in C57BL/6 mice. Hepatology. 2009;50(4):1152–1161. doi: 10.1002/hep.23100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu H., Ng R., Chen X., Steer C. J., Song G. MicroRNA-21 is a potential link between non-alcoholic fatty liver disease and hepatocellular carcinoma via modulation of the HBP1-p53-Srebp1c pathway. Gut. 2015;65(11):1850–1860. doi: 10.1136/gutjnl-2014-308430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Calo N., Ramadori P., Sobolewski C., et al. Stress-activated miR-21/miR-21∗ in hepatocytes promotes lipid and glucose metabolic disorders associated with high-fat diet consumption. Gut. 2016;65(11):1871–1881. doi: 10.1136/gutjnl-2015-310822. [DOI] [PubMed] [Google Scholar]
- 60.Vinciguerra M., Sgroi A., Veyrat-Durebex C., Rubbia-Brandt L., Buhler L. H., Foti M. Unsaturated fatty acids inhibit the expression of tumor suppressor phosphatase and tensin homolog(PTEN) via microRNA-21 up-regulation in hepatocytes. Hepatology. 2009;49(4):1176–1184. doi: 10.1002/hep.22737. [DOI] [PubMed] [Google Scholar]
- 61.Dreyer C., Keller H., Mahfoudi A., Laudet V., Krey G., Wahli W. Positive regulation of the peroxisomal β-oxidation pathway by fatty acids through activation of peroxisome proliferator-activated receptors (PPAR) Biology of the Cell. 1993;77(C):67–76. doi: 10.1016/S0248-4900(05)80176-5. [DOI] [PubMed] [Google Scholar]
- 62.Forman B. M., Chen J., Evans R. M. Hypolipidemic drugs, polyunsaturated fatty acids, and eicosanoids are ligands for peroxisome proliferator-activated receptors alpha and delta. Proceedings of the National Acadamy of Sciences of the United States of America. 1997;94(9):4312–4317. doi: 10.1073/pnas.94.9.4312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gottlicher M., Widmark E., Li Q., Gustafsson J. Fatty acids activate a chimera of the clofibric acid-activated receptor and the glucocorticoid receptor. Proceedings of the National Acadamy of Sciences of the United States of America. 1992;89(10):4653–4657. doi: 10.1073/pnas.89.10.4653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kliewer S. A., Sundseth S. S., Jones S. A., et al. Fatty acids and eicosanoids regulate gene expression through direct interactions with peroxisome proliferator-activated receptors α and γ. Proceedings of the National Acadamy of Sciences of the United States of America. 1997;94(9):4318–4323. doi: 10.1073/pnas.94.9.4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Krey G., Braissant O., L'Horset F., et al. Fatty acids, eicosanoids, and hypolipidemic agents identified as ligands of peroxisome proliferator-activated receptors by coactivator-dependent receptor ligand assay. Molecular Endocrinology. 1997;11(6):779–791. doi: 10.1210/me.11.6.779. [DOI] [PubMed] [Google Scholar]
- 66.Staels B., Fruchart J.-C. Therapeutic roles of peroxisome proliferator-activated receptor agonists. Diabetes. 2005;54(8):2460–2470. doi: 10.2337/diabetes.54.8.2460. [DOI] [PubMed] [Google Scholar]
- 67.Keech A., Simes R. J., Barter P. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. The Lancet. 2005;366(9500):1849–1861. doi: 10.1016/s0140-6736(05)67667-2. [DOI] [PubMed] [Google Scholar]
- 68.Tenenbaum A., Motro M., Fisman E. Z., Tanne D., Boyko V., Behar S. Bezafibrate for the secondary prevention of myocardial infarction in patients with metabolic syndrome. JAMA Internal Medicine. 2005;165(10):1154–1160. doi: 10.1001/archinte.165.10.1154. [DOI] [PubMed] [Google Scholar]
- 69.Ahmadian M., Suh J. M., Hah N., et al. PPARγ signaling and metabolism: the good, the bad and the future. Nature Medicine. 2013;19(5):557–566. doi: 10.1038/nm.3159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Poulsen L. L. C., Siersbaek M., Mandrup S. PPARs: fatty acid sensors controlling metabolism. Seminars in Cell & Developmental Biology. 2012;23(6):631–639. doi: 10.1016/j.semcdb.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 71.Collino M., Benetti E., Rogazzo M., et al. Reversal of the deleterious effects of chronic dietary HFCS-55 intake by PPAR- δ agonism correlates with impaired NLRP3 inflammasome activation. Biochemical Pharmacology. 2013;85(2):257–264. doi: 10.1016/j.bcp.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 72.Barroso E., Rodríguez-Calvo R., Serrano-Marco L., et al. The PPARβ/δ activator GW501516 prevents the down-regulation of AMPK caused by a high-fat diet in liver and amplifies the PGC-1α-lipin 1-PPARα pathway leading to increased fatty acid oxidation. Endocrinology. 2011;152(5):1848–1859. doi: 10.1210/en.2010-1468. [DOI] [PubMed] [Google Scholar]
- 73.Sid B., Verrax J., Calderon P. B. Role of AMPK activation in oxidative cell damage: Implications for alcohol-induced liver disease. Biochemical Pharmacology. 2013;86(2):200–209. doi: 10.1016/j.bcp.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 74.Wen H., Gris D., Lei Y., et al. Fatty acid-induced NLRP3-ASC inflammasome activation interferes with insulin signaling. Nature Immunology. 2011;12(5):408–415. doi: 10.1038/ni.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bays H. E., Schwartz S., Littlejohn T., III, et al. MBX-8025, a novel peroxisome proliferator receptor-δ agonist: lipid and other metabolic effects in dyslipidemic overweight patients treated with and without atorvastatin. The Journal of Clinical Endocrinology & Metabolism. 2011;96(9):2889–2897. doi: 10.1210/jc.2011-1061. [DOI] [PubMed] [Google Scholar]
- 76.Handschin C., Spiegelman B. M. Peroxisome proliferator-activated receptor γ coactivator 1 coactivators, energy homeostasis, and metabolism. Endocrine Reviews. 2006;27(7):728–735. doi: 10.1210/er.2006-0037. [DOI] [PubMed] [Google Scholar]
- 77.Austin S., St-Pierre J. PGC1 α and mitochondrial metabolism-emerging concepts and lerevance in aging and neurodegenerative disorders. Journal of Cell Science. 2012;125(21):4963–4971. doi: 10.1242/jcs.106625. [DOI] [PubMed] [Google Scholar]
- 78.Pettinelli P., Videla L. A. Up-regulation of PPAR-γ mRNA expression in the liver of obese patients: an additional reinforcing lipogenic mechanism to SREBP-1c induction. The Journal of Clinical Endocrinology & Metabolism. 2011;96(5):1424–1430. doi: 10.1210/jc.2010-2129. [DOI] [PubMed] [Google Scholar]
- 79.Defronzo R. A., Mehta R. J., Schnure J. J. Pleiotropic effects of thiazolidinediones: implications for the treatment of patients with type 2 diabetes mellitus. Hospital Practice. 2013;41(2):132–147. doi: 10.3810/hp.2013.04.1062. [DOI] [PubMed] [Google Scholar]
- 80.Stojanovic M., Prostran M., Radenkovic M. Thiazolidinediones improve flow-mediated dilation: A meta-analysis of randomized clinical trials. European Journal of Clinical Pharmacology. 2016;72(4):385–398. doi: 10.1007/s00228-015-1999-4. [DOI] [PubMed] [Google Scholar]
- 81.Goto T., Kim Y. I., Takahashi N., Kawada T. Natural compounds regulate energy metabolism by the modulating the activity of lipid-sensing nuclear receptors. Molecular Nutrition & Food Research. 2013;57:20–33. doi: 10.1002/mnfr.201200522. [DOI] [PubMed] [Google Scholar]
- 82.Gong Z., Huang C., Sheng X., et al. The role of tanshinone IIA in the treatment of obesity through peroxisome proliferator-activated receptor γ antagonism. Endocrinology. 2009;150(1):104–113. doi: 10.1210/en.2008-0322. [DOI] [PubMed] [Google Scholar]
- 83.Lee J., Jung E., Hwang W., Kim Y. S., Park D. Isorhamnetin-induced anti-adipogenesis is mediated by stabilization of beta-catenin protein. Life Science. 2010;86:416–423. doi: 10.1016/j.lfs.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 84.Lee J., Jung E., Lee J., et al. Isorhamnetin represses adipogenesis in 3T3-L1 cells. Obesity. 2009;17(2):226–232. doi: 10.1038/oby.2008.472. [DOI] [PubMed] [Google Scholar]
- 85.Zhang N., Pei F., Wei H., et al. Isorhamnetin protects rat ventricular myocytes from ischemia and reperfusion injury. Experimental and Toxicologic Pathology. 2011;63(1-2):33–38. doi: 10.1016/j.etp.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 86.Lin J.-J., Hsu H.-Y., Yang J.-S., et al. Molecular evidence of anti-leukemia activity of gypenosides on human myeloid leukemia HL-60 cells in vitro and in vivo using a HL-60 cells murine xenograft model. Phytomedicine. 2011;18(12):1075–1085. doi: 10.1016/j.phymed.2011.03.009. [DOI] [PubMed] [Google Scholar]