Abstract
Objective: The aim of this study was to compare the 30-day emergency department (ED) return rate between patients given a Take Home Medication pack (THM) versus a standard paper prescription (SPP) prior to discharge. Methods: This was an observational, prospective cohort study in an urban, university-affiliated, level I trauma center. Patients were identified through daily pharmacy reports. Consecutive adult patients discharged from the ED with either a THM or equivalent SPP were included. For each patient, baseline characteristics including age, gender, primary care provider (PCP), primary language, ethnicity, marital status, and insurance status were recorded from the electronic medical record (EMR). Review of the EMR was used to determine whether patients returned to the ED within 30 days and whether the return visit was for all-causes or for the same complaint targeted by the THM or SPP from the index visit. Similarly, visits to other providers in the health system within 30 days were recorded. Results: A total of 711 patients were included in the study, with 268 receiving a THM and 443 receiving a SPP. In comparison with the SPP group, the THM group was more likely to have an all-cause return (Relative Risk [RR] = 1.7, P < .01). Variables associated with increased odds of returning to the ED within 30 days included study group (adjusted Odds Ratio [aOR]: 1.7), male gender (aOR: 1.6), African American ethnicity (aOR: 3.0), public insurance (aOR: 3.3), and institutional financial assistance (aOR: 5.0). The difference between study groups for index visit complaint-specific returns was not significant. Conclusions: Patients receiving a THM demonstrated a higher all-cause return rate than patients receiving a SPP. A randomized study is needed evaluating the effect of THM on return ED visits.
Keywords: readmissions, patient discharge, prescriptions, health care utilization
Introduction
Background and Importance
Medication nonadherence following emergency department (ED) discharge is associated with recurrent ED visits, leading to increased costs to the health care system.1-4 Such repeat visits have recently gained greater attention given the potential associated financial ramifications of the Centers for Medicare and Medicaid Services (CMS) Hospital Readmissions Reduction Program. Several studies have found low rates of medication adherence following discharge from the ED, and it has been reported that as many as 4 in 10 ED patients do not take discharge medications as prescribed.5-10 Nonadherence to medications has been reported to be as high as 22.5% and even higher for new prescriptions at 28.3%.11,12
One potential strategy to address medication nonadherence is to provide patients with Take Home Medication packs (THM) prior to ED discharge. A THM is a packaged full course of a prescribed medication that can be given to a patient in place of a standard paper prescription (SPP), thereby eliminating the need for the patient to go to a pharmacy. However, there are few studies examining such interventions.5,13-15
Goals of This Investigation
The aim of the study was to compare rate of returns to the ED between patients given a THM prior to discharge and patients receiving an equivalent SPP. We hypothesized that patients receiving THMs would be less likely to return to the ED within 30 days of the index visit.
Methods
Study Design and Setting
This was an observational, prospective cohort study. The study site is an academic ED in an urban, university hospital with a census of approximately 90 000 adult patients per year. All adults evaluated in the ED were eligible for study inclusion. THMs have been available in this institution for approximately 10 years and are accepted as an established component of ED practice, but the effects of this resource have not previously been formally evaluated. THM are prepackaged by pharmacy and are available in automated dispensing cabinets in the ED. Available THMs range from an albuterol inhaler to a full course of antibiotics (Table 1). Institutional guidelines state that THMs are intended for patients enrolled in the county-funded institutional financial assistance program and are to be given to patients discharged outside of outpatient pharmacy hours. However, in practice the decision to prescribe a THM is at the discretion of individual providers. In this study, we compared patients receiving THMs with the patients receiving SPPs.
Table 1.
Available Take Home Medications (THM).
| Albuterol inhaler 90 µg THM—Inhale 1 to 2 puffs by mouth every 4 hours as needed for shortness of breath |
| Amoxicillin 500 mg #30 THM—Take 1 capsule by mouth every 8 hours until all taken |
| Azithromycin 250 mg #6 THM—Take 2 tables by mouth today, then take 1 tablet every day for 4 days |
| Bactrim DS #20 THM—Take 1 tablet by mouth every 12 hours until all taken |
| Beclomethasone 40 µg THM—Inhale __ puffs by mouth twice a day |
| Cephalexin 500 mg #40 THM—Take 1 capsule by mouth every 6 hours for 10 days |
| Ciprofloxacin 250 mg #6 THM—Take 1 tablet by mouth 2 times a day for 3 days |
| Ciprofloxacin 500 mg #14 THM—Take 1 tablet by mouth 2 times a day as directed |
| Clindamycin 150 mg #56 THM–Take __ capsule(s) by mouth every __ hour(s) as directed |
| Clonidine 0.1 mg #25 THM—Take 1 tablet by mouth 4 times a day for 3 days, 3 times a day for 2 days, twice daily for 2 days, then 1 daily |
| Diphenhydramine 25 mg #20 THM—Take 1 tablet by mouth every 6 to 8 hours as needed for itching, anxiety, insomnia |
| Doxycycline 100 mg #20 THM—Take 1 capsule by mouth every 12 hours for 10 days |
| Ibuprofen 600 mg #10 THM—Take 1 tablet by mouth every 6 to 8 hours as directed |
| Methocarbamol 750 mg #28 THM—Take 1 tablet by mouth 4 times a day or as directed |
| Moxifloxacin 400 mg #7 THM—Take 1 tablet by mouth every day for 7 days |
| Nitrofurantoin 100 mg #28—Take 1 capsule by mouth 4 times daily for 7 days |
| Penicillin VK 500 mg #40 THM –Take __tablet(s) by mouth every __ hours. Take until all finished. |
| Phenytoin 100 mg #21 THM—Take 1 capsule by mouth 3 times a day as directed |
| Prednisone 10 mg #30 THM—Take __ tablet(s) by mouth every __ hour(s) as directed |
| Promethazine 25 mg #6 THM—Take 1 tablet by mouth every 8 hours as needed for nausea |
Selection of Participants
Consecutive adult patients discharged from the ED with either a THM or an equivalent SPP from August 26, 2012, to September 22, 2012, were considered for inclusion. Patients were excluded if they were younger than 18 years, received a combination of THMs and SPPs, were admitted to the hospital, or were discharged to a location other than home. In addition, patients were excluded from analysis if they returned to the ED after being instructed to do so upon discharge from the index visit, such as for a wound recheck. Inclusion was not contingent on presenting complaint or discharge diagnosis.
Methods and Measurements
ED patients discharged with a THM or equivalent SPP during the study period were prospectively identified through daily pharmacy reports. For each patient, baseline characteristics including age, gender, identification of a PCP, primary language, ethnicity, marital status, and insurance status were recorded from the electronic medical record (EMR). Review of the EMR was used to determine whether patients returned to the ED within 30 days, and whether any repeat visits were complaint-specific, that is, the same complaint targeted by the THM or SPP from the index visit. We also recorded whether patients saw another provider in the university health care system, such as a primary care clinic or urgent care, within 30 days. The study was IRB approved.
Data Analysis
Patient demographic characteristics and types of medications prescribed were compared between the study groups using the appropriate bivariate analysis (t test for continuous and chi-square for categorical variables, respectively).
The all-cause 30-day return rate was the primary outcome variable. All variables were examined for bivariate significance in relation to this outcome variable. Significant variables were included in the model. Multiple logistic regression was used to compare the odds of a 30-day ED visit between the study groups after controlling for potential confounders. Hosmer-Lemeshow statistic was used to determine goodness of fit.
Data analysis was performed using SPSS 21 (IBM, Armonk, New York). A power analysis was performed assuming equal sized groups and a normal return rate to the ED of 25% based on previous experience. We found 80% power to show a decrease of 10% in return rates using 250 patients per group or 500 total patients.
Results
Characteristics of Study Subjects
Pharmacy reports identified 826 eligible patients, of whom 115 were excluded (Figure 1). The most common reason for exclusion was planned repeat ED visit (34.8%). Among the 711 subjects included, 268 received a THM and 443 received a SPP. No significant differences were found between groups in demographic characteristics or the reason for medication; however, there were significant differences in the medication prescribed. Compared with the SPP group, individuals in the THM group were more likely to receive antibiotics (66% vs 49%), methocarbamol (9% vs 5%), and albuterol (12% vs 4%) but were less likely to receive ibuprofen (15% vs 34%). These results can be seen in Table 2.
Figure 1.
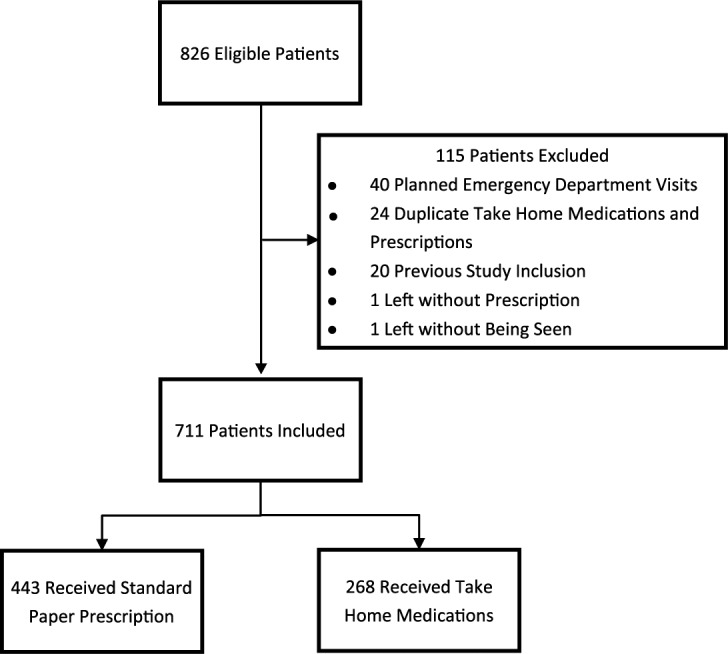
Patient Flow.
Table 2.
Demographic Comparison of Study Groups.
| All subjects (n = 711) | THM (n = 268) | SPP (n = 443) | P value | |
|---|---|---|---|---|
| All-cause 30-day ED return | 100 (15%) | 53 (20%) | 56 (13%) | .01 |
| Age | 41 ± 15 | 40 ± 14 | 42 ± 16 | NS |
| Male gender | 334 (47%) | 132 (49%) | 202 (46%) | NS |
| Has a PCP | 281 (40%) | 99 (37%) | 182 (41%) | NS |
| English | 615 (87%) | 241 (90%) | 374 (84%) | NS |
| Single | 493 (69%) | 199 (74%) | 294 (66%) | NS |
| Ethnicity | NS | |||
| Caucasian | 171 (24%) | 64 (24%) | 107 (24%) | |
| Hispanic | 361 (51%) | 130 (49%) | 231 (52%) | |
| Native American | 66 (9%) | 29 (11%) | 37 (8%) | |
| African American | 28 (4%) | 11 (4%) | 17 (4%) | |
| Insurance | .02 | |||
| Self-pay | 261 (37%) | 115 (43%) | 146 (33%) | |
| Public | 208 (29%) | 67 (25%) | 141 (32%) | |
| Private | 105 (15%) | 31 (12%) | 74 (17%) | |
| Institutional | 137 (19%) | 55 (21%) | 82 (19%) | |
| Reason for initial visit | <.01 | |||
| Pain | 198 (28%) | 45 (17%) | 153 (35%) | |
| Respiratory illness | 101 (14%) | 52 (19%) | 49 (11%) | |
| Skin/wound care | 122 (17%) | 65 (24%) | 57 (13%) | |
| UTI | 102 (14%) | 32 (12%) | 70 (16%) | |
| Other | 188 (26%) | 74 (28%) | 114 (26%) | |
| Medicationa | ||||
| Antibiotics | 392 (55%) | 176 (66%) | 216 (49%) | <.01 |
| Ibuprofen | 191 (27%) | 39 (15%) | 152 (34%) | <.01 |
| Methocarbamol | 45 (6%) | 25 (9%) | 20 (5%) | .01 |
| Albuterol | 49 (7%) | 33 (12%) | 16 (4%) | <.01 |
| Prednisone | 51 (7%) | 19 (7%) | 32 (7%) | NS |
| Phenergan | 50 (7%) | 13 (5%) | 37 (8%) | NS |
| Other | 29 (4%) | 11 (4%) | 18 (4%) | NS |
Note. THM = Take Home Medication; SPP = standard paper prescription; ED = emergency department; NS = nonsignificant; PCP = primary care provider; UTI = urinary tract infection.
Because of overlap in medication use, each medication was its own variable.
Analysis of 30-Day Returns
No significant difference was found between the THM and SPP groups with respect to non-ED provider visits in the university system. Among THM patients, 81 (30%) saw a non-ED provider within 30 days. Within the SPP group, 165 patients (37%) had a recorded visit with a non-ED provider.
In the bivariate analysis, there was a significant difference between patients receiving THMs (53/268, 20%) versus those receiving SPPs (56/443, 13%) in all-cause 30-day returns to the ED (difference = 7%, 95% confidence interval [CI], 0%-15%). For cause-specific 30-day returns, there was no significant difference comparing THM (33/268, 12%) to SPP (35/443, 8%) groups (difference = 4%, 95% CI, -2 to 11). There were multiple reasons for the return ED visits. Approximately 3/4 of the cases were pain related (28%), respiratory complaints (14%), urinary tract infection (14%), and skin/wound care (17%). Other diagnostic categories each represented less than 5% of the cases. For consideration in the multivariable analysis, the variable was reduced to one of these 4 diagnostic groups or other.
A bivariate analysis comparing 30-day all-cause returns to the study group, all demographic variables, and medication variables was only significant for the study group (THM vs SPP, P = .01), ethnicity (P < .01), and insurance (P < .01). Gender trended toward significance (P = .067) and was also included in the multiple variable model. The logistic regression model compared all-cause return to the ED as the outcome variable to these significant demographic variables and the study group (THM vs SPP) as independent variables. A number of independent predictors of all-cause ED returns were identified. Variables associated with increased odds of returning to the ED within 30 days included study group (aOR: 1.7), male gender (aOR: 1.6), African American ethnicity (aOR: 3.0), public insurance (aOR: 3.3), and institutional financial assistance (aOR: 5.0). Table 3 lists the results of the logistic model and 95% CIs. The Hosmer-Lemeshow statistic was 0.8 indicating good fit to the model.
Table 3.
Logistic Regression Model Using 30-Day All-Cause ED Returns as the Outcome Variable and All Variable With Bivariate Significance as Predictors.
| Adjusted odds | 95% CI | P value | |
|---|---|---|---|
| THM vs SPP | 1.7 | 1.1-2.6 | .01 |
| Male gender | 1.6 | 1.1-2.5 | .03 |
| Ethnicity | |||
| Caucasian | Ref | ||
| Hispanic | 1.0 | 0.6-1.7 | NS |
| Native American | 1.2 | 0.6-2.7 | NS |
| African American | 3.0 | 1.2-7.4 | .02 |
| Insurance | |||
| Private | Ref | ||
| Self-pay | 2.2 | 0.9-5.4 | NS |
| Public | 3.3 | 1.3-8.3 | .01 |
| Institutional | 5.1 | 2.0-13.0 | <.01 |
| Reason for initial visit | |||
| Pain | Ref | ||
| Respiratory | 0.4 | 0.1-1.5 | NS |
| Skin/wound care | 0.9 | 0.3-3.3 | NS |
| Urinary tract infection | 1.2 | 0.3-4.7 | NS |
Note. CI = confidence interval; THM = Take Home Medication; SPP = standard paper prescription; NS = nonsignificant.
Discussion
Our study showed that patients given THMs were more likely to return to the ED within 30 days but often for a problem unrelated to the initial complaint. These study findings contradict the initial hypothesis that patients receiving THMs would be less likely to return to the ED within 30 days. The trend for cause-specific ED returns was in the same direction as the all-cause returns suggesting that had our sample size been larger we may have found the same results for this group.
There are several potential explanations for these results. It is possible that providers preferentially give THMs to patients with fewer resources, who are more likely to use the ED as a usual source of care. This would be consistent with the finding that the THM group had a higher rate of return visits for all-causes but did not demonstrate significantly increased return rate for the index visit complaint. Along similar lines, it may be that without the availability of THMs, the group receiving these medications would have had significantly higher rates of return. In other words, THMs may equalize patients who face increased barriers to access with those who have adequate ability to access discharge prescriptions as outpatients.
Another possibility is that THMs enhance patient satisfaction, increasing the likelihood of using the ED as a preferred source of care. For patients with barriers to follow-up, such as lack of transportation and limited financial resources, it is likely more convenient to receive both medical care and the necessary THM together in a single location as compared with adding a visit to the pharmacy, as would be the case if receiving treatment in most outpatient clinic settings. Of note, our institution does not have an outpatient pharmacy physically located in the hospital, which could be a barrier to patients filling a SPP.
There are few previous studies examining THMs. One study by Strang et al found that patients given education and a home naloxone supply were able to successfully use naloxone to reverse opiate overdose. Another study describing the use of medication kits for symptomatic emergencies found 86% of home hospice services reported the kits averted hospital or ED visits.16,17 However, neither of these studies addressed the effect of dispensing medication packs on ED recidivism. Lark and Phillips examined the effect of providing 3 day starter packs of antibiotics in the ED and found only 48% of patients receiving these packs ultimately obtained the follow-up prescription from either a general practitioner or hospital pharmacy.15 Similarly, Lam et al found that among patients provided a full antibiotic course to take at home, 9% reported taking none of the medication, while an additional 22% stated they did not complete the full medication course.13 Another study reported no difference in adherence rates for patients given a complete antibiotic course rather than prescription.14 A study by Ginde et al showed only 74.2% of patients given paper prescriptions actually filled them but found no difference in recurrent ED visits or hospitalizations when compared with patients given a complete 5-day course of azithromycin dispensed from the ED.5 More recently, Hayes et al demonstrated a 50% reduction in return ED visits for specific conditions when patients were discharged with “to-go” antibiotics.18
Our findings differ from those found in the recent study by Hayes et al.18 Both studies were performed in urban academic settings in which provision of THMs is at the discretion of the primary provider rather than strictly protocol-driven. However, there are also several differences in design between the 2 studies. The Hayes study used a retrospective approach, using a convenience sample, with a follow-up period of 7 days. In contrast, the current study was prospective, reviewed all patients seen in the ED during the study period for eligibility, and used a 30-day follow-up window. While Hayes et al looked at antibiotics and a specified set of diagnoses, we included all available THMs and did not proscribe specific diagnoses. For comparison to the Hayes study, we re-ran an analysis of our data looking at 7-day return and found the same trend toward increased ED returns by the THM group (10% vs 6%, P = .6) still present. It is possible that the distinct follow-up duration as well as medications and conditions included underlie the divergent results.
Limitations
This study had several limitations. The research was conducted within a single university health system, and it is unknown whether patients presented to other EDs within the 30-day window. Furthermore, it is unknown whether patients in the SPP group filled their prescriptions and whether patients in either group completed the full course of medications.
In addition, as noted above the decision to provide a THM is at the discretion of the treating provider. Because THMs have been an integral part of practice in our ED for many years, it was not possible to conduct a prospective randomized controlled trial or to examine rates of return before and after introduction of this resource. Furthermore, as this was an observational study, the results reflect association but do not indicate causation.
Conclusions
Within this study population, patients receiving THMs demonstrated a higher all-cause return rate than patients receiving SPP. We identified specific variables that help predict the reason for these returns.
As CMS places increasing emphasis on preventable readmissions or “bounce-backs,” strategies for improving the quality of discharge care, such as the use of THMs, will continue to be of wide interest throughout the medical community.19 The results of this study suggest that further research is needed in the area of utilizing THMs to reduce repeat ED visits.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Thomas EJ, Burstin HR, O’Neil AC, Orav EJ, Brennan TA. Patient noncompliance with medical advice after the emergency department visit. Ann Emerg Med. 1996;27(1):49-55. [DOI] [PubMed] [Google Scholar]
- 2. Gadkari AS, McHorney CA. Medication nonfulfillment rates and reasons: narrative systematic review. Curr Med Res Opin. 2010;26(3):683-705. [DOI] [PubMed] [Google Scholar]
- 3. James TD, Smith PC, Brice JH. Self-reported discharge instruction adherence among different racial groups seen in the emergency department. J Natl Med Assoc. 2010;102(10):931-936. [DOI] [PubMed] [Google Scholar]
- 4. Olshaker JS, Barish RA, Naradzay JF, Jerrard DA, Safir E, Campbell L. Prescription noncompliance: contribution to emergency department visits and cost. J Emerg Med. 1999;17(5):909-912. [DOI] [PubMed] [Google Scholar]
- 5. Ginde AA, Von Harz BC, Turnbow D, Lewis LM. The effect of ED prescription dispensing on patient compliance. Am J Emerg Med. 2003;21(4):313-315. [DOI] [PubMed] [Google Scholar]
- 6. Hohl CM, Abu-Laban RB, Brubacher JR, et al. Adherence to emergency department discharge prescriptions. CJEM. 2009;11(2):131-138. [DOI] [PubMed] [Google Scholar]
- 7. Saunders CE. Patient compliance in filling prescriptions after discharge from the emergency department. Am J Emerg Med. 1987;5(4):283-286. [DOI] [PubMed] [Google Scholar]
- 8. Freeman CP, Guly HR. Do accident and emergency patients collect their prescribed medication? Arch Emerg Med. 1985;2(1):41-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Matsui D, Joubert GI, Dykxhoorn S, Rieder MJ. Compliance with prescription filling in the pediatric emergency department. Arch Pediatr Adolesc Med. 2000;154(2):195-198. [DOI] [PubMed] [Google Scholar]
- 10. Kajioka EH, Itoman EM, Li ML, Taira DA, Li GG, Yamamoto LG. Pediatric prescription pick-up rates after ED visits. Am J Emerg Med. 2005;23(4):454-458. [DOI] [PubMed] [Google Scholar]
- 11. Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication in primary care. BMJ. 1993;307(6908):846-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25(4):284-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lam F, Stevenson FA, Britten N, Stell IM. Adherence to antibiotics prescribed in an accident and emergency department: the influence of consultation factors. Eur J Emerg Med. 2001;8(3):181-188. [DOI] [PubMed] [Google Scholar]
- 14. Ho J, Taylor DM, Cabalag MS, Ugoni A, Yeoh M. Factors that impact on emergency department patient compliance with antibiotic regimens. Emerg Med J. 2010;27(11):815-820. [DOI] [PubMed] [Google Scholar]
- 15. Lark KA, Phillips CE. Do patients get the best deal when antibiotics are prescribed out of hours? J Accid Emerg Med. 1997;14(3):159-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Strang J, Manning V, Mayet S, et al. Overdose training and take-home naloxone for opiate users: prospective cohort study of impact on knowledge and attitudes and subsequent management of overdoses. Addiction. 2008;103(10):1648-1657. [DOI] [PubMed] [Google Scholar]
- 17. Bishop MF, Stephens L, Goodrich M, Byock I. Medication kits for managing symptomatic emergencies in the home: a survey of common hospice practice. J Palliat Med. 2009;12(1):37-44. [DOI] [PubMed] [Google Scholar]
- 18. Hayes BD, Zaharna L, Winters ME, Feemster AA, Browne BJ, Hirshon JM. To-go medications for decreasing ED return visits. Am J Emerg Med. 2012;30(9):2011-2014. [DOI] [PubMed] [Google Scholar]
- 19. Barrueto F, Pimentel L, Hornyak DJ. Analyzing the impact of electronic charting on physician productivity and charge capture using statistical process control: a pilot study. Ann Emerg Med. 2012;60(4):S14. [Google Scholar]


