Abstract
Background: Ketamine in adults has been identified as a safe and effective alternative for multiple indications, each with specific evidence-based dosing ranges. Emergency department (ED) providers are tasked with appropriate ordering of ketamine. A multi-institutional retrospective analysis within EDs at a large health system from November 2013 to October 2015 reviewed ED adult ketamine prescribing patterns for procedural sedation (PS), rapid sequence intubation (RSI), and analgesia. Retrospective cohort results revealed 56% (84 of 150) of PS, 64% (16 of 25) of RSI, and 81.5% (53 of 65) of analgesia ketamine doses fell within indication-specific dosing ranges. Objective: The study purpose was to evaluate the impact of standardizing ED ordering processes to increase appropriate dosing of ketamine. Methodology: Indication-specific adult ED ketamine order panels based on available clinical trial data were implemented in the electronic medical record and ED provider education conducted. Adults at least 18 years of age who received ketamine in the ED for PS, RSI, or analgesia from March 2016 to May 2016 were included. Patients were excluded if no weight or indication was documented. The primary outcome was percentage change in frequency of appropriately dosed ketamine versus the retrospective cohort. The secondary outcome was use of ketamine order panels. Mantel-Haenszel tests were used for statistical analysis. Results: Ketamine for prospective cohort adult ED patients was significantly more likely to be dosed appropriately than in the retrospective cohort (odds ratio: 2.94, 95% confidence interval: 1.1-7.8; P = .0231). Conclusion: Results suggest increased standardization with added decision support increased appropriate indication-specific dosing of ketamine for adults in the ED.
Keywords: ketamine, procedural sedation, rapid sequence intubation, analgesia, emergency department
Background
Ketamine in adults has been identified as a safe and effective alternative for a variety of indications,1 such as procedural sedation,2-4 rapid sequence intubation (RSI),5,6 and analgesia.7-9 A keto-amine structurally similar to Phencyclidine (PCP), ketamine primarily acts by competitive inhibition of N-methyl-d-aspartate. Ketamine’s sedative properties create a state of dissociative isolation, allowing patients to maintain spontaneous airway reflexes while remaining fully sedated. The most common use of ketamine in adults is in procedural sedation, often used in conjunction with propofol. Ketamine use may also be indicated in RSI when a difficult airway is anticipated or encountered or in situations where a patient may be hypotensive. Analgesia is not a first-line indication, but ketamine can be considered when a contraindication to opioids is present or when opioids are ineffective. Absolute contraindications to ketamine use include infants less than 3 months of age and schizophrenia (even if controlled). Relative contraindications include elevated intracranial and/or intraocular pressures and conditions where elevated blood pressure may be hazardous. Emergence reactions have been associated with ketamine, with hallucinations and visual disturbances occurring at a rate of approximately 12% in clinical trials.1
Emergency department (ED) physicians often order ketamine in adults for multiple indications without specific decision support or dosing guidance. Inappropriate dosing can lead to unwanted adverse effects or inadequate treatment of analgesia or sedation. A multi-institutional retrospective analysis reviewed adult ED ketamine usage within a large health system from November 1, 2013, to October 1, 2015, to gain insight into ED prescribing patterns for the most commonly prescribed ketamine indications: procedural sedation, RSI, and analgesia. The retrospective period yielded 240 ketamine doses system-wide, with the majority of doses (n = 150) falling in the procedural sedation category as expected, followed by analgesia (n = 65) and RSI (n = 25). Retrospective analysis results revealed 56% of procedural sedation, 64% of RSI, and 81.5% of analgesia ketamine doses fell within indication-specific evidence-based dosing ranges. The purpose of this study was to evaluate the impact of standardizing the ordering process with the intent of increasing appropriate dosing of ketamine in the ED.
Methodology
To standardize the adult ketamine ordering process in the ED and provide a greater degree of decision support for emergency department providers (EDPs), indication-specific adult ED ketamine order panels which included dosing information (see Appendix) and contraindications based on available clinical trial data were implemented in the electronic medical record (EMR). Previously, EDPs were presented with generic ketamine order choices based on medication strength and route (eg, “Ketamine (KETALAR) injection 10 mg/mL (IV use)”). The individual orders contained wording conveying ordering provider restrictions on ketamine but no further decision support or dosing guidance. Figure 1 shows the previous EDP order list view when searching “KETAMINE.” The new ketamine order process instead associates ketamine order choices with specific indications (eg, “Ketamine – Analgesia”). Figure 2 displays the newly implemented EDP order list view for “KETAMINE.”
Figure 1.
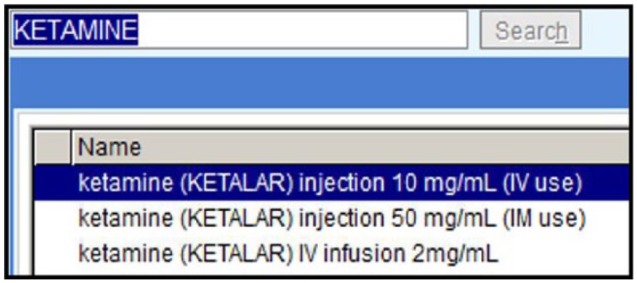
Previous emergency department provider electronic medical record order list view when searching “KETAMINE.”
Figure 2.
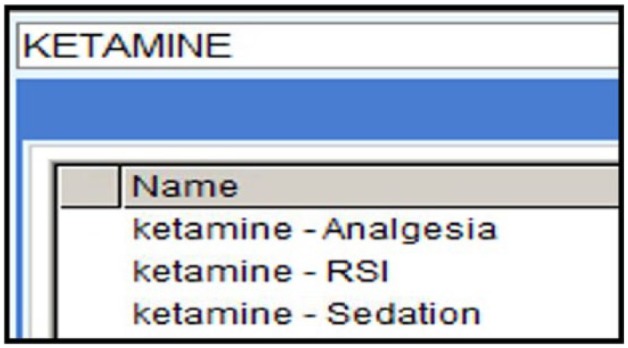
New emergency department provider electronic medical record order list view when searching “KETAMINE.”
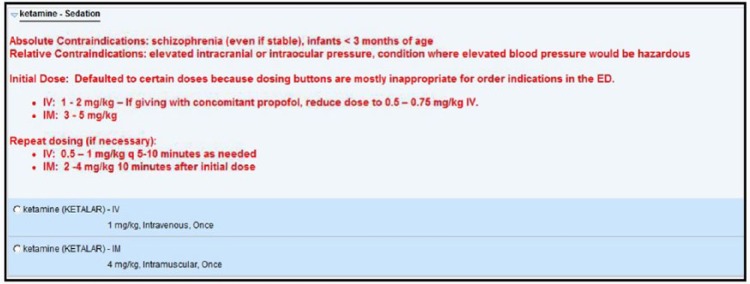
In addition to the previously included ordering provider restrictions, decision support for EDPs was added within the indication-specific adult ED ketamine orders. Information on absolute and relative contraindications and information on ketamine initial and repeat dosing for both intravenous and intramuscular routes were included in the “Notes” section of the order for convenient reference. Prespecified doses within the evidence-based indication-specific ranges were also autopopulated to aid providers in efficient and appropriate ketamine prescribing, with the opportunity to alter the default dose if desired by the EDP. Figure 3 shows an example view of the “Ketamine – Sedation” adult ED ketamine order. Due to the need for ketamine use in non-ED settings, the generic ketamine order entry options were not removed; however, these generic order options were replaced by the indication-specific order options on the EDP order entry preference list to aid in choosing these options instead.
Figure 3.
Example view of new adult indication-specific ketamine order (shown: Ketamine – Sedation).
Provider education was conducted on ketamine and the new ordering process at an EDP monthly meeting, and EDPs were supportive and willing to use the indication-specific ketamine order panels going forward. The ketamine education and ordering process changes were placed on the EDP main EMR login-screen for reference.
Eligible patients for the study post-implementation of the adult ED ketamine order panels included adults at least 18 years of age who received ketamine in the ED for procedural sedation, RSI, or analgesia from March 1, 2016, to May 1, 2016. Patients were excluded in both the retrospective and prospective study phases if no ketamine indication and/or weight was documented in the EMR or if ketamine was ordered for an alternate indication not included in this study. Figure 4 displays the retrospective patient selection process. Figure 5 displays the prospective patient selection process. The primary outcome was percentage change in frequency of appropriately dosed ketamine compared with the retrospective cohort. The secondary outcome was use of indication-specific adult ED ketamine order panels. Mantel-Haenszel tests were used for statistical analysis, controlling for indication.
Figure 4.
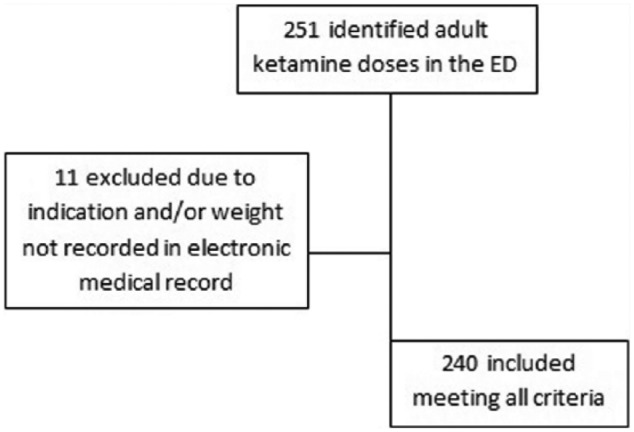
Retrospective phase patient selection.
Note. ED = emergency department.
Figure 5.
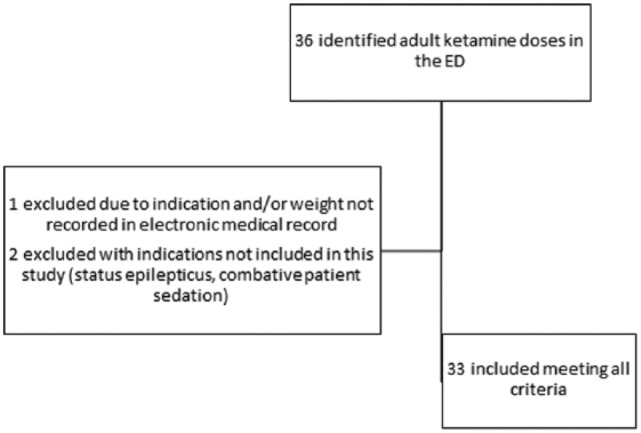
Prospective phase patient selection.
Note. ED = emergency department.
Baseline demographics were similar between groups with regard to age. More males versus females were seen in the prospective cohort versus the retrospective cohort, and patients in the prospective cohort weighed an average of 8 kg more than the retrospective cohort patients. Table 1 displays study group baseline characteristics.
Table 1.
Baseline Characteristics.
| Characteristic | Retrospective | Prospective |
|---|---|---|
| Age (mean), y | 48.3 | 49 |
| Sex (male), n (%) | 110 of 240 (45.8) | 17 of 33 (51.5) |
| Weight (mean), kg | 82.2 | 90.2 |
Results
Thirty-three patients were included in the prospective cohort versus 240 patients included in the retrospective cohort. Analysis demonstrated adult ED ketamine doses in the prospective cohort were significantly more likely to be dosed appropriately than ketamine doses in the retrospective cohort (odds ratio: 2.94, 95% confidence interval: 1.1-7.8; P = .0231). Orders for ketamine were always placed prior to administration due to ketamine storage in the central/ED satellite pharmacies rather than automated dispensing cabinets. Table 2 shows the percentage of appropriately dosed ketamine versus retrospective data. Improvement in appropriate dosing was seen across indications, with 75% (15 of 20) of procedural sedation, 88.9% (8 of 9) of RSI, and 100% (4 of 4) of analgesia doses falling within appropriate indication-specific ranges. Table 3 displays the percentages of appropriately dosed ketamine versus retrospective data by indication. During the prospective cohort, 81.8% (27 of 33) of ketamine doses were ordered using the new indication-specific adult ED ketamine order panels (shown in Table 4). An improvement was also seen with reduced numbers of analgesia doses given first-line without a documented reason, with 0% (0 of 4) in the prospective phase versus 12.3% (8 of 65 doses) in the retrospective phase. Ketamine doses ordered for patients with a documented contraindication to therapy were 1.3% (3 of 240 doses) in the retrospective phase versus 0% (0 of 33 doses) in the prospective phase. Six emergence reactions were documented in the retrospective phase of 240 ketamine doses (2.5%), whereas zero were documented in the prospective phase. The prospective phase included one documented ketamine order each for status epilepticus and combative patient sedation indications, not included in the analysis.
Table 2.
Primary Outcome: Percentage of Appropriately Dosed Ketamine Versus Retrospective Data.
| All indications | Retrospective, n (%) | Prospective, n (%) | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Total ketamine doses | 153 of 240 (63.8) | 27 of 33 (81.8) | 2.94 | 1.1-7.8 | .0231 |
Note. OR = odds ratio; CI = confidence interval.
Table 3.
Percentages of Appropriately Dosed Ketamine Versus Retrospective Data by Indication.
| Indication | Retrospective, n (%) | Prospective, n (%) |
|---|---|---|
| Analgesia | 53 of 65 (81.5) | 4 of 4 (100) |
| Rapid sequence intubation | 16 of 25 (64) | 8 of 9 (88.9) |
| Procedural sedation | 84 of 150 (56) | 15 of 20 (75) |
Table 4.
Secondary Outcome: EDP Use of Indication-Specific Adult Ketamine Order Panels.
| Indication | Prospective, n (%) |
|---|---|
| Analgesia | 4 of 4 (100) |
| Rapid sequence intubation | 6 of 9 (66.7) |
| Procedural sedation | 17 of 20 (85) |
| Total | 27 of 33 (81.8) |
Note. EDP = emergency department provider.
Discussion
Indication-specific adult ketamine order panels in the ED provided EDPs added decision support and autopopulation of default doses. These new order panels increased standardization of the adult ED ketamine ordering process and helped to significantly increase appropriate indication-specific dosing of ketamine in adults in the ED. For example, procedural sedation dosing appropriateness issues seemed to center around the differences in dosing recommendations surrounding the concomitant use of propofol with ketamine versus dosing recommendations for ketamine alone,4 and the new ordering process displayed both dosing ranges on the order screen for provider reference. Ketamine dosing for procedural sedation was evaluated as a whole, and differences in dosing patterns of the ketamine/propofol combination were not evaluated versus ketamine alone in this analysis. EDP education conducted on ketamine may also be a factor in improved appropriateness of ketamine ordering. No inappropriate first-line ketamine for analgesia doses were ordered in the prospective cohort, whereas 8 doses were ordered in the retrospective cohort without clear documentation of the patient having a contraindication to or inadequate response to opioids. Also, no ketamine doses were ordered for patients with contraindications to therapy in the prospective cohort, an improvement over 3 in the retrospective cohort, although the sample size may be too small to definitively make this statement. Ketamine for RSI seemed to be the indication utilized the least, in part due to ketamine not being included in pre-made “RSI kits” readily available in the ED automated dispensing cabinets. EDPs must obtain ketamine from the central pharmacy or ED satellite pharmacies, potentially limiting practical use of ketamine for this often more time-sensitive indication. Of note, 6 emergence reactions were documented in the retrospective phase of 240 ketamine doses (2.5%), whereas zero were documented in the prospective phase. A wide array of reported frequency of emergence reactions in literature suggests the true percentage of emergence reaction occurrence to be currently unknown, with most drug references reporting a frequency of approximately 12%.1 This study’s evaluation of emergence reaction frequency was somewhat limited by whether or not the reaction was documented in the EMR by the EDP. The small size of the prospective cohort in comparison with the retrospective cohort was not ideal and difficult to avoid, with retrospective data spanning 2 years and prospective data spanning only 3 months in comparison due to time limitations associated with a residency-related project. Preliminary data look promising, but ideally, a larger prospective cohort sample size would be desired to more adequately make comparisons between groups.
Despite no longer displaying on the EDP order preference list, the previous generic ketamine order entry options were still available for use in non-ED settings, meaning the EDP could still select these options if desired. As evidenced by 81.8% usage of the new ketamine order panels, EDPs were supportive of the new ordering process with added decision support and associated education. The willingness of providers to participate in using the ED ketamine order panels was a key factor in the success of this study. Health care providers can play a role in impacting the ketamine ordering process for adults in the ED by helping direct EDPs to indication-specific ketamine order panels if applicable, encouraging evidence-based indication-specific dosing, and encouraging first-line use of ketamine only in appropriate situations.
Indication-specific orders for ketamine worked very well in this setting, and this concept is simplistic enough to potentially be applied to other agents and environments. Implementing this type of intervention for other medications with indication-specific dosing may be an option to facilitate appropriate evidence-based dosing and improve patient safety outcomes without drastically changing provider workflows.
Conclusion
Increased standardization with added decision support for the adult ketamine ordering process in the ED increased the appropriate indication-specific dosing of ketamine for adults in the ED. Education surrounding ketamine also seemed to improve appropriate and more consistent ketamine use. The general concept of the addition of decision support in the form of indication-specific orders could prove beneficial to apply to other agents in specific situations.
Appendix
Appendix.
Summary of Adult Ketamine Indication-Specific, Evidence-Based Dosing Ranges in ED.
| Indication | Dosing | Order default dosing |
|---|---|---|
| Analgesia | Bolus (ie, subdissociative dosing) 0.15 mg/kg, up to <1 mg/kg IV Alternatively, 1.5-2 mg/kg IM Repeat dosing (assess after 30 minutes) 0.15-0.3 mg/kg IV 1.5 mg/kg IM |
0.3 mg/kg IV or 1.5 mg/kg IM |
| Rapid sequence intubation | Bolus: 1-2 mg/kg IV Repeat dose if adequate sedation not achieved: 0.5-1 mg/kg IV |
1 mg/kg IV |
| Procedural sedation | Bolus 1-2 mg/kg IV (If given with concomitant propofol, give 0.5-0.75 mg/kg IV) Alternatively, 3-5 mg/kg IM Repeat dosing (if necessary) 0.5-1 mg/kg IV every 5-10 minutes as needed Repeat dosing (if necessary—10 minutes after initial dose) 2-4 mg/kg IM |
1 mg/kg IV or 4 mg/kg IM |
Note. ED = emergency department; IV = intravenous; IM = intramuscular.
Footnotes
Authors’ Note: This paper was previously presented at Southeastern Residency Conference (SERC) held in Athens, Georgia (April 29, 2016).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Evers AS, Crowder CM, Balser JR. General anesthetics. In: Brunton LL, ed. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 11th ed. New York, NY: McGraw-Hill; 2006;341-368. [Google Scholar]
- 2. Green M, Roback MG, Kennedy RM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med. 2011;57:449-461. [DOI] [PubMed] [Google Scholar]
- 3. Morris C, Perris A, Klein J, Mahoney P. Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agents? Anaesthesia. 2009;64:532-539. [DOI] [PubMed] [Google Scholar]
- 4. Thomas MC, Jennett-Reznek AM, Patanwala AE. Combination of ketamine and propofol versus either agent alone for procedural sedation in the emergency department. Am J Health Syst Pharm. 2011;68:2248-2256. [DOI] [PubMed] [Google Scholar]
- 5. Jabre P, Combes X, Lapostolle F, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet. 2009;374:293-300. [DOI] [PubMed] [Google Scholar]
- 6. Patanwala AE, McKinney CB, Erstad BL, Sakles JC. Retrospective analysis of etomidate versus ketamine for first-pass intubation success in an academic emergency department. Acad Emerg Med. 2014;21:88-91. [DOI] [PubMed] [Google Scholar]
- 7. Beaudoin FL, Lin C, Guan W, Merchant RC. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double-blind, clinical trial. Acad Emerg Med. 2014;21:1194-1202. [DOI] [PubMed] [Google Scholar]
- 8. Jouguelet-Lacoste J, La Colla L, Schilling D, Chelly JE. The use of intravenous infusion or single dose of low-dose ketamine for postoperative analgesia: a review of the current literature. Pain Med. 2015;16:383-403. [DOI] [PubMed] [Google Scholar]
- 9. Motov S, Rockoff B, Cohen V, et al. Intravenous subdissociative-dose ketamine versus morphine for analgesia in the emergency department: a randomized controlled trial. Ann Emerg Med. 2015;66:222-229.e1. [DOI] [PubMed] [Google Scholar]