Summary
Ebola virus (EBOV) infection is characterized by sporadic outbreaks caused by zoonotic transmission. Fixed changes in amino acid sequence, such as A82V in the EBOV glycoprotein (GP) that occurred early in the 2013–16 epidemic, are suspected to confer selective advantage. We used biochemical assays of GP function to show that A82V, as well as a polymorphism in residue 544 identified in other outbreaks, enhances infection by decreasing the threshold for activation of membrane fusion activity triggered by host factors cathepsin B and Niemann-Pick C1. Importantly, the increase in infectivity comes with the cost of decreased virus stability. Thus, emergence of a virus GP with altered properties that can affect transmission and virulence may have contributed to the severity and scope of the 2013–16 EBOV epidemic.
Keywords: Ebola, Glycoprotein, NPC1, Membrane fusion, Virus infection, West African outbreak, Makona, Stability
Introduction
The largest documented outbreak of Ebola virus disease (EVD) occurred in West Africa from December 2013 to 2016. Analysis of the nucleotide sequences of early isolates suggests the outbreak was initiated by zoonotic transmission from a unique Ebola virus (EBOV), designated Makona, to one or a few human hosts near Meliandou, Guinea (Holmes et al., 2016). Key features of EBOV Makona infection are characteristic of infections from previous EVD outbreaks: transmission by human-to-human contact, an incubation period between 7–21 days, and principal clinical manifestations of fever and hypovolemia due to diarrhea and cytokine-mediated capillary leak (Team, 2014). Despite these similarities, the Makona outbreak is unique in two significant ways: (1) The location of the outbreak in West Africa was more than 3500 miles away from the site of previous outbreaks in Central Africa, raising the possibility of a unique source, and (2) the size of the outbreak was substantially larger than previous outbreaks (Holmes et al., 2016). By late 2015, the epidemic had spread from Guinea to Liberia and Sierra Leone, and had infected more than 25,000 people with case fatality rates around 40% (Holmes et al., 2016). Thus, important aspects of the EBOV Makona epidemic were distinct from previous EVD outbreaks.
Several teams of scientists in West Africa collected and sequenced EBOV isolates from hundreds of infected hosts, creating a database that catalogued several hundred mutations (Carroll et al., 2015; Gire et al., 2014; Ladner et al., 2015; Park et al., 2015; Quick et al., 2016; Simon-Loriere et al., 2015; Tong et al., 2015). Due to the size and duration of the 2013–16 epidemic, there was public concern that the large number of circulating viruses carrying new mutations provided a pool for selection of rare variants that might be more transmissible or pathogenic. Indeed, sequence analysis identified a mutation encoding a valine substitution for alanine at residue 82 of the EBOV glycoprotein (GP) that appeared in late March 2014 and was present in all subsequent isolates, including in viruses that spread to Liberia, Sierra Leone in two independent introductions, and then returned to Guinea (Gire et al., 2014; Holmes et al., 2016; Ladner et al., 2015). Two recent reports found that infection of primate cells was enhanced by EBOV Makona isolates containing V82 (Diehl et al., 2016; Urbanowicz et al., 2016). In addition, epidemiologic analysis identified an increase in viremia and mortality among hosts infected after July 2014 that closely corresponds to the appearance of V82 (Diehl et al., 2016; Faye et al., 2015). Thus, these findings suggest that alterations in the function of EBOV GP conferred by V82 favor growth and/or transmission of EBOV Makona. As a test of this possibility, we analyzed the effect of A82V on EBOV infectivity and stability using biochemical assays of GP function.
Results
EBOV Makona A82V is more resistant than EBOV Makona to an NPC1-targeting inhibitor
We analyzed murine leukemia virus (MLV) particles pseudotyped with full-length (FL) EBOV GPs from viruses isolated in Guinea (Makona Kissidougou) in early March 2014 and from Sierra Leone in June 2014 that differ solely by A82V (Figures S1 and S2A). As a test of GP function during infection, we measured the sensitivities of these viruses to 3.47, a small molecule inhibitor of EBOV infection that targets the host receptor, Niemann-Pick C1 (NPC1) (Carette et al., 2011; Cote et al., 2011; Lee et al., 2013). We found that particles expressing Makona GP were more sensitive to inhibition by 3.47 than particles expressing Makona A82V GP or 1976 Mayinga GP (Figure 1A). Deletion of the mucin-like domain did not significantly alter virus incorporation or function of GP (Figure S2B) including the 20-fold reduction in the sensitivity to 3.47 inhibition conferred by A82V (Figure 1B, Table 1). As a result, subsequent experiments were performed using mucin-like domain-deleted GPs.
Figure 1. Sensitivity of Makona virus transduction to the NPC1-targeting inhibitor 3.47.

Vero cells were cultured in media containing increasing concentrations of 3.47 (0–2 μM) for 1h before transduction with MLV particles encoding GFP and pseudotyped with either FL GP from Makona, Makona A82V or Mayinga viruses (A) or mucin-like domain deleted GP from Makona or Makona A82V viruses (B). Virus transduction is reported as % of GFP-positive cells relative to cells exposed to DMSO alone. Data are mean ± s.d. (n = 3). See also Table 1. Data in Figure 1B was collected in the same experiment as data in Figures 2B, 3B, S4 and Table 1.
Table 1.
Summary of Sensitivities of Makona and Mayinga GPs to 3.47 Inhibition
| GP | 3.47 IC50 (nM) | LogIC50 |
|---|---|---|
| Mayinga | 5.71 | 0.756 ± 0.181 |
| Makona | 0.682 | −0.167 ± 0.0642 |
| Makona A82V | 14.7 | 1.17 ± 0.170 |
| Mayinga A82V | 6,920 | 3.84 ± 0.141 |
| Mayinga I544T | 0.429 | −0.368 ± 0.0508 |
| Mayinga A82V/I544T | 26.6 | 1.42 ± 0.164 |
| Mayinga A82V/A503V | 9,000 | 3.95 ± 0.223 |
| Mayinga A82V/A503V/I544T | 20.7 | 1.32 ± 0.128 |
Vero cells were grown in media containing the indicated amounts of 3.47 for 1 hr before the addition of MLV particles encoding GFP and pseudo-typed with the indicated GPs. Virus transduction is reported as the percentage of GFP-positive cells relative to cells exposed to DMSO vehicle alone. Data are mean ± SD (n = 3) and summarize data from Figures 1B, 2B, 3B, and S4, which were collected in one experiment. IC50: half maximal inhibitory concentration.
A82V increases activation of EBOV GP by NPC1
Since the target of 3.47 is NPC1, we developed an assay to assess the effect of A82V on GP function. Trimeric ectodomains of GP were purified and cleaved to expose the receptor binding domain, and then incubated with lysosome membranes expressing NPC1. As expected, binding of Makona and Mayinga GPs to lysosome membranes was dependent on expression of NPC1 (Figure S3). Membrane binding by Mayinga GP containing the well-characterized loss of function mutation F535R was markedly reduced (Figure S3A, left panel). This effect was not due to a change in affinity of GP for binding to NPC1 (Figure S3A, right panel), but rather residue 535 is located near the N-terminus of GP2 at the tip of the loop that inserts into the target membrane during virus membrane fusion (Brecher et al., 2012; Gregory et al., 2014; Ito et al., 1999; Lee et al., 2008), indicating that under these conditions, GP binding was dependent on insertion of the fusion loop into the lysosome membrane. Consistent with these results, membrane binding of Makona and Mayinga GPs was also inhibited by KZ52 (Figure S3B), a neutralizing antibody that recognizes and stabilizes the prefusion conformation of GP2 (Lee et al., 2008; Maruyama et al., 1999). These findings indicate that GP binding to lysosome membranes in this assay is dependent on activation of the conformational change in GP2 that is triggered by GP1 binding to NPC1. Using this assay, we observed that the specific activity of Makona A82V GP for activation by NPC1 membranes was significantly greater than that of Makona GP (Figure 2A, top panel) and correspondingly, activation of Makona GP was more sensitive to inhibition by 3.47 (Figure 2A, bottom panel). Taken together with the studies of GP-dependent transduction (Figure 1), these findings suggest that A82V reduces the threshold for NPC1 activation of the conformational change in GP2 that mediates membrane fusion and EBOV infection.
Figure 2. Makona A82V GP has increased NPC1-induced specific activity.

A. Lysosome membranes from CHONPC1 and CHONull cells were incubated with increasing concentrations of Makona or Makona A82V GPΔTM that were cleaved to expose the NPC1 binding domain (top) or incubated with increasing concentrations of 3.47 for 30min prior to the addition of cleaved Makona or Makona A82V GPΔTM (bottom). Membrane-bound and input GP were determined by immunoblot using anti-GP1 serum. See also Figure S3.
B. Vero cells were grown in media containing the indicated concentrations of 3.47 (0–2 μM) for 1h and then transduced with MLV particles encoding GFP and pseudotyped with Makona or Makona A82V GP. Virus transduction is reported as % of GFP-positive cells relative to cells exposed to DMSO vehicle alone. Data are mean ± s.d. (n = 3). See also Table 1. Data was collected in the same experiment as data in Figures 1B, 3B, S4 and Table 1.
C. Comparison of Mayinga and Mayinga A82V GPΔTM binding to lysosome membranes alone (top) or in the presence of 3.47 (bottom) was performed as in A. See also Figure S3.
GP A82 is conserved in all virus isolates from the previous 13 outbreaks of EBOV that have been sequenced (Holmes et al., 2016). To determine if the effect of A82V on GP function is limited to EBOV Makona, we analyzed the properties of Mayinga GP A82V. We found that A82V did not significantly alter Mayinga GP processing or titer of pseudotyped MLV particles on Vero cells (Figure S2B). However like Makona GP, the A82V substitution also increased the sensitivity of Mayinga GP to activation by NPC1 (Figure 2C, top panel) and conferred resistance to 3.47 inhibition (Figures 2B, 2C, bottom panel, Table 1). Thus, the effect of A82V on GP function is not restricted to EBOV Makona.
Identification of an additional polymorphism that regulates GP activity
During the course of these experiments, we noted that transduction by Makona GP-pseudotyped MLV particles was more sensitive to 3.47 inhibition than Mayinga GP-pseudotyped MLV particles (Figure 1A), and this difference was correlated with decreased activation of Makona GP by NPC1 membranes (Figure 3A). Since these proteins share A82, this indicated the existence of an additional determinant(s) of GP activation by NPC1. The amino acid sequences of proteolytically cleaved Mayinga and Makona GPs lacking the mucin-like and glycan cap domains differ at only two positions: A503V and I544T (Figure S1). We evaluated chimeric GPs created by reciprocal exchange of each of these two residues and identified residue 544 as the determinant of the difference in the specific activity of NPC1 activation between Mayinga and Makona GPs. Substitution of threonine for I544 abolished the disparity in sensitivity of transduction to 3.47 inhibition between Mayinga and Makona GPs (Figure 3B), and this effect was correlated with a decrease in NPC1 activation (Figure 3C). In contrast, substitution of valine for A503 had no effect on GP activation. Thus, the magnitudes of the effects of A82V and I544T on GP function are approximately equal and opposite (Table 1, Figure S4).
Figure 3. Residue 544 in GP2 is also a determinant of GP specific activity and transduction.

A. Lysosome membranes from CHONPC1 and CHONull cells were incubated with increasing concentrations of cleaved Mayinga or Makona GPΔTM (top) or incubated with increasing concentrations of 3.47 for 30min prior to the addition of cleaved Mayinga or Makona GPΔTM (bottom). Membrane-bound and input GP1 were analyzed by immunoblot using anti-GP1 serum. See also Figure S3.
B. Vero cells were cultured in media containing the indicated concentrations of 3.47 (0–2 μM) for 1h and then challenged with MLV particles encoding GFP and pseudotyped with Mayinga or Mayinga I544T GP. Virus transduction is reported as % of GFP-positive cells relative to cells exposed to DMSO vehicle alone. Data are mean ± s.d. (n = 3). See also Table 1. Data was collected in the same experiment as data in Figures 1B, 2B, S4 and Table 1.
C. Comparison of Mayinga and Mayinga I544T GPΔTM binding to lysosome membranes alone (top) or in the presence of 3.47 (bottom) were performed as in A. See also Figure S3.
Residues 82 and 544 do not regulate receptor binding
We pursued the role of residue 82 in infection. This residue is located within the α-1 helix that comprises the base of the NPC1 binding pocket at the top of cleaved GP1 (Gong et al., 2016; Lee et al., 2008; Wang et al., 2016). To determine if this residue contributes to receptor binding, we purified the NPC1 lumenal C domain that mediates binding of NPC1 to GP1 (Gong et al., 2016; Miller et al., 2012; Wang et al., 2016), and measured binding of this domain to virus particles expressing GP that had been cleaved to expose the NPC1 binding domain (Miller et al., 2012). We found that binding was concentration-dependent and saturable (Figure 4A). Scatchard analysis indicated the kinetics of NPC1 Domain C binding to GP were first order, consistent with 1:1 stoichiometry observed in the structure of GP/NPC1 complexes determined by cryo-electron microscopy (Gong et al., 2016). Under these conditions, the presence of substitutions A82V or I544T did not significantly alter the binding kinetics of Makona or Mayinga GPs to NPC1 Domain C (Figure 4A). These findings indicate that the salutary effects of V82 and I544 on activation of EBOV infection are not due to an increased affinity of GP1 for NPC1.
Figure 4. Comparative analysis of receptor binding to Makona and Mayinga GPs.
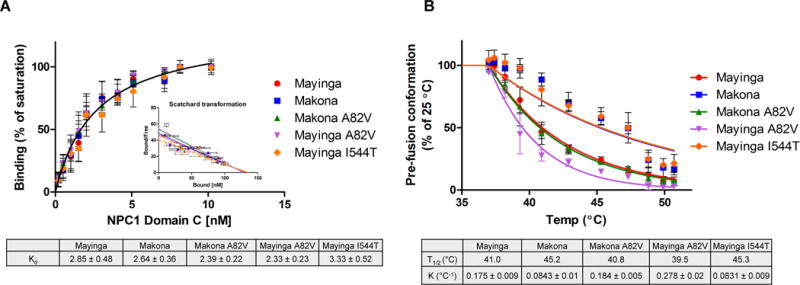
A. MLV particles pseudotyped with the indicated GPs were cleaved to expose the NPC1 binding domain and bound to plates using KZ52 mAb. Bound particles were incubated with increasing concentrations of purified NPC1 Domain C-His6. Bound NPC1 Domain C was detected using α-His6 antibody. Binding is reported as mean ± s.d. (n = 4) of the % of maximum binding for each GP. Pairwise comparison indicates the affinities of these GPs for NPC1 Domain C are not statistically significant (p = 0.18). See also Figure S3.
B. MLV particles pseudotyped with the indicated GPs were cleaved and then heated for 30min at the specified temperatures (T = 25–51.7°C). After cooling to room temperature, virus particles were captured on ELISA plates coated with the GP2 prefusion conformation-specific mAb KZ52. Results are mean ± s.d. (n = 3) of the % of binding for each GP at T = 25°C. Makona vs Makona A82V: p = <0.0001; Mayinga vs Mayinga A82V: p = <0.0001; Mayinga vs Mayinga I544T: p = <0.0001; Mayinga vs Makona A82V: p = 0.4; Makona vs Mayinga I544T: p = 1. See also Figure S5.
Residues 82 and 544 regulate the stability of prefusion GP
Previous studies indicate that like influenza hemagglutinin and HIV envelope glycoprotein, the prefusion conformation of the transmembrane GP2 subunit that mediates EBOV membrane fusion is metastable, and the membrane distal GP1 subunit functions as a clamp to stabilize GP2 as well as a sensor for the NPC1 signal that releases the clamp (Eckert and Kim, 2001; Harrison, 2008; Weissenhorn et al., 1999). It has been shown that brief exposure of metastable virus glycoproteins to elevated temperatures can substitute for host entry factors by providing sufficient energy to release the GP1 clamp on GP2 and initiate the fusion mechanism (Blacklow et al., 1995; Carr et al., 1997; Smith et al., 2004). Based on this model, we measured the effects of A82V and I544T on the thermal sensitivity of GP in virus particles. MLV particles pseudotyped with Makona and Mayinga GPs containing these polymorphisms were incubated at a specific temperature between 25–51.7°C and then analyzed by ELISA for binding to KZ52. The findings reveal that virus particles containing V82 or I544 were significantly more sensitive to thermal inactivation of KZ52 binding than cognate viruses containing A82 or T544, and the effects of V82 and I544 were additive (Figure 4B). Importantly, the thermal inactivation profiles of these virus particles closely correspond to that of sensitivity to activation by NPC1 and to 3.47 resistance exhibited by purified GPs in the NPC1 activation assay, thus indicating that temperature-induced loss of KZ52 binding to GP2 is a marker for GP activation. Taken together, these findings show that V82 and I544 reduce the stability of the prefusion conformation of EBOV GP compared to A82 and T544, and thus reduce the threshold for the conformational change that is induced by NPC1 binding and that mediates membrane fusion and infection.
EBOV infection is dependent on cleavage of GP1 by the endosomal cysteine protease cathepsin B to remove the mucin-like and glycan cap domains and to expose the NPC1 binding domain (Chandran et al., 2005). According to the current model of infection, the spatial and temporal coordination of multiple activated GPs is required to create the pore in the host membrane that is the conduit for transit of the virion core into the cytoplasm (Davey et al., 1999; Harrison, 2008). These studies suggest that a decrease in the threshold for GP activation might increase the efficiency of pore formation and thus reduce the dependence of infection on protease activity (Misasi et al., 2012; Wong et al., 2010). To test this possibility, we analyzed transduction in cells treated with the cathepsin B inhibitor CA074. We found that transduction by particles expressing Makona and Mayinga GPs was inhibited by >80%, and sensitivity to CA074 inhibition was reduced significantly by the introduction of V82. Conversely, the substitution I544T sensitized Mayinga GP and Mayinga A82V GP to inhibition by CA074 (Figure 5A). Taken together with the studies of the NPC1-targeting inhibitor 3.47, these findings indicate that the presence of V82 and I544 reduces the dependence of EBOV infection on expression of the host factors NPC1 and cathepsin B.
Figure 5. Functional comparison of Makona and Mayinga GPs.
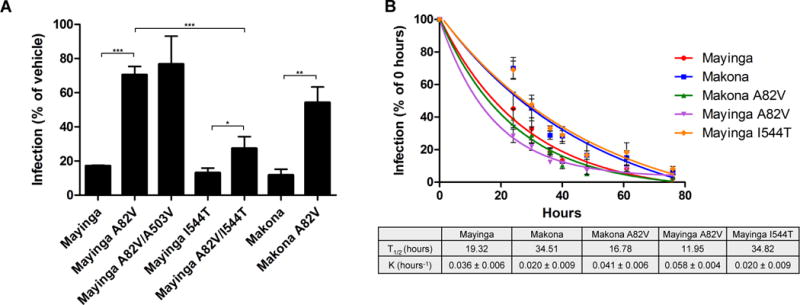
A. Analysis of requirements for the host factor cathepsin B. Vero cells were grown in media containing the cathepsin B inhibitor CA074 (10μM) for 4h before transduction with MLV particles encoding GFP and pseudotyped with the indicated GP. Virus transduction is reported as percent GFP-positive cells relative to cells exposed to DMSO vehicle alone. Data are mean ± s.d. (n = 3). *: p = <0.05; **: p = <0.01; ***: p = <0.001. Mayinga vs Mayinga I544T: n.s.; Makona vs Mayinga I544T: n.s.; Mayinga A82V vs Mayinga A82V/A503V: n.s.
B. Stability of Makona and Mayinga GPs on virus particles. MLV particles encoding GFP and pseudotyped with the indicated GP were incubated at 37°C for the specified times (T = 0–76h) and then assayed for transduction of Vero cells. Data are mean ± s.d. (n = 3) and reported as % of infection at T0. Makona vs Makona A82V: p = 0.02; Mayinga vs Mayinga A82V: p = 0.04; Mayinga vs Mayinga I544T: p = 0.03; Mayinga vs Makona A82V: p = 0.8; Makona vs Mayinga I544T: p = 1.
To model the potential effects of changes in GP stability on virus transmission, we measured the stability of virus particles during incubation at 37°C. We found that particles bearing Makona or Mayinga I544T GPs were significantly more stable than particles bearing Makona A82V and Mayinga GPs, and the destabilizing effects of V82 and I544 (Mayinga A82V GP) were additive (Figure 5B). These findings indicate that the effects of V82 and I544 on virus stability at 37°C are inversely correlated with their effects on NPC1 activation.
Discussion
Extensive sequencing of virus isolates from the 2013–16 EBOV outbreak identified a mutation encoding for substitution of valine for residue A82 in the viral glycoprotein that appeared during the early stages of the outbreak and spread through West Africa during the subsequent expansion resulting in the majority of EVD cases (Carroll et al., 2015; Gire et al., 2014; Ladner et al., 2015; Quick et al., 2016; Simon-Loriere et al., 2015; Tong et al., 2015). Recent studies identified a correlation between the appearance of A82V and an increase in mortality and geographic expansion of the outbreak, suggesting a possible role in EBOV virulence and transmission (Diehl et al., 2016). In this report, we present the results of biochemical analyses of GP that support this view. Our findings show that A82V reduces the stability of the prefusion conformation of GP, which decreases the threshold for activation of membrane fusion and infection.
Residue 82 is located within an α-helix that sits at the base of the NPC1 binding pocket at the top of GP1 (Gong et al., 2016; Lee et al., 2008; Wang et al., 2016). However, our studies do not support the suggestion that changes in residue 82 alter receptor affinity (Diehl et al., 2016; Dietzel et al., 2016; Urbanowicz et al., 2016). The recently obtained structure of GP bound to NPC1 revealed that the α-helix containing A82 is displaced by NPC1 binding, and it was proposed that this conformational change promotes the release of the internal fusion loop in GP2 (Wang et al., 2016). In the receptor bound conformation, the side chain of A82 is located in close proximity to the side chains of W86 and Y109. This is consistent with the possibility that the substitution of valine for A82 enhances the hydrophobic interactions between residues 82, W86 and Y109 that stabilize the displaced conformation of the α-helix and thus reduce the threshold for receptor or thermal signals to activate GP2. Successful infection requires activation of several GPs within a narrow spatial and temporal constraint (Harrison, 2008) and therefore, small changes in receptor expression, receptor affinity for GP1 or in the threshold for activation of GP can markedly alter the probability of productive infection (Davey et al., 1999). Thus the analysis of binding of cleaved GP to NPC1 Domain C may not fully model the effect of A82V on infection. In addition, mutations in the glycan cap and mucin-like domain that appeared during the outbreak may modify the effect of A82V on infection as has been reported (Urbanowicz et al., 2016).
Our studies also led to the discovery that like V82, I544 also destabilizes prefusion GP and enhances GP activation. Unlike V82, which is unique to the West African 2013–16 epidemic, I544 has been found in virus isolates from the Mayinga 1976, Gabon 1994 and Kikwit 1995 outbreaks. A major consequence of the destabilizing effects of V82 and I544 on GP is that these viruses are less sensitive to inhibitors targeting the host factors NPC1 and cathepsin B. This strongly predicts that V82 and I544 promote infection under conditions where expression of NPC1 and/or cathepsin B in target cells is low, such as in tissue monocytes and dendritic cells (DCs) in boundary tissues that are early targets for infection (Bray and Geisbert, 2005; Martinez et al., 2013). Expansion of infection in the host to cells where NPC1 and cathepsin B expression is low, as modeled by the use of 3.47 and CA074, may result in the reported increase in viremia associated with A82V (Diehl et al., 2016; Dietzel et al., 2016). A recent study found that Makona C07 containing T544 grows more slowly and is less virulent than 1976 Yambuku Ecran which, after cleavage, differs from Makona C07 solely by the presence of I544 in GP (Smither et al., 2016). Also, previous comparisons between GPs from a Makona isolate containing V82 and from 1976 Mayinga containing I544 did not find a significant difference in infectivity, cell tropism or membrane fusion activity, which is in line with our findings that V82 and I544 have independent and opposite effects on GP activation (Hofmann-Winkler et al., 2015). Taken together, these findings suggest that polymorphisms that contribute to the stability of the prefusion conformation of GP, including residues 82 and 544, play an important role in viral pathogenesis. To test this hypothesis, detailed studies of the relationship between NPC1 and cathepsin B expression and the replication kinetics and tropism of these viruses in animal models are warranted.
A key finding of our studies is that V82 and I544 reduce the threshold for inactivation of virus infectivity at 37°C, and this is closely correlated with their effects on the thermal stability of prefusion GP. One implication of this finding is that the presence of stabilizing residues A82 and T544 in the Makona isolates obtained from early stages of the outbreak may reflect their suspected origin in bats, whose body temperature can reach 42°C (Brook and Dobson, 2015; O’Shea et al., 2014). In addition, the destabilizing effects of V82 and I544 may also have implications for human-to-human transmission. For example, the results of a recent study of EBOV infectivity under conditions designed to mimic transmission during the West African outbreak found that Makona C05 containing GP T544 had a slower decay rate in drying blood than Mayinga 1976 containing GP I544 (Schuit et al., 2016). Additional studies of the requirements for host-to-host transmission of EBOV Makona particles are needed to assess the effect of A82V on the West African epidemic.
Experimental Procedures
Contact for Reagent and Resource Sharing
Further information and requests for reagents may be directed to and will be fulfilled by the Lead Contact James Cunningham, jcunningham@rics.bwh.harvard.edu (J.M.C.).
Experimental Model Details
Cell Lines
HEK293T and Vero E6 cell lines were obtained from ATCC. CHO-derived cell lines (CHONull and CHONPC1) were a kind gift from the lab of Daniel Ory (Millard et al., 2000). Cell lines (HEK293T, Vero, CHO) were grown at 37°C in 5% CO2. HEK293T and Vero E6 were maintained in DMEM (Invitrogen) containing 10% fetal bovine serum (FBS, Gemini Bio-Products), 100units Penicillin/Streptomycin and 0.292mg/ml L-glutamine (Invitrogen). CHO-derived cell lines were maintained in DMEM/F12 (Invitrogen) containing 5% FBS, 50units Penicillin/Streptomycin and 0.146mg/ml L-glutamine.
Method Details
Generation of expression plasmids
Full length (FL) and mucin domain-deleted (ΔM) 1976 Mayinga GP were previously described (Chandran et al., 2005). Makona GP FL was synthesized to match the reference Kissidougou Guinean sequence (GenBank accession KJ660346) and the mucin domain-deleted (ΔM) derivative (amino acids 309–489 deleted), was created using site-directed mutagenesis (5′-AGAGCAGGACTGATCACAGGCG-3′, 5′-AGAGAAAGACAACTCTTCACTGCGAATT-3′). This PCR added a silent XbaI site at the site of the deletion in each GP. Full length and ΔM Makona A82V GPs were created by substituting a valine for an alanine at position 82 in the Makona GP (5′-TGACTAAAAGATGGGGCTTCAGGT-3′, 5′-CAGATGGCACGTCAGTTGCCAC-3′). Mayinga GPΔM mutants were created by site-directed mutagenesis. Mayinga GPΔM A82V (5′-TAACTAAAAGATGGGGCTTCAGGT-3′, 5′CAGATGGCACGTCAGTTGCCAC-3′); Mayinga I544T GPΔM (5′-CAGAGGGGCTAATGCACAATCAAGATGG-3′, 5′-TGTAAATTCCCTCGGCTGCTGGCC-3′); Mayinga A503V GPΔM (5′-TAATTGTCAATGCTCAACCCAAAT-3′, 5′-CTTCTCTTCGAGTTCTTCTCCCG-3′). Double and triple Mayinga GPΔM mutants (A82V/A503V, A82/I544T and A82V/A503V/I544T) were created by successive site-directed mutagenesis using the primers listed above. Mayinga GPΔMΔTM was previously described (Cote et al., 2011). Makona GPΔMΔTM, Makona A82V GPΔMΔTM, Mayinga A82V GPΔMΔTM and Mayinga I544T GPΔMΔTM were created by deleting the transmembrane domain at the C-terminus (amino acids 657–676 deleted), and replacing it with a GCN4-derived trimerization domain (MKQIEDKIEEILSKIYHIENEIARIKKLIGEV) and a 6×His tag. NPC1 Domain C was previously described (Misasi et al., 2016).
Production and purification of pseudotyped virions
To produce green fluorescent protein (GFP)-encoding Murine Leukemia Virus (MLV) pseudotyped with the indicated EBOV GP, HEK293T cells were plated 24h previously in 15cm plates for 70% confluency the next day. Cells were co-transfected with 8μg MLV gag/pol, 8μg LTR-GFP and 16μg EBOV GP (FL or ΔM) with calcium phosphate. Approximately 24h after transfection, the media was replaced with 14ml fresh media. Supernatants containing EBOV GP pseudotyped MLV particles was collected 24h later and cells were supplemented with an additional 14ml of fresh media. 24h later, supernatants were collected again and combined with supernatants from the first collection. To purify pseudotyped virions, supernatants were spun down at 3,000rpm for 10min at 4°C to remove cell debris and then placed over a 20% sucrose cushion. Virions were pelleted over the sucrose cushion by spinning at 25,000rpm for 1.5h. Pellets were resuspended in NT buffer (10 mM Tris-HCl pH 7.5, 135 mM NaCl) by gentle shaking at 4°C for at least 6h.
Production and purification of EBOV GPΔTM and NPC1 Domain C recombinant proteins
HEK293T cells were plated in a 15cm dish for 90% confluency the next day. Approximately 24h later, media was replaced with DMEM supplemented with 10% FBS and 0.292mg/ml L-glutamine and cells were transfected with 32μg of plasmids encoding EBOV GPΔTM or NPC1 Domain C using Lipofectamine 2000 (Invitrogen) and Opti-MEM I Reduced Serum Media, GlutaMAX Supplement (Invitrogen). Approximately 24h post-transfection, media was replaced with 12ml 293SFMII media (Invitrogen) supplemented with 100units Penicillin/Streptomycin, 0.292mg/ml L-glutamine, 1× MEM Nonessential Amino Acids (Invitrogen) and 2mM CaCl2. 24h later, cell supernatant containing the recombinant proteins was collected and EZ-Block EDTA-Free Protease Inhibitor Cocktail diluted to 1× was added. Cells were supplemented with an additional 12ml of 293SFMII media. 24h later, supernatant were collected again, EZ-Block EDTA-Free Protease Inhibitor Cocktail diluted to 1× was added, and collected supernatants were pooled. To purify recombinant proteins, pooled supernatants were spun down at 3,000rpm for 10min at 4°C to pellet cell debris and filtered through a 0.45μM filter. After filtering, final concentrations of 50mM Na2HPO4, pH 8.0, 300mM NaCl, and 1× EZ-Block EDTA-Free Protease Inhibitor Cocktail were added to supernatants, followed by spinning at 3,000rpm for 10min at 4°C. 1ml Ni-NTA resin (Qiagen) was washed 4× with wash buffer (50mM Na2HPO4, pH 8.0, 300mM NaCl, 20mM Imidazole) at 4°C and added to the supernatants. The resin-supernatant mixture was allowed to rotate at 4°C for 48h. 48h later, Ni-NTA resin was pelleted by spinning at 3,000rpm for 10min at 4°C and supernatants were removed. Ni-NTA resin was washed 3× with wash buffer at 4°C, spinning at 3,000rpm for 10min at 4°C between each wash. After washing, Ni-NTA resin was resuspended in 1ml wash buffer and spun down at 10,000rpm for 3min at 4°C. Protein was eluted from the resin by 4 successive incubations with elution buffer (50mM Na2HPO4, pH 8.0, 300mM NaCl, 250mM Imidazole) for 10min at 25°C and spinning at 10,000rpm for 3min at 4°C between each elution. Eluted protein was dialyzed in PBS using Slide-A-Lyzer Dialysis cartridges (Thermo Fisher) at 4°C for 20h.
Cleavage of EBOV GP Virus and EBOV GPΔTM
Purified EBOV GPΔTM or MLV particles pseudotyped with the indicated GPs were incubated at 37°C for 1h with the metalloprotease thermolysin (0.2mg/ml) or 37°C for 30min with chymotrypsin (0.2mg/ml) in NT buffer (10mM Tris-HCl pH 7.5, 135mM NaCl). The reaction was stopped using 500μM phosphoramidon or 1mM PMSF respectively and incubating at 4°C for 10min. Cleaved EBOV GPΔTM was stored in phosphate-buffered saline (PBS) supplemented with 1mM EDTA, 1mM PMSF and 1× EZ-Block EDTA-Free Protease Inhibitor Cocktail.
Transduction assays with pseudotyped virus
MLV pseudotyped viruses were added to Vero cells in serial ten-fold dilutions and assayed 72h later using fluorescence microscopy. An infectious unit (i.u.) is defined as one GFP-expressing cell within a range where the change in GFP-positive cells is directly proportional to the virus dilution. In experiments involving inhibitors, stock solutions of 3.47 (10mM) or CA074 (10mM) in DMSO were diluted to a final concentration of 1% DMSO in media. Vero cells at 50% confluency and plated in 48-well plates were pre-incubated for 1h (3.47) or 4h (CA074) with the indicated concentrations of inhibitors prior to challenge with equal infectious units of MLV pseudotyped with the indicated GPs. 72h post-infection, the number of GFP positive cells was counted. IC50 values were calculated in GraphPad Prism by fitting to a single-slope dose response curve. All assays were done in triplicate.
For the virus stability assay, MLV particles pseudotyped with EBOV GP were incubated at 37°C for increasing times between 0–78h. Equal initial infectious units (at T0) were used to infect Vero cells at 50% confluency plated in 48-well plates. The number of GFP positive cells was counted 72h post-infection. Curves were fitted to a model of one-phase exponential decay where K is the rate constant and T1/2 = ln(2)/K in GraphPad Prism. Assay was done in triplicate.
Lysosome membrane binding assay
Lysosome membranes were purified from CHONull or CHONPC1 cells. 3×108 cells were washed with PBS twice, scraped in homogenization (HM) buffer (0.25M sucrose, 1mM EDTA, 10mM HEPES pH 7.0), and disrupted with a Dounce homogenizer. Nuclei and debris were pelleted by centrifugation at 1,000g for 10min. The post-nuclear supernatant was centrifuged at 15,000g for 30min at 4°C and the pellet, containing the lysosome membrane, was resuspended in a total volume of 0.9ml composed of 20% Percoll (Sigma) and 0.4% BSA (Sigma) in HM and centrifuged at 36,000g for 30min at 4°C. A 500ml fraction was collected from the bottom of the tube and incubated in 20mM methionine methyl-ester (Sigma) for 1h at room temperature. Following LE/LY disruption, 1×EZ-Block EDTA-Free Protease Inhibitor Cocktail and 1mM PMSF was added.
Disrupted lysosome membranes were blocked for 2h at 25°C with binding buffer (PBS, 5% FBS, 1mM PMSF, 1mM EDTA, 1×EZ-Block EDTA-Free Protease Inhibitor Cocktail). Membranes were pelleted by centrifugation at 13,000rpm for 1min and supernatants were aspirated. Pellets were resuspended in binding buffer containing the indicated amount of purified EBOV GPΔTM, pretreated with thermolysin, and incubated for 1h at room temperature. Unbound proteins were removed by pelleting the membranes as above. Membranes were washed 3× with PBS by resuspending and pelleting. Membrane-bound EBOV GPΔTM was solubilized in SDS-loading buffer with 5% β-mercaptoethanol. Bound and input EBOV GPΔTM were incubated in 1×SDS-loading buffer with 5% β-mercaptoethanol at 70°C for 10min before detection by immunoblot using the rabbit anti-EboV GP1 serum. For binding assays in the presence of 3.47, membranes were pre-incubated at 25°C with the indicated concentration of 3.47 or vehicle (10% DMSO) in binding buffer (10% DMSO final concentration). After 30min, thermolysin-cleaved EBOV GPΔTM was added in the continuous presence of compound, and bound and input GP was measured as described above. For KZ52 inhibition studies, thermolysin-cleaved EBOV GPΔTM was pre-incubated with KZ52 mAb for 1h at 25°C prior to incubation with membranes, and bound and input GP was measured as described above. The specific activity of binding for each GP was defined as the ratio of the intensities of the bands in the immunoblots of bound and input GPs.
GP-NPC1 Domain C binding ELISA
GP-NPC1 Domain C binding ELISA was performed as previously described (Miller et al., 2012). ELISA plates (Corning) were coated with 1μg/ml KZ52 antibody diluted in PBS by incubating overnight at 4°C. The next day, excess KZ52 was removed by washing wells 4× with PBS, and wells were blocked with blocking buffer (PBS + 3% BSA) for 1h at 25°C. Blocking buffer was removed from the wells and replaced with blocking buffer containing MLV particles pseudotyped with EBOV GP that were pre-cleaved with chymotrypsin and incubated at 37°C for 1h. Unbound MLV particles were removed, and wells were washed 4× with PBS. The indicated concentrations of NPC1 Domain C diluted in blocking buffer were added to the wells and incubated at 37°C for 1h. Unbound NPC1 Domain C was removed, and wells were washed 4× with PBS. Wells were incubated with anti-6×His antibody (0.3μg/ml diluted in blocking buffer) for 1h at 25°C, washed 4× with PBS, followed by incubation with anti-mouse IgG-HRP antibody (0.2μg/ml diluted in blocking buffer) for 1h at 25°C to detect bound NPC1 Domain C. Wells were washed 4× with PBS and HRP was developed using ultra TMB substrate. The reaction was stopped with an equal volume of 2M H2SO4 and the OD450 was read. Binding saturation (100%) for each GP was defined as the mean of binding obtained at three increasing concentrations of NPC1 Domain C such that binding at each concentration was not statistically significantly different from the mean. The affinity binding constants (Kd) for each GP were determined by Scatchard analysis and curve fitting to a model of 1:1 binding using GraphPad Prism. Assay was done in quadruplicate.
GP thermal inactivation ELISA
ELISA plates were coated with KZ52 antibody diluted in PBS (1μg/ml) by incubating overnight at 4°C. The next day, excess KZ52 was removed by washing 4× with PBS, and wells were incubated with blocking buffer for 1h at 25°C. Chymotrypsin-cleaved EBOV GP-pseudotyped MLV particles were incubated at a specific temperature between 25–51.7°C for 30min, cooled to room temperature and added to KZ52-coated wells in blocking buffer, followed by incubation for 1h at 37°C. The presence of bound virus was detected using a saturating amount of purified NPC1 Domain C as a probe. Bound NPC1 Domain C was detected as in the GP-NPC1 Domain C binding ELISA outlined above. Curves were fitted to a model of one-phase exponential decay where K is the rate constant and T1/2 = 37°C + ln(2)/K using GraphPad Prism. Assay was done in triplicate.
Co-immunoprecipitation
MLV particles pseudotyped with EBOV GP were cleaved with chymotrypsin to expose the NPC1 binding domain and incubated at 25°C or 51.7°C for 30min. After cooling to room temperatures, virus particles were incubated with NPC1 Domain C at 37°C for 1h. GPs were then solubilized in RIPA buffer (150mM NaCl, 1% NP-40, 0.5% deoxycholic acid, 0.1% SDS, 50mM Tris pH 8.0) containing 1×EZ-Block EDTA-Free Protease Inhibitor Cocktail by incubating on ice for 20min and samples were spun down at 13,000rpm at 4°C for 20min. Supernatants were transferred to a fresh tube and incubated with anti-6×His antibody (2μg/ml), rotating overnight at 4°C. Protein A/G beads (Thermo Fisher) were added to the samples and incubated for 2h at 4°C. Beads were washed three times with RIPA buffer containing 1×EZ-Block EDTA-Free Protease Inhibitor Cocktail, and proteins were eluted from the beads at 95°C for 5 min with 2×SDS loading buffer with 5% β-mercaptoethanol. Immunoprecipitated GP-NPC1 Domain C complexes were detected by immunoblot using the rabbit anti-EboV GP1 serum and rabbit anti-HA antibody. Input GP was detected by immunoblot using the rabbit anti-EboV GP1 serum.
Quantification and Statistical Analysis
Statistical parameters and significance are reported in the Figures and the Figure Legends. Data are determined to be statistically significant when p <0.05 by an unpaired Student’s T-Test (CA074 inhibition) or extra sum-of-squares F test. Asterisks denote statistical significance as: *: p = <0.05; **: p = <0.01; ***: p = <0.001. Statistical analysis was performed in GraphPad Prism 5.
Supplementary Material
Acknowledgments
We would like to thank Marceline Côté and John Misasi for technical advice and assistance. This work was supported by 1U19AI109740 awarded to J.M.C. M.K.W. was supported by NIH grant T32 AI007245.
Footnotes
Author Contributions
M.K.W designed and performed experiments and wrote the manuscript. J.M.C. designed experiments and wrote the manuscript. S-Y.L. performed experiments. S.M.L. carried out preliminary studies.
Authors declare no conflict of interest.
References
- Blacklow SC, Lu M, Kim PS. A trimeric subdomain of the simian immunodeficiency virus envelope glycoprotein. Biochemistry. 1995;34:14955–14962. doi: 10.1021/bi00046a001. [DOI] [PubMed] [Google Scholar]
- Bray M, Geisbert TW. Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. Int J Biochem Cell Biol. 2005;37:1560–1566. doi: 10.1016/j.biocel.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Brecher M, Schornberg KL, Delos SE, Fusco ML, Saphire EO, White JM. Cathepsin cleavage potentiates the Ebola virus glycoprotein to undergo a subsequent fusion-relevant conformational change. J Virol. 2012;86:364–372. doi: 10.1128/JVI.05708-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook CE, Dobson AP. Bats as ‘special’ reservoirs for emerging zoonotic pathogens. Trends Microbiol. 2015;23:172–180. doi: 10.1016/j.tim.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;477:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr CM, Chaudhry C, Kim PS. Influenza hemagglutinin is spring-loaded by a metastable native conformation. Proc Natl Acad Sci U S A. 1997;94:14306–14313. doi: 10.1073/pnas.94.26.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll MW, Matthews DA, Hiscox JA, Elmore MJ, Pollakis G, Rambaut A, Hewson R, García-Dorival I, Bore JA, Koundouno R, et al. Temporal and spatial analysis of the 2014–2015 Ebola virus outbreak in West Africa. Nature. 2015;524:97–101. doi: 10.1038/nature14594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cote M, Misasi J, Ren T, Bruchez A, Lee K, Filone CM, Hensley L, Li Q, Ory D, Chandran K, et al. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature. 2011;477:344–348. doi: 10.1038/nature10380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey RA, Zuo Y, Cunningham JM. Identification of a receptor-binding pocket on the envelope protein of friend murine leukemia virus. J Virol. 1999;73:3758–3763. doi: 10.1128/jvi.73.5.3758-3763.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl WE, Lin AE, Grubaugh ND, Carvalho LM, Kim K, Kyawe PP, McCauley SM, Donnard E, Kucukural A, McDonel P, et al. Ebola Virus Glycoprotein with Increased Infectivity Dominated the 2013–2016 Epidemic. Cell. 2016;167:1088–1098.e1086. doi: 10.1016/j.cell.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietzel E, Schudt G, Krähling V, Matrosovich M, Becker S. Functional characterization of adaptive mutations during the West African Ebola virus outbreak. J Virol. 2016 doi: 10.1128/JVI.01913-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckert DM, Kim PS. Mechanisms of viral membrane fusion and its inhibition. Annu Rev Biochem. 2001;70:777–810. doi: 10.1146/annurev.biochem.70.1.777. [DOI] [PubMed] [Google Scholar]
- Faye O, Andronico A, Salje H, Boëlle PY, Magassouba N, Bah EI, Koivogui L, Diallo B, Diallo AA, Keita S, et al. Use of Viremia to Evaluate the Baseline Case Fatality Ratio of Ebola Virus Disease and Inform Treatment Studies: A Retrospective Cohort Study. PLoS Med. 2015;12:e1001908. doi: 10.1371/journal.pmed.1001908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gire SK, Goba A, Andersen KG, Sealfon RS, Park DJ, Kanneh L, Jalloh S, Momoh M, Fullah M, Dudas G, et al. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science. 2014;345:1369–1372. doi: 10.1126/science.1259657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong X, Qian H, Zhou X, Wu J, Wan T, Cao P, Huang W, Zhao X, Wang X, Wang P, et al. Structural Insights into the Niemann-Pick C1 (NPC1)-Mediated Cholesterol Transfer and Ebola Infection. Cell. 2016;165:1467–1478. doi: 10.1016/j.cell.2016.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory SM, Larsson P, Nelson EA, Kasson PM, White JM, Tamm LK. Ebolavirus entry requires a compact hydrophobic fist at the tip of the fusion loop. J Virol. 2014;88:6636–6649. doi: 10.1128/JVI.00396-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison SC. Viral membrane fusion. Nat Struct Mol Biol. 2008;15:690–698. doi: 10.1038/nsmb.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann-Winkler H, Gnirß K, Wrensch F, Pöhlmann S. Comparative Analysis of Host Cell Entry of Ebola Virus From Sierra Leone, 2014, and Zaire, 1976. J Infect Dis. 2015;212(Suppl 2):S172–180. doi: 10.1093/infdis/jiv101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EC, Dudas G, Rambaut A, Andersen KG. The evolution of Ebola virus: Insights from the 2013–2016 epidemic. Nature. 2016;538:193–200. doi: 10.1038/nature19790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito H, Watanabe S, Sanchez A, Whitt MA, Kawaoka Y. Mutational analysis of the putative fusion domain of Ebola virus glycoprotein. J Virol. 1999;73:8907–8912. doi: 10.1128/jvi.73.10.8907-8912.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladner JT, Wiley MR, Mate S, Dudas G, Prieto K, Lovett S, Nagle ER, Beitzel B, Gilbert ML, Fakoli L, et al. Evolution and Spread of Ebola Virus in Liberia, 2014–2015. Cell Host Microbe. 2015;18:659–669. doi: 10.1016/j.chom.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JE, Fusco ML, Hessell AJ, Oswald WB, Burton DR, Saphire EO. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature. 2008;454:177–182. doi: 10.1038/nature07082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K, Ren T, Côté M, Gholamreza B, Misasi J, Bruchez A, Cunningham J. Inhibition of Ebola Virus Infection: Identification of Niemann-Pick C1 as the Target by Optimization of a Chemical Probe. ACS Med Chem Lett. 2013;4:239–243. doi: 10.1021/ml300370k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Johnson JC, Honko A, Yen B, Shabman RS, Hensley LE, Olinger GG, Basler CF. Ebola virus exploits a monocyte differentiation program to promote its entry. J Virol. 2013;87:3801–3814. doi: 10.1128/JVI.02695-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruyama T, Rodriguez LL, Jahrling PB, Sanchez A, Khan AS, Nichol ST, Peters CJ, Parren PW, Burton DR. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol. 1999;73:6024–6030. doi: 10.1128/jvi.73.7.6024-6030.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millard EE, Srivastava K, Traub LM, Schaffer JE, Ory DS. Niemann-pick type C1 (NPC1) overexpression alters cellular cholesterol homeostasis. J Biol Chem. 2000;275:38445–38451. doi: 10.1074/jbc.M003180200. [DOI] [PubMed] [Google Scholar]
- Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, et al. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J. 2012;31:1947–1960. doi: 10.1038/emboj.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misasi J, Gilman MS, Kanekiyo M, Gui M, Cagigi A, Mulangu S, Corti D, Ledgerwood JE, Lanzavecchia A, Cunningham J, et al. Structural and molecular basis for Ebola virus neutralization by protective human antibodies. Science. 2016;351:1343–1346. doi: 10.1126/science.aad6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea TJ, Cryan PM, Cunningham AA, Fooks AR, Hayman DT, Luis AD, Peel AJ, Plowright RK, Wood JL. Bat flight and zoonotic viruses. Emerg Infect Dis. 2014;20:741–745. doi: 10.3201/eid2005.130539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park DJ, Dudas G, Wohl S, Goba A, Whitmer SL, Andersen KG, Sealfon RS, Ladner JT, Kugelman JR, Matranga CB, et al. Ebola Virus Epidemiology, Transmission, and Evolution during Seven Months in Sierra Leone. Cell. 2015;161:1516–1526. doi: 10.1016/j.cell.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quick J, Loman NJ, Duraffour S, Simpson JT, Severi E, Cowley L, Bore JA, Koundouno R, Dudas G, Mikhail A, et al. Real-time, portable genome sequencing for Ebola surveillance. Nature. 2016;530:228–232. doi: 10.1038/nature16996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuit M, Miller DM, Reddick-Elick MS, Wlazlowski CB, Filone CM, Herzog A, Colf LA, Wahl-Jensen V, Hevey M, Noah JW. Differences in the Comparative Stability of Ebola Virus Makona-C05 and Yambuku-Mayinga in Blood. PLoS One. 2016;11:e0148476. doi: 10.1371/journal.pone.0148476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon-Loriere E, Faye O, Koivogui L, Magassouba N, Keita S, Thiberge JM, Diancourt L, Bouchier C, Vandenbogaert M, Caro V, et al. Distinct lineages of Ebola virus in Guinea during the 2014 West African epidemic. Nature. 2015;524:102–104. doi: 10.1038/nature14612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JG, Mothes W, Blacklow SC, Cunningham JM. The mature avian leukosis virus subgroup A envelope glycoprotein is metastable, and refolding induced by the synergistic effects of receptor binding and low pH is coupled to infection. J Virol. 2004;78:1403–1410. doi: 10.1128/JVI.78.3.1403-1410.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smither SJ, Eastaugh L, Ngugi S, O’Brien L, Phelps A, Steward J, Lever MS. Ebola Virus Makona Shows Reduced Lethality in an Immune-deficient Mouse Model. J Infect Dis. 2016;214:S268–S274. doi: 10.1093/infdis/jiw145. [DOI] [PubMed] [Google Scholar]
- Team, W.H.O.E.R. Ebola virus disease in West Africa–the first 9 months of the epidemic and forward projections. N Engl J Med. 2014;371:1481–1495. doi: 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong YG, Shi WF, Liu D, Qian J, Liang L, Bo XC, Liu J, Ren HG, Fan H, Ni M, et al. Genetic diversity and evolutionary dynamics of Ebola virus in Sierra Leone. Nature. 2015;524:93–96. doi: 10.1038/nature14490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanowicz RA, McClure CP, Sakuntabhai A, Sall AA, Kobinger G, Müller MA, Holmes EC, Rey FA, Simon-Loriere E, Ball JK. Human Adaptation of Ebola Virus during the West African Outbreak. Cell. 2016;167:1079–1087.e1075. doi: 10.1016/j.cell.2016.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Shi Y, Song J, Qi J, Lu G, Yan J, Gao GF. Ebola Viral Glycoprotein Bound to Its Endosomal Receptor Niemann-Pick C1. Cell. 2016;164:258–268. doi: 10.1016/j.cell.2015.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissenhorn W, Dessen A, Calder LJ, Harrison SC, Skehel JJ, Wiley DC. Structural basis for membrane fusion by enveloped viruses. Mol Membr Biol. 1999;16:3–9. doi: 10.1080/096876899294706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


