Abstract
Despite having lower levels of education and limited access to health care services, Mexican immigrants report better health outcomes than U.S.-born individuals. Research suggests that the Mexican health advantage may be partially attributable to selective return migration among less healthy migrants—often referred to as “salmon bias.” Our study takes advantage of a rare opportunity to observe the health status of Mexican-origin males as they cross the Mexican border. To assess whether unhealthy migrants are disproportionately represented among those who return, we use data from two California-based studies: the California Health Interview Survey; and the Migrante Study, a survey that samples Mexican migrants entering and leaving the United States through Tijuana. We pool these data sources to look for evidence of health-related return migration. Results provide mixed support for salmon bias. Although migrants who report health limitations and frequent stress are more likely to return, we find little evidence that chronic conditions and self-reported health are associated with higher probabilities of return. Results also provide some indication that limited health care access increases the likelihood of return among the least healthy. This study provides new theoretical considerations of return migration and further elucidates the relationship between health and migration decisions.
Keywords: Migrant Health, Health Selection, Return Migration, Deportation, Mexican Migrants
Introduction
A great deal of research has examined health differences between Mexican immigrant and native-born populations in the United States. Despite having lower levels of education and limited access to health care services, Mexicans exhibit a paradoxical health advantage compared with native-born whites and blacks (Kimbro et al. 2008; Morales et al. 2002; Sorlie et al. 1995). Scholars have hypothesized that this pattern is partly attributable to return migration among those who are less healthy (e.g., Abraido-Lanza et al. 1999; Palloni and Arias 2004). Direct assessments of health-related return migration, however, remain theoretically and empirically underexplored.
We look for evidence of health-related return migration, commonly referred to as “salmon bias,” by drawing on a combination of data sources. The first is a California-based study that includes Mexican-born respondents who migrated to the United States. The second data source is broadly representative of Mexican immigrants who are voluntarily returning to Mexico as well as those who have been deported by U.S. authorities—the vast majority of whom resided in California prior to departure. Pooling these two data sets provides an opportunity to test whether unhealthy immigrants are disproportionately represented among those returning to Mexico.
Our study has three goals. First, we look for evidence of health-related return migration among Mexican males. This comparison allows us to directly observe the health of migrants who stay in the United States and the health of those who return to Mexico at the exact moment of transit. We separately compare the health of Mexican-born men leaving the United States —via deportation and voluntary return migration—with the health of those who remain. The ability to distinguish between voluntary and involuntary return migrant flows offers a rich assessment of these unique health profiles, which is typically overlooked in prior studies of health selection. We then ask whether migrants’ health status is associated with return migration. Here we adjust for factors that are likely associated with both health and the probability of return—including age, socioeconomic status (SES), and acculturation-related indicators. We conclude by investigating whether access to medical services in the United States is modifying patterns of voluntary health-related return migration. Because the data used in this study coincide with the recent adoption of universal health insurance coverage in Mexico (e.g., Knaul et al. 2012), we suspect that salmon bias will be magnified among those migrants without access to U.S. health care.
Answering these questions allows us to effectively assess health selection and also sheds light on the sociodemographic characteristics and well-being of voluntary and involuntary return migrants—two vulnerable populations that are difficult to capture with traditional methods of data collection. By examining variation between distinct migrant flows, we offer a more complete understanding of population health disparities that span the U.S.-Mexico border.
Theoretical Background
Migrant Selection
Foreign-born Hispanics who reside in the United States report lower rates of smoking and alcohol use (Abraido-Lanza et al. 2005; Buttenheim et al. 2010), are less likely to be overweight (Hao and Kim 2009; Jasso et al. 2004; Rubalcava et al. 2008), experience lower rates of all-cause mortality (Abraido-Lanza et al. 1999; Hummer et al. 2004), consume more fruits and vegetables (Akresh 2007; Lara et al. 2005), and appear to have better self-rated health (Acevedo-Garcia et al. 2010; Bostean 2013) than their native-born counterparts. This health advantage has been markedly observed among infants (Hummer et al. 2007; Powers 2013), older age groups (Elo et al. 2004; Lariscy et al. 2015), and Mexican-origin populations (Hummer et al. 2000; Palloni and Arias 2004). Given the relatively disadvantaged SES profile of Hispanic immigrants, these health patterns are largely considered paradoxical.
A number of explanations support the so-called Hispanic paradox, including data misreporting (Dechter and Preston 1991; Rosenberg et al. 1999), protective cultural factors among migrant populations (Hummer et al. 1999; Scribner 1996), and selective migration flows (Crimmins et al. 2005; Palloni and Morenoff 2001; Turra and Elo 2008; Ullmann et al. 2011). Theories of selection, suggesting that migrants systematically differ from nonmigrants in both sending and receiving areas, have received substantial attention in health and mortality literature.
The healthy migrant hypothesis posits that immigrants exhibit better health than those who remain in their country of origin. Some researchers have argued that formal health screenings are part of the selection process (Chiswick et al. 2008), whereas others have stressed that the physical and mental demands of migration prevent less-healthy individuals from relocating (Lu and Qin 2014). Because households initiate migration decisions to maximize economic success and reduce risk (e.g., Stark and Bloom 1985), more-capable (healthy) individuals are presumably more likely to migrate. As such, mortality and morbidity comparisons of immigrants and nonmigrants will be downwardly biased because the former are a highly selected population.
The salmon bias hypothesis posits that the apparent Hispanic health advantage arises from selective return migration when those who are comparably less healthy return to their country of origin (Abraído-Lanza et al. 1999). This phenomenon may result from a distinctive migration flow in which migrants return to their sending country upon falling ill—possibly to reside with family members or obtain health services. Salmon bias may also be indirectly induced when factors associated with success in the receiving society, such as occupational status or family formation, are linked to return migration and health. For instance, salmon bias will occur if less-successful migrants, who also happen to be less healthy, subsequently engage in return migration.
Extant work suggests that migrants may return to seek medical care or family support (Ceballos 2011; Van Hook and Zhang 2011), although empirical support for either account is lacking. Nevertheless, scholars have argued that return migration is most likely to occur among Hispanic populations, mainly Mexicans, because of the proximity of Mexico and other Latin American countries (Macias and Morales 2001; Wallace et al. 2009).1 If less-healthy migrants leave the United States in nontrivial numbers, mortality and morbidity estimates for those who remain will also be downwardly biased. In the sections that follow, we review the evidence supporting claims of migrant selection—with an explicit focus on salmon bias—and highlight the conceptual and empirical limitations of current scholarship.
The Evidence for Salmon Bias
Scholars investigating the mortality advantage among Hispanic immigrants have found evidence for both the healthy migrant and salmon bias hypothesis, although some have argued that the effects of salmon bias are more influential (e.g., Markides and Eschbach 2005). More specifically, the mortality slope for foreign-born Mexicans is less steep compared with other foreign-born Hispanics at older ages, which is consistent with patterns of selective return migration (Palloni and Arias 2004). Drawing on U.S. Social Security data, Turra and Elo (2008) reported that foreign-born Hispanics who return to their country of origin experience higher mortality rates than their counterparts who remain in the United States. However, the authors cautioned that these mortality differentials supporting salmon bias are not large enough to solely explain the Hispanic mortality advantage. In the context of maternal and infant health, Hummer and colleagues (2007) found that rates of infant mortality during the first week of life are lower for offspring born to Mexican-origin mothers than those born to natives. Because mothers and their newborns are unlikely to out-migrate, the authors argued that these results cannot be adequately reconciled with salmon bias.
Extant work has also documented that Mexican return migrants are significantly more likely to report poor global and mental health, chronic conditions, hypertension, and heart disease as well as higher rates of obesity and smoking than Mexican immigrants who remain in the United States (Arenas et al. 2015; Bostean 2013). Although substantial contributions emerged from recent scholarship on salmon bias, the factors that could be driving return migration remain unclear.
Potential Mechanisms of Return Migration
Several processes may explain why migrants in comparably poor health are more likely to voluntarily return to their country of origin. We highlight three processes that may be driving patterns of health-related return migration: medical returns, diminished labor supply/earnings, and preferences for family reunification. These explanations are discussed in the broader health literature, but they have yet to be integrated in the framework of migrant selection. We now consider the patterns and the conditions under which medical returns, diminished labor supply, and family reunification are most likely to occur.
Medical Returns
Mexican immigrants living in the United States are less likely to visit a physician than native-born Mexicans or whites (Ortega et al. 2007). In fact, nearly one-half million Mexican-origin individuals living in California cross into Mexico to receive medical care (Horton and Cole 2011). Among this migrant population, undocumented persons face the greatest barriers to receiving medical care (Bustamante et al. 2012; Goldman et al. 2005; Ku and Matani 2001), making them especially likely to seek health facilities elsewhere. Although some may obtain medical services outside the United States due to lack of insurance (Landeck and Garza 2003; LeClere et al. 1994), cost of care (Herrick 2007; Warner 1991), or language barriers (Flores 2006), others may have preferences for Mexican care. Migrants are thus likely to engage in medical returns upon becoming ill in the host society (Bastida et al. 2008; Fong 2008; Wallace et al. 2009). Given the recent adoption of universal health coverage in Mexico, medical returns may be an increasingly relevant mechanism of return in the current period (Arenas et al. 2015; Knaul et al. 2012). In the event that U.S. health care is unaffordable or undesirable, we may expect selection to be driven—or magnified—by those seeking medical attention in their country of origin.
Employment Incentives
The manifestation of chronic conditions, such as hypertension or work-related injuries, limits the number of hours that one is able to work (Chirikos and Nestel 1985; Smith 1999). In the event that less-healthy migrants experience unemployment (or are unable to find work), the economic incentives for remaining in the United States are likely to decline. As such, they may engage in return migration to find alternate sources of employment or income in their country of origin.
Family Reunification
Family reunification could also be a significant driver of return migration with direct links to health. Some researchers have posited that unhealthy migrants are more likely to return to their country of origin to reunite with relatives and friends (e.g., Abraido-Lanza et al. 1999). These migrants may be seeking a source of inexpensive care or may desire the company of loved ones during a difficult period.
The Role of Deportation
The preceding explanations speak only to voluntary return migration. Migrants who are forcibly removed from the United States—that is, involuntary return migration—are inherently not returning to their country of origin for health care purposes, employment incentives, or even preferences for family reunification.
Theories of migration selection—including the healthy migrant and salmon bias hypotheses—implicitly focus on voluntary return. As a consequence, other forms of population movement, such as deportation, are overlooked. This glaring omission is especially problematic given the rapid and steep rise of deportations. In 2005, U.S. immigration officials forcibly removed nearly 208,100 individuals, 70 % of whom were of Mexican-origin (Dougherty et al. 2006). Reports indicated that this number more than doubled, to reach 438,421 removals in 2013; Mexicans continued to account for upward of 70 % of deportees, with males being dramatically overrepresented (Dreby 2015; Simanski 2014).
Given these skyrocketing deportation rates, it is reasonable to suspect that deportation is influencing health differences across migrant flows. On the one hand, we may observe a more diverse pool of returnees if deportation reduces the pressure of self-selection. On the other hand, deportations could exacerbate salmon bias if migrants in poorer health are more likely to experience forcible removal. This latter possibility would occur, for instance, if those who are ultimately deported have limited access to health and social resources. Poorer health among deported migrants than among voluntary return migrants would suggest that deportation is a nontrivial contributor to the Hispanic health advantage in the United States.
Study Design: Limitations and Considerations
Many studies that investigated migrant selection in the form of salmon bias faced a number of data and conceptual issues that limit conclusions regarding whether and how health can influence return migration. A primary limitation in existing surveys is the long duration—and potential disconnect—between sampling return migrants and measuring their health status. More specifically, migrants who are captured by retrospective surveys are questioned well after they made the return trip to Mexico. Because the circumstances and consequences of return likely affect subsequent health, such an approach will misstate the extent to which salmon bias occurs.
A more refined test would measure migrants’ health when the decision to return was finalized by the migrant or a designated government official and draw comparisons with migrants who remain in the United States during the same period. In the absence of a single data source that simultaneously samples return migrants and those who stay, an alternative approach would pool data from two sources: one containing respondents who remain in the United States, and the other comprising a flow of return migrants.
For such an approach to be successful, a number of conditions and assumptions must be met. First, the data must be representative: that is, the sample of return migrants and the sample of stayers must adequately represent their respective population. This approach also requires that both surveys contain overlapping measures. In other words, identical (or near identical) question and answer categories must be present across data sets to draw effective comparisons. As such, one must strategically choose samples for detailed and overlapping health information. Finally, one must assume that the composition of movers and stayers is relatively stable over the period of investigation. Although this assumption cannot be directly tested, one can reduce concerns of compositional shifts by ensuring that data sources were collected during the same period as well as accounting for differences in age and duration of stay among respondents.
Existing work has also devoted comparably little consideration to the mechanisms that may be driving voluntary return migration. Directly assessing potential modifiers of the relationship between health and return could not only strengthen evidence of salmon bias but could also help elucidate the conditions under which return migration occurs. In the absence of available data that asks respondents to state their reason(s) for return, factors that drive this migration flow can be approximated by using theoretically informed indicators that likely moderate the association between health status and return, such as health care access and availability. Given the policy relevance of health care inaccessibility among such vulnerable populations in the United States, we argue that focusing on medical returns is of particular importance.
Study Objectives
We begin by simply asking whether Mexican-born males who return to their country of origin are less healthy than those who remain in the United States. Because salmon bias does not imply that poor health necessarily leads to return migration, we also examine adjusted correlations to test whether health predicts the probability of voluntary and involuntary return to Mexico. In addition to relying on a global measure of health status, we also draw on indicators of chronic conditions and mental health to capture multiple dimensions of well-being. We conclude by testing whether medical returns are a significant modifier of health-related return migration. To answer these questions, we jointly analyze data from two surveys that represent Mexican-origin adults who returned to Mexico at a primary border crossing point in California and those who were living in California during a nearly contemporaneous period.
Data and Measures
Data used in this study come from (1) the Migrante Project, a health survey administered to Mexican migrants at the Tijuana border in 2013; and (2) the California Health Interview Survey (CHIS), a cross-sectional population-based survey of California residents in 2011–2012. We restrict our analyses to Mexican-born males, which is a decision detailed in our analytic approach.
Migrante Project
The Migrante Project comprises a series of cross-sectional surveys administered to Mexican migrants traveling through the Tijuana-San Diego border region. Migrante was designed with collaboration from the University of Wisconsin-Madison, the Center for Behavioral Epidemiology and Community Health at San Diego State University, the Colegio de la Frontera Norte, and the Mexico Section of the United States-Mexico Border Health Commission in Tijuana, Mexico.
A multistage, multisite sampling strategy was modeled after the Encuesta sobre Migración en la Frontera Norte de México (EMIF)—a large and well-established survey of Mexican migrants—to ensure that data are representative of migrants crossing the Tijuana-San Diego border. The Tijuana-San Diego area concentrated approximately 40 % of the Mexican migrant flow in 2013, making this a major gateway of return. Data were collected from Mexican-born adults who represent four distinct migrant flows: (1) those returning to Mexico from the United States, (2) migrants traveling north (into the United States or into Tijuana) from Mexican regions, (3) individuals leaving the Tijuana area (to the United States or other parts of Mexico) after a stay in the border region, and (4) unauthorized migrants arriving to Tijuana as a result of deportation or forced removal from the United States by immigration authorities. Respondents were sampled in primary venues of border crossing, including the Tijuana International Airport, bus stations, and the San Ysidro deportation facility in Tijuana. For additional information on Migrante, including data collection and sampling procedures, see Amuedo-Dorantes et al. (2013) and Martinez-Donate et al. (2015).
For this study, we focus on deportees and return migrants (flows 1 and 4) in the Migrante data. Deportees (N = 446) are individuals who have been deported, removed, or repatriated by U.S. immigration authorities. Return migration (N = 695) is considered voluntary if respondents report living in the United States for longer than 30 days and are returning to Mexico on their own accord. Subject to these conditions, voluntary returners consist of all return migrants who were not deported. The overall response rate for the study was 57.9 % for all four flows combined. Approximately 97 % of deportees and 57 % of voluntary return migrants participated.2 Detailed information pertaining to migration history, sociodemographic characteristics, and health and health care usage are collected, making these data ideal for our analyses. Most importantly, Migrante provides insight into migrants’ health status the moment they cross the U.S.-Mexico border. In this way, health measured during this period is unlikely to be correlated with the consequences following relocation. For information on migrant “stayers,” we turn to a representative sample of California residents.
California Health Interview Survey (CHIS), 2011–2012
The CHIS is a telephone survey conducted by the University of California Los Angeles Center for Health Policy Research, the California Department of Public Health, and the Department of Health Care Services to represent noninstitutionalized residents of California. The CHIS uses a multistage probability sampling design based on geographic sampling strata to obtain a representative sample of residents during a two-year period (Cervantes et al. 2014). In 2011, CHIS drew approximately 78 % of its sample from a landline sampling frame and 22 % from a cellular service-sampling frame that included all cellphones used by adults for nonbusiness functions. The inclusion of cellphone-only respondents ensures that comparably disadvantaged populations are represented in these data (e.g., Blumberg et al. 2006), which is crucial for our purposes. For the interviews, one adult per household was randomly selected.
Data were collected using computer-assisted telephone interviews, which were conducted in Spanish as needed. The CHIS achieved similar response rates to other California surveys, including the California Behavioral Risk Factor Surveillance System (BRFSS).3 Similar to the Migrante survey, CHIS contains detailed information pertaining to health care, sociodemographic characteristics, health-related behaviors, and chronic conditions.
To create an appropriate comparison group for the Migrante study, we select a subsample that represents Mexican-origin migrants residing in California (N = 4,372), collected from 2011 to 2012.4 The CHIS is a strong compliment to the Migrante data, particularly because 90 % of return and deported migrants sampled by the Migrante study lived in California. In combination, these two data sources provide the opportunity to directly test health-related return migration.
Measures
Our primary interest is whether male migrants in poorer health are more likely to return to Mexico. Using the Migrante data, we create two dichotomous indicators: whether respondents voluntarily return to Mexico, and whether they experience deportation. From the CHIS, we create our reference group for both outcomes: Mexican-born men who remain in the United States.
Health Status
Our main predictor is health status, which we specify in a number of different ways. We follow past work on health disparities more broadly and rely on a global measure of self-reported health. In both questionnaires, respondents are asked, “Would you say that in general your health is excellent, very good, good, fair, or poor?”
We supplement this measure of general health status with reports of health limitations in the past 12 months and separate indicators for having ever being diagnosed with any of the following chronic conditions: diabetes, hypertension, heart disease, asthma, or arthritis. We also include a measure of whether the respondent is obese (BMI ≥ 30) as a broad indicator of physical fitness. Three items representing mental health and well-being are also assessed: the frequency to which respondents felt discouraged or sad, had a lot of energy, and felt stressed in the past four weeks. Respondents were assigned a value of 1 if they reported such feelings “all of the time” or “most of the time” (versus “sometimes,” “a few times,” or “never”).
Sociodemographic Characteristics
In subsequent analyses, we adjust for sociodemographic characteristics that are likely correlated with both return migration and health, including the respondent’s age at the time of survey, whether the respondent resides in an urban area, whether the respondent has children, and whether he is married or living with a romantic partner. Educational attainment is specified using four categories: junior high or less, some high school, high school completion or vocational school, and some college or more. Given the comparably lower educational distribution in Mexico (e.g., Chiquiar and Hanson 2005), this categorization more accurately reflects educational distinctions among Mexican-born persons.
We assign a value of 1 to respondents who report being a permanent resident or undocumented (versus being a naturalized citizen). We also include a measure of whether the respondent speaks at least some English at home. Finally, four categories are used to represent duration of stay (<2 years, 2–4 years, 5–9 years, or 10+ years). Together, these three measures can be thought of as proxies for exposure to U.S. society.5
Health Care
To test whether limited access to health care is contributing to patterns of return migration (e.g., medical returns), we use two dichotomous measures that likely moderate the association between health and migration: whether the respondent had U.S. health insurance, or whether the respondent received any medical care in the United States during past 12 months.
Analytic Approach
We begin by estimating an unadjusted association to assess whether migrants who return to Mexico are less healthy than migrants who stay in the United States. Because we suspect that the selection process differs among voluntary and deported migrants, we also conduct separate analyses for these two return flows—comparing them with migrants who remain in the United States. Together, these results will serve as a direct test of the salmon bias hypothesis.
We then ask a closely related, but distinct question: whether health is correlated with the probability of return. Here, we run a series of logistic regressions to predict whether one’s health status is associated with returning to Mexico after adjusting for confounding factors that likely influence health as well as the probability of return. Again, we have the ability to conduct separate analyses for voluntary and deported samples—comparing them with Mexican immigrants who live in California (stayers). The inclusion of the deported sample helps sheds light on whether involuntary return exacerbates or mitigates processes of health selection. In additional analyses, we investigate whether specific dimensions of health—such as mental health and chronic conditions—are associated with the probability of return.
We conclude by testing whether health insurance coverage or having received medical care moderate processes of voluntary return. If access to health-related services is partially responsible for driving patterns of salmon bias, less-healthy migrants with limited U.S. health care access should be most likely to return to Mexico. However, if we find that return is not influenced by access to health care, perhaps other factors—such as employment or family reunification—play a greater role in return migration.
Analyses are restricted to Mexican-born males (N = 2,653) for two reasons. First, a long line of work has argued that gender influences migration decisions as well as the migration experience itself (e.g., Espiritu 1999; Menjívar 1999). In the context of this study, we expect that health as well as migration decisions may systematically vary between men and women.6 Second, U.S. deportation efforts and enforcement policies disproportionally target men. Although 57 % of all undocumented migrants are men, they account for approximately 93 % of the detained population (Kohli et al. 2011). In this way, the current deportation regime is one that is highly gendered and male-centered (e.g., Golash-Boza and Hondagneu-Sotelo 2013). Given the gender imbalance in our data—particularly among deportees in the Migrante sample—we are confident that our results best speak to return migration among Mexican-born males.7
We use multiple imputation with chained equations to impute missing items when participants in either data set do not respond to a questionnaire item. Approximately 5 % of all cases are missing in the Migrante samples; language spoken in the home and health insurance indicators are responsible for the majority of missing values. For the CHIS, less than 2 % of total cases are missing from our analytic sample, with most missing values stemming from items pertaining to medical visits and care. Given our combination of data sources, a series of 25 imputations are run separately for each migrant flow.
Results
Descriptive Statistics
Table 1 describes returners, deportees, and stayers from the Migrante and CHIS data. Mexican-born persons who remain in the United States report worse health, more chronic conditions, and higher rates of health care usage than voluntary return migrants or those who were deported. Approximately 26 % of stayers report having excellent or very good health compared with approximately 44 % of voluntary and 49 % of deportees. A higher percentage of stayers have been diagnosed with diabetes (15 % vs. 8 %, 5 %), heart disease (6 % vs. 1 %, 0.5 %), and hypertension (19 % vs. 12 %, 5 %); similar patterns also exist for asthma and arthritis. Slightly more voluntary return migrants and stayers report having a health limitation (approximately 16 %) than deportees (12.8 %). Obesity is comparably lower among the deported sample (21 %) than among voluntary return migrants (31 %) or stayers (35 %).
Table 1.
Descriptive statistics by migrant flow
| Migrante Data | CHIS Data | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Return Flow (N = 511) |
Deported (N = 404) |
Stayers (N = 1,739) |
||||
|
|
||||||
| Mean or % |
SD | Mean or % | SD | Mean or % |
SD | |
| Health Indicators | ||||||
| Self-reported health | ||||||
| Excellent | 25.35 | 31.33 | 13.08 | |||
| Very good | 18.16 | 17.54 | 13.31 | |||
| Good | 30.34 | 30.33 | 36.92 | |||
| Fair | 23.55 | 19.55 | 31.39 | |||
| Poor | 2.59 | 1.25 | 5.30 | |||
| Any health limitations | 16.17 | 12.78 | 16.58 | |||
| In the past 4 weeks: | ||||||
| Had energy all/most of the time | 73.65 | 69.17 | 75.97 | |||
| Felt sad all/most of the time | 5.59 | 13.03 | 3.51 | |||
| Felt stressed all/most of time | 12.77 | 20.10 | 6.34 | |||
| Obese | 30.53 | 21.79 | 35.02 | |||
| BMI | 28.60 | 4.5 | 27.26 | 8.5 | 29.33 | 6.7 |
| Diagnosis | ||||||
| Diabetes | 8.47 | 5.05 | 15.31 | |||
| Hypertension | 12.15 | 4.77 | 19.40 | |||
| Heart disease | 1.21 | 0.51 | 6.00 | |||
| Asthma | 1.01 | 0.76 | 4.83 | |||
| Arthritis | 1.21 | 1.26 | 12.03 | |||
| Demographics | ||||||
| Age | 44.14 | 14.1 | 34.59 | 10.2 | 46.93 | 14.6 |
| Lives in urban area | 85.94 | 87.89 | 83.50 | |||
| Married/cohabiting with partner | 66.73 | 48.76 | 73.49 | |||
| Has children | 80.83 | 72.25 | 48.36 | |||
| Highest level of education | ||||||
| Junior high or less | 60.67 | 66.58 | 40.20 | |||
| Some high school | 5.68 | 12.87 | 13.11 | |||
| High school | 16.05 | 16.09 | 24.55 | |||
| Some college+ | 17.61 | 4.46 | 22.14 | |||
| Speaks some English at home | 17.62 | 24.92 | 54.24 | |||
| Duration of latest U.S. stay | ||||||
| <2 years | 24.85 | 21.98 | 0.29 | |||
| 2–4 years | 6.51 | 14.21 | 2.47 | |||
| 5–9 years | 8.09 | 15.28 | 6.84 | |||
| 10+ years | 60.55 | 48.53 | 90.40 | |||
| Noncitizen | 53.97 | 100.00 | 59.98 | |||
| Health Services | ||||||
| Any care in past 12 months | 48.90 | 47.61 | 66.76 | |||
| Has usual source of care | 32.58 | 33.24 | 67.91 | |||
| Place of usual care | ||||||
| Doctor’s office | 11.98 | 8.58 | 31.97 | |||
| Clinic | 38.84 | 28.69 | 35.19 | |||
| ER | 0.00 | 0.27 | 1.15 | |||
| Other | 2.48 | 16.89 | 0.75 | |||
| No place of care | 46.69 | 45.58 | 30.94 | |||
| Number of doctor’s visits in past 12 months | ||||||
| 0 | 73.30 | 97.76 | 33.24 | |||
| 1 | 9.71 | 0.45 | 20.64 | |||
| 2–3 | 11.41 | 1.35 | 22.71 | |||
| 4+ | 5.58 | 0.45 | 23.40 | |||
| ER visit in past 12 months | 4.81 | 7.79 | 12.22 | |||
| Health insurance in past 12 months | 46.23 | 21.17 | 66.47 | |||
| Type of insurance | ||||||
| Medicare/Medicaid/Public | 16.87 | 7.02 | 31.40 | |||
| Private insurance | 20.37 | 5.90 | 32.32 | |||
| Other | 7.20 | 7.02 | 0.00 | |||
| Uninsured | 55.56 | 80.06 | 36.29 | |||
Deported migrants exhibit lower levels of mental health and well-being than return migrants or stayers. Specifically, more than 20 % of deportees report feeling stressed all/most of the time, compared with 13 % of voluntary return migrants and 6 % of stayers. A higher percentage of deported migrants also report feelings of sadness and discouragement during the past four weeks. Fewer deportees report having energy all or most of the time (69 %) compared with both return migrants (74 %) and stayers (76 %). We suspect, however, that the event of deportation itself is largely responsible for driving mental health burdens among this group of returners.
Striking differences in health care access and usage also emerge. A greater percentage of Mexican men who remain in the United States have regular access to health care and insurance. Approximately 67 % received U.S. medical care during the past 12 months (vs. 49 % and 48 % of return and deported migrants, respectively). A higher percentage of stayers also have a usual source of care, receive this care in a doctor’s office, and are currently insured.8 As a whole, deported migrants appear particularly vulnerable with respect to limited health care access and usage.
Some sociodemographic differences are also worth mentioning. Stayers report higher levels of education and are more likely to speak English at home than voluntary or involuntary migrants. Compared with deportees—who are undocumented—nearly 54 % and 60 % of returnees and stayers, respectively, are not U.S. citizens. Deported migrants tend to be younger and are less likely to be married/cohabiting than either voluntary return migrants or stayers. Perhaps most shockingly, a number of deportees have substantial U.S. experience: nearly 49 % of those who were deported lived in the United States for 10 years or more.
Assessing Health Selection
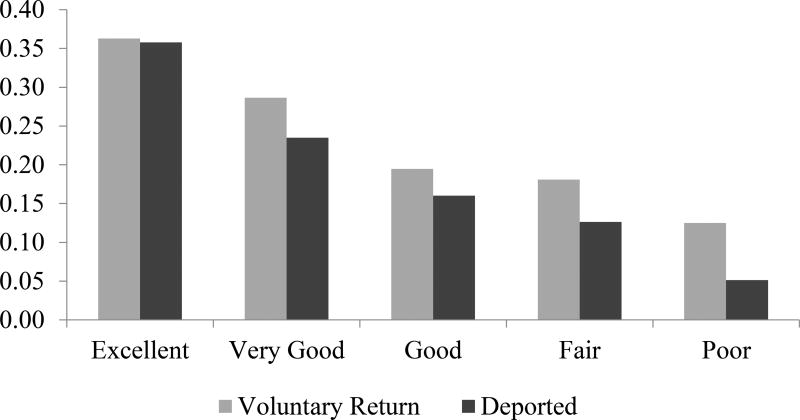
Table 2, panel A, contains results from three separate logistic regressions that assess the relationship between self-reported health and return migration. Estimates indicate that return migrants who report being in worse health are less likely to return than their healthier counterparts. More specifically, those who report being in excellent health are more likely to engage in return migration than migrants in poor health by nearly 37 percentage points. 9 In addition, the predicted probability of return steadily declines at each level of self-reported health for all migrants.
Table 2.
Predicting odds of return using migrants’ self-reported health
| All Return Migrants | Voluntary Return | Deported Migrants | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Odds Ratio | SE | Odds Ratio | SE | Odds Ratio | SE | |
| Panel A | ||||||
| Self-reported health (ref. = excellent) | ||||||
| Very good | 0.628** | (0.086) | 0.704* | (0.117) | 0.551** | (0.097) |
| Good | 0.384*** | (0.045) | 0.424*** | (0.061) | 0.342*** | (0.051) |
| Fair | 0.324*** | (0.040) | 0.387*** | (0.058) | 0.260*** | (0.043) |
| Poor | 0.175*** | (0.048) | 0.251*** | (0.079) | 0.097*** | (0.046) |
| Constant | 1.127 | (0.103) | 0.570*** | (0.063) | 0.557*** | (0.062) |
| Panel B | ||||||
| Self-reported health (ref. = excellent) | ||||||
| Very good | 0.804 | (0.151) | 0.819 | (0.189) | 0.816 | (0.206) |
| Good | 0.395*** | (0.062) | 0.421*** | (0.081) | 0.337*** | (0.072) |
| Fair | 0.296*** | (0.051) | 0.372*** | (0.077) | 0.241*** | (0.057) |
| Poor | 0.177*** | (0.066) | 0.200*** | (0.088) | 0.166** | (0.100) |
| Age | 0.984** | (0.005) | 1.002 | (0.006) | 0.949*** | (0.007) |
| Married/Cohabiting | 0.188*** | (0.028) | 0.210*** | (0.038) | 0.156*** | (0.031) |
| Has children | 9.950*** | (1.555) | 14.315*** | (2.817) | 8.065*** | (1.742) |
| Lives in urban area | 2.017*** | (0.323) | 1.783** | (0.340) | 2.344*** | (0.553) |
| Level of education (ref. = junior high or less) | ||||||
| Some high school | 0.332*** | (0.061) | 0.214*** | (0.056) | 0.411*** | (0.093) |
| High school | 0.368*** | (0.056) | 0.440*** | (0.082) | 0.247*** | (0.052) |
| Some college or more | 0.299*** | (0.052) | 0.462*** | (0.090) | 0.088*** | (0.028) |
| Duration of time in United States (ref. = 10+ years) | ||||||
| <2 years | 83.584*** | (39.573) | 99.394*** | (50.086) | 82.578*** | (44.200) |
| 2–4 years | 5.119*** | (1.187) | 4.064*** | (1.233) | 6.817*** | (1.888) |
| 5–9 years | 1.888*** | (0.344) | 1.860* | (0.450) | 1.955** | (0.444) |
| Speaks some English in home | 0.259*** | (0.033) | 0.168*** | (0.028) | 0.382*** | (0.069) |
| Noncitizen | 0.820 | (0.109) | 0.369*** | (0.056) | — | — |
| Constant | 1.764 | (0.588) | 0.584 | (0.240) | 3.261** | (1.362) |
Notes: Results in panels A and B are from three separate regression analyses. All return migrants (N = 915), voluntary migrants (N = 511), and deported migrants (N = 404) are compared with migrants who remain in the United States (stayers, N = 1,739). Results presented in panel B adjust for socioeconomic characteristics and exposure to U.S. society.
p < .05;
p < .01;
p < .001
Figure 1 illustrates predicted probabilities of return among voluntary migrants and deported persons, where both flows are compared with stayers. Yet again, we observe that the probability of return is higher for those reporting comparably better health. And despite trivial differences in the probability of return among voluntary and deported migrants in excellent health, voluntary migrants in poorer health are more likely to return than deportees who share their health status, suggesting that the relation between health and deportation is even stronger than that for voluntary returners. Although we find evidence for health-related return migration, it is not in the direction anticipated: healthier Mexican migrants are more likely to return to their country of origin than remain in the United States.
Fig. 1.
Predicted probability of return among voluntary and deported migrants by self-reported health
Does Health Influence Return Migration?
To test whether health independently influences return migration, we include a number of measures that capture sociodemographic characteristics and exposure to U.S. society—factors likely related to both health and return (Table 2, panel B). After we account for such measures, the pattern between self-reported health and the probability of return does not change, although many indicators are significantly associated with the likelihood of return.
Results indicate that individuals with higher levels of education are less likely to leave the United States than those who completed junior high or fewer years of schooling. Respondents who speak English in the home, who are currently married or living with their partner, and who have spent longer periods in the United States are also significantly less likely to return to Mexico. Stronger ties to the host society apparently discourage return, perhaps because the financial and social incentives of retuning to Mexico are comparably small. These patterns hold for voluntary, deported, and all return migrants as a whole. Noncitizens are also less likely to return, which aligns with prior work on migration patterns (e.g., Cornelius 2001). And although having children significantly increases the odds of return, we suspect that the presence of children outside the United States may be driving these migration decisions.
Assessing Chronic Conditions and Mental Health
Thus far, we have observed that Mexican migrants who return to their country of origin exhibit better self-reported health than those remaining in the United States. However, relying on a single indicator of health could be problematic if respondents employ different reference points to assess their well-being (Groot 2000; Jürges 2007; Salomon et al. 2004). As such, we also consider indicators of chronic conditions and mental health.
Results from this set of specifications provide mixed support for salmon bias (Table 3). Migrants have significantly higher odds of voluntarily returning to Mexico—as opposed to staying—if health limits their daily activities. We also observe that migrants who are frequently stressed report two to three times higher odds of voluntary or forced return (panel A). The direction of these correlations is consistent with the salmon bias hypothesis. Contrary to our expectations, however, chronic conditions—including diabetes, hypertension, heart disease, asthma, arthritis, and obesity—are associated with significantly lower odds of return among both voluntary and deported migrants. Assessing diagnoses instead of symptoms presents a potential underestimation of chronic disease burden among those without health care providers—a particularly important issue given that returnees are less likely to receive regular medical care.
Table 3.
Predicting odds of return using migrants’ reports of chronic conditions and mental health
| All Return Migrants | Voluntary Return | Deported Migrants | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | SE | Odds Ratio | SE | Odds Ratio | SE | |
| Panel A | ||||||
| Health limitations | 1.337* | (0.179) | 1.451* | (0.225) | 1.098 | (0.211) |
| Diabetes | 0.619** | (0.104) | 0.676* | (0.131) | 0.556* | (0.145) |
| Hypertension | 0.639** | (0.096) | 0.844 | (0.143) | 0.338*** | (0.090) |
| Heart disease | 0.154*** | (0.061) | 0.200*** | (0.088) | 0.100** | (0.074) |
| Asthma | 0.206*** | (0.079) | 0.220** | (0.104) | 0.181** | (0.110) |
| Arthritis | 0.078*** | (0.026) | 0.077*** | (0.033) | 0.083*** | (0.041) |
| Obesity | 0.773** | (0.075) | 0.934 | (0.109) | 0.564*** | (0.080) |
| Felt stressed all/most of the time | 2.897*** | (0.467) | 2.540*** | (0.517) | 3.589*** | (0.710) |
| Felt sad all/most of the time | 2.204*** | (0.472) | 1.280 | (0.374) | 3.259*** | (0.816) |
| Had energy all/most of the time | 0.933 | (0.097) | 1.000 | (0.126) | 0.925 | (0.130) |
| Constant | 0.671*** | (0.068) | 0.339*** | (0.042) | 0.322*** | (0.043) |
| Panel B | ||||||
| Health limitations | 1.427* | (0.244) | 1.363 | (0.272) | 1.184 | (0.304) |
| Diabetes | 0.643* | (0.140) | 0.618 | (0.157) | 0.871 | (0.289) |
| Hypertension | 0.983 | (0.195) | 0.932 | (0.208) | 0.928 | (0.311) |
| Heart disease | 0.182** | (0.095) | 0.333* | (0.172) | 0.029** | (0.037) |
| Asthma | 0.295** | (0.127) | 0.279* | (0.152) | 0.349 | (0.220) |
| Arthritis | 0.129*** | (0.049) | 0.123*** | (0.056) | 0.194** | (0.111) |
| Obesity | 0.751* | (0.092) | 0.861 | (0.126) | 0.549** | (0.100) |
| Felt stressed all/most of the time | 2.494*** | (0.513) | 2.592*** | (0.696) | 3.336*** | (0.871) |
| Felt sad all/most of the time | 1.826* | (0.478) | 0.770 | (0.287) | 2.978** | (0.940) |
| Had energy all/most of the time | 0.882 | (0.116) | 0.908 | (0.148) | 0.824 | (0.153) |
| Age | 0.984** | (0.005) | 1.005 | (0.006) | 0.944*** | (0.008) |
| Married/Cohabiting | 0.195*** | (0.029) | 0.218*** | (0.040) | 0.158*** | (0.032) |
| Has children | 9.308*** | (1.479) | 13.417*** | (2.690) | 8.050*** | (1.788) |
| Lives in urban area | 1.895*** | (0.306) | 1.786** | (0.345) | 2.046** | (0.489) |
| Level of education (ref. = junior high or less) | ||||||
| Some high school | 0.333*** | (0.062) | 0.213*** | (0.057) | 0.409*** | (0.094) |
| High school | 0.419*** | (0.064) | 0.478*** | (0.090) | 0.298*** | (0.063) |
| Some college or more | 0.374*** | (0.064) | 0.543** | (0.105) | 0.120*** | (0.038) |
| Duration of time in United States (ref. = 10+ years) | ||||||
| <2 years | 81.181*** | (38.500) | 100.202*** | (50.909) | 73.443*** | (39.106) |
| 2–4 years | 4.886*** | (1.148) | 4.157*** | (1.263) | 6.296*** | (1.783) |
| 5–9 years | 1.948*** | (0.362) | 1.957** | (0.482) | 1.916** | (0.448) |
| Speaks some English in home | 0.276*** | (0.035) | 0.183*** | (0.030) | 0.403*** | (0.074) |
| Noncitizen | 0.712* | (0.097) | 0.334*** | (0.052) | — | — |
| Constant | 1.093 | (0.377) | 0.317** | (0.134) | 2.147 | (0.960) |
Notes: Results in panels A and B are from three separate regression analyses. All return migrants (N = 915), voluntary migrants (N = 511), and deported migrants (N = 404) are compared with migrants who remain in the United States (stayers, N = 1,739). Results presented in panel B adjust for socioeconomic characteristics and exposure to U.S. society.
p < .05;
p < .01;
p < .001
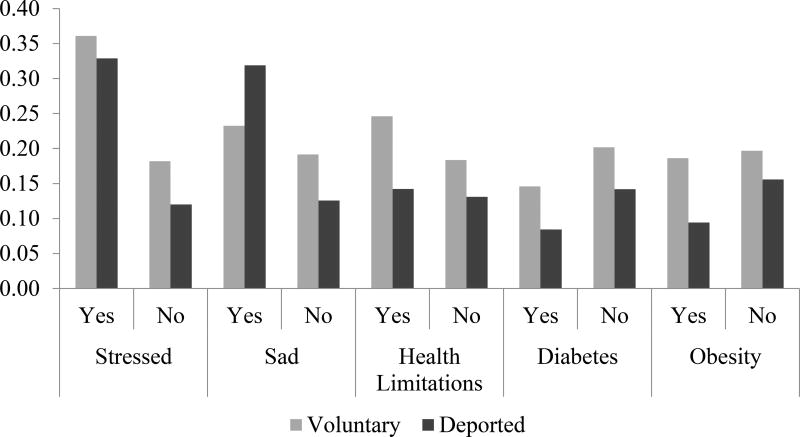
We present selected health indicators in the form of predicted probabilities (Fig. 2) to highlight the magnitude of these differences. Reports of feeling stressed all/most of the time are associated with, respectively, an 18 and 21 percentage point increase in the probability of voluntary return and deportation. Migrants who report feeling sad the majority of the time have a significantly higher predicted probability of deportation—one that is approximately 19 percentage points greater than those who report feeling sad less frequently. However, we believe that the deportation process itself is likely driving many of these mental health disparities. Of final note, the probability of voluntary return is slightly higher for migrants reporting health limitations (6 percentage points), while diabetes and obesity are associated with a lower probability of return, ranging between 5 and 10 percentage points for voluntary and deported migrants, respectively.
Fig. 2.
Predicted probability of return among voluntary and deported migrants by chronic conditions
The association between these health conditions and return remains largely unchanged with the inclusion of sociodemographic measures, suggesting that health conditions appear to independently influence return migration. The one exception is the presence of health limitations, which is no longer precisely estimated with the addition of our covariates. As in our analysis of self-reported health, we find that return migrants tend to be younger; are more likely to have children; and are less likely to be highly educated, married, and speak English in their home. Both voluntary and deported migrants also have significantly less experience in the United States than those who remain.
Overall, our results provide mixed support for salmon bias. On the one hand, we find that health limitations and reports of stress and sadness are associated with an increased probability of return—an expected pattern if less-healthy migrants are indeed engaging in return migration. On the other hand, those with chronic conditions and worse self-reported health are less likely to return to Mexico. Put differently, salmon bias appears to operate for some health conditions and not others, although the overall patterns are similar for voluntary and deported migrants. Results also indicate that health influences the probability of return above and beyond sociodemographic characteristics and exposure to U.S. society.
It is thus possible that salmon bias arises because of a direct link between health and migration decisions. Given the recent expansion of universal health insurance coverage in Mexico (e.g., Knaul et al. 2012), one may anticipate health-related return migration to be influenced by those seeking affordable and immediate medical care.
What Could Be Driving Voluntary Return Migration?
We anticipated that the association between poor health and return migration would be most pronounced among those without health insurance or access to health care. Not only would uninsured migrants in poor health incur additional costs, but incentives for engaging in medical returns are likely to be greater. We assess this possibility using health limitations, which is an indicator consistent with patterns of return migration under salmon bias. Because of concerns that migrants’ reports of stress and sadness could be correlated with the act of migration, we do not include these indicators in our moderation analyses.
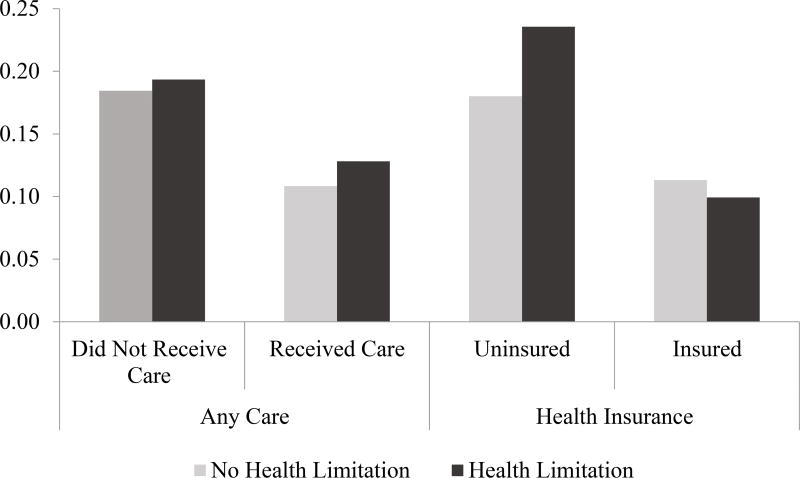
We find some support that a lack of health insurance exacerbates the correlation between poor health and return (Fig. 3). Among individuals who are insured, the predicted probability of return is 1.4 percentage points higher for those without limitations than for those with limitations. For migrants without health insurance coverage in the past year, however, the predicted probability of return is 5.5 percentage points higher for those with health limitations. This provides some evidence that limited health care access exacerbates the association between poor health and return.
Fig. 3.
Predicted probability of return by health care access and health limitations
We also consider whether having received any medical care in the United States modifies the association between health and return migration (Fig. 3). Among migrants who received any kind of medical care in the past year, the predicted probability of return is approximately 2 percentage points higher for those with health limitations than for those who do not report health limitations. For migrants who did not receive care, the difference in the probability of return among those with and without health limitations is practically zero—an unexpected pattern if receipt of care was truly modifying the relationship between health and return. However, results generally suggest that migrants who receive U.S. medical care and who are insured are less likely to return to Mexico than those without health care access.
Discussion
For nearly 30 years, scholars acknowledged patterns of health selection among migrants, especially with respect to the Mexican population. The salmon bias hypothesis, which posits that the apparent Hispanic health advantage is due to return migration among less-healthy migrants, has received an increasing amount of support in the literature (e.g., Arenas et al. 2015; Palloni and Arias 2004; Turra and Elo 2008). We contribute to this growing body of work by pooling data from two California-based studies to look for evidence of health-related return migration among both voluntary return migrants and deportees. We ask whether health influences the probability of return above and beyond migrants’ sociodemographic characteristics and exposure to the U.S. context, and test whether medical returns are a potential driver of health-related return migration.
We find that return migrants report higher levels of stress and health limitations than those who remain in the United States. However, voluntary and deported migrants are less likely to report poorer overall health or chronic conditions, which is contrary to the salmon bias hypothesis. This finding could be an artifact of differential access to health providers between stayers and returnees rather than true differences in health, particularly if those without access to health care are unaware of their conditions. If these findings reflect actual health differences, however, it would suggest that health conditions do not equally influence migrants’ decision to return. These patterns remain after adjusting for socioeconomic characteristics and exposure to U.S. society, indicating that these factors are largely independent of the relation between health status and the probability of return.
The discrepancy between our results and prior studies investigating salmon bias (e.g., Arenas et al. 2015; Bostean 2013) is likely due to the timing at which migrants’ health is measured. Scholars have traditionally assessed the health of return migrants after they returned to Mexico, which reflects migrants’ health prior to departure as well as any changes in health that arose during transit and resettlement. Our study relies on measures of health that are collected the moment migrants cross the U.S.-Mexico border, which help to alleviate such concerns. In addition, our data and results directly speak to patterns of health-related return among Mexican-born males who reside in California. Thus, our population may differ (i.e., be healthier) from those captured via other methods of data collection.
Our findings also suggest that migrants in better physical health are at a higher risk of forced removal, even after conditioning on age and other sociodemographic factors. One explanation could be that deportation selects on other traits that are correlated with better health, such as employment. For instance, jobs that present higher risks of deportation may also be more physically demanding and thus select on health (e.g., certain jobs in agriculture and construction). The better average physical health among deportees relative to stayers or voluntary return migrants suggests that the observed Hispanic health advantage in the United States would be even more pronounced in the absence of forcible removal. Nevertheless, substantial mental health burdens are associated with deportation, including elevated stress and depression. Programs that promote overall well-being in medical centers near the U.S.-Mexico border region may be a partial remedy to this unsettling pattern.
We also find that a substantial number of deportees have resided in the United States for 10 years or longer. Given that migrants’ emotional well-being suffers when social and economic ties are abruptly severed following deportation (Dreby 2015; Hagan et al. 2011), we suspect that mental health consequences will be magnified among those who have remained in the United States for lengthier periods. It is also possible that the composition of deportees has changed because of the increased number of forced removals. In supplementary analyses, we compare sociodemographic characteristics among Mexican-origin men who were returned by U.S. immigration authorities using the 2005 and 2013 EMIF surveys.10 Descriptive results suggest that contemporary deportation flows are more diverse than in the past. Specifically, a greater percentage of recent forced returners report speaking English and earn a level of attainment beyond primary school. Although speculative, it is also possible that a larger share of recent deportees report favorable health conditions, which would indicate that the Hispanic health advantage has waned as the composition of forced returners become increasingly diverse. Much more research is needed to investigate population-level consequences of deportation.
We also find that migrants who have been uninsured in the past year are more likely to engage in medical returns, and that this exacerbates the probability of return among comparably less-healthy migrants. This result is precisely what we had anticipated based on the literature on health care-related return migration (e.g., Wallace et al. 2009). However, these differences in the probability of return were quite modest, particularly when we assessed receipt of care. Although the results are somewhat surprising given Mexico’s shift in health care coverage, two plausible explanations exist. First, salmon bias may operate through other avenues—including migrants’ preferences for family reunification or declining employment incentives—as opposed to medical returns. Second, perhaps more-refined measures of health care access are needed, particularly with respect to quality of care and migrants’ preferences for medical receipt.
Limitations
Despite the rigorous sampling methods used for collecting the CHIS, it is possible that the data are not representative of California’s first-generation Mexican immigrants. Of particular concern is that our analytic sample may overrepresent a certain subset of men, such as those who are less healthy or more likely to have health care access. Although the CHIS made great efforts to representatively include undocumented migrants, estimating the true response rate for this group is difficult. As such, it is possible that the undocumented are underrepresented in this data set compared with the Migrante Study.
Concerns are also warranted that Migrante and CHIS may not be representative of Mexican migrants more generally. To address some of these concerns, we compare the health of the CHIS sample with another population-based survey: the 2011–2012 National Health and Nutrition Examination Survey (NHANES). Overall, the health profiles of male respondents in both samples are quite similar (Table 4). Approximately 26 % of CHIS respondents reported being in excellent or very good health compared with approximately 25.5 % of Mexican-born males sampled in the NHANES. We also observe similar levels of obesity, hypertension, diabetes, and asthma across surveys; the one exception is heart disease, which is significantly higher in the CHIS. Nevertheless, this comparison provides some evidence that the health characteristics of CHIS respondents generally overlap with those found among Mexican immigrants more widely.
Table 4.
Comparing health characteristics across data sources
| CHIS Sample N = 1,739 |
NHANES N = 182 |
Difference t/z test (sig.) |
Migrante N = 868 |
MMP N = 1,353 |
Difference t test (sig.) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Mean (%) |
SD | Mean (%) |
SD | Mean (%) |
SD | Mean (%) |
SD | |||
| Age | 46.93 | 14.61 | 43.67 | 14.98 | 2.84 (**) | — | — | — | — | — |
| Excellent/Very Good Health | 26.38 | 25.52 | 0.23 (ns) | — | — | — | — | — | ||
| Obese | 35.02 | 41.76 | −1.81 (ns) | — | — | — | — | — | ||
| BMI | 29.33 | 6.70 | 28.96 | 4.85 | 0.72 (ns) | — | — | — | — | — |
| Diagnosis | — | — | — | — | — | |||||
| Diabetes | 15.31 | 12.99 | 0.82 (ns) | — | — | — | — | — | ||
| Hypertension | 19.40 | 18.13 | 0.41 (ns) | — | — | — | — | — | ||
| Heart disease | 6.00 | 2.31 | 2.00 (*) | — | — | — | — | — | ||
| Asthma | 4.83 | 7.14 | −1.35 (ns) | — | — | — | — | — | ||
| Arthritis | 12.03 | 7.51 | 1.77 (ns) | — | — | — | — | — | ||
| Height (inches) | — | — | — | — | — | 66.89 | 2.78 | 66.42 | 3.41 | 3.37 (***) |
| Height Percentiles | — | — | — | — | — | |||||
| 25th | — | — | — | — | — | 64.96 | 64.57 | |||
| 50th | — | — | — | — | — | 66.93 | 66.93 | |||
| 75th | — | — | — | — | — | 68.54 | 68.90 | |||
Notes: Data are from the 2011–2012 California Health Interview Survey (CHIS), the Migrante Study, the 2011–2012 National Health and Nutrition Examination Survey (NHANES), and the Mexican Migration Project (MMP). All analyses are restricted to Mexican-born males. A t test of means and z test of proportions are used, with equal variances assumed across samples.
p < .05;
p < .01;
p < .001
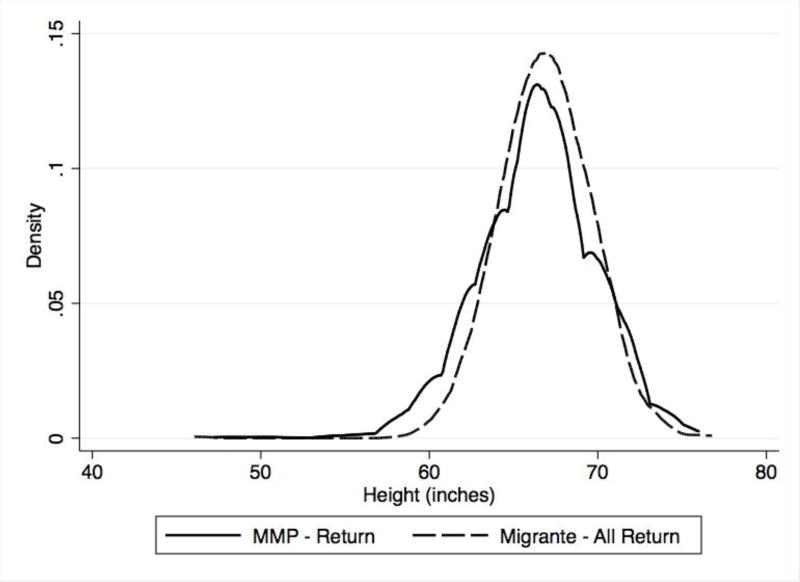
Given similar concerns with the Migrante data, we also draw on return migrants sampled by the Mexican Migrant Project (MMP). To obtain relevant comparisons, we limit analyses to MMP respondents who returned from the United States during the 2013–2014 period. Because differences in health could reflect consequences of return, we focus on a presumably fixed indicator of adult health: height. If we observe that the height distribution overlaps across surveys, it would suggest that respondents sampled in the Migrante study are likely representative of return migrants. A t test indicates significant differences in average height across both surveys: Migrante respondents—particularly voluntary return migrants—tend to be slightly taller than those sampled in the MMP (Table 4). We supplement this approach with kernel density estimates of height for both samples (Fig. 4). Although the majority of the distribution overlaps across samples, a Kolmogorov-Smirnov test indicates the distributions are not equivalent. Clearly, the MMP data are characterized by more variation; we see this at lower and higher values of height (below 65 inches and above 70 inches). Although these differences are noteworthy, little evidence exists to suggest these samples wildly differ in their health characteristics.
Fig. 4.
Height distribution of respondents from Migrante and the Mexican Migration Project
Although we find mixed support for salmon bias, analyses suggest that barriers to health care may increase the probability of return migration. The literature on health selection would benefit from further theoretical development as well as a closer investigation of the health-related mechanisms involved in return migration, including employment incentives and family reunification. Doing so will provide an opportunity to better understand the role of health in migration decisions, and also has significant implications for studying and ameliorating health disparities in the United States.
Acknowledgments
The Migrante study was supported by the National Institutes of Health (NIH) and Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant R01 HD046886; PI: Martinez-Donate). The second author received support from the National Institute on Aging (Grant T32 AG00129), the Center for Demography and Ecology (Grant P2C HD047873), and the Center for Demography of Health and Aging at the University of Wisconsin-Madison (Grant P30 AG017266). An early version of this article was presented at the 2015 Annual Meetings of the Population Association of America. The authors would like to thank Erin Hamilton, Jenna Nobles, and Alberto Palloni for helpful comments on earlier drafts. Authors are solely responsible for all content.
Footnotes
The salmon bias hypothesis is also supported outside the U.S.-Mexico context: foreign-born whites and Chinese internal migrants who engage in return migration report poorer health outcomes than those remaining in receiving communities (Lu and Qin 2014; Turra and Elo 2008).
The combined response rate for these two flows is 67.7 %. Supplementary analyses of voluntary returners indicate that respondents who were unmarried, female, and earned a high school diploma or a higher level of attainment were significantly less likely to participate. We address this source of bias by controlling for such observables (excluding gender) in our analyses of Mexican-origin men.
The CHIS landline sample household response rate was 17.0 %, a product of the screener and extended interview at 31.6 % and 53.9 %, respectively; the cellphone sample household response rate was 18.3 % (screener = 33.0 %, extended interview = 55.5 %).
CHIS data were continuously collected over two years (during 7- to 9-month periods each year) in order to reduce risks related to nonrepresentativeness due to seasonality of surveying.
Among the Migrante sample, duration of stay is asked for the latest U.S. trip and does not include prior U.S. visits.
For instance, female migrants may require additional health services, including prenatal care and breast cancer screening, or could be more inclined to seek medical care than their male counterparts.
Based on the Migrante data, a higher percentage of return migrants and deportees are male (73 % and 87 %, respectively).
Although stayers appear to be advantaged compared with return migrants, their rate of health care usage are much lower than that of the overall U.S. population. In 2013, 13.4 % of all persons in the United States did not have health insurance coverage (Smith and Medalia 2014) compared with 34 % of Mexican-born stayers in our data.
We estimated similar specifications that exclude stayers with comparably less U.S. experience in light of concerns surrounding seasonal migration patterns. Because the average length of stay for Mexican-origin males is approximately three years (e.g., Reyes 2001), we excluded those who resided in the United States for less than five years (2.8 % of stayers) as a conservative test. These results, which are available upon request, are substantively similar to all results shown.
Encuesta sobre Migraciün en la Frontera Norte de México (EMIF Norte) is supported by Mexico’s Colegio de la Frontera Notre. More details are available online (http://www.colef.mx/emif/eng/bases_metodologicas.php). Results from this exercise are available upon request.
References
- Abraído-Lanza AF, Chao MT, Flórez KR. Do healthy behaviors declines with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: A test of the “salmon bias” and healthy migrant hypotheses. American Journal of Public Health. 1999;89:1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Bates LM, Osypuk TL, McArdle N. The effect of immigrant generation and duration on self-rated health among U.S. adults 2003–2007. Social Science & Medicine. 2010;71:1161–1172. doi: 10.1016/j.socscimed.2010.05.034. [DOI] [PubMed] [Google Scholar]
- Akresh IR. Dietary assimilation and health among Hispanic immigrants to the United States. Journal of Health and Social Behavior. 2007;48:404–417. doi: 10.1177/002214650704800405. [DOI] [PubMed] [Google Scholar]
- Amuedo-Dorantes C, Puttitanun T, Martinez-Donate AP. How do tougher immigration measures impact unauthorized immigrants? Demography. 2013;50:1067–1091. doi: 10.1007/s13524-013-0200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arenas E, Goldman N, Pebley AR, Teruel G. Return migration to Mexico: Does health matter? Demography. 2015;52:1853–1868. doi: 10.1007/s13524-015-0429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastida E, Brown HS, III, Pagán JA. Persistent disparities in the use of health care along the US-Mexico border: An ecological perspective. American Journal of Public Health. 2008;98:1987–1995. doi: 10.2105/AJPH.2007.114447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg SJ, Luke JV, Cynamon ML. Telephone coverage and health survey estimates: Evaluating concern about wireless substitution. American Journal of Public Health. 2006;96:926–931. doi: 10.2105/AJPH.2004.057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostean G. Does selective migration explain the Hispanic paradox? A comparative analysis of Mexicans in the U.S. and Mexico. Journal of Immigrant and Minority Health. 2013;15:624–635. doi: 10.1007/s10903-012-9646-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bustamante AV, Fang H, Garza J, Carter-Pokras O, Wallace SP, Rizzo JA, Ortega AN. Variations in healthcare access and utilization among Mexican immigrants: The role of documentation status. Journal of Immigrant and Minority Health. 2012;14:146–155. doi: 10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttenheim A, Goldman N, Pebley AR, Wong R, Chung C. Do Mexican immigrants “import” social gradients in health to the US? Social Science & Medicine. 2010;71:1268–1276. doi: 10.1016/j.socscimed.2010.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceballos M. Simulating the effects of acculturation and return migration on the maternal and infant health of Mexican immigrants in the United States: A research note. Demography. 2011;48:425–436. doi: 10.1007/s13524-011-0017-4. [DOI] [PubMed] [Google Scholar]
- Cervantes IF, Brick JM, Edwards S. Report 4: Response rates (CHIS 2011–2012 Methodology Report Series) Los Angeles, CA: UCLA Center for Health Policy Research; 2014. [Google Scholar]
- Chiquiar D, Hanson GH. International migration, self-selection, and the distribution of wages: Evidence from Mexico and the United States. Journal of Political Economy. 2005;113:239–281. [Google Scholar]
- Chirikos TN, Nestel G. Further evidence on the economic effects of poor health. Review of Economics and Statistics. 1985;67:61–69. [Google Scholar]
- Chiswick BR, Lee YL, Miller PW. Immigrant selection systems and immigrant health. Contemporary Economic Policy. 2008;26:555–578. [Google Scholar]
- Cornelius WA. Death at the border: Efficacy and unintended consequences of US immigration control policy. Population and Development Review. 2001;27:661–685. [Google Scholar]
- Crimmins EM, Soldo BJ, Kim JK, Alley DE. Using anthropometric indicators for Mexicans in the United States and Mexico to understand the selection of migrants and the “Hispanic paradox.”. Biodemography and Social Biology. 2005;52:164–177. doi: 10.1080/19485565.2005.9989107. [DOI] [PubMed] [Google Scholar]
- Dechter AR, Preston SH. Age misreporting and its effects on adult mortality estimates in Latin America. Population Bulletin of the United Nations. 1991;31–32:1–16. [PubMed] [Google Scholar]
- Dougherty M, Wilson D, Wu A. Immigration enforcement actions: 2005 (Annual report) Washington, DC: U.S. Department of Homeland Security, Office of Immigration Statistics; 2006. [Google Scholar]
- Dreby J. Everyday illegal: When policies undermine immigrant families. Oakland: University of California Press; 2015. [Google Scholar]
- Elo IT, Turra CM, Kestenbaum B, Ferguson BR. Mortality among elderly Hispanics in the United States: Past evidence and new results. Demography. 2004;41:109–128. doi: 10.1353/dem.2004.0001. [DOI] [PubMed] [Google Scholar]
- Espiritu YL. Gender and labor in Asian immigrant families. American Behavioral Scientist. 1999;42:628–647. [Google Scholar]
- Flores G. Language barriers to health care in the United States. New England Journal of Medicine. 2006;355:229–231. doi: 10.1056/NEJMp058316. [DOI] [PubMed] [Google Scholar]
- Fong VL. The other side of the healthy immigrant paradox: Chinese sojourners in Ireland and Britain who return to China due to personal and familial health crises. Culture, Medicine & Psychiatry. 2008;32:627–641. doi: 10.1007/s11013-008-9112-4. [DOI] [PubMed] [Google Scholar]
- Golash-Boza T, Hondagneu-Sotelo P. Latino immigrant men and the deportation crisis: A gendered racial removal program. Latino Studies. 2013;11:271–292. [Google Scholar]
- Goldman DP, Smith JP, Sood N. Legal status and health insurance among immigrants. Health Affairs. 2005;24:1640–1653. doi: 10.1377/hlthaff.24.6.1640. [DOI] [PubMed] [Google Scholar]
- Groot W. Adaptation and scale of reference bias in self-assessments of quality of life. Journal of Health Economics. 2000;19:403–420. doi: 10.1016/s0167-6296(99)00037-5. [DOI] [PubMed] [Google Scholar]
- Hagan JM, Rodriguez N, Castro B. Social effects of mass deportation by the United States government, 2000–10. Ethnic and Racial Studies. 2011;38:1374–1391. [Google Scholar]
- Hao L, Kim JHJ. Immigration and the American obesity epidemic. International Migration Review. 2009;43:237–262. doi: 10.1111/j.1747-7379.2009.00764.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick DM. Medical tourism: Global competition in health care (Report No. 304) Washington, DC: National Center for Policy Analysis; 2007. [Google Scholar]
- Horton S, Cole S. Medical returns: Seeking health care in Mexico. Social Science & Medicine. 2011;72:1846–1852. doi: 10.1016/j.socscimed.2011.03.035. [DOI] [PubMed] [Google Scholar]
- Hummer RA, Benjamins MR, Rogers RG. Racial and ethnic disparities in health and mortality among the U.S. elderly population. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on racial and ethnic differences in health in late life. Washington, DC: National Academies Press; 2004. pp. 53–94. [PubMed] [Google Scholar]
- Hummer RA, Biegler M, De Turk PB, Forbes D, Frisbie WP, Hong Y, Pullum SG. Race/ethnicity, nativity, and infant mortality in the United States. Social Forces. 1999;77:1083–1117. [Google Scholar]
- Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): Infant mortality among the Mexican-origin population in the United States. Demography. 2007;44:441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer RA, Rogers RG, Amir SH, Forbes D, Frisbie WP. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Social Science Quarterly. 2000;81:459–476. [PubMed] [Google Scholar]
- Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: Selectivity and acculturation. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington, DC: National Academies Press; 2004. pp. 227–266. [PubMed] [Google Scholar]
- Jürges H. True health vs response styles: Exploring cross country differences in self reported health. Health Economics. 2007;16:163–178. doi: 10.1002/hec.1134. [DOI] [PubMed] [Google Scholar]
- Kimbro RT, Bzostek S, Goldman N, Rodríguez G. Race, ethnicity, and the education gradient in health. Health Affairs. 2008;27:361–372. doi: 10.1377/hlthaff.27.2.361. [DOI] [PubMed] [Google Scholar]
- Knaul FM, Gonzales-Pier E, Gomez-Dantes O, Garcia-Junco D, Arreola-Ornelas H, Barraza-Llorens M, Frenk J. The quest for universal health coverage: Achieving social protection for all in Mexico. Lancet. 2012;380:1259–1279. doi: 10.1016/S0140-6736(12)61068-X. [DOI] [PubMed] [Google Scholar]
- Kohli A, Markowitz PL, Chavez L. Secure communities by the numbers: An analysis of demographics and due process (Chief Justice Earl Warren Institute on Law and Social Polity research report) Berkeley: University of California, Berkeley Law School; 2011. [Google Scholar]
- Ku L, Matani S. Left out: Immigrants’ access to health care and insurance. Health Affairs. 2001;20:247–256. doi: 10.1377/hlthaff.20.1.247. [DOI] [PubMed] [Google Scholar]
- Landeck M, Garza C. Utilization of physician health care services in Mexico by U.S. Hispanic border residents. Health Marketing Quarterly. 2003;20:3–16. doi: 10.1300/J026v20n01_02. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Buatista DEH. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lariscy JT, Hummer RA, Hayward MD. Hispanic older adult mortality in the United States: New estimates and an assessment of factors shaping the Hispanic paradox. Demography. 2015;52:1–14. doi: 10.1007/s13524-014-0357-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeClere FB, Jensen L, Biddlecom AE. Health care utilization, family context, and adaptation among immigrants to the United States. Journal of Health and Social Behavior. 1994;35:370–384. [PubMed] [Google Scholar]
- Lu Y, Qin L. Healthy migrant and salmon bias hypotheses: A study of health and internal migration in China. Social Science & Medicine. 2014;102:41–48. doi: 10.1016/j.socscimed.2013.11.040. [DOI] [PubMed] [Google Scholar]
- Macias EP, Morales LS. Crossing the border for health care. Journal of Health Care for the Poor and Underserved. 2001;12:77–87. doi: 10.1353/hpu.2010.0643. [DOI] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Aging, migration, and mortality: Current status of research on the Hispanic paradox. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2005;60(Special Issue 2):S68–S75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- Martinez-Donate AP, Hovell MF, Rangel MF, Zhang X, Sipan CL, Magis-Rodriguez C, Gonzalez-Fagoaga J. Migrants in transit: The importance of monitoring HIV risk among migrant flows converging on the Mexico-U.S. border. American Journal of Public Health. 2015;105:497–509. doi: 10.2105/AJPH.2014.302336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menjívar C. The intersection of work and gender: Central American immigrant women and employment in California. American Behavioral Scientist. 1999;42:601–627. [Google Scholar]
- Morales LS, Marielena L, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. Journal of Health Care for the Poor and Underserved. 2002;13:477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega AN, Fang H, Perez VH, Rizzo JA, Carter-Pokras O, Wallace SP, Gelberg L. Health care access, use of services, and experiences among undocumented Mexicans and other Latinos. Archives of Internal Medicine. 2007;167:2354–2360. doi: 10.1001/archinte.167.21.2354. [DOI] [PubMed] [Google Scholar]
- Palloni A, Arias E. Paradox lost: Explaining the Hispanic Adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox. Annals of the New York Academy of Sciences. 2001;954:140–174. doi: 10.1111/j.1749-6632.2001.tb02751.x. [DOI] [PubMed] [Google Scholar]
- Powers DA. Paradox revisited: A further investigation of racial/ethnic differences in infant mortality by maternal age. Demography. 2013;50:495–520. doi: 10.1007/s13524-012-0152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes BI. Immigrant trip duration: The case of immigrants from Western Mexico. International Migration Review. 2001;35:1185–1204. [Google Scholar]
- Rosenberg HM, Maurer JD, Sorlie PD, Johnson NJ, MacDorman MF, Hoyert DL, Scott C. Quality of death rates by race and Hispanic origin: A summary of current research, 1999 (Vital and Health Statistics, Series 2, No. 128) Hyattsville, MD: National Center for Health Statistics; 1999. [PubMed] [Google Scholar]
- Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: New findings from the Mexican Family Life Survey. American Journal of Public Health. 2008;98:78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon JA, Tandon A, Murray CJL. Comparability of self rated health: Cross sectional multi-country survey using anchoring vignettes. BMJ. 2004;328:258. doi: 10.1136/bmj.37963.691632.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner R. Paradox as paradigm—The health outcomes of Mexican Americans. American Journal of Public Health. 1996;86:303–305. doi: 10.2105/ajph.86.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simanski JF. Immigration enforcement actions: 2013 (Annual report) Washington, DC: U.S. Department of Homeland Security, Office of Immigration Statistics; 2014. [Google Scholar]
- Smith JC, Medalia C. Health insurance coverage in the United States: 2013 (Current Population Reports, No. P 60-250) Washington, DC: U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2014. [Google Scholar]
- Smith JP. Healthy bodies and thick wallets: The dual relation between health and economic status. Journal of Economic Perspectives. 1999;13(2):144–166. [PMC free article] [PubMed] [Google Scholar]
- Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: The National Longitudinal Mortality Study. American Journal of Public Health. 1995;85:949–956. doi: 10.2105/ajph.85.7.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark O, Bloom DE. The new economics of labor migration. American Economic Review. 1985;75:173–178. [Google Scholar]
- Turra CM, Elo IT. The impact of salmon bias on the Hispanic mortality advantage: New evidence from Social Security data. Population Research and Policy Review. 2008;27:515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullmann SH, Goldman N, Massey DS. Healthier before they migrate, less healthy when they return? The health of returned migrants in Mexico. Social Science & Medicine. 2011;73:421–428. doi: 10.1016/j.socscimed.2011.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hook J, Zhang W. Who stays? Who goes? Selective emigration among the foreign-born. Population Research and Policy Review. 2011;30:1–24. doi: 10.1007/s11113-010-9183-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace SP, Mendez-Luck C, Castañeda X. Heading south: Why Mexican immigrants in California seek health services in Mexico. Medical Care. 2009;47:662–669. doi: 10.1097/MLR.0b013e318190cc95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner DC. Health issues at the US-Mexican border. Journal of the American Medical Association. 1991;265:242–247. [PubMed] [Google Scholar]