Abstract
Background
A novel index, total liver LU15, has been identified as a surrogate marker for liver function. We evaluated the ability of preoperative remnant liver LU15 values to predict postoperative hepatic failure.
Methods
Preoperative risk factors for postoperative hepatic failure and remnant liver LU15 were evaluated in 123 patients undergoing liver resection for several diseases from September 1st, 2007 to December 1st, 2016. We calculated the remnant liver LU15 value from the total liver LU15 value and the functional remnant liver ratio. Risk factors for postoperative hepatic failure was determined by univariate and multivariate analysis.
Results
Hepatic failure grade B/C developed postoperatively in six patients of seven patients within Makuuchi criteria / without criteria for remnant liver LU15. Operative time (p = 0.0242) and criteria for remnant liver LU15 (p = 0.0001) were prognostic factors for hepatic failure according to the univariate analysis. And criteria for remnant liver LU15 (p = 0.0009) was only prognostic factor by multivariate analysis.
Conclusion
Based on the findings form this pilot study, it appears that patients with a remnant liver LU15 value of 13 or less may have a high risk of postoperative hepatic failure.
Keywords: Remnant liver LU15, Hepatic failure, 99mTc-labelled galactosyl human serum albumin liver scintigraphy
Background
Before a hepatectomy, it is necessary to evaluate liver function and estimate the function of the future liver remnant. Assessment of hepatic functional reserve is one of the most important issues in hepatic resection [1–4]. This is especially true for patients with both hepatocellular carcinoma (HCC) and liver cirrhosis, or both hilar cholangiocarcinoma and jaundice, that often need an extended hepatectomy. To avoid a resection that would likely lead to postoperative hepatic failure, various methods have been developed for the preoperative assessment of liver function. However, some of these are complex and require calculations involving multiple formulas. To estimate the hepatic functional reserve, 99mTc-labelled diethylene triamine pentaacetate–galactosyl-human serum albumin (99mTc-GSA), a radiopharmaceutical that binds specifically to the hepatic asialoglycoprotein receptor (ASGP-R) has been developed and used clinically to estimate hepatic function [5, 6]. Because ASGP-R is a natural superficial antigen of viable hepatocytes, the uptake of 99mTc-GSA is independent of biochemical processes and allows direct estimation of the functioning hepatocyte mass [7]. In addition, the distribution of 99mTc-GSA in the liver is not dependent on liver blood flow [8]. Koizumi et al. reported that several parameters for 99mTc-GSA liver scintigraphy were estimated and that LU3 and GSAR15 were interesting and promising parameters for assessing liver function [9].
When a hepatic resection involves more than two sections, evaluation of future functional reserve by using 99mTc-GSA and computed tomography (CT) combined fusion images is currently supposed to be more accurate than a combined estimation using an indocyanine green (ICG) retention test and CT [10]. In this study, remnant liver LU15, which was considered the remnant hepatic functional reserve, was estimated using 99mTc-GSA single-photon emission computed tomograpic (SPECT) scintigraphy and CT fusion images. In addition, the functional reserve of the future liver remnant was also estimated before surgery by using fusion images obtained from contrast-enhanced CT and 99mTc-GSA SPECT, and was used to predict liver failure after a hepatic resection. A retrospective study was performed to determine whether the remnant liver LU15 value could enable a final decision regarding a hepatectomy in order to avoid postoperative hepatic failure.
Methods
Patients
From September 1st, 2007 to December 1st, 2016 after a 99mTc-labelled galactosyl-human serum albumin liver scintigrapy, a liver resection without biliary tract reconstruction was performed in 123 patients in our department, including 72 patients with HCC, 12 with cholangiocarcinomas, and 35 with metastatic cancers (Table 1). A preoperative portal vein embolization was performed in 21 patients, because their future remnant liver volume was expected to be too small. Liver pathology was classified according to the International Association for the Study of the Liver [11], and the surgical resections were performed according to the liver anatomy of Couinaud [12].
Table 1.
Patients characteristics
| No. of patients (n = 123) | |
|---|---|
| Gender ratio M:F | M:F = 87 : 36 |
| Median age (range) | 70 (23–85) |
| Disease | |
| HCC | 72 |
| CCC | 12 |
| Metastatic | 35 |
| Others | 4 |
| Child-Pugh grade A:B | 116:7 |
| Portal vein occlusion (+) | 21 |
| Operation procedure | |
| Partial resection | 15 |
| Segmentectomy | 18 |
| Mono-sectionectomy | 31 |
| Hemihepatectomy | 53 |
| Tri-sectionectomy | 6 |
| ICG15R | 12.1 (0.3–30.7) |
| Makuuchi criteria | |
| Within | 96 |
| Without | 27 |
| Parameter from liver scintigraphy | |
| LHL15 | 0.918 (0.703–0.977) |
| HH15 | 0.623 (0.419–0.906) |
| LU15 | 26.7 (10.3–43.5) |
| remnant liver LU15 | 17.0 (3.7–43.2) |
| Criteria for remnant liver LU15 | |
| Within | 110 |
| Without | 13 |
| Postoperative hepatic failure | |
| grade B | 5 |
| grade C | 2 |
HCC Hepatocellular carcinoma, CCC Cholangiocellular carcinoma
Preoperatively, each patient was evaluated using 99mTc-GSA scintigraphy, conventional liver biochemistry tests, Child-Pugh grading, and a 15-min retention rate of indocyanine green (ICGR15) test, and the liver volume was measured from CT scans.
Calculation of remnant liver LU15
All the patients received 3 mg of 99mTc-GSA (185 MBq; Nihon Medi-Physics, Nishinomiya, Japan) as a bolus injection into the antecubital vein. Total liver LU15 was calculated from the cumulative liver uptake of the tracer 15 to 16 min after an injection of a radiotracer. The hepatic SPECT images were acquired after the dynamic study. Data analyses were performed by creating a ROI of the liver and heart and then by drawing their time-activity curves. Each set of projection data was obtained in a 128 X 128 matrix, and 72 projections were acquired. Total LU15 represents the percentage of the integral cumulative count in the liver for 1-min period from 15 to 16 min after tracer injection to total injected dose. Remnant liver LU15 was calculated as an index or residual liver function by applying the following equation; Remnant liver LU15 = Total LU15 x residual count ratio. In the recent cases, with the use of the SPECT images by scintigraphy and a three-dimensional (3D) image of the liver constructed by Synapse Vinscent (FujiFilm, Japan), the regional LU15 of the predicted remnant liver (remnant liver LU15) was calculated according to the operative procedures (Fig. 1). Remnant liver LU15 values of 13.0 and more were considered to represent a remnant liver with good liver function, according to Koizumi et al. [9, 13].
Fig. 1.
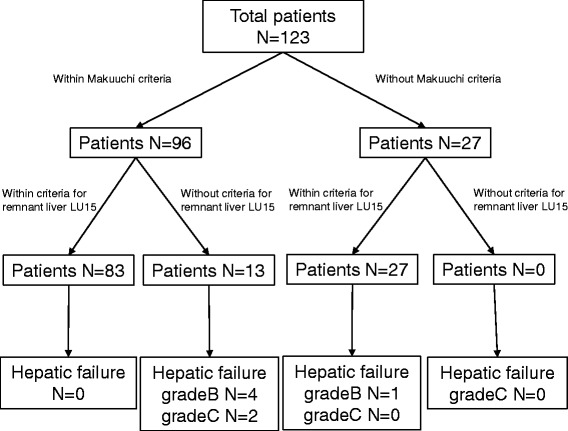
Distribution of patients according to Makuuchi criteria and remnant liver LU15 criteria. All 123 patients were distributed into 96 patients within Makuuchi crietaria and 27 patients without Makuutchi criteria. And 13 patients of 96 patients developed without remnant liver LU15 criteria and all 27 patients without Makuuchi criteria were developed within remnant liver LU15 criteria
Postoperative hepatic failure
Postoperative hepatic failure was defined according to the International Study Group of Liver Surgery (ISGLS) classification [14]. The group also differentiated the severity of postoperative liver failure into three different grades from A to C, depending on the level of treatment needed. In this study, grade B and C was defined postoperative hepatic failure. Grade B suggests the degree of liver failure needed clinical management but not invasive therapy; grade C is acute postoperative liver failure requiring invasive treatment [14].
Operative procedure
The operative procedures included the following; partial resection, segmentectomy, monosectionectomy (eg, right anterior sectionectomy, bisegmentectomy), hemihepatectomy (eg, right or left hepatectomy) and trisectionectomy (eg, right or left trisectionectomy), according to the Brisbane Nomenclature from the International Hepato-Pancreato-Biliary Association [15].
Statistical analysis
The Mann–Whitney U test was used to examine differences in the laboratory test results. The Fisher’s exact test or the χ2 test was used to compare categorical data between the groups. Correlations between the remnant liver LU15 criteria and the other laboratory test results were determined using the Pearson’s correlation coefficient. Odds ratios were used to estimate the relative risk of postoperative hepatic failure. Logistic regression was used for a univariate analysis, while a multiple logistic regression analysis was used for multivariate analysis. For a multivariate analysis, variables with significant (p < 0.05) by the univariate analysis were evaluated. P values of less than 0.05 were considered significant.
Results
The mean age of the patients was 70 years, with a range of 23 to 85 years. There were 87 (71%) male and 36 (29%) female patients, yielding a male:female ratio of 2:1; the patients’ Child-Pugh grades included A (94%) and B (6%). The surgical procedures consisted of a partial resections (15), segmentectomy (18), mono-sectionectomy (31), hemihepatectomy (53), and tri-sectionectomy (6) (Table 1). In 21 patients with portal vein occlusion, remnant liver volume increased from 490 g to 607 g.
Ninety six patients within Makuuchi criteria and 27 patients developed without Makuuchi criteria (Fig. 1). 13 patients of all 96 patients within Makuuchi criteria developed without criteria for remnant liver LU15. And 27 patients without Makuuchi criteria were within criteria for remnant liver LU15. Total seven patients developed potoperative hepatic failure over grade B. Table 2 shows the details of seven patients developed postoperative hepatic failure. Two patients developed hepatic failure grade C were performed sgmentectomy, S7/8 segmentactomy and S8 segmentectomy. All two patients died of a hepatic failure while still in the hospital.
Table 2.
Patients with postoperative hepatic failure grade B/C
| Age | Gender | Disease | Child-Pugh | PTPE | ICG15R | LU15 | Remnant liver LU15 | Operative procedure | Postoperative complication |
|---|---|---|---|---|---|---|---|---|---|
| 68 | F | CCC | A | (-) | 9.5 | 16.7 | 11.5 | Left Hemi. | HF grade B |
| 73 | F | HCC | A | (-) | 12.3 | 15.2 | 12.6 | Left Hemi. | HF grade B |
| 68 | M | HCC | A | (-) | 17.8 | 14.1 | 12.1 | Left Hemi. | HF grade B |
| 71 | M | HCC | A | (-) | 15.0 | 12.6 | 10.7 | S8 Seg. | HF grade B |
| 72 | M | HCC | A | (-) | 7.2 | 26.3 | 12.8 | S7/8 Seg. | HF grade C |
| 85 | M | HCC | A | (-) | 28.5 | 16.1 | 12.3 | S8 Seg. | HF grade C |
| 73 | M | HCC | A | (+) | 11.0 | 31.1 | 18.8 | Right Tri. | HF grade B |
CCC Cholangio carcinoma, HCC Hepatocellular carcinoma, Hemi. Hemihepatectomy, Seg. Segmentectomy, Tri. Trisectionectomy, HF Hepatic failure
Table 3 shows the hazard ratios (HR) for the candidate risk factors associated with postoperative hepatic failure as calculated by the univariate and multivariate analysis. Although serum albumin concentration, ICGR15, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and the other factors including the ICGR15 criteria by Makuuchi, et al. were not risk factors, operative time and the criteria for remnant liver LU15 were risk factors for postoperative hepatic failure by univariate analysis. And the criteria for remnant liver LU15 was an only risk factor for postoperative hepatic failure by multivariate analysis.
Table 3.
Prognostic factor for postoperative hepatic failure
| Univariate analysis | Odds ratio | 95% CI | p-value |
| Age | 1.175 | 0.950–1.351 | 0.1239 |
| Sex | |||
| Male | 1 | ||
| Female | 1.024 | 0.189–5.538 | 0.9779 |
| Child-Pugh grade | |||
| A | 1 | ||
| B | 2.944 | 0.304–6.540 | 0.3514 |
| ICG R15 | 1.001 | 0.996–1.007 | 0.5973 |
| Total billirubin | 0.004 | 0.001–7.003 | 0.1451 |
| Albumin | 0.214 | 0.019–3.656 | 0.2870 |
| AST | 0.983 | 0.921–1.049 | 0.6065 |
| Prothoronbin test | 0.946 | 0.847–1.057 | 0.3270 |
| Intraoperative blood loss | 1.000 | 0.998–1.001 | 0.6229 |
| Operation time | 1.137 | 1.017–1.271 | 0.0242 |
| LHL 15 | 0.041 | 0.007–15.070 | 0.3927 |
| HH 15 | 0.074 | 0.009–72.115 | 0.6485 |
| LU 15 | 0.965 | 0.884–1.054 | 0.9650 |
| Remnant liver LU 15 | 0.915 | 0.789–1.062 | 0.2425 |
| Makuuchi criteria | |||
| Within | 1 | ||
| Without | 1.400 | 0.257–7.640 | 0.6975 |
| Criteria for remnant liver LU15 | |||
| > 13.0 | 1 | ||
| < 13.0 | 81.750 | 8.741–764.566 | 0.0001 |
| Multivariate analysis | |||
| Operation time | 1.073 | 0.938–1.226 | 0.3041 |
| Criteria for remnant liver LU15 | 67.724 | 6.840–670.561 | 0.0009 |
Discussion
In this study, we attempted to develop a preoperative risk marker for predicting postoperative hepatic failure in patients with any diseases that were candidates for a hepatic resection using 99mTc-GSA scintigraphy. After a bolus intravenousinjection of a radiotracer, sequential anterior abdominal 128 X 128 matrix size images, including the liver and heart, were acquired every 20 s for 20 min. The parameters; HH15, LHL15 and LU15 were calculated from the time-activity curves. Two parameters, HH15 and LHL15, should be used together as complementary indications of liver function, because these parameters seem to reach a plateau value in cases of severe liver dysfunction in HH15 and in cases of liver function improvement in LHL15. In this study, HH15 and LHL15 had week correlation with ICGR15 (data not shown), and the criteria for LHL15 and HH15 were not risk factors for postoperative hepatic failure in univariate analysis. Therefore, HH15 and LHL15 might not be suitable surrogate marker for postoperative hepatic failure. Because LU15 has the advantages of a wider range and a higher value level, as well as better correlation with that of other parameters except ICGR15, LU15 is expected to be the best parameter for regional liver function and seem to be the good surrogate marker for postoperative hepatic failure.
Measurement of the remnant liver volume using planar images obtained by 99mTc-GSA scintigraphy is not accurate, but by creating a cut line in each section of the transaxial or frontal SPECT image, precise measurement of the remnant liver hepatic binding concentration is possible [16]. The amount of remnant liver LU15 could be calculated more correctly before surgery by using fusion images of 99mTc-GSA SPECT and contrast-enhanced CT scans with the Vinsent software. By using these fusion images, any resection area (partial resection, sub-segmentectomy, and any sectionectomy) could be drawn manually on SPECT scans on the basis of the anatomy observed on CT, permitting calculation of the volume of the future liver remnant. Moreover, remnant liver LU15 could be evaluated in cases with obstructive jaundice (for example, hilar cholangiocarcinoma) or a post portal vein embolization, because the hepatic asialoglycoprotein receptor is not affected by jaundice or a portal vein embolization. Thus, radioactivity within the volume of the future liver remnant could be estimated and the remnant liver LU15 values could be calculated.
Many authors have reported methods for assessing liver volume and function using a standard CT, 99mTc-GSA SPECT, or both [17, 18]. In HCC with liver cirrhosis, chronic hepatitis or fibrosis, hepatic dysfunction in the hepatic segment or lobe containing HCC was greater than that of the segments or lobe without HCC because the liver parenchyma around the tumor was damaged by mechanical compression, possibly the result of tumor compression of the vessels and bile ducts. If hepatic CT and SPECT images obtained using 99mTc-GSA were compared, the defect seen on the SPECT images was larger than that of the tumor seen on the CT image. On the other hand, for cases of hilar cholangiocarcinoma with high serum bilirubin levels, we clarified the usefulness of 99mTc-GSA volumetry because evaluation of the ICG test was unreliable, as bilirubin competes with hepatic ICG excretion. Further, a diseased liver without drainage of the obstructive bile duct showed poor functioning. Application of volumetry by 99mTc-GSA scintigraphy might address the limitations of the ICG test, as this test can evaluate separated liver functions in any situation or background liver function [19]. In this study, remnant liver volume estimated by CT volumetry was greater than that of 99mTc-GSA scintigraphy in cases of hilar cholangiocarcinoma (data not shown).
Other studies have evaluated a variety of quantitative liver function tests to predict the risk of postoperative death and complications. Conventional biochemical liver tests, such as serum bilirubin, prothrombin time, and Child-Pugh classification, have only limited value with respect to estimating the hepatocellular reserve. Yamanaka et al. reported that an ICG test, in combination with a radiologic estimation of the liver volume, was of value for predicting liver failure after a hepatectomy [20]. Kinetic analysis of hepatic ICG uptake has been a useful method to evaluate hepatic function, and has been reported to be a good preoperative predictor of death and complications in patients undergoing a liver resection for HCC [21]. The occasional discrepancy between the ICG clearance values and histologic liver findings are thought to depend mainly on the hepatic blood supply and intra/extrahepatic shunt. First, ICG retention is expected to increase in patients with jaundice, because ICG is excreted into the biliary system. Second, a rare constitutional dye excretory disorder has been reported. Moreover, as a test agent, it is well-known that ICG has some adverse reactions such as shock, nausea, rashes and itching. The ability to make a final decision about the extent of liver resection with an underlying liver disease requires new methods to estimate the functional hepatic reserve in the predicted remnant liver, rather than the entire liver.
Conclusions
Preoperative remnant liver LU15 values independently predicted hepatic failure following a liver resection for any disease, including HCC with liver cirrhosis and hilar cholangiocarcinma with obstructive jaundice. It appears that patients with a remnant liver LU15 value of 13 or less may have a high risk of postoperative hepatic failure.
Acknowledgements
Not applicable.
Funding
All authors had no funding for this research.
Availability of data and materials
All authors and all reviewer had availability of these data and materials.
Authors’ contributions
NC, KK and SK participated in the design of the study. NC drafted the manuscript and performed the statistical analysis. SK conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors performed operation procedures, read and approved the final manuscript.
Ethics approval and consent to participate
This research data was approved by Tokyo Medical University Hachioji Medical Center Ethics committee (Approval No. H175).
Consent for publication
This research data had consent of publications from all patents.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arii S, Yamada Y, Futagawa S, et al. Results of surgical and nonsurgical treatment for small-sized hepatocellular carcinomas: a retrospective and nationwide survey in Japan. The liver cancer study Group of Japan. Hepatology. 2000;32:1224–1229. doi: 10.1053/jhep.2000.20456. [DOI] [PubMed] [Google Scholar]
- 2.Nagino M, Kamiya J, Nishio H, et al. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg. 2006;243:364–372. doi: 10.1097/01.sla.0000201482.11876.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitsumori A, Nagaya I, Kimoto S, et al. Preoperative evaluation of functional reserve following hepatectomy by technetium-99m galactosyl human serum albumin liver scintigraphy and computed tomography. Eur J Nucl Med. 1998;25:1377–1382. doi: 10.1007/s002590050311. [DOI] [PubMed] [Google Scholar]
- 4.Hayashi H, Beppu T, Okabe H, et al. Functional assessment versus conventional volumetric assessment in the prediction of operative outcomes after major hepatectomy. Surgery. 2015;157:20–26. doi: 10.1016/j.surg.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Onodera Y, Takahashi K, Togashi T, et al. Clinical assessment of hepatic functional reserve using 99mTc DTPA galactosyl human serum albumin SPECT to prognosticate chronic hepatic diseases--validation of the use of SPECT and a new indicator. Ann Nucl Med. 2003;17(3):181–188. doi: 10.1007/BF02990020. [DOI] [PubMed] [Google Scholar]
- 6.Kudo M, Todo A, Ikekubo K, et al. Quantitative assessment of hepatocellular function through in vivo radioreceptor imaging with technetium 99m galactosyl human serum albumin. Hepatology. 1993;17:814–819. [PubMed] [Google Scholar]
- 7.Kwon AH, Ha-Kawa SK, Uetsuji S, et al. Use of technetium 99m diethylenetriamine-pentaacetic acid–galactosyl-human serum albumin liver scintigraphy in the evaluation of preoperative and postoperative hepatic functional reserve for hepatectomy. Surgery. 1995;117:429–434. doi: 10.1016/S0039-6060(05)80063-7. [DOI] [PubMed] [Google Scholar]
- 8.Kokudo N, Vera DR, Koizumi M, et al. Recovery of hepatic asialoglycoprotein receptors after major hepatic resection. J Nucl Med. 1999;40:137–141. [PubMed] [Google Scholar]
- 9.Koizumi K, Uchiyama G, Arai T, et al. A new liver functional study using Tc-99m DTPA-galactosyl human serum albumin: evaluation of the validity of several functional parameters. Ann Nucl Med. 1992;6:83–87. doi: 10.1007/BF03164647. [DOI] [PubMed] [Google Scholar]
- 10.Sumiyoshi T, Shima Y, Okabayashi T, et al. Liver function assessment using 99mTc-GSA single-photon emission computed tomography (SPECT)/CT fusion imaging in hilar bile duct cancer: a retrospective study. Surgery. 2016;160(1):118–126. doi: 10.1016/j.surg.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Anthony PP, Ishak KG, Nayak NC, et al. The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health Organization. J Clin Pathol. 1978;31:395–414. doi: 10.1136/jcp.31.5.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Couinaud C. Surgical anatomy of the liver. Several new aspects. Chirurgie. 1986;112:337–342. [PubMed] [Google Scholar]
- 13.Uetake M, Koizumi K, Yagawa A, et al. Use of Tc-99m DTPA galactosyl human serum albumin to predict postoperative residual liver function. Clin Nucl Med. 1999;24(6):428–434. doi: 10.1097/00003072-199906000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the international study Group of Liver Surgery (ISGLS) Surgery. 2011;145:713–724. doi: 10.1016/j.surg.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 15.Kubota K, Makuuchi M, Kusaka K, et al. Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resectional surgery for hepatic tumors. Hepatology. 1997;26:1176–1181. doi: 10.1053/jhep.1997.v26.pm0009362359. [DOI] [PubMed] [Google Scholar]
- 16.Kwon AH, Ha-Kawa SK, Uetsuji S, et al. Preoperative determination of the surgical procedure for hepatectomy using technetium-99m-galactosyl human serum albumin (99mTc-GSA) liver scintigraphy. Hepatology. 1997;25:426–429. doi: 10.1002/hep.510250228. [DOI] [PubMed] [Google Scholar]
- 17.Beppu T, Nitta H, Hayashi H, et al. Effect of branched-chain amino acid supplementation on functional liver regeneration in patients undergoing portal vein embolization and sequential hepatectomy: a randomized controlled trial. J Gastroenterol. 2015;50(12):1197–1205. doi: 10.1007/s00535-015-1067-y. [DOI] [PubMed] [Google Scholar]
- 18.Yoshida M, Beppu T, Shiraishi S, et al. (99m)Tc-GSA SPECT/CT fused images for assessment of hepatic function and hepatectomy planning. Ann Transl Med. 2015;3(2):17. doi: 10.3978/j.issn.2305-5839.2014.12.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nanashima A, Yamaguchi H, Shibasaki S, et al. Relationship between indocyanine green test and technetium-99m galactosyl serum albumin scintigraphy in patients scheduled for hepatectomy: clinical evaluation and patient outcome. Hepatol Res. 2004;28:184–190. doi: 10.1016/j.hepres.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Yamanaka N, Okamoto E, Oriyama T. A prediction scoring system to select the surgical treatment of liver cancer. Further refinement based on 10 years of use. Ann Surg. 1994;219:342–346. doi: 10.1097/00000658-199404000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lau H, Man K, Fan ST, et al. Evaluation of preoperative hepatic function in patients with hepatocellular carcinoma undergoing hepatectomy. Br J Surg. 1997;84:1255–1259. doi: 10.1002/bjs.1800840917. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All authors and all reviewer had availability of these data and materials.


