Abstract
Purpose
Cervical cancer is a common cancer among women worldwide. An estimated 528,000 new cases and 266,000 deaths occurred in 2012. More than 85% of invasive cervical cancer cases occur in low- and middle-income countries. Cervical cancer ranks as the most common cancer among women in Ghana. We conducted a retrospective study to assess the descriptive epidemiology of cervical cancer in Ghana. We describe cervical cancer incidence and mortality rates for the regions served by two large hospitals in Ghana.
Patients and Methods
Information for women diagnosed with invasive cervical cancer between 2010 and 2013 was collected from the Komfo Anokye and Korle Bu Teaching Hospitals through review of medical, computer, and pathology records at the oncology units and the obstetrics and gynecology departments. Telephone interviews were also conducted with patients and relatives. Data were analyzed using summary statistics.
Results
A total of 1,725 women with cervical cancer were included in the study. Their ages ranged from 11 to 100 years (mean, 56.9 years). The histology of the primary tumor was the basis of diagnosis in 77.5% of women and a clinical diagnosis was made in 22.5% of women. For the 1,336 women for whom tumor grade was available, 34.3% were moderately differentiated tumors. Late stage at presentation was common. The incidence and mortality rates of cervical cancer increased with age up until the 75 to 79–year age group and began to decrease at older ages. The Greater Accra region had higher overall incidence and mortality rates than the Ashanti region.
Conclusion
Our study suggests that improvements in the application of preventive strategies could considerably reduce the burden of cervical cancer in Ghana and other low- and middle-income countries. The study provides important information to inform policy on cancer prevention and control in Ghana.
INTRODUCTION
Cancer causes more deaths in the world than HIV/AIDS, tuberculosis, or malaria.1 Among female cancers, cervical cancer is the fourth most common in the world, with an estimated 528,000 new cases in 2012.2 Despite the fact that cervical cancer is potentially preventable through vaccination and screening, more than 250,000 women per annum are estimated to die of the disease worldwide.2 Incidence and mortality have declined in most high-income countries, mainly as a result of the introduction of cervical screening. However, this is not the case in most low- and middle-income countries, where approximately 85% of the disease occurs.2 The incidence and mortality rates are high in Africa and some parts of Asia, and are low in Australasia and West Asia.2
In Ghana, cervical cancer is the most common cancer among women, with an estimated 3,052 new cases and 1,556 deaths in 2012.2 Despite the magnitude of the problem, accurate data on cervical cancer incidence and mortality are not available. Currently, there are two hospital-based cancer registries, located in the two large tertiary referral hospitals: Komfo Anokye Teaching Hospital (KATH), Kumasi, and Korle Bu Teaching Hospital (KBTH), Accra. These hospitals are the main referral centers where patients with malignancy are diagnosed and treated, and they see most cases of cervical cancer in Ghana, receiving referrals from all over the country.
The registry at KATH has recently been converted into a population-based cancer registry to cover the city of Kumasi. Ghana is divided into 10 administrative regions. The KATH total catchment area covers approximately 50% of the population of Ghana.3 The KBTH catchment area covers the entire southern part of Ghana, but the hospital also receives patients from other parts of the country. Hence its catchment area is not as well defined.4
Several studies of cancer in Ghana have focused on all cancers and have mainly been institution-based studies without a reference population.5-7 Additionally, no previous research has tried to assess both the cervical cancer incidence and mortality in Ghana and link the data from the two referral hospitals. Knowing the incidence and mortality rates of cervical cancer is important for the formulation of policy and implementation of control measures. This study examined the characteristics of cases of cervical cancer in Ghana and estimated the incidence and mortality rates in two regions of the country.
PATIENTS AND METHODS
The study population consisted of all histologically confirmed and suspected cases of invasive cervical cancer in the oncology units and the obstetrics and gynecology departments at the KATH and the KBTH between 2010 and 2013. We reviewed paper-based (medical), electronic, and pathology records at the oncology units and the obstetrics and gynecology departments of the two hospitals. We collected information about women newly diagnosed with invasive cervical cancer during the 2010 to 2013 time period.
One hundred twenty-eight deaths from cervical cancer were recorded in patients’ medical records. Most of the women were lost to follow-up at the two hospitals. Hence information on the outcome of disease (whether women were alive or dead) could not be obtained from review of paper-based and electronic records for the majority of women. However, we attempted to contact all women with a diagnosis of cervical cancer by telephone to obtain basic descriptive and outcome information for this study. For those who could not be reached as a result of death or other reasons, their relatives were contacted. For some women with cervical cancer, the hospital did not have any contact information.
For each department, available information for women with cervical cancer was abstracted from paper-based, electronic, and pathology records onto a standard data collection sheet. Once data from all departments were reviewed for accuracy, the following variables were used to link cases between departments: histology report number, patient’s name, age, and telephone number. After linking the data from the two departments and removing duplicates, data were stripped of all identifiers and the final data set was defined for analysis. Because deaths from cervical cancer were only obtained for cases from 2010, only the mortality rates for the 2012 to 2013 periods are presented because most women in Ghana who die as a result of cervical cancer do so within 2 years.
Approval to conduct the study was sought from the University of Otago Ethics (Health) Committee, Ghana Health Service Ethical Committee and the Committee on Human Research, Publication and Ethics of the Kwame Nkrumah University of Science and Technology and KATH, Ghana. The two hospitals also have internal ethical committees that assess proposed research to take place in the hospitals; the research was also submitted to these committees.
Statistical Analysis
We used STATA version 12.1 (STATA Corporation, College Station, TX) for the data analysis. Frequencies were run for all variables for the purposes of describing proportions or percentages. Statistical tests were performed using the χ2 and Fisher’s exact tests. Statistical significance was determined at a P value < .05.
Population data from the Greater Accra and Ashanti regions were obtained from the 2010 Population and Housing Census in Ghana. The census provided information on the population by region of residence, age, and sex.8 The census data were not extrapolated for 2011 to 2013 because little increase in population was expected for that time period. The population data from the Ghana Statistical Service showed that there was a < 1% increase in the population from 2010 to 2013.
The place of residence was obtained from the medical records and was verified during telephone interview for those who could be contacted. The place of residence had not changed for the majority of women (approximately 95%) and was similar to that recorded in the medical records. To calculate the person-years, the number of females in a region (as estimated by the 2010 census) was multiplied by four (the number of years the cases were accrued) for each age group for incidence and by two for mortality.
Cervical cancer mortality rates were also calculated. Death ascertainment was done by telephone interview of relatives and review of medical records. The deaths recorded in the medical records agreed with those obtained by telephone interview when relatives of women were contacted. To provide regional comparisons adjusted for age, the age-standardized rate (ASR; with 95% CI) was calculated using the direct method and applied to the WHO world standard population for each region.9 For crude and age-specific rates, 95% CIs were calculated using the binomial exact method.
RESULTS
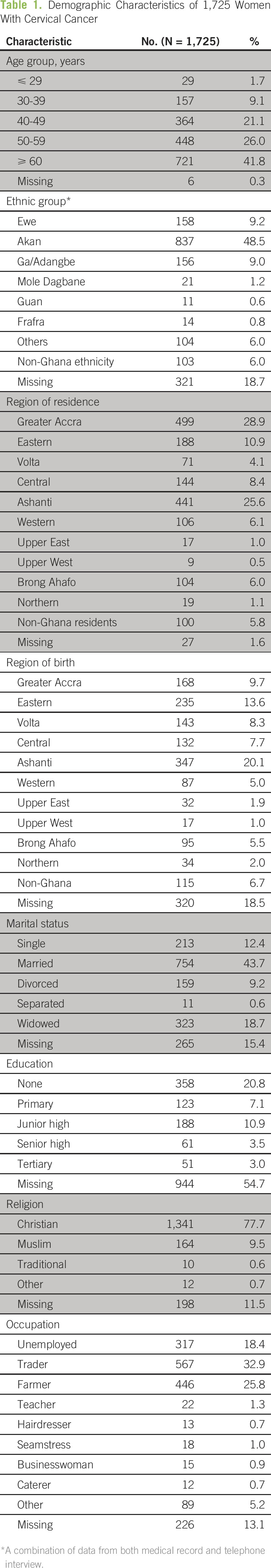
The basic demographic characteristics of women diagnosed with cervical cancer (recorded) are shown in Table 1. A total of 1,725 women with cervical cancer were identified for the 2010 to 2013 time period in the two hospitals. The majority of women with cervical cancer were recruited through the records of the oncology units. The mean age at diagnosis was 56.9 years (range, 11 to 100 years). One subject, whose age was recorded as 11 years, was diagnosed with adenocarcinoma of the cervix. However, the type of adenocarcinoma was not stated. Most of the women (58.7%) with cervical cancer were of a trader or farmer occupation.
Table 1.
Demographic Characteristics of 1,725 Women With Cervical Cancer
Histology of the primary site formed the basis of the diagnosis for the majority of the women (Table 2). Among women with histologically confirmed cervical cancer, squamous cell carcinoma was the most common histologic type (64.9%). Among those for whom tumor grade was available, moderate differentiation was most common (34.3%). The size of the cervical tumor was not measured for most of the women (54.1%). The distribution of International Federation of Gynecology and Obstetrics stages were as follows: stage I, n = 90 (5.2%), stage II, n = 428 (24.8%), stage III, n = 631 (36.6%), and stage IV, n = 162 (9.4%). For 24% of women, no staging was recorded, although 40% of the 414 with no stage were documented as having advanced disease. There was a statistically significant difference between the two hospitals with respect to tumor characteristics (Table 3). Younger women were more likely to receive both external beam radiation and brachytherapy compared with older women (data not shown).
Table 2.
Tumor Characteristics

Table 3.
Distribution of Tumor Characteristics Between Komfo Anokye Teaching Hospital and Korle Bu Teaching Hospital

Table 4 shows the age-specific incidence rates for the Greater Accra and Ashanti regions for the period 2010 to 2013. There were 949 and 676 women with newly diagnosed cervical cancer at KBTH and KATH, respectively, during the 2010 to 2013 time period. The largest number of cases was diagnosed for the Greater Accra region. The majority of women with cervical cancer were ≥ 40 years of age.
Table 4.
Age-Specific Incidence Rate (per 100,000 person-years) for Greater Accra and Ashanti Regions for the Period 2010 to 2013

The crude incidence rates for the Greater Accra and Ashanti regions during the 2010 to 2013 period were 14.5 (95% CI, 13.6 to 15.4) and 9.1 (95% CI, 8.4 to 9.8) per 100,000 person-years, respectively. As expected, the incidence of cervical cancer increased with age for both regions. The incidence rates began to increase noticeably from age 25 to 29 years for Greater Accra and 30 to 34 years for the Ashanti region. Incidence rates were highest for women 70 to 74 years of age in Greater Accra (113.8; 95% CI, 92.3 to 138.9) and women 75 to 79 years of age in the Ashanti region (91.3; 95% CI, 71.6 to 114.8). The ASR (world standard population) for the Greater Accra and Ashanti regions for incidence was 24.5 (95% CI, 22.9 to 26.1) and 14.0 (95% CI, 12.9 to 15.1) per 100,000, respectively.
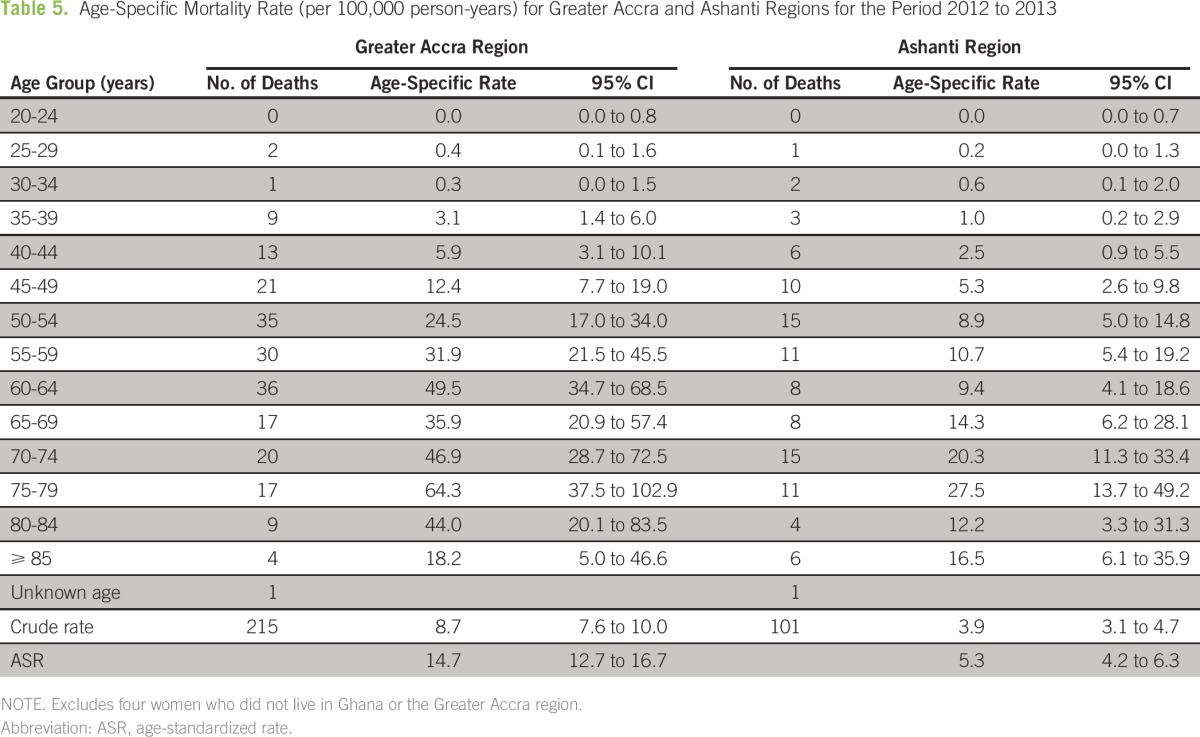
Table 5 presents the age-specific mortality for Greater Accra and the Ashanti region for the period 2012 to 2013. A total of 215 and 101 deaths from cervical cancer were recorded at KBTH and KATH, respectively, between 2012 and 2013. The majority of deaths from cervical cancer occurred in women ≥ 40 years of age. Mortality rates also increased to 75 to 79 years of age for both regions. The crude mortality rate was higher for Greater Accra (8.7; 95% CI, 7.6 to 10.0) compared with the Ashanti region (3.9; 95% CI, 3.1 to 4.7). The ASR (world standard population) for mortality was also higher in the Greater Accra region (14.7; 95% CI, 12.7 to 16.7) compared with the Ashanti region (5.3; 95% CI, 4.2 to 6.3).
Table 5.
Age-Specific Mortality Rate (per 100,000 person-years) for Greater Accra and Ashanti Regions for the Period 2012 to 2013
DISCUSSION
In this study, we found that the majority of the women with cervical cancer in Ghana presented with advanced disease. We also estimated the incidence and mortality rates of cervical cancer in two large regions of the country. These data provide important information that can be compared with the findings from other studies and global estimates with respect to the epidemiology of cervical cancer.
That the majority of the women with cervical cancer presented with advanced disease is consistent with findings from other parts of Africa.10-13 This may be related to personal factors as well as poor access to health care. Patients may delay visiting the hospital because they are not aware of the signs and symptoms of the disease, and the cost of diagnosis and treatment may be an impediment. Studies have reported a low level of knowledge of cervical cancer among Ghanaian women and men.14,15 Additionally, traditional and alternative medical practitioners constitute a significant proportion of the health care delivery system in Ghana. Because of their accessibility, affordability, and cultural role, traditional medicines are an important aspect of the health system. These practitioners are the first point of contact for many health-related issues and this is often associated with a late stage of cancer at diagnosis.12,16 The occupations of trader or farmer were the most common among women with cervical cancer. These occupations have been associated with cervical cancer in some studies.17,18
The incidence rates of cervical cancer across the two regions in this study were lower than the Globocan estimate of 35.4 per 100,000 populations,2 which used rates in neighboring populations to estimate the rates in Ghana. Not all possible data sources in the Greater Accra and Ashanti regions were able to be included in the data collection. There are three hospitals that offer radiotherapy for cancer: KATH, KBTH, and the Swedish Ghana Medical Centre. The latter is a private oncology center that provides radiotherapy (excluding brachytherapy) and chemotherapy but not surgery. Patients attending this hospital are those who can afford private medical care. Thus, the majority of women are more likely to be referred to KATH and KBTH.
There are also three hospitals that offer radical surgery for gynecologic cancer: KATH, KBTH, and Battor Catholic Hospital. Data were not obtained from the Battor Catholic Hospital. However, some women were referred to KBTH from this hospital. Women who require radiotherapy are mostly referred to KATH and KBTH because these are the only hospitals in the country with the requisite human resources and logistics to manage cancer cases.19
The study may also have missed cases among residents who may have sought treatment outside the two regions or had not been diagnosed before death. The exact number of cases is difficult to estimate because there currently exists no national database of cases of diseases seen in other health facilities.19 With the few radiotherapy centers in West Africa, it is unlikely that women would have obtained treatment in other countries.
Some women were clinically diagnosed with cervical cancer without histologic confirmation. For women with cervical cancer identified through the review of electronic records at the obstetrics and gynecology department at KBTH, the electronic records had no information on histology reports. The pathology records at the pathology department were reviewed to identify the histology reports of these women. Only a few pathology reports (5.4%) were obtained directly from the pathology department at KBTH. The pathology reports for the rest of the women diagnosed with cervical cancer, as recorded from the electronic records at KBTH, were not located. It is probable that biopsies were not performed for those women or that the samples were taken to a laboratory outside of these hospitals. Additionally, it could be the case that patients refused to return to the hospital for a biopsy to be done. This information could not be verified because patients of the obstetrics and gynecology department at KBTH take their medical folders home (ie, the folder that contains the patient’s medical records). From the review of paper-based medical records, < 1% of women with an initial clinical diagnosis of cervical cancer had a later histology report that did not agree with the clinical diagnosis. Additionally, because women were referred from other hospitals, there was little chance that the two physicians would both misdiagnose the disease.
It is unlikely that women with cervical cancer have been misclassified in this study. After cases were recorded, they were cross-checked carefully by a gynecologic oncologist and the study team to ensure that cases met suitable diagnostic criteria. However, the high number of women for whom some of the data were missing limits the precision of some of the results obtained.
The Greater Accra region had the highest cervical cancer incidence and mortality rates. One possible explanation for the higher incidence rates in the Greater Accra region may include the geographical coverage of KBTH, urbanization, and a historically high prevalence of sexually transmitted infections in the region. The estimate for the Ashanti region was higher than what has been reported in previous studies.19,20
The incidence of cervical cancer increased with age in this study. Of interest, the incidence increased with ages from 50 to 54 years when a reduction at older ages is more common.2 However, the higher than expected incidence in older ages may represent high exposure to human papillomavirus (HPV) in these generations when they were younger or an older age at diagnosis. In this study, cervical cancer incidence peaked in women 75 to 79 years of age in the Ashanti region and 70 to 74 years old in the Greater Accra region. It is possible that exposure to HPV may have been, on average, at a younger age in the Greater Accra region.
The presence of high-risk oncogenic HPV DNA is the major cause of cervical cancer. In most populations, the prevalence of HPV DNA is higher among sexually active young women.21-23 However, a second peak in HPV DNA prevalence at older ages has been reported in some countries, particularly those in Southern America and Africa.24-26 Currently, the age-specific prevalence of HPV DNA among the Ghanaian female population is unknown. However, a second peak in HPV DNA prevalence might be expected in middle-aged women on the basis of the high cervical cancer incidence rate reported for older women.
The cervical cancer mortality also increased with age in this study. This is a common observation.2 Younger women were more likely to have cervical cancer of an earlier stage compared with older women, possibly because they were more likely to recognize symptoms early or were diagnosed through screening at antenatal clinics. In addition to the stage at presentation, younger women were more likely to receive therapy with a curative intent, which may contribute to the lower mortality rates in younger women.
In conclusion, this study has provided a summary of the epidemiology of cervical cancer in Ghana. Late stage at diagnosis was common, and it is clear that cervical cancer is an important public health issue. Considerable improvement in patient outcomes in low- to middle-income countries may be achieved through initially raising awareness and knowledge of the disease to encourage risk reduction and early diagnosis.
ACKOWLEDGMENT
We thank the staff of the Komfo Anokye Teaching Hospital (KATH) and the Korle Bu Teaching Hospital (KBTH) cancer registries for assisting with case ascertainment. We are extremely grateful to all of those who contributed in various ways to the study and acknowledge Nelson Damale, MD, Samuel Anenyi Obed, MD, R.A. Kwame Aryee, MD, Mumuni Kareem, MD, Baawiah Osei Bonsu, MD, Nana Afriyie, Asobonteng Attah Nkrumah, Joycelyn Sarfo-Frimpong, Baffour Awuah Ofosu, Nancy Appiah, Freda Kwarteng Boampong, Agartha Agyei Boadi, Mallet Sankah Kodi, Philip Oduro, Isaac Agyemang Duah, Charles Akoto Aidoo, Ernest Agbenyeke, and Raymond Atiemo Danso for their great work during the data collection at the KATH and the KBTH.
Footnotes
Supported by the Directors' Cancer Research Trust (B.C.). The Department of Preventive and Social Medicine and the Directors’ Cancer Research Trust provided funding for the study.
AUTHOR CONTRIBUTIONS
Conception and design: Yvonne Nartey, Philip C. Hill, Kwabena Amo-Antwi, Kofi M. Nyarko, Brian Cox
Financial support: Brian Cox
Administrative support: Kofi M. Nyarko, Joel Yarney, Brian Cox
Provision of study materials or patients: Brian Cox
Collection and assembly of data: All authors
Data analysis and interpretation: Yvonne Nartey, Philip C. Hill, Brian Cox
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO’s conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Yvonne Nartey
No relationship to disclose
Philip C. Hill
No relationship to disclose
Kwabena Amo-Antwi
No relationship to disclose
Kofi M. Nyarko
No relationship to disclose
Joel Yarney
No relationship to disclose
Brian Cox
No relationship to disclose
REFERENCES
- 1. American Cancer Society: Overview of the global cancer and tobacco burden, and our global programs. http://www.cancer.org/aboutus/globalhealth/ourglobalprograms/index.
- 2. Ferlay J, Soerjomataram I, Ervik M, et al: GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France, International Agency for Research on Cancer, 2013. http://globocan.iarc.fr.
- 3.Komfo Anokye Teaching Hospital . Annual Report 2012. Kumasi, Ghana: Komfo Anokye Teaching Hospital; 2012. [Google Scholar]
- 4.Calys-Tagoe BN, Yarney J, Kenu E, et al. Profile of cancer patients’ seen at Korle Bu Teaching Hospital in Ghana (a cancer registry review) BMC Res Notes. 2014;7:577. doi: 10.1186/1756-0500-7-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wiredu EK, Armah HB. Cancer mortality patterns in Ghana: A 10-year review of autopsies and hospital mortality. BMC Public Health. 2006;6:159. doi: 10.1186/1471-2458-6-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gyasi R, Tettey Y. Childhood deaths from malignant neoplasms in Accra. Ghana Med J. 2007;41:78–81. doi: 10.4314/gmj.v41i2.55306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Der EM, Gyasi RK, Tettey Y, et al. Triple-negative breast cancer in Ghanaian women: The Korle Bu Teaching Hospital experience. Breast J. 2015;21:627–633. doi: 10.1111/tbj.12527. [DOI] [PubMed] [Google Scholar]
- 8. Ghana Statistical Service: 2010 Population and Housing Census. Summary Report of Final Results. Accra, Ghana, Sakoa Press Limited, 2012. [Google Scholar]
- 9.Ahmad O, Boschi-Pinto C, Lopez AD, et al. Age Standardization of Rates: A New WHO Standard. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 10.Maranga IO, Hampson L, Oliver AW, et al. Analysis of factors contributing to the low survival of cervical cancer patients undergoing radiotherapy in Kenya. PLoS One. 2013;8:e78411. doi: 10.1371/journal.pone.0078411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clegg-Lamptey J, Hodasi W. A study of breast cancer in Korle Bu Teaching Hospital: Assessing the impact of health education. Ghana Med J. 2007;41:72–77. doi: 10.4314/gmj.v41i2.55305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clegg-Lamptey J, Dakubo J, Attobra YN. Why do breast cancer patients report late or abscond during treatment in Ghana? A pilot study. Ghana Med J. 2009;43:127–131. [PMC free article] [PubMed] [Google Scholar]
- 13.Anorlu RI, Orakwue CO, Oyeneyin L, et al. Late presentation of patients with cervical cancer to a tertiary hospital in Lagos: What is responsible? Eur J Gynaecol Oncol. 2004;25:729–732. [PubMed] [Google Scholar]
- 14.Ebu NI, Mupepi SC, Siakwa MP, et al. Knowledge, practice, and barriers toward cervical cancer screening in Elmina, Southern Ghana. Int J Womens Health. 2014;7:31–39. doi: 10.2147/IJWH.S71797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams MS, Amoateng P. Knowledge and beliefs about cervical cancer screening among men in Kumasi, Ghana. Ghana Med J. 2012;46:147–151. [PMC free article] [PubMed] [Google Scholar]
- 16.Clegg-Lamptey JN, Dakubo JC, Attobra YN. Psychosocial aspects of breast cancer treatment in Accra, Ghana. East Afr Med J. 2009;86:348–353. doi: 10.4314/eamj.v86i7.54152. [DOI] [PubMed] [Google Scholar]
- 17.Adewuyi SA, Shittu SO, Rafindadi AH. Sociodemographic and clinicopathologic characterization of cervical cancers in northern Nigeria. Eur J Gynaecol Oncol. 2008;29:61–64. [PubMed] [Google Scholar]
- 18.Alterman T, Burnett C, Peipins L, et al. Occupation and cervical cancer: An opportunity for prevention. J Womens Health. 1997;6:649–657. doi: 10.1089/jwh.1997.6.649. [DOI] [PubMed] [Google Scholar]
- 19.Laryea DO, Awuah B, Amoako YA, et al. Cancer incidence in Ghana, 2012: Evidence from a population-based cancer registry. BMC Cancer. 2014;14:362. doi: 10.1186/1471-2407-14-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Brien KS, Soliman AS, Awuah B, et al. Establishing effective registration systems in resource-limited settings: Cancer registration in Kumasi, Ghana. J Registry Manag. 2013;40:70–77. [PMC free article] [PubMed] [Google Scholar]
- 21.Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007;297:813–819. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 22.Bauer HM, Hildesheim A, Schiffman MH, et al. Determinants of genital human papillomavirus infection in low-risk women in Portland, Oregon. Sex Transm Dis. 1993;20:274–278. doi: 10.1097/00007435-199309000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Burk RD, Kelly P, Feldman J, et al. Declining prevalence of cervicovaginal human papillomavirus infection with age is independent of other risk factors. Sex Transm Dis. 1996;23:333–341. doi: 10.1097/00007435-199607000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Lazcano-Ponce E, Herrero R, Muñoz N, et al. Epidemiology of HPV infection among Mexican women with normal cervical cytology. Int J Cancer. 2001;91:412–420. doi: 10.1002/1097-0215(20010201)91:3<412::aid-ijc1071>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 25.Herrero R, Castle PE, Schiffman M, et al. Epidemiologic profile of type-specific human papillomavirus infection and cervical neoplasia in Guanacaste, Costa Rica. J Infect Dis. 2005;191:1796–1807. doi: 10.1086/428850. [DOI] [PubMed] [Google Scholar]
- 26.Thomas JO, Herrero R, Omigbodun AA, et al. Prevalence of papillomavirus infection in women in Ibadan, Nigeria: A population-based study. Br J Cancer. 2004;90:638–645. doi: 10.1038/sj.bjc.6601515. [DOI] [PMC free article] [PubMed] [Google Scholar]


